Abstract
The term “Primary age-related tauopathy” (PART) was coined in 2014 to describe the common neuropathological observation of neurofibrillary tangles without associated beta-amyloid (Aβ) pathology. It is possible for PART pathology to be present in both cognitively normal and cognitively impaired individuals. Genetically, Apolipoprotein E (APOE) ε4 has been shown to occur less commonly in PART than in Alzheimer’s disease (AD). Here, we investigate the relationships between PART, AD and those pathologically normal for age, with an emphasis on APOE and cognition, using 152 selected participants from The University of Manchester Longitudinal Study of Cognition in Normal Healthy Old Age and the Manchester arm of the Brains for Dementia Research cohort. APOE genotype differed between PART and AD with APOE ε2 more common in the former and APOE ε4 more common in the latter. Individuals with definite PART were less likely to be cognitively impaired than those with AD and those with pathology considered pathologically normal for age. We postulate that the lack of Aβ in definite PART cases may be due either to an increased frequency of APOE ε2 or decreased frequency of APOE ε4 as their resulting protein isoforms have differing binding properties in relation to Aβ. Similarly, an increased frequency of APOE ε2 or decreased frequency of APOE ε4 may lead to decreased levels of cognitive impairment, which raises questions regarding the impact of Aβ pathology on overall cognition in elderly subjects. We suggest that it may be possible to use the increased frequency of APOE ε2 in definite PART to assist neuropathological diagnosis.
Keywords: Primary age-related tauopathy, Alzheimer’s disease, APOE, Cognition
Introduction
For many years, neuropathologists have observed neurofibrillary tangles (NFTs) without associated beta-amyloid (Aβ) pathology in the brains of aged individuals both with and without cognitive impairment. NFTs are almost ubiquitous in the brains of older people [22]. Significant tau burden (Braak tau stage III-IV) but few Aβ plaques have been observed in 2–10% of individuals in community-based settings [15, 21, 29]. The inability to assign a diagnosis of Alzheimer’s disease (AD) to cognitively impaired individuals with these findings led to terms such as “senile dementia with tangles” or “tangle-only dementia” [11]. In those cognitively intact, “age-related changes” were often cited. To address this phenomenon, the term “primary age-related tauopathy” (PART) was suggested and consensus guidelines on diagnosis were proposed [6].
PART has been shown to be equally as common in males and females [8]. Although cognitive impairment can be present or absent in PART, the age group primarily affected (over 75 years) commonly report subjective memory issues. However, these memory complaints generally do not progress to dementia in those with a post-mortem diagnosis of PART [16].
PART is primarily diagnosed post-mortem. Macroscopically, no significant brain abnormalities are usually present although widespread cerebral atrophy has been documented in some cognitively impaired cases [1]. Microscopically, NFTs are found in similar regions to those affected by AD but with the notable exception of the neocortex. Thus, those with PART are generally considered Braak tau stage III or lower. For PART diagnosis, Aβ load should be minimal (or absent). A maximum Thal phase of 2 is required. Stratification into ‘possible PART’ and ‘definite PART’ is based on the level of Aβ burden (Table 1). Secondary pathologies have been noted in PART including cerebrovascular pathology [12], argyrophilic grains, hippocampal sclerosis, and TAR DNA-binding protein 43 (TDP-43) [13, 37]. Other secondary findings in PART, such as cerebral amyloid angiopathy (CAA) [12] and Lewy bodies [13] are less common. The presence of co-existing pathologies are unsurprising as mixed brain pathologies are often found in aged individuals [14].
Table 1.
Inclusion criteria for the four groups used in the present study
| Study group | Characteristics for inclusion |
|---|---|
| Normal pathology for age | Braak stage 0 |
| Thal phase 0–1 | |
| No other significant pathological changes | |
| AD pathological changes | Braak stage III or higher |
| Thal phase 3 or higher | |
| No other significant pathological changes | |
| Possible PART | Braak stage III or lower |
| Thal phase 1–2 | |
| No other disease associated with NFTs present | |
| Definite PART | Braak stage III or lower |
| Thal phase 0 | |
| No other disease associated with NFTs present |
It is well known that apolipoprotein E (APOE) ε4 carriers are at a greater risk of AD [32] whereas APOE ε2 carriers are thought to be at lower risk of AD [27] but at a greater risk of CAA–related haemorrhage [18]. Previous studies have shown that APOE ε4 is less frequently found in PART when compared to AD [2, 3, 6, 36]. Conversely, APOE ε2 has been shown to be more common in PART when compared to AD [3, 6]. Other studies have shown that microtubule associated protein tau (MAPT) H1/H1 haplotype is more commonly found in PART than in AD [28].
