Abstract
Objective
To test the hypothesis that health systems provide better care to patients with high needs by comparing differences in quality between system‐affiliated and nonaffiliated physician organizations (POs) and to examine variability in quality across health systems.
Data Sources
2015 Medicare Data on Provider Practice and Specialty linked physicians to POs. Medicare Provider Enrollment, Chain, and Ownership System (PECOS) and IRS Form 990 data identified health system affiliations. Fee‐for‐service Medicare enrollment and claims data were used to examine quality.
Study Design
This cross‐sectional analysis of beneficiaries with high needs, defined as having more than twice the expected spending of an average beneficiary, examined six quality measures: continuity of care, follow‐up visits after hospitalizations and emergency department (ED) visits, ED visits, all‐cause readmissions, and ambulatory care‐sensitive hospitalizations. Using a matched‐pair design, we estimated beneficiary‐level regression models with PO random effects to compare quality of care in system‐affiliated and nonaffiliated POs. We then limited the sample to system‐affiliated POs and estimated models with system random effects to examine variability in quality across systems.
Principal Findings
Among 2 323 301 beneficiaries with high needs, 52.3% received care from system‐affiliated POs. Rates of ED visits were statistically significantly different in system‐affiliated POs (117.5 per 100) and nonaffiliated POs (106.8 per 100, P < .0001). Small differences in the other five quality measures were observed across a range of sensitivity analyses. Among systems, substantial variation was observed for rates of continuity of care (90% of systems had rates between 70.8% and 89.4%) and follow‐up after ED visits (90% of systems had rates between 56.9% and 73.5%).
Conclusions
Small differences in quality of care were observed among beneficiaries with high needs receiving care from system POs and nonsystem POs. Health systems may not confer hypothesized quality advantages to patients with high needs.
Keywords: health care delivery, health care systems, Medicare, quality of health care, vulnerable populations
What is Known on this Topic
A growing number of physician organizations (POs) are affiliating with health systems, yet little is known about how health systems may influence care delivered to patients who have high needs as most studies have focused on care delivered to broad patient populations.
What this Study Adds
System‐affiliated POs had higher rates of ED visits than nonaffiliated POs, and small differences in the other five quality measures were observed across a range of sensitivity analyses.
In health system‐level analyses, performance on these six quality measures was mixed, suggesting that systems were unlikely to be consistently high (or low) performing.
Overall findings suggest that health systems may not confer hypothesized quality advantages to patients with high needs, suggesting that a variety of care management and informal integration approaches used by POs promote patient care.
1. INTRODUCTION
The health care landscape is evolving, as an increasing number of physician organizations (POs) are joining health systems or becoming acquired by them. The percentage of POs affiliated with health systems increased from 14% to 31% from 2012 to 2018, accompanied by a 26% to 44% increase in the percentage of physicians employed by health systems during the same time frame. 1 As the number of POs joining health systems grows, policy makers and regulators are increasingly interested in understanding the impact of this change on cost, quality, and health outcomes. Systematic reviews suggest there is some benefit of health system ownership of POs on clinical process measures of quality, but no differences or worse outcomes for measures of spending and utilization. 2 , 3 Little is known, however, about how health system affiliation may influence care delivered to patients who have high needs.
Individuals who have high needs may benefit from care delivered in health systems because they are likely to seek care in multiple settings (eg, ambulatory setting and hospitals) and interact with multiple providers (eg, primary care providers (PCPs) and subspecialists), and health systems may be better able to manage these interactions. Although the literature includes varying definitions of “high needs,” as was noted in a 2017 National Academy of Medicine report, these individuals are generally described as having one or more of the following characteristics: high use of health care services, high health care costs, multiple chronic conditions or disabilities, and limitations with activities of daily living. 4 Evidence from a recent systematic review indicates that care management is beneficial to patients with high needs, as measured by improved health, health care use and spending, and patient satisfaction. 5 We hypothesize that health systems may be well‐positioned to deliver high‐quality care to patients who have high needs through better care management for several reasons. First, system‐affiliated POs may have greater access to capital, 6 allowing them to invest in interventions to promote care for patients who have high needs. Second, health systems may be more engaged in care management of patients who have high needs, as POs report greater use of care management processes following acquisition by a hospital. 7 Third, system‐affiliated POs report greater health IT adoption than nonaffiliated POs. 8 Health IT functionalities may facilitate care management by enabling POs to construct registries of high‐need patients, exchange information across providers and settings, and communicate electronically with patients.
On the other hand, it is possible that similar levels of care are provided by POs that are not affiliated with health systems. Care management is a widely used strategy for addressing the needs of this population 9 , 10 , 11 and both affiliated and nonaffiliated POs report increasing use of care management processes over time. 8 Additionally, health systems do not uniformly pursue the same strategies and may not have the same health IT functionalities available at all of their delivery sites. For example, a recent analysis reported variation in health IT adoption across systems, with POs affiliated with smaller systems reporting fewer functionalities than larger systems. 12
Empirical evidence about the quality of care received by patients who have high needs and receive care within and outside of health systems is limited. To our knowledge, only one study has examined this question, finding reductions in unplanned admissions and ED visits for ambulatory care‐sensitive (ACS) chronic conditions and no impact on mortality or spending among Medicare beneficiaries in affiliated POs compared with nonaffiliated POs. 13 The generalizability and validity of that study's findings are uncertain because it was not peer‐reviewed, did not use a national sample, used a measure of affiliation that was self‐reported by POs, and examined only a limited number of quality measures. 13 Therefore, the question of whether systems may provide better care to patients who have high need remains unanswered.
