Abstract
Objective:
To describe the deployment of otolaryngologists and evaluate factors associated with the geographic distribution of otolaryngologists in the United States
Design:
Cross-sectional study
Methods:
The otolaryngology physician supply was defined as the number of otolaryngologists per 100,000 in the hospital referral region (HRR). The otolaryngology physician supply was derived from American Medical Association (AMA) Masterfile or from the Medicare Enrollment and Provider Utilization Files. Multiple linear regression tested the association of population, physician and hospital factors on the supply of Medicare-enrolled otolaryngologists/HRR.
Results:
Two methods of measuring the otolaryngology workforce were moderately correlated across hospital referral regions (Pearson coefficient 0.513, p=.0001); the supply of otolaryngology providers varies greatly over different geographic regions. Otolaryngologists concentrate in regions with many other physicians, particularly specialist physicians. The otolaryngology supply also increases with regional population income and education levels. Using AMA- derived data, there was no association between the supply of otolaryngologists and staffed acute care hospital beds or the presence of an otolaryngology residency-training program. In contrast, the supply of otolaryngology providers enrolled in Medicare independently increases for each HRR by 0.8/100,000 for each unit increase in supply of hospital beds (p<.0001) and by 0.49/100,000 in regions with an otolaryngology residency training program (p=.006), accounting for all other factors.
Conclusions:
Irrespective of methodology, the supply of otolaryngologists varies widely across geographic regions in the United States. For Medicare beneficiaries, regional hospital factors including presence of an otolaryngology residency program may improve access to otolaryngology services.
Keywords: workforce, otolaryngology, distribution, Medicare, access
Introduction
Over the next several decades, the medical needs of the aging population are expected to increase. In light of anticipated changes, concerns about the adequacy of the otolaryngology workforce have been raised1,2, and remains a subject of considerable controversy3-8. Yet physician maldistribution 9,10 and the selective participation of physicians in specific health plans including Medicare could effectively induce relative shortages in some regions, resulting in failure to meet contemporary local health care needs.
The optimal method of measuring the otolaryngology workforce remains unsettled. Prior studies in otolaryngology have used databases of otolaryngologists participating in private insurance health plans4 or data derived from the American Academy of Otolaryngology-Head and Neck Surgery membership, which correlate closely with the American Medical Association (AMA) Masterfile11. Most physician workforce calculations of other physician groups use a headcount of physicians derived from the AMA Masterfile, the primary source of data on all physicians in the United States12,13. However, the AMA Masterfile contains information collected from physician surveys that may not accurately reflect clinical activity and do not consider the types of insurance plans the physicians participate in. An adequate supply of physicians may not meet demand if there is inadequate participation in Medicare and other health plans, or in the face of limited physician productivity. Consequently alternative methods of measuring the physician supply have been devised based on Medicare claims data14. Both the AMA Masterfile and CMS/ Physician Compare database have been used to track the physician workforce in other specialties such as oncology15.
Moreover, workforce calculations often fail to account for physician maldistribution. The distribution of the physician workforce has been called irrational 16, because it does not appear to be related to the health needs of the population; instead, the physician supply has been associated with measurable local population characteristics, physician specialty mix, hospital system factors and insurance provider types, which influence the local physician carrying capacity 17,18. Thus the supply of physicians is partly determined by the medical needs of the community, partly by the community’s financial resources, the supply of hospital resources and other physicians and providers18.
In this study, the otolaryngology supply derived from Medicare enrollment and utilization data was compared with a measure derived from the AMA Masterfile. We tested these two measures of otolaryngology physician supply against factors associated with the local physician carrying capacity: population-level demographic and socioeconomic characteristics, the regional physician provider supply, hospital capacity measures and the presence of an otolaryngology residency-training program. We hypothesized that regional otolaryngology physician supply was not random, but associated with local physician market characteristics and health system factors.