Here, using selected participants from The University of Manchester Longitudinal Study of Cognition in Normal Healthy Old Age (UMLCHA) and the Manchester arm of the Brains for Dementia Research (BDR) cohort, we investigate the relationships between PART, AD and those pathologically normal for age, with an emphasis on APOE and cognition. We demonstrate that APOE genotype differs between PART and AD with APOE ε2 more common in the former and APOE ε4 more common in the latter. Furthermore, we show that individuals with definite PART were less likely to be cognitively impaired than those with AD and those with pathology considered pathologically normal for age implying that Aβ load may impact on cognitive outcome.
Materials and methods
Participants and study design
The present study uses selected participants from UMLCHA and the Manchester arm of the BDR cohort. Clinical and neuropathological characteristics of these cohorts have been previously described [24–26].
As the present study aims to assess relationships between AD, PART and those considered pathologically normal for age, there was a need to exclude a number of participants from each cohort (BDR 84 excluded; UMLCHA 54 excluded). The following exclusion criteria were applied to ensure suitability:
Participants with primary neuropathological diagnosis other than AD, PART or pathologically normal for age
Participants with significant confounding pathology (such as Lewy bodies). Note that cases with CAA were included in the analyses.
Participants with no available APOE genotype
Participants with a high probability of cognitive impairment due to vascular pathology (as measured by vascular cognitive impairment neuropathology guidelines [31]).
After applying the exclusion criteria, 152 participants (72 BDR and 80 UMLCHA) were considered eligible for the present study (Additional file 1: Table 1).
Clinical assessment
The two cohorts conducted different assessment schedules to assign cognitive status. UMLCHA used the modified Telephone Instrument for Cognitive Status (TICSm) score with a cut-off point of 21 and BDR used the Clinical Dementia Rating (CDR) with a cut-off point of 0.5. Scores for TICSm and CDR have been shown to be highly correlated [30]. For the present study, we also used patient notes obtained via the participants’ general practitioner, cause of death (on death certification) and information gained from Brain Bank Coordinator (PT) to ensure the assignment of cognitive status at death was as accurate as possible.
Pathological methods
The pathological methods associated with these cohorts have been previously described in detail [25, 26].
In short, donated brains were cut down the mid-line to result in two hemispheres. One hemisphere (usually the left) was fixed in 10% neutral buffered formalin for at least three weeks. The other hemisphere was frozen at −80 °C.
Standard blocks were dissected from fixed tissue (as according to BDR protocols) and processed into paraffin wax blocks. One paraffin section (6 µm) was cut from each block and stained with haematoxylin and eosin. Further paraffin sections (6 µm) were cut and used in immunohistochemistry for Aβ (Cambridge Bioscience, clone 4G8, 1:3000), tau proteins phosphorylated at Ser202 and Thr205 (Innogenetics, monocolonal AT8, 1:750), phosphorylated α-synuclein (polyclonal antibody (#1175), 1:1000 [23]), phosphorylated and non-phosphorylated TDP-43 (Proteintech, polyclonal antibody, 1:1000) and p62 (BD Transduction Labs, monoclonal, 1:100). For antigen retrieval, sections were either immersed in 70% formic acid for 20 min (for Aβ only) or microwaved in 0.1 M citrate buffer, pH 6.0 (all other antibodies) prior to incubation with primary antibody.
Consensus criteria were used to ascertain presence and stage of neurodegenerative disease. Final neuropathological diagnoses were assigned by experienced neuropathologists (DM & FR).
Study group assignment
Criteria for inclusion into the four study groups included in this study can be found in Table 1.
Genetic analysis
DNA was extracted from frozen brain tissue using REDExtract-N-Amp™ Tissue PCR Kit (Sigma) or from blood (3 cases). The APOE genotype was determined using routine polymerase chain reaction methods [34].
