Abstract
Background:
Anterior cruciate ligament (ACL) reconstruction (ACLR) using bone-tendon-bone (BTB) autograft is associated with increased postoperative anterior knee pain and pain with kneeling and has the risk of intra- and postoperative patellar fracture. Additionally, graft-tunnel mismatch is problematic, often leading to inadequate osseous fixation. Given the disadvantages of BTB, an alternative is a bone-tendon autograft (BTA) procedure that has been developed at our institution. BTA is a patellar tendon autograft with the single bone plug taken from the tibia.
Purpose/Hypothesis:
The purpose of this study was to evaluate the short-term outcomes of BTA ACLR. We hypothesized that this procedure will provide noninferior failure rates and clinical outcomes when compared with a BTB autograft, as well as a lower incidence of anterior knee pain, pain with kneeling, and patellar fracture.
Methods:
A consecutive series of 52 patients treated with BTA ACLR were retrospectively identified and compared with 50 age-matched patients who underwent BTB ACLR. The primary outcome was ACL graft failure, while secondary outcomes included subjective instability, anterior knee pain, kneeling pain, and functional outcome scores (Single Assessment Numeric Evaluation, Lysholm, and International Knee Documentation Committee subjective knee form).
Results:
At a mean follow-up of 29.3 months after surgery, there were 2 reruptures in the BTA cohort (4.0%) and 2 in the BTB cohort (4.0%). In the BTA group, 18% of patients reported anterior knee pain versus 36% of the BTB group (P = .04). A total of 22% of patients noted pain or pressure with kneeling in the BTA cohort, as opposed to 48% in the BTB cohort (P = .006). There were no differences in functional scores. In the BTA group, 94.2% of patients reported that their knees subjectively felt stable, as compared with 86% in the BTB group (P = .18).
Conclusion:
This study demonstrated that the BTA ACLR leads to similarly low rates of ACL graft failure requiring revision surgery, with significantly decreased anterior knee pain and kneeling pain when compared with a BTB. Additionally, the potential complications of graft-tunnel mismatch and patellar fracture are eliminated with the BTA ACLR technique.
Keywords: ACL, reconstruction, graft, knee
Anterior cruciate ligament (ACL) reconstruction (ACLR) remains one of the most commonly performed procedures by orthopaedic surgeons. Yearly, more than 200,000 ACLRs are performed in the United States.22 While multiple graft options are available for use in ACLR, bone-tendon-bone (BTB) and hamstring tendon autografts remain the most commonly used sources. BTB autograft has historically been considered the gold standard for ACLR.6 While ACLR using BTB and hamstring tendon have shown similar clinical results, there are several reported advantages of the BTB autograft. Studies have demonstrated decreased risk of graft rupture with BTB autograft compared with hamstring autograft.5,7,21,24 Additionally, BTB autograft has been shown to result in a lower rate of infection when compared with hamstring tendon.8,11,16 Instrumented measures of knee stability also tend to show superior results with BTB autograft.2,24
While excellent results have been achieved with BTB autograft ACLR, utilization of this autograft is not without morbidity. Patients receiving BTB autograft have significantly more postoperative and long-term anterior knee pain when compared with patients who receive a hamstring autograft.10,18 Pain reported with kneeling is also significantly higher after BTB autograft, with approximately half of patients expressing this complaint in multiple studies.10,12 Additionally, BTB graft harvest involves the risk of intra- and postoperative patellar fracture, at a rate of 0.2% to 1.3%, according to the literature.1,13,22,23
An unfortunate and common challenge for the ACL surgeon, when using endoscopic femoral tunnel techniques, is graft-tunnel mismatch. Graft-tunnel mismatch is problematic and often results in a bone plug recession or protrusion from the tibial tunnel, leading to inadequate graft fixation distally. Previous studies have focused on avoiding graft-tunnel mismatch through preoperative planning.3,4,14,17 However, to date, there is no ideal solution with regard to addressing graft-tunnel mismatch that occurs intraoperatively.