Materials and methods
Physician supply definitions
The size of the physician workforce was defined as the number of physicians per 100,000 residents of a hospital referral region (HRR). The supply of otolaryngologists by HRR was obtained from the Dartmouth Atlas Project (www.DartmouthAtlas.org). This measure was derived from the AMA Masterfile that included otolaryngologists (but not residency trainees) 26-65 years old who spent at least 20 hours per week in clinical practice. The supply of otolaryngologists enrolled in Medicare was calculated using data obtained from the Centers for Medicare and Medicaid Services (CMS) Physician Compare website and the CMS Medicare Provider Utilization File from 2012 and 2013. The zip code listed in the Medicare Provider Enrollment, Chain, and Ownership System (PECOS) enrollment form, representing the physician practice address was used to map unique otolaryngology-specific national provider identification numbers (NPIs) to a geographic unit, the HRR. When there was a discrepancy between addresses listed in the PECOS and PUF file, the PECOS address was used.
Extraction from the CMS data yielded 9821 otolaryngology providers in the United States. Eighty-one from Puerto Rico and the Virgin Islands were subsequently excluded. Each provider was mapped to one of 306 HRRs. The supply of otolaryngologists enrolled in Medicare was defined as the number of enrolled otolaryngologists per 100,000 total population in the HRR.
Hospital factors
The number of staffed hospital beds was derived from the American Hospital Association database for 2013. The supply of acute care hospital beds was defined as the number of staffed hospital beds per 1000 residents in the HRR. Hospital teaching status was derived from the American Association of Medical Colleges (AAMC) and the AHA. The presence of an American Council of Graduate Medical Education (ACGME)-accredited residency program was derived from the American Association of Medical Colleges.
Population and Medicare beneficiary factors
The mean population age, percent female, African-American and Hispanic were obtained from the United States Census for 2010. Mean income and percent of the population with a Bachelors degree or greater was obtained from the American Home Survey.
Statistical analysis
Changes in the supply of otolaryngologists/ HRR over time was tested using the AMA-derived dataset for 1996, 2006 and 2011 using a paired t-test. Pearson correlations were used to describe the relationships between otolaryngologist supply and population, physician, and hospital characteristics at the HRR level. Multiple linear regression was used to evaluate predictors of Medicare-enrolled physician supply by HRR. Predictors included population demographics, income, and education data from the United States Census. Of the physician groups considered, physicians likely to serve as referral sources or competitors to otolaryngologists in a region were included in the multivariable model. The choice of predictors was based on a framework of physician carrying capacity described by Jiang and Rundall17,19. R software version 3.2 was used for multivariable modeling. Statistical tests were two sided and significant at the p=.05 level. A study exemption was obtained from the Institutional Review Board at the Fox Chase Cancer Center, Temple University Health System.
Results
Otolaryngology supply measures
The supply of otolaryngologists by HRR, obtained from the Dartmouth Atlas group revealed that the supply of otolaryngologists per HRR decreased slightly between 1996 and 2011 (mean 2.73 to 2.66,p=.029). The supply ranged between 1.01-5.38/100,000 in 1996 (SD .66); 1.18-5.31/100,000 in 2006 (SD .65) and 1.18-5.67/100,000 in 2011 (SD .65). The decrease in the mean supply of otolaryngologists over time was much smaller than the standard deviation of otolaryngology supply across geographic regions (.06/100,000 vs .65/100,000). Thus the decrease in the mean supply of otolaryngologists by HRR was far smaller than the differences in the mean supply of otolaryngologists across HRRs.
The supply of otolaryngology providers enrolled in Medicare varied to an even greater extent, ranging from .53 to 11.3/ 100,000 residents, (mean 3.04/100,000, standard deviation 1.4), geographically depicted in Figure 1. One third of HRRs had a supply of greater than 4.4 providers per 100,000 or less than 1.6 providers per 100,000, corresponding to one standard deviation around the mean. Thus the range in supply of CMS-derived otolaryngologists was wider than that derived from the AMA Masterfile. However, the two measures are not directly comparable. By design, the measure derived from the AMA included otolaryngologists who spent at least 20 hours per week in clinical practice, and excluded physicians over 65 years old in 2011. In contrast, the CMS-derived supply measure included all providers self-identifying as otolaryngologists enrolled in Medicare in 2012-3 who billed for a sufficient number of services (for privacy reasons, services must have been provided to 11 or more patients to be included). Despite different inclusion criteria, the otolaryngology supply measures were moderately correlated (.513, p=.0001) (Figure 2). Thus, regions with a high supply of otolaryngologists according to the AMA Masterfile typically had a high supply of otolaryngologists enrolled in Medicare.