Statistical analyses
Chi squared test was used to analyse whether there were differences in sex, severity of CAA, frequency of APOE ε4 allele(s) and frequency of APOE ε2 allele(s) between allocated pathology groups. Fisher’s Exact test was used when the expected count was less than five. T test assessed differences in age at death.
Logistic regression was used to investigate whether adjustment for sex and age at death made any difference to significant outcomes when analysing presence of APOE ε4 allele(s) and presence of APOE ε2 allele(s) between allocated pathology groups.
A p value of < 0.05 was considered significant.
Results
Demographics
Demographic information, stratified by pathology group, can be found in Table 2. Overall, 61.2% of participants were female. 50% of all participants were cognitively impaired. Mean age at death was 84.4 (± 9.2) years.
Table 2.
Demography of eligible cases stratified by pathology group
| Normal for age | AD pathological changes | Possible PART | Definite PART | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Sex (female) | 9 | 60.0 | 49 | 59.0 | 23 | 79.3 | 12 | 48.0 |
| Cognitive impairment at death | 4 | 26.7 | 66 | 79.5 | 6 | 20.7 | 0 | 0 |
| Age at death (Mean ± s.d) | 79.7 (± 14.1) | 83.0 (± 9.2) | 88.3 (± 6.1) | 87.1 (± 6.4) | ||||
There was a significantly greater proportion of females in the possible PART group compared with the AD pathological changes group (χ2 = 3.848; p = 0.050) and the definite PART group (χ2 = 5.771; p = 0.016). As expected, there was a significantly greater proportion of cognitively impaired individuals in the AD pathological changes group when compared with the pathologically normal for age group (χ2 = 17.388; p < 0.001), the possible PART group (χ2 = 32.395; p < 0.001) and the definite PART group (χ2 = 51.119; p < 0.001). Likewise, there were significantly more cognitively impaired individuals in the possible PART group when compared with the definite PART group (χ2 = 5.819; p = 0.016). There were also significantly more cognitively impaired participants in the pathologically normal for age group when compared with the definite PART group (χ2 = 7.407; p = 0.006).
Mean age at death was significantly higher in the possible PART group compared with the pathologically normal for age group (p = 0.037) and the AD pathological changes group (p = 0.001). Similarly, mean age at death was significantly higher in the definite PART group compared with the AD pathological changes group (p = 0.015).
CAA
In the AD pathological changes group, 45.8% of individuals had moderate to severe CAA pathology. In the PART pathology groups, moderate to severe CAA was much less prevalent (possible PART 20.7%; Definite PART 4%) and was completely absent from those considered pathologically normal for age. Proportionally, moderate to severe CAA was significantly more likely in with AD pathological changes than those with possible PART (χ2 = 5.674; p = 0.017) or definite PART (χ2 = 14.539; p < 0.001). There were no differences in severity of CAA between possible and definite PART groups (χ2 = 3.315; p = 0.069).
APOE genotype
Breakdown of APOE genotype can be found in Fig. 1.
Fig. 1.
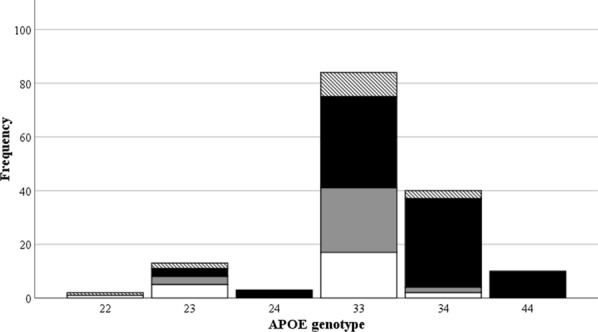
Breakdown of APOE genotype, stratified by pathology group (Hatched = Normal for age; Black = AD pathological changes; Grey = Possible PART; White = Definite PART)
As expected, APOE 3,3 was the most common genotype (55.3%). When stratifying by group, APOE 3,3 was the most common genotype in the pathologically normal for age (60.0%), possible PART (82.8%) and definite PART (68.0%) groups. All cases of APOE 4,4 were found in the AD pathological changes group. In addition, 39.8% of cases in the AD pathological changes group were APOE 3,4. The genotype APOE 2,4 was only present in the AD pathological changes group.
Allele frequency of APOE ε4/APOE ε2, stratified by pathology group, can be found in Fig. 2.