Given the disadvantages of the BTB autograft, an alternative may be ACLR based on a bone-tendon autograft (BTA) procedure, which has been developed at our institution. This technique utilizes an autograft composed of the central third of the patellar tendon and a tibial tubercle bone plug without inclusion of the patellar bone plug. This graft has been hypothesized to decrease kneeling pain as well as anterior knee pain. Additionally, it theoretically eliminates the complication of patellar fracture. Last, the BTA technique provides a versatile option by allowing an intraoperative decision based on patellar tendon length and total construct length. During graft harvest, if the surgeon encounters a construct that will lead to graft-tunnel mismatch, the BTA allows the surgeon to easily proceed with a BTA without the need for different instrumentation. Furthermore, the BTA graft has the benefits of the osseous component of the tibial bone plug without the associated morbidity of the patellar bone plug.
The purpose of our study was to compare the results of the BTA and BTB autografts used for ACLR. We hypothesized that ACLR with a BTA will provide noninferior failure rates and clinical results, as well as lower incidences of anterior knee pain and pain with kneeling when compared with BTB autograft. Additionally, we hypothesized that the BTA eliminates the risk of graft-tunnel mismatch and patellar fracture.
Methods
A consecutive series of 52 patients treated with BTA ACLR between June 2016 and April 2018 were retrospectively identified. Additionally, an age-matched cohort of patients who had undergone BTB autograft ACLR during the same time frame were identified. All patients were evaluated at a single military medical facility. The majority of patients in both cohorts were active duty military, who are required to perform high levels of physical activity. Preoperatively, patients who had clinical and magnetic resonance imaging–based evidence of a ruptured ACL were counseled on the benefits and risks of ACLR. For those patients who elected ACLR, graft choice was based on surgeon and patient preference. All BTA ACLRs were performed at a single institution by the senior author (C.R.B.), who is board certified and fellowship trained in sports medicine. The BTB ACLRs were performed at the same institution by 3 board-certified and sports medicine–trained orthopaedic surgeons (B.J.M., K.S.M., and C.R.B.). Medical records were reviewed and telephone inquiries performed to obtain study data. All participants provided informed consent, and an institutional review board determined the study to be exempt before the initiation of data collection. Exclusion criteria included alternate graft choice, revision ACLR, multiligamentous knee injuries, anterior knee pain before the injury, and lack of 2-year follow-up at the time of data collection.
Surgical Procedure
Bone-Tendon Autograft
All patients underwent an examination under anesthesia to confirm pathologic laxity of the ACL. An arthroscopic examination before graft harvest was performed to confirm an ACL rupture. In the BTA cohort, the central third of the patellar tendon was harvested with a trapezoidal 20- to 25-mm tibial tubercle bone plug. If the tendon was >45 mm and the total construct at least 70 mm, then the BTA technique proceeded. At the inferior pole of the patella, electrocautery was used to harvest the tendon from the patella (Figures 1 and 2). The tibial bone plug was typically sized to a 9 on a standard graft-measuring device, and the free tendinous end was secured with a locking-loop suture (Figure 3). Arthroscopically, a thorough fat pad resection was performed with a minimal notchplasty if indicated. The tibial footprint of the native ACL was used for accurate placement of the tibial tunnel. The tibial tunnel location was established with a standard tibial guide (AR-1510 T; Arthrex), which was typically set between 55° and 60° and was created after guide pin placement. For femoral tunnel placement, the knee was hyperflexed, and a Beath pin was inserted through the medial portal to the start point of the femoral tunnel. The pin was then advanced through the femoral condyle and out of the lateral thigh skin. Once appropriate pin placement was confirmed, an acorn reamer was used to drill the femoral tunnel to 25 to 30 mm in depth, and a tunnel notcher was used to create a notch on the anterior aspect of the tunnel. The femoral tunnel was drilled to the same size as the bone block. The tibial tunnel was therefore then drilled to the same size to facilitate bone block passage. The tibial bone plug portion of the graft was passed into the femoral tunnel with the soft tissue component fixed in the tibial tunnel. Femoral fixation was then achieved with a 7 × 20–mm BioComposite or metal interference screw (FastThread; Arthrex). Tibial fixation was obtained via a BioComposite screw (RetroScrew; Arthrex) inserted into the tunnel antegrade from within the joint (Figure 4). The diameter of the screw was generally 1 mm smaller than the tibial tunnel. It is standard at our institution to obtain secondary tibial fixation. The sutures of the graft were secured using a SwiveLock C (4.75 × 19.1 mm, BioComposite; Arthrex), which was then inserted into the tibia just distal to the tibial tunnel.