Figure 1.
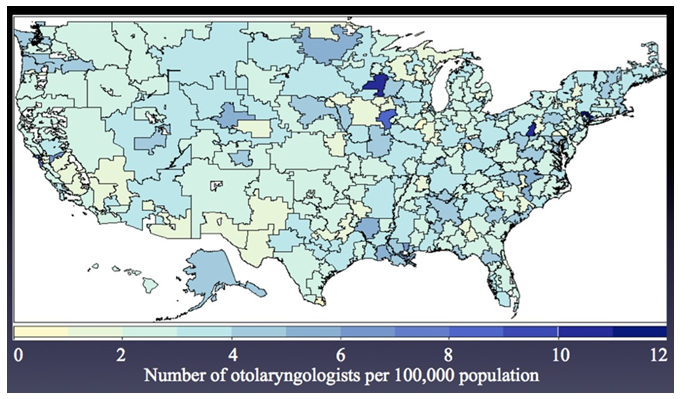
The supply of otolaryngologists enrolled in Medicare varies widely across hospital referral regions ranging from .53 to 11.3 per 100,000 (mean 3.05, standard deviation 1.4).
Figure 2.
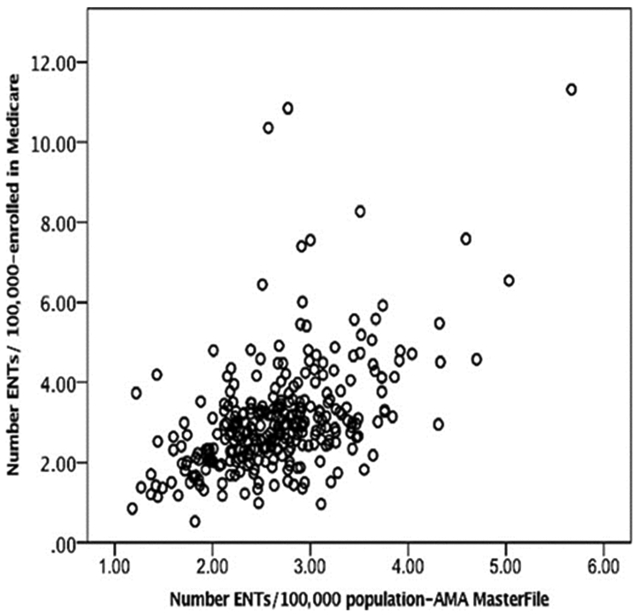
For each hospital referral region, the supply of otolaryngologists identified in the AMA-Masterfile correlated with those obtained from the CMS dataset (Pearson correlation coefficient .513, p=.0001).
Correlation of physician supply and regional hospital and population factors
Regardless of the measure used, the supply of otolaryngologists in a region increased with the mean income of the population as well as the percent of the population with at least a Bachelors degree (Table 1). Both measures of otolaryngology supply were also strongly associated with the supply of other physicians in the region. The supply of otolaryngologists was significantly associated with the supply of physicians listed in Table 1 in addition to: orthopedic surgeons, urologists, hospital based physicians, allergists, vascular surgeons, plastic and reconstructive surgeons, neurosurgeons and internal medicine physicians (data not shown). Indeed, the only physician group not associated with a high otolaryngology supply was family medicine: a high supply of family practitioners in a region was negatively associated with the supply of otolaryngologists enrolled in Medicare, and not associated with the otolaryngology supply derived from the AMA Master File (Table 1).
Table 1.