Fig. 2.
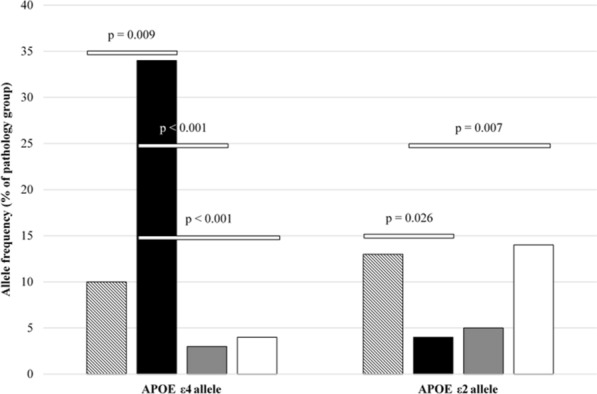
Allele frequency of APOE ε4/APOE ε2, stratified by pathology group (Hatched = Normal for age; Black = AD pathological changes; Grey = Possible PART; White = Definite PART)
The APOE ε4 allele appeared more frequently in the AD pathology group when compared with those pathologically normal for age (χ2 = 6.803; p = 0.009), those with possible PART (χ2 = 20.547; p < 0.001) and those with definite PART (χ2 = 17.297; p < 0.001).
APOE ε2 allele was found more frequently in the pathologically normal for age group when compared with the AD pathology group (χ2 = 4.957; p = 0.026). Likewise, APOE ε2 allele was more frequent in the definite PART group when compared with the AD pathology group (χ2 = 7.327; p = 0.007).
Regression analysis showed that sex and age at death had no effect on the outcome of significant results found for presence of APOE ε4 when comparing AD pathology group with pathologically normal for age group (OR = 5.928; p = 0.011), possible PART group (OR = 0.071; p = 0.001) and definite PART group (OR = 0.081; p = 0.001). Likewise, controlling for sex and age at death had no effect on the significant outcome found for presence of APOE ε2 when comparing definite PART group and AD pathology group (OR = 4.196; p = 0.032). However, sex and age at death affected the significant outcome found for presence of APOE ε2 when comparing pathologically normal for age group and AD pathology group (OR = 0.304; p = 0.113).
When considering CAA, the APOE ε4 allele was found more frequently in those individuals with moderate to severe CAA (χ2 = 17.778; p < 0.001) than none to mild CAA. There was no such difference when applying the same analysis to those with the APOE ε2 allele.
Discussion
Our results show that the APOE ε2 allele appeared significantly more frequently in those found to be definite PART when compared with those who had AD pathological changes at death. Conversely, the APOE ε4 allele was more frequently found in those with AD pathological changes when compared with possible PART, definite PART or those pathologically normal for age. Present data are consistent with an earlier, less extensive study which pre-dates the inception of PART consensus criteria [9] and also a more recent study on individuals older than 85 years of age at death [3].
Previous studies have shown average age at death of those with PART to be higher than those with AD pathology [12]. Here, we show that, although those with AD pathological changes died at a younger age than those with PART changes, the difference was not statistically significant. This is probably due to different recruitment strategies of the two cohorts with BDR being case/control and UMLCHA more community or population based. These differences have been discussed in an earlier publication [26].
Cognitive impairment due to PART pathology is not yet fully understood. The majority of those with PART diagnosed post-mortem are considered to be non-demented [16] and it is thought that cognitive impairment is mainly associated with very severe PART pathology [6]. We show that cognitive impairment was only found in 20% of individuals with possible PART and was completely absent in those considered definite PART. Interestingly, there were significantly more individuals with cognitive impairment in the pathologically normal for age group when compared with those in the definite PART group. One interpretation could be statistical ‘noise’, though at p = 0.006, this would be unlikely. Another could be the inclusion of individuals at Thal phase 1, which reflects cortical Aβ pathology at its earliest stage, in the pathologically normal for age group as cognitive impairment can be apparent in individuals with a low burden of Aβ pathology [35]. This finding could also be due to the increased frequency of APOE ε2 in the definite PART group when compared with the pathologically normal for age group. It is worthy of note that our group has recently shown that carrying APOE ε2 may increase the chances of remaining cognitively normal [27].