Figure 1.

The paratenon is split and carefully reflected off the underlying tendon. The middle third of the patellar tendon is used with a typical width of 10 to 11 mm. A full-thickness longitudinal incision of the patellar tendon is made from the inferior pole of the patella to the tibial tubercle.
Figure 2.

At the inferior pole of the patella, electrocautery is used to harvest the tendon. Typically, an additional 5 to 10 mm of tendon can be obtained from the inferior pole.
Figure 3.
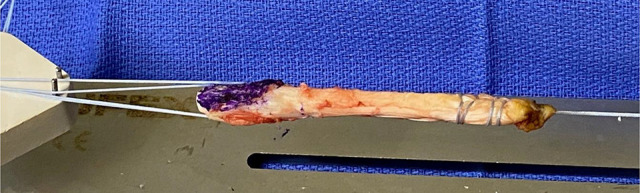
A standard BTA graft. The tendinous end of the BTA graft is prepared with a locking-loop suture passed through the tendon. The bone plug is secured by passing a suture through two 2.0-mm drill holes. The cancellous portion of the bone plug is colored purple, and the graft is placed on 15 to 20 lb (7-9 kg) of tension. BTA, bone-tendon autograft.
Figure 4.

While tension is maintained on the graft and a large curette is used to provide downward pressure, a RetroScrew is secured into the tibia, obtaining interference fixation against the tendinous portion of the graft.
BTB Autograft
The BTB reconstruction was completed in accordance with surgeon preference through previously described techniques.13 The patellar bone plug harvest site was bone grafted in all cases with cancellous bone trimmed from the tibial and patellar bone plugs. There were 2 instances of graft-tunnel mismatch, for which the tibial tunnel was redrilled to increase the length of the tunnel.
Postoperative Management
Postoperatively, both cohorts followed the same rehabilitation protocol. Patients were immediately permitted to be weightbearing as tolerated with a hinged knee brace locked in extension for the first 2 weeks. When not weightbearing, the patients were permitted knee range of motion as tolerated if no concomitant procedures, such as meniscal repair, were performed. If a meniscal repair had been performed, patients were nonweightbearing, and range of motion was restricted to 90° of flexion for 6 weeks postoperatively. In nonmeniscal repair, for the next 4 weeks, patients continued to wear the hinged knee brace; however, they were allowed to have unlocked range of motion with the use of a crutch for ambulation. All patients followed a standardized ACLR rehabilitation protocol supervised by a physical therapist. Full active motion was encouraged in all cases. The hinged knee brace was typically discontinued at 4 weeks postoperatively. Patients were allowed to return to sport or military activity when cleared by the physical therapist, at a minimum of 8 months postoperatively.