Univariable association between ENT supply and population factors, non-ENT physician supply and hospital factors
| Medicare-enrolled ENTs/HRR |
AMA Masterfile ENTs/HRR |
|||
|---|---|---|---|---|
| Population factors by HRR | r1 | p-value | r1 | p-value |
| Population Mean Income | 0.252 | p=.0001 | 0.286 | p=.0001 |
| Population Unemployment rate | −0.018 | p=.753 | −0.12 | p=.035 |
| Population Bachelors or higher | 0.276 | p=.0001 | 0.29 | p=.0001 |
| Proportion Medicaid hospitals | −0.009 | p=.877 | −0.082 | p=.153 |
| Percent Female Population | 0.051 | p=.375 | −0.047 | p=.411 |
| Percent African-American Population | 0.052 | p=.365 | 0.115 | p=.044 |
| Mean population age | 0.028 | p=.623 | 0.012 | p=.831 |
| Physician supply by HRR | ||||
| Supply physicians (all specialties) | 0.379 | p=.0001 | 0.428 | p=.0001 |
| Supply medical specialists | 0.412 | p=.0001 | 0.365 | p=.0001 |
| Supply dermatologists | 0.375 | p=.0001 | 0.389 | p=.0001 |
| Supply general surgeons | 0.184 | p=.001 | 0.368 | p=.0001 |
| Supply primary care physicians | 0.216 | p=.0001 | 0.274 | p=.0001 |
| Supply family practitioners | −0.135 | p=.018 | 0.005 | p=.934 |
| Supply of staffed acute care hospital beds by HRR | ||||
| Total acute care hospital beds | 0.206 | p=.0001 | −0.013 | p=.827 |
| Non-teaching hospital beds | −0.004 | p=.944 | −0.026 | p=.895 |
| Major teaching hospital beds | 0.338 | p=.0001 | 0.071 | p=.657 |
Pearson correlation. Abbreviations: ENT, Ear, Nose and Throat physician; HRR, hospital referral region; AMA American Medical Association
However, the two measures of otolaryngology supply strongly diverged with respect to associations with hospital-based factors. The Medicare-enrolled otolaryngology supply in a region increased with the supply of staffed acute care hospital beds and particularly the supply of hospital beds in major teaching hospitals in a region (Table 1). The presence of an otolaryngology residency-training program in a region was also associated with an increase in the supply of otolaryngology providers enrolled in Medicare. Resident physicians were not included in the otolaryngology supply calculations (Table 2).
Table 2.
Otolaryngology residency training and the regional otolaryngology supply
| Medicare-enrolled | AMA Masterfile | ||||
|---|---|---|---|---|---|
| Number residency slots in the HRR |
Number HRRs |
Mean number1 ENTs/100,000 |
(SD) | Mean number1 ENTs/100,000 |
(SD) |
| None | 228 | 2.81 | 1.3 | 2.62 | .69 |
| 1-2 | 25 | 3.26 | 1.0 | 2.56 | .44 |
| 3-4 | 39 | 3.93 | 1.5 | 2.88 | .50 |
| 5 or more | 14 | 4.19 | 1.5 | 2.81 | .57 |
| Overall | 306 | 3.05 | 1.4 | 2.66 | .65 |
| p=.0001 | p=.088 | ||||
Otolaryngology supply excludes resident physicians. Abbreviations: HRR, hospital referral region; ENT, ear nose and throat/ otolaryngologist; SD, standard deviation
Regional predictors of Medicare-enrolled otolaryngology physician supply: Multivariable analysis
In the multivariable analysis, population income was positively associated while percent African-American and Hispanic race were negatively associated with Medicare-enrolled otolaryngology supply (Table 3). Both the number of staffed acute care hospital beds and the presence of an otolaryngology residency-training program remained independent predictors of the supply of Medicare- enrolled otolaryngologists in a region. Physician and hospital-level factors were more strongly associated with the supply of otolaryngologists than population-level factors. Longer average duration since medical school graduation (a surrogate for average age of the workforce) was negatively associated with the Medicare-enrolled otolaryngology supply in the multivariable analysis (Table 3).
Table 3.