The role of APOE ε4 as a risk factor for AD has been known for many years [4, 32] as has the role of APOE ε2 as a protective agent against AD [5]. APOE ε4 carriers are more likely to have significant Aβ load [20] whereas APOE ε2 carriers have a reduced Aβ burden [7]. Hence, in the present study, those with classic AD pathological changes (tau and Aβ) were more likely to carry APOE ε4 whereas those with definite PART were more likely to carry APOE ε2 and, thus, show no Aβ pathology.
This raises the question of what influence (if any) APOE ε2 has on the disease process. By definition, there is a lack of Aβ in PART and it is possible that APOE ε2 has an effect on amyloidogenesis or clearance of Aβ [17]. Likewise, it is also possible that the lack of Aβ in PART may be due to an absence of APOE ε4, which is known to strongly facilitate the deposition of Aβ [19], rather than the presence of APOE ε2, which may simply have a ‘neutral’ effect. However, a recent study [10] has shown that Aβ levels in those with APOE 2,4 genotype increased at half the rate with respect to increasing age when compared with those with APOE 3,4 which suggests that APOE ε2 has an effect on Aβ deposition even in those with a coexisting APOE ε4 allele. If APOE ε2 does in fact play a part, it may prevent deposition of Aβ by binding and stabilising it in brain parenchyma or vessels. If Aβ is excreted from the brain via perivascular channels and the role of APOE ε4 protein is to stabilise Aβ within the brain tissue and vessels, then the lack of Aβ in brain tissue in those with APOE ε2 ought to result in low levels of CAA. Here, we show that this is the case as those with APOE ε4 were more likely to have moderate to severe CAA whereas there was no such difference when applying the same analysis to those with the APOE ε2.
Another potential role for APOE could be the facilitation of NFTs in PART. Work using induced pluripotent stem cells which were differentiated into cultures of forebrain excitatory neurons has already shown that the presence of APOE ε4 can speed up the spread of tau pathology [33]. Another study has shown that the APOE ε2 allele is associated with a greater tau burden in brains with progressive supranuclear palsy (PSP) and that those with APOE ε2/ε2 genotype were found to have increased risk of PSP and corticobasal degeneration [38]. However, we have shown a lack of NFTs in those considered pathologically normal for age with APOE ε2 which would argue against such a role. Hence, the role of APOE ε2 seems to be restricted to any influence it may have over Aβ deposition. Although NFTs and Aβ coexist in AD, it is clear that Aβ is not (always) a prerequisite for NFT formation as, in PART, NFTs can occur independently of Aβ deposition. It is possible that, even in AD, the two pathological events are coincidental rather than causal.
Conclusions
The differences in APOE allele frequency between the groups in the present study supports the conclusion that PART and AD are distinct entities. We show that those with definite PART are significantly more likely to carry APOE ε2 allele(s) and be considered cognitively normal at death compared to those with AD pathological changes. In addition, those with possible/definite PART are less likely to carry APOE ε4 allele(s) than those with AD pathological changes. We postulate that the lack of Aβ in definite PART cases may be due either to an increased frequency of APOE ε2 (or decreased frequency of APOE ε4) in these cases. Similarly, an increased frequency of APOE ε2 (or decreased frequency of APOE ε4) leads to decreased levels of cognitive impairment, which raises questions regarding the impact of Aβ pathology on overall cognition in elderly subjects. It may be possible to use the increased frequency of APOE ε2 in definite PART to assist neuropathological diagnosis.
Supplementary information
Additional file 1 .Table 1. Neuropathological overview of the 152 eligible participants. Description of data: Breakdown of neuropathological findings which was used to determine pathology groups for the present study. (XLSX 23 kb)
Acknowledgements
The work of Manchester Brain Bank is supported by Alzheimer’s Research UK and Alzheimer’s Society through the Brains For Dementia Research (BDR) Programme.