Evaluation at Latest Follow-up
All study patients were contacted by telephone to complete a survey to ascertain if they had sustained an ACL graft rupture requiring revision surgery or if they had clinically significant instability. Telephone surveys were performed by a single investigator (D.G.) from a separate institution who was blinded as to which patients had received which graft type. A Single Assessment Numeric Evaluation (SANE) score was also obtained. Additionally, patients were asked if they had anterior knee pain, and they were separately asked if they had kneeling pain; in each case, those with pain rated it on a scale of 0 to 10 (10 being worst). Two online questionnaires were administered via email to assess functional outcomes: the Lysholm knee scoring scale and the International Knee Documentation Committee (IKDC) subjective knee form. Postoperative complications were assessed via chart review and telephone questionnaire.
Statistical Analysis
Based on the historical data, a power analysis was conducted with kneeling pain as the variable of interest. This variable was chosen because it was thought to be the most likely to differ postoperatively between the study groups. Based on an effect size of 0.5 and an alpha value of .8, a minimum of 48 patients per study group (96 total) was required to achieve a power of 0.9. Descriptive statistics were performed for ACL graft failures, outcome scores (Lysholm, IKDC, and SANE), postoperative anterior knee pain and kneeling pain, and patient satisfaction. The primary outcome was ACL graft failure requiring revision surgery. Secondary outcomes were anterior knee pain, kneeling knee pain, and patient-reported functional scores. Statistical analysis was performed using Microsoft Excel. Unpaired t tests were performed to compare SANE, Lysholm, and IKDC scores. Chi-square tests were performed to determine if differences in categorical variables were present between the BTA and BTB cohorts. Significance was assumed for P values <.05.
Results
There were 52 patients in the BTA group and 50 in the BTB group who underwent ACLR between June 2016 and April 2018. The mean age of all patients included in the study was 26.1 years. There were no significant differences in sex, age, or number of active duty patients between the groups (Table 1). There were also no differences between the groups regarding medial meniscal tears, lateral meniscal tears, tears requiring repair, medial femoral condyle chondromalacia, lateral femoral condyle chondromalacia, and, importantly, patellofemoral chondromalacia (Table 2).
TABLE 1.
Patient Demographics Between Study Groupsa
| BTA Group (n = 52) | BTB Group (n = 50) | P Value | |
|---|---|---|---|
| Sex | |||
| Male | 41 | 35 | .84 |
| Female | 11 | 15 | |
| Age, y | 27.0 ± 6.0 | 25.3 ± 7.1 | .29 |
| Active duty | 42 | 40 | .53 |
aData are reported as No. or mean ± SD. BTA, bone-tendon autograft; BTB, bone-tendon-bone.
TABLE 2.
Concomitant Intra-articular Pathology Between Groupsa
| BTA Group | BTB Group | P Value | |
|---|---|---|---|
| Tear | |||
| MM | 3 | 6 | .29 |
| LM | 26 | 18 | .11 |
| MM + LM | 11 | 6 | .18 |
| Meniscal repair | 7 | 11 | .30 |
| Chondromalaciab | |||
| PF | 3 | 6 | .29 |
| MFC | 5 | 5 | ≥.99 |
| LFC | 1 | 3 | .31 |
aData are reported as No. of patients. BTA, bone-tendon autograft; BTB, bone-tendon-bone; LFC, lateral femoral condyle; LM, lateral meniscus; MFC, medial femoral condyle; MM, medial meniscus; PF, patellofemoral.
bChondromalacia was diagnosed and graded intraoperatively.
At a mean 2.4 years after surgery (29.3 and 30.1 months in the BTA and BTB cohorts, respectively), there were 2 reruptures in the BTA cohort (4.0%) and 2 in the BTB autograft cohort (4.0%) (P ≥ .99). In the BTA cohort, 9 (18%) patients reported anterior knee pain, as opposed to 18 (36%) in the BTB cohort (P = .04). In the BTA cohort, 11 (22%) patients cited pain or pressure with kneeling, compared with 24 (48%) patients in the BTB cohort (P = .006) (Figure 5). Of the patients who noted anterior knee pain, the mean pain score was 3.6 in the BTA cohort and 4.7 in the BTB cohort (P = .04).