Multivariable associations: Supply of Medicare-enrolled otolaryngologists and regional population, physician and hospital factors
| Population factors/ HRR | Coefficient | (95% CI) | p-value |
|---|---|---|---|
| Median population age | −0.0122 | (−.0458-.0215) | 0.479 |
| Percent female population | −0.1824 | (−.3911-.0262) | 0.088 |
| Percent African American population | −0.0179 | (−.0351- −.0006) | 0.043 |
| Percent Hispanic population | −0.0193 | (−.0392-.0007) | 0.059 |
| Median income/ $10,000 | 0.1815 | (.0026-.3603) | 0.048 |
| Percent population with bachelors degree | 0.0016 | (−.0325-.0357) | 0.927 |
| Physician factors/HRR | |||
| ENTs: Mean years since medical school graduation1 | −0.0340 | (−.0662- −.0019) | 0.039 |
| Supply primary care physicians | −0.0148 | (−.0311-.0015) | 0.076 |
| Supply medical specialist physicians | 0.0549 | (.0326-.0773) | <.0001 |
| Supply general surgeons | 0.0794 | (−.0450-.2038) | 0.212 |
| Hospital system factors/HRR | |||
| Supply staffed acute care hospital beds | 0.7967 | (.5534-1.040) | <.0001 |
| Presence of otolaryngology residency | 0.4899 | (.1460-.8337) | 0.006 |
Mean age of otolaryngologists practicing in the HRR. Definitions: HRR, hospital referral regions, CI, confidence interval.
Discussion
Over the last two decades, there has been a steady expansion of the otolaryngology workforce4. However, concerns regarding the adequacy of the workforce have been raised in anticipation of increased demand from an aging population11. Specific increases in workload demands in head and neck surgery2 and otology 20 that largely involve the care of the elderly have also been predicted. In assessing trends, most studies have averaged the total number of otolaryngologists over large regions or the entire United States. Such approaches have the potential to obscure the pronounced geographic maldistribution of the otolaryngology workforce that may impact the delivery of care. Moreover, most studies have not considered selective participation in specific health plans which may limit the availability of some providers.
In this study, variations in the supply of otolaryngology observed across HRRs were far greater in magnitude than changes within hospital region over time. Physician supply data derived from the AMA Masterfile demonstrated that there was indeed a slight decrease in the supply of otolaryngologists per HRR between 1996 and 2011 (from 2.72 to 2.66 per 100,000 persons). However, the magnitude of this difference in otolaryngology supply was far smaller than the standard deviation of .65 of the otolaryngology supply by hospital referral region; thus the differences in otolaryngology supply among different geographic regions was greater than the change in the otolaryngology supply over a 15 year period. An analysis of CMS enrollment data suggested that the supply of Medicare-enrolled otolaryngologists varies even more.
The two measures in this study are not directly comparable. The CMS dataset was more comprehensive and included physicians 65 and older and those with limited clinical responsibilities or productivity, but excluded those with insufficient Medicare billing. The same inclusion criteria used in the AMA Masterfile could not be applied to the CMS derived database for methodological reasons, even if the raw data from the AMA Masterfile were available. Thus the Medicare participation rate among otolaryngologists could not be determined.
Based on Medicare enrollment data, it seems plausible that a substantial number of regions in the United States have an inadequate supply of otolaryngologists enrolled in Medicare. In describing the pattern of hospital utilization for head and neck cancer, Bhattacharyya and Abemayor recently described a pattern of hospital utilization for head and neck cancer which resulted in the neediest patients obtaining suboptimal care21. Our findings suggest that this pattern of utilization may reflect care delivery in underserved geographic regions.
Despite differences, the measures of otolaryngology provider supply used in this study were highly correlated. Regions with a high supply of otolaryngologists using the AMA-derived measure were also noted to have a high supply of otolaryngologists using the CMS-derived measure. Regardless of methodology, otolaryngologists preferentially practice in regions with higher population income and education levels, consistent with the observation that a community’s wealth and education increase its carrying capacity for specialist physicians18.
Otolaryngologists also preferentially serve communities with high a supply of other physicians, especially specialist physicians. Regardless of measure used, the supply of otolaryngologists was correlated with the regional supply of all physicians, and indeed every other physician group tested, except family practitioners. The tendency for physicians to aggregate has been described previously. The physician market has been described as one of symbiotic interdependence, with generalists acting as a point of entry for patients, with specialists delegated to treating more difficult cases and contributing to a greater specialty mix 17-19,22.