Abbreviations
- Aβ
beta-amyloid
- AD
Alzheimer’s disease
- APOE
Apolipoprotein E
- BDR
Brains for Dementia Research
- CAA
cerebral amyloid angiopathy
- CDR
clinical dementia rating
- MAPT
microtubule associated protein tau
- NFTs
neurofibrillary tangles
- PART
primary age-related tauopathy
- PSP
progressive supranuclear palsy
- TDP-43
TAR DNA-binding protein 43
- TICSm
modified Telephone Instrument for Cognitive Status
- UMLCHA
The University of Manchester Longitudinal Study of Cognition in Normal Healthy Old Age
Authors’ contributions
AR devised and designed the study, performed all statistical analysis and wrote the paper. YD performed immunochemistry and assisted with preparation of the manuscript. FR finalised neuropathological diagnosis and assisted with preparation of the manuscript. JM performed immunochemistry and assisted with preparation of the manuscript. PT provided clinical data for BDR cohort. MH helped to finalise clinical cognitive impairment diagnosis and provided clinical data for UMLCHA cohort. AP assisted with preparation of the manuscript. NP finalised clinical cognitive impairment diagnosis and assisted with preparation of the manuscript. DM finalised neuropathological diagnosis and assisted with preparation of the manuscript. All authors read and approved the final manuscript.
Funding
UMLCHA was funded by Medical Research Council, Economic and Social Research Council, The Wellcome Trust (grant reference number 003889) and Unilever PLC. The work of Manchester Brain Bank is supported by Alzheimer’s Research UK and Alzheimer’s Society through the Brains For Dementia Research (BDR) Programme.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by Manchester Brain Bank Management Committee (REC reference 19/NE/0242). Under conditions agreed with the Research Ethics Committee, The Manchester Brain Bank can supply tissue or data to researchers, without requirement for researchers to apply individually to the REC for approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Neil Pendleton and David M. A. Mann have contributed equally to this work
Supplementary information
Supplementary information accompanies this paper at 10.1186/s40478-020-01095-1.
References
- 1.Bancher C, Jellinger KA. Neurofibrillary tangle predominant form of senile dementia of Alzheimer type: a rare subtype in very old subjects. Acta Neuropathol. 1994;88:565–570. doi: 10.1007/bf00296494. [DOI] [PubMed] [Google Scholar]
- 2.Bancher C, Egensperger R, Kosel S, Jellinger K, Graeber MB. Low prevalence of apolipoprotein E epsilon 4 allele in the neurofibrillary tangle predominant form of senile dementia. Acta Neuropathol. 1997;94:403–409. doi: 10.1007/s004010050726. [DOI] [PubMed] [Google Scholar]
- 3.Bell WR, An Y, Kageyama Y, English C, Rudow GL, Pletnikova O, et al. Neuropathologic, genetic, and longitudinal cognitive profiles in primary age-related tauopathy (PART) and Alzheimer’s disease. Alzheimers Dement. 2019;15:8–16. doi: 10.1016/j.jalz.2018.07.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzhiemer’s disease in late onset families. Science. 1993;261:921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 5.Corder EH, Saunders AM, Risch NJ, Strittmatter WJ, Schmechel DE, Gaskell PC, Jr, et al. Protective effect of apolipoprotien E type 2 for late onset Alzheimer disease. Nat Genet. 1994;7:180–184. doi: 10.1038/ng0694-180. [DOI] [PubMed] [Google Scholar]
- 6.Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I, et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 2014;128:755–766. doi: 10.1007/s00401-014-1349-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fleisher AS, Chen K, Liu X, Ayutyanont N, Roontiva A, Thiyyagura P, et al. Apolipoprotein E ε4 and age effects on florbetapir positron emission tomography in healthy aging and Alzheimer disease. Neurobiol Aging. 2013;34:1–12. doi: 10.1016/j.neurobiolaging.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 8.Hickman RA, Flowers XE, Wisniewski T. Primary age-related tauopathy (PART): addressing the spectrum of neuronal tauopathic changes in the aging brain. Curr Neurol Neurosci Rep. 2020;20:39. doi: 10.1007/s11910-020-01063-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ikeda K, Akiyama H, Arai T, Sahara N, Mori H, Usami M, et al. A subset of senile dementia with high incidence of the apolipoprotein E epsilon2 allele. Ann Neurol. 1997;41:693–695. doi: 10.1002/ana.410410522. [DOI] [PubMed] [Google Scholar]