Figure 5.
Comparison of anterior knee pain and kneeling pain between bone-tendon autograft (BTA) and bone-tendon-bone (BTB) autograft. A significantly higher percentage of BTB patients reported anterior knee pain (P = .04) and kneeling pain (P = .006) compared with BTA patients. Error bars represent SE.
In the BTA cohort, 94.2% of patients reported that the knee felt subjectively stable, as compared with 86% in the BTB cohort (P = .18). There was no significant difference in postoperative SANE, Lysholm, or IKDC scores between the groups (Table 3).
TABLE 3.
Postoperative Patient-Reported Outcomes Comparing BTA and BTBa
| BTA Group | BTB Group | P Value | |
|---|---|---|---|
| SANE | 84.37 ± 17.2 | 81.40 ± 11.6 | .35 |
| Lysholm | 84.83 ± 17.7 | 80.36 ± 16.4 | .11 |
| IKDC | 80.99 ± 18.4 | 76.89 ± 15.7 | .14 |
aData are reported as mean ± SD. BTA, bone-tendon autograft; BTB, bone-tendon-bone; IKDC, International Knee Documentation Committee; SANE, Single Assessment Numeric Evaluation.
There was 1 patellar fracture in the BTB cohort, which occurred 3 months postoperatively and required open reduction internal fixation. There were no complications outside of graft failure in the BTA cohort.
Discussion
The principal findings of this study were that, similar to BTB, the BTA ACLR led to low rates of ACL graft failure requiring revision surgery; however, the BTA procedure resulted in significantly decreased anterior knee pain as well as significantly decreased kneeling pain as compared with the BTB autograft. Additionally, BTA ACLR resulted in excellent postoperative functional scores, similar to those of BTB. Last, in the BTA cohort, there were no cases of patellar fracture or complications other than rerupture.
Numerous studies have examined the long- and short-term outcomes of ACLR after soft tissue and bony graft reconstruction. Persson et al19 performed a cohort study of 12,643 patients who underwent patellar tendon and hamstring autografts and found an overall revision rate of 4.2% at 5 years. A case-control study by Hettrich et al9 of 980 prospectively evaluated patients demonstrated a 7.7% revision rate. Furthermore, Samuelsen et al21 reported a 2.8% rerupture rate at a mean follow-up of 68 months after BTB autograft ACLR in a meta-analysis of 47,613 patients. In a study evaluating ACLR survivability in an active duty military population, the authors found an 11% failure rate of BTB autografts at 1.5 years from the index procedure.18 Therefore, our BTA technique has resulted in noninferior rates of rerupture as compared with short- and long-term data on ACLR. Given that the number of patients in our study who met adequate follow-up was relatively small, we will continue to collect longer term data on our increasing patient population.
The BTB autograft is a reliable graft option for ACLR with low rates of rerupture and potentially earlier return to sport, and it is associated with a lower incidence of infection as compared with hamstring autograft. However, as previously mentioned, BTB autograft ACLR is not without morbidity. Lund et al15 reported a rate of 34% for anterior kneeling pain after ACL BTB reconstruction. The results of our study similarly demonstrated a 48% rate for anterior kneeling pain after a BTB autograft. Supporting our hypothesis, the BTA cohort showed a statistically significantly lower rate of anterior kneeling pain (22%) as compared with the BTB autograft cohort (48%). Although BTA ACLR did not completely eliminate anterior knee or kneeling pain, the BTA cohort’s rate of anterior knee pain was significantly lower, not only compared with our BTB autograft cohort, but also compared with previously published BTB data from larger studies.12,15
Graft-tunnel mismatch is a common technical complication for the ACL surgeon, often resulting in plug recession or protrusion from the tibial tunnel and leading to inadequate osseous fixation. Prior authors have attempted to provide solutions for decreasing the risk of graft-tunnel mismatch.3,4,17 One option includes increasing the length of the tibial tunnel by adjusting the angle at which the tunnel is drilled. However, this may lead to decreased graft obliquity and potential alterations in the biomechanical properties of the graft. The BTA ACLR provides a versatile alternative, which allows the ACL surgeon to make an intraoperative decision whether to proceed with a BTA or a BTB autograft reconstruction based on construct length, without the need for significant changes in instrumentation. There was a 4% incidence of graft-tunnel mismatch in this study. In all cases, the surgeon was able to correct the graft-tunnel mismatch by decreasing the size of the bone plug. The potential complication of graft-tunnel mismatch is therefore eliminated with the BTA ACLR. Last, this study proves that single bone plug fixation provides adequate fixation, with noninferior failure rates at short-term follow-up. Thus, if a surgeon encounters graft-tunnel mismatch, the BTB can be converted to a BTA without consequence.