While the otolaryngology supply increases with regional population income and physician supply were observed for both measures, the measures diverged with respect to associations with hospital-based factors. The supply of otolaryngologists enrolled in Medicare independently increased with the number of staffed acute care hospital beds and the presence of an otolaryngology residency-training program in a region; the supply of physicians derived from the AMA Masterfile was not related to either factor. Hospital-based otolaryngologists, and those associated with an otolaryngology residency-training program are usually enrolled in Medicare while the general otolaryngology workforce may choose whether or not to enroll in the program. Consequently, the presence of hospital resources apparently increased a region’s carrying capacity for otolaryngologists enrolled in Medicare. The degree to which hospital-based otolaryngologists provide care for Medicare beneficiaries is a subject that merits further study.
Medicare enrollment is a prerequisite in caring for the elderly population. Yet Medicare reimbursement is less remunerative for physician services than most private carriers. Studies have shown that the number of specialists in a region decreases as the number of elderly individuals increases18 (although, of note, this was not observed for otolaryngology in this study). In addition, physicians have previously been shown to preferentially treat privately insured individuals over Medicare beneficiaries, increasing care to Medicare patients during times of increasing unemployment23. Medicare beneficiaries may increasingly obtain care both inpatient and outpatient care through hospital systems. Ongoing market consolidations and changes in payment model will likely alter the regional physician carrying capacities and specialist mix18 making workforce predictions subject to substantial error11.
Several limitations of this analysis should be emphasized. Comprehensive and accurate information on the otolaryngology workforce is surprisingly difficult to obtain. Lack of access to raw data within the AMA Masterfile has already been noted. In addition, the CMS database may be subject to errors specific to any large national database. We identified two otolaryngologists with more than one NPI number. We also identified at least one otolaryngology extender in the CMS database under otolaryngology providers, although the number of extenders included is difficult to discern but appears to be small. CMS and claims data is also subject to local billing practices in which services are billed under several members of the group. These limitations however serve to overestimate rather than underestimate the number of providers available to care for Medicare population. Providers of otolaryngology-type services (surgical oncologists, allergists) were not included. Misclassification of otolaryngology providers is a possibility. Future studies should involve a provider level analysis to address questions not suitable for an aggregate level study.
Conclusions
The supply of otolaryngologists varies greatly across geographic regions, diverging in important ways depending on how it is measured. The expansion of an otolaryngology workforce able to carry out high-level procedures and manage the otolaryngology-related needs of Medicare beneficiaries may depend on hospital system factors. Future studies should evaluate the role of hospital system factors in delivering otolaryngology care to the Medicare population.
Acknowledgments
Funding: Devlin Fund
Footnotes
Conflicts of interests: None
Level of Evidence: Level 2b
Triological Society Meeting, Chicago Illinois, May 20, 2016
References:
- 1.Kennedy DW. Otolaryngology workforce planning: why we cannot wait for perfect data. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2012; 147:399. [DOI] [PubMed] [Google Scholar]
- 2.Bhattacharyya N. The increasing workload in head and neck surgery: An epidemiologic analysis. The Laryngoscope 2011; 121:111–115. [DOI] [PubMed] [Google Scholar]
- 3.Pillsbury HC 3rd, Cannon CR, Sedory Holzer SE et al. The workforce in otolaryngology-head and neck surgery: moving into the next millennium. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2000; 123:341–356. [DOI] [PubMed] [Google Scholar]
- 4.Cannon CR, Giaimo EM, Lee TL, Chalian A. Special report: reassessment of the ORL-HNS workforce: perceptions and realities. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2004;131:1–15. [DOI] [PubMed] [Google Scholar]