- 10.Insel PS, Hansson O, Mattsson-Carlgren N. Association between apolipoprotein E ε2 vs ε4, age, and β-amyloid in adults without cognitive impairment. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jellinger KA, Bancher C. Senile dementia with tangles (tangle predominant form of senile dementia) Brain Pathol. 1998;8:367–376. doi: 10.1111/j.1750-3639.1998.tb00160.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jellinger K, Attems J. Neurofibrillary tangle-predominant dementia: comparison with classical Alzheimer disease. Acta Neuropathol. 2007;113:107–117. doi: 10.1007/s00401-006-0156-7. [DOI] [PubMed] [Google Scholar]
- 13.Josephs KA, Murray ME, Tosakulwong N, Whitwell JL, Knopman DS, Machulda MM, et al. Tau aggregation influences cognition and hippocampal atrophy in the absence of beta-amyloid: a clinic-imaging-pathological study of primary age-related tauopathy (PART) Acta Neuropathol. 2017;133:705–715. doi: 10.1007/s00401-017-1681-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kovacs GG, Alafuzoff I, Al-Sarraj S, Arzberger T, Bogdanovic N, Capellari S, et al. Mixed brain pathologies in dementia: the BrainNet Europe consortium experience. Dement Geriatr Cogn Disord. 2008;26:343–350. doi: 10.1159/000161560. [DOI] [PubMed] [Google Scholar]
- 15.Kovacs GG, Milenkovic I, Wöhrer A, Höftberger R, Gelpi E, Haberler C, et al. Non-Alzheimer neurodegenerative pathologies and their combinations are more frequent than commonly believed in the elderly brain: a community-based autopsy series. Acta Neuropathol. 2013;126:365–384. doi: 10.1007/s00401-013-1157-y. [DOI] [PubMed] [Google Scholar]
- 16.Kryscio RJ, Abner EL, Jicha GA, Nelson PT, Smith CD, Van Eldik LJ, et al. Self-reported memory complaints: a comparison of demented and unimpaired outcomes. J Prev Alzheimers Dis. 2016;3:13–19. doi: 10.14283/jpad.2015.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu CC, Kanekiyo T, Xu H, Bu G. Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat Rev Neurol. 2013;9:106–118. doi: 10.1038/nrneurol.2012.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCarron M, Nicoll J. High frequency of apolipoprotein E e2 allele is specific for patients with cerebral amyloid angiopathy-related haemorrhage. Neurosci Lett. 1998;247:45–48. doi: 10.1016/S0304-3940(98)00286-9. [DOI] [PubMed] [Google Scholar]
- 19.Manelli AM, Stine WB, Van Eldik LJ, LaDu MJ. ApoE and Abeta1-42 interactions: effects of isoform and conformation on structure and function. J Mol Neurosci. 2004;23:235–246. doi: 10.1385/JMN:23:3:235. [DOI] [PubMed] [Google Scholar]
- 20.Morris JC, Roe CM, Xiong C, Fagan AM, Goate AM, Holtzman DM, et al. APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol. 2010;67:122–131. doi: 10.1002/ana.21843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nelson PT, Abner EL, Schmitt FA, Kryscio RJ, Jicha GA, Santacruz K, et al. Brains with medial temporal lobe neurofibrillary tangles but no neuritic amyloid plaques are a diagnostic dilemma but may have pathogenetic aspects distinct from Alzheimer disease. J Neuropathol Exp Neurol. 2009;68:774–784. doi: 10.1097/NEN.0b013e3181aacbe9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nelson PT, Alafuzoff I, Bigio EH, Bouras C, Braak H, Cairns NJ, et al. Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. J Neuropathol Exp Neurol. 2012;71:362–381. doi: 10.1097/NEN.0b013e31825018f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Obi K, Akiyama H, Kondo H, Shimomura Y, Hasegawa M, Iwatsubo T, et al. Relationship of phosphorylated alpha-synuclein and tau accumulation to Abeta deposition in the cerebral cortex of dementia with Lewy bodies. Exp Neurol. 2008;210:409–420. doi: 10.1016/j.expneurol.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 24.Rabbitt PMA, McInnes L, Diggle P, Holland F, Bent N, Abson V, et al. The University of Manchester Longitudinal Study of Cognition in Normal Healthy Old Age, 1983 through 2003. Aging Neuropsychol C. 2004;11:245–279. doi: 10.1080/13825580490511116. [DOI] [Google Scholar]