An additional source of morbidity with BTB ACLR is the risk of patellar fracture. In the BTB cohort, there was 1 patellar fracture that required open reduction internal fixation. The fracture was atraumatic and occurred during a hike 3 months postoperatively. Stein et al23 reported a 1.3% incidence of patellar fracture after BTB ACLR. Of the 52 patients who underwent BTA ACLR in our study, there were no cases of patellar fracture.
Last, there are few weaknesses to the BTA graft. In our opinion, the only identifiable weakness is the lack of bone-on-bone healing provided by the patellar bone plug. However, soft tissue ACLR grafts have provided excellent long-term outcomes.2,7,20 Therefore, we believe the benefits of significantly decreased anterior knee pain and kneeling pain and the elimination of graft-tunnel mismatch and patellar fracture outweigh this weakness. Anatomic studies have demonstrated that quadriceps tendon autograft is longer, thicker, and wider and has greater strength than patellar tendon autografts.8 As such, further studies are necessary to evaluate the BTA ACLR as compared with quadriceps and hamstring tendon autografts.
Limitations
This study was retrospective in nature and therefore subject to recall bias. All patients who underwent a BTA ACLR had their surgery performed by a single surgeon, whereas the BTB ACLR procedures were performed by 3 surgeons. Additionally, this was a relatively small cohort with a short-term follow-up; longer-term data on the BTA ACLR will continue to be published. In this study, instability was assessed subjectively via telephone interview, which is less valuable than objective measurement, including Lachman test and KT-2000 arthrometer evaluation. Thus, some failures (ie, laxity >5 mm) may not have been detected. We did not control for patient position within the military; therefore, there could be a difference in activity level between the cohorts. Last, we did not report on postoperative imaging to evaluate for patellar cartilage wear.
Conclusion
Our study demonstrated that ACLR with BTA results in equally low rates of rerupture requiring revision reconstruction as compared with the gold standard BTB autograft. Additionally, we found significantly decreased anterior knee pain and kneeling pain with the BTA ACLR. Both cohorts had excellent postoperative patient-reported outcomes, with no significant differences between them. Possibly most important, the rare but challenging complication of graft-tunnel mismatch and patellar fracture was eliminated with the BTA ACLR technique.
Footnotes
Final revision submitted July 28, 2020; accepted August 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.S.M. has received grant support from Arthrex and Zimmer Biomet and education payments from Smith & Nephew. C.R.B. has received education payments, consulting fees, and nonconsulting fees from Arthrex and honoraria from the Musculoskeletal Transplant Foundation. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Walter Reed National Military Medical Center (No. WRNMMC-EDO-2020-0456, 918208).