- 5.Pillsbury HC 3rd. Analysis of the workforce and otolaryngology specialty planning. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2012; 146:340; author reply 340-341. [DOI] [PubMed] [Google Scholar]
- 6.Neuwahl S, Fraher E, Pillsbury H 3rd, Weissler MC, Ricketts T, Gaul K. Trends in the otolaryngology workforce in the U.S. Bulletin of the American College of Surgeons 2012; 97:30–34. [PubMed] [Google Scholar]
- 7.Pryor SP, Brodsky L, Chandrasekhar SS et al. Commentary on “Otolaryngology-head and neck surgery physician workforce issues an analysis for future specialty planning” by Kim, Cooper, and Kennedy. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2012; 146:203–205. [DOI] [PubMed] [Google Scholar]
- 8.Cooper RA. A call for future adequacy of the otolaryngology-head and neck surgery workforce: response to Pryor et al. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2012; 147:182; author reply 182-183. [DOI] [PubMed] [Google Scholar]
- 9.Jacoby I. Geographic distribution of physician manpower: the GMENAC (Graduate Medical Education National Advisory Committee) legacy. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association 1991; 7:427–436. [PubMed] [Google Scholar]
- 10.Williams AP, Schwartz WB, Newhouse JP, Bennett BW. How many miles to the doctor? The New England journal of medicine 1983; 309:958–963. [DOI] [PubMed] [Google Scholar]
- 11.Kim JS, Cooper RA, Kennedy DW. Otolaryngology-head and neck surgery physician work force issues: an analysis for future specialty planning. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2012; 146:196–202. [DOI] [PubMed] [Google Scholar]
- 12.Grumbach K, Becker SH, Osborn EH, Bindman AB. The challenge of defining and counting generalist physicians: an analysis of Physician Masterfile data. American journal of public health 1995; 85:1402–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper RA. Seeking a balanced physician workforce for the 21st century. JAMA : the journal of the American Medical Association 1994; 272:680–687. [PubMed] [Google Scholar]
- 14.Chang CH, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries' health outcomes. JAMA : the journal of the American Medical Association 2011; 305:2096–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirkwood MK, Bruinooge SS, Goldstein MA, Bajorin DF, Kosty MP. Enhancing the American Society of Clinical Oncology workforce information system with geographic distribution of oncologists and comparison of data sources for the number of practicing oncologists. Journal of oncology practice / American Society of Clinical Oncology 2014; 10:32–38. [DOI] [PubMed] [Google Scholar]
- 16.Goodman DC FE, Bronner KK. Hospital and Physician Capacity Update [Regional variation in hospital and physician capacity reveals the irrational distribution of valuable and expensive health care resources. Better planning of future growth in capacity can help build a more effective and affordable health care system.]. Available at: http://www.dartmouthatlas.org/downloads/reports/Capacity_Report_2009.pdf. . 2009.
- 17.Rundall TG, McClain JO. Environmental selection and physician supply. AJS; American journal of sociology 1982; 87:1090–1112. [DOI] [PubMed] [Google Scholar]
- 18.Jiang HJ, Begun JW. Dynamics of change in local physician supply: an ecological perspective. Soc Sci Med 2002; 54:1525–1541. [DOI] [PubMed] [Google Scholar]
- 19.Rundall TG. The organization of medical practice: a population ecology perspective. Medical care review 1987; 44:375–405. [DOI] [PubMed] [Google Scholar]
- 20.Lin HW, Bhattacharyya N. Otologic diagnoses in the elderly: current utilization and predicted workload increase. The Laryngoscope 2011; 121:1504–1507. [DOI] [PubMed] [Google Scholar]
- 21.Bhattacharyya N, Abemayor E. Patterns of hospital utilization for head and neck cancer care: changing demographics. JAMA otolaryngology-- head & neck surgery 2015; 141:307–312; quiz 400. [DOI] [PubMed] [Google Scholar]
- 22.Chiang TL. Deviation from the carrying capacity for physicians and growth rate of physician supply: the Taiwan case. Soc Sci Med 1995; 40:371–377. [DOI] [PubMed] [Google Scholar]
- 23.He D, McInerney M, Mellor J. Physician responses to rising local unemployment rates: Healthcare provision to Medicare and privately insured patients. Journal of health economics 2015; 40:97–108. [DOI] [PubMed] [Google Scholar]