- 25.Robinson AC, Davidson YS, Horan MA, Pendleton N, Mann DMA. Pathological correlates of cognitive impairment in The University of Manchester Longitudinal Study of Cognition in Normal Healthy Old Age. J Alzheimers Dis. 2018;64:483–496. doi: 10.3233/JAD-180171. [DOI] [PubMed] [Google Scholar]
- 26.Robinson AC, Chew-Graham S, Davidson YS, Horan MA, Roncaroli F, Minshull J, et al. A comparative study of pathological outcomes in The University of Manchester Longitudinal Study of Cognition in Normal Healthy Old Age and Brains for Dementia Research Cohorts. J Alzheimers Dis. 2020;73:619–632. doi: 10.3233/JAD-190580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robinson AC, Davidson YS, Roncaroli F, Minshull J, Tinkler P, Horan MA, et al. Influence of APOE genotype on mortality and cognitive impairment. J Alzheimers Dis Rep. 2020;4:281–286. doi: 10.3233/ADR-200203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santa-Maria I, Haggiagi A, Liu X, Wasserscheid J, Nelson PT, Dewar K, et al. The MAPT H1 haplotype is associated with tangle-predominant dementia. Acta Neuropathol. 2012;124:693–704. doi: 10.1007/s00401-012-1017-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider JA, Aggarwal NT, Barnes L, Boyle P, Bennett DA. The neuropathology of older persons with and without dementia from community versus clinic cohorts. J Alzheimers Dis. 2009;18:691–701. doi: 10.3233/JAD-2009-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seo EH, Lee DY, Kim SG, Kim KW, Kim DH, Kim BJ, et al. Validity of the telephone interview for cognitive status (TICS) and modified TICS (TICSm) for mild cognitive impairment (MCI) and dementia screening. Arch Gerontol Geriatr. 2011;25:e26–e30. doi: 10.1016/j.archger.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Skrobot OA, Attems J, Esiri M, Hortobágyi T, Ironside JW, Kalaria RN, et al. Vascular cognitive impairment neuropathology guidelines (VCING): the contribution of cerebrovascular pathology to cognitive impairment. Brain. 2016;139:2957–2969. doi: 10.1093/brain/aww214. [DOI] [PubMed] [Google Scholar]
- 32.Strittmatter WJ, Roses AD. Apolipoprotein E and Alzheimer’s disease. Ann Rev Neurosci. 1996;19:53–77. doi: 10.1146/annurev.ne.19.030196.000413. [DOI] [PubMed] [Google Scholar]
- 33.Wadhwani AR, Affaneh A, Van Gulden S, Kessler JA. Neuronal apolipoprotein E4 increases cell death and phosphorylated tau release in Alzheimer’s disease. Ann Neurol. 2019;85:726–739. doi: 10.1002/ana.25455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wenham PR, Price WH, Blandell G. Apolipoprotein E genotyping by one-stage PCR. Lancet. 1991;337:1158–1159. doi: 10.1016/0140-6736(91)92823-k. [DOI] [PubMed] [Google Scholar]
- 35.Wharton SB, Wang D, Parikh C, Matthews FE, Brayne C, Ince PG, et al. Epidemiological pathology of Aβ deposition in the ageing brain in CFAS: addition of multiple Aβ-derived measures does not improve dementia assessment using logistic regression and machine learning approaches. Acta Neuropathol Commun. 2019;7:198. doi: 10.1186/s40478-019-0858-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamada M, Itoh Y, Suematsu N, Otomo E, Matsushita M. Apolipoprotein E genotype in elderly nondemented subjects without senile changes in the brain. Ann Neurol. 1996;40:243–245. doi: 10.1002/ana.410400217. [DOI] [PubMed] [Google Scholar]
- 37.Zhang X, Sun B, Wang X, Lu H, Shao F, Rozemuller AJM, et al. Phosphorylated TDP-43 staging of primary age-related tauopathy. Neurosci Bull. 2019;35:183–192. doi: 10.1007/s12264-018-0300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao N, Liu CC, Van Ingelgom AJ, Linares C, Kurti A, Knight JA, et al. APOE ε2 is associated with increased tau pathology in primary tauopathy. Nat Commun. 2018;9:4388. doi: 10.1038/s41467-018-06783-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 .Table 1. Neuropathological overview of the 152 eligible participants. Description of data: Breakdown of neuropathological findings which was used to determine pathology groups for the present study. (XLSX 23 kb)
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.