References
- 1. Almazán A, Miguel A, Odor A, Ibarra JC. Intraoperative incidents and complications in primary arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(11):1211–1217. [DOI] [PubMed] [Google Scholar]
- 2. Biau DJ, Katsahian S, Kartus J, et al. Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. Am J Sports Med. 2009;37(12):2470–2478. [DOI] [PubMed] [Google Scholar]
- 3. Brown JA, Brophy FH, Fanco J. Avoiding allograft length mismatch during anterior cruciate ligament reconstruction: patient height as an indicator of appropriate graft length. Am J Sports Med. 2007;35:986–989. [DOI] [PubMed] [Google Scholar]
- 4. Fowler BL, Distefano VJ. Tibial tunnel bone grafting: a new technique for dealing with graft-tunnel mismatch in endoscopic anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:224–228. [DOI] [PubMed] [Google Scholar]
- 5. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. [DOI] [PubMed] [Google Scholar]
- 6. Fu FH, Schulte KR. Anterior cruciate ligament surgery 1996: state of the art? Clin Orthop Relat Res. 1996;325:19–24. [DOI] [PubMed] [Google Scholar]
- 7. Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42(10):2319–2328. [DOI] [PubMed] [Google Scholar]
- 8. Harris NL, Smith DA, Lamoreaux L, Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction, part I: morphometric and biomechanical evaluation. Am J Sports Med. 1997;25(1):23–28. [DOI] [PubMed] [Google Scholar]
- 9. Hettrich CM, Dunn WR, Reinke EK; MOON Group, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41(7):1534-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Järvelä T, Kannus P, Järvinen M. Anterior knee pain 7 years after an anterior cruciate ligament reconstruction with a bone–patellar tendon–bone autograft. Scand J Med Sci Sports. 2000;10(4):221–227. [DOI] [PubMed] [Google Scholar]
- 11. Judd D, Bottoni C, Kim D, Burke M, Hooker S. Infections following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(4):375–384. [DOI] [PubMed] [Google Scholar]
- 12. Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971–980. [DOI] [PubMed] [Google Scholar]
- 13. Lee GH, McCulloch P, Cole BJ, Bush-Joseph CA, Bach BR. The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):162–166. [DOI] [PubMed] [Google Scholar]
- 14. Lubowitz JH. Anteromedial portal technique for the anterior cruciate ligament femoral socket: pitfalls and solutions. Arthroscopy. 2009;25:95–101. [DOI] [PubMed] [Google Scholar]
- 15. Lund B, Nielsen T, Faunø P, Christiansen SE, Lind M. Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy. 2014;30(5):593-598. [DOI] [PubMed] [Google Scholar]
- 16. Maletis GB, Inacio MC, Reynolds S, Desmond JL, Maletis MM, Funahashi TT. Incidence of postoperative anterior cruciate ligament reconstruction infections: graft choice makes a difference. Am J Sports Med. 2013;41(8):1780–1785. [DOI] [PubMed] [Google Scholar]
- 17. McAllister DR, Bergfeld JA, Parker RD, Groof PN, Valdevit AD. A comparison of preoperative imaging techniques for predicting patellar tendon graft length before cruciate ligament reconstruction. Am J Sports Med. 2001;29:461–465. [DOI] [PubMed] [Google Scholar]
- 18. Pallis M, Svodboda SJ, Cameron KL, Owens BD. Survival comparison of allograft and autograft anterior cruciate ligament reconstruction at the United States Military Academy. Am J Sports Med. 2012;40(6):1242–1246. [DOI] [PubMed] [Google Scholar]
- 19. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42(2):285–291. [DOI] [PubMed] [Google Scholar]
- 20. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. [DOI] [PubMed] [Google Scholar]
- 21. Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shelton WR, Fagan BC. Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2011;19(5):259–264. [DOI] [PubMed] [Google Scholar]
- 23. Stein DA, Hunt SA, Rosen JE, Sherman OH. The incidence and outcome of patella fractures after anterior cruciate ligament reconstruction. Arthroscopy. 2002;18(6):578–583. [DOI] [PubMed] [Google Scholar]
- 24. Viola R, Vianello R. Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone–patellar tendon–bone autograft. Arthroscopy. 1999;15(1):93–97. [DOI] [PubMed] [Google Scholar]