Using 2015 data on Medicare beneficiaries who have high needs and information on PO health system affiliation, our study had three objectives. First, we determined the fraction of Medicare beneficiaries who have high needs and whose usual source of care was a PO affiliated with a health system. Second, we tested the hypothesis that health systems provide better care for beneficiaries with high needs by comparing differences in quality of care across six measures for affiliated and nonaffiliated POs. Third, because no studies have characterized variability in quality across health systems for this patient population, we examined system‐level variability in the quality of care provided to beneficiaries who have high needs to identify whether there was meaningful variability in care provided across systems for different measures.
2. METHODS
2.1. Data
This cross‐sectional analysis of 100% of fee‐for‐service (FFS) claims for Medicare beneficiaries in the United States aged 18 years and older used 2015 Medicare enrollment and claims data to examine quality of care and the 2015 Medicare Data on Provider Practice and Specialty (MD‐PPAS) to link physicians to POs. To identify system‐affiliated POs, we used data from the 2015 Medicare Provider Enrollment, Chain, and Ownership System (PECOS) and the Internal Revenue Service (IRS) Form 990 database. PECOS is the gold standard source for identifying ownership relationships between POs and health systems. The IRS Form 990 database is a publicly available repository of tax documents that are filed by not‐for‐profit companies, which include many health systems, hospitals, and POs. Form 990 Schedule R lists organizations related to the parent organization and thus provides a second source for identifying system‐affiliated POs and other relationships. We also used 2014 files for these data sources to construct a sample that excluded POs newly affiliating with a health system in the year preceding the study year in order to explore the sensitivity of our results to this exclusion, hypothesizing that these newly affiliated POs may not yet be fully integrated into their systems.
2.2. Sample
Using the MD‐PPAS data, we identified POs and their associated physicians using taxpayer identification numbers (TINs) and National Provider Identifiers (NPIs). TINs were combined into a single PO if they were from the same academic POs or shared a large fraction of their physicians. POs were identified as affiliated with health systems using PECOS and IRS Form 990, which enabled linkage of POs and hospitals that were mutually related through common ownership or management arrangements. Building on definitions from the Agency for Healthcare Research and Quality's Comparative Health System Performance Initiative, 14 health systems were defined as comprising one or more short‐term general acute care hospitals and one or more POs with at least one PCP and at least five total physicians total across all of the system's affiliated POs. Medicare beneficiaries were attributed to POs based on the plurality of their ambulatory visits to PCPs (ie, general internists or family physicians), or, for those beneficiaries who did not visit PCPs, the plurality of visits with internal medicine subspecialists (ie, cardiology, endocrinology, gastroenterology, hematology/oncology, infectious disease, nephrology, pulmonology/critical care, rheumatology/immunology, and physical medicine/rehabilitation). Among 50 996 POs providing primary care to Medicare beneficiaries, we excluded 34 766 POs that had only one physician, 223 POs affiliated with health systems comprising fewer than 5 total physicians, and 44 POs that could not be assigned to one or more hospital referral regions (HRRs) because all ZIP codes of attributed beneficiaries were either missing or located outside of the 50 US states or District of Columbia. We then excluded HRRs where most or very few beneficiaries received care from system POs, based on the 10th and 90th percentiles of the percentage of beneficiaries attributed to a system PO in an HRR, to facilitate matching of system and nonsystem POs in the same HRR, leading to the exclusion of 1638 POs. The analytic sample prior to matching included 14 325 POs.
Beneficiaries were identified as having high needs if they had twice the expected spending of an average Medicare beneficiary (ie, Hierarchical Condition Categories (HCC) risk scores of two or greater). HCC risk scores are derived from a predictive model based on diagnosis codes and used to estimate a beneficiary's risk for generating high health care expenditures during the coming year. They are used by CMS for Medicare Advantage plan payment 15 and have been used to identify beneficiaries who have high needs. 16 , 17
2.3. Dependent variables
Six quality‐of‐care measures were selected based on their relevance to beneficiaries with high needs, reflecting goals of interventions focused on this population to facilitate care transitions and receipt of primary care. 18 , 19 Full measure specifications are included in the Appendix S1. Related to care transitions, we examined two dichotomous measures identifying beneficiaries receiving follow‐up outpatient visits within 14 days of an emergency department (ED) visit and within 30 days of a hospital discharge. We also examined all‐cause readmissions within 30 days of hospital discharge and all‐cause ED visits. Related to provision of primary care, we examined hospitalizations for ACS chronic conditions, which identify hospitalizations that could have been avoided with appropriate primary and preventive care. 20 We also examined continuity of care, using the Usual Provider Continuity index, defined as the proportion of primary care visits made to the beneficiary's usual source of care (range = 0‐1), among beneficiaries who had three or more primary care visits. 21 Usual source of care was defined as the provider (ie, National Provider Identifier) associated with a plurality of primary care visits. A description of the approach used to identify primary care visits and follow‐up visits is included in the Appendix S1.
2.4. Explanatory variables
The key explanatory variable of interest was a dichotomous variable indicating whether a PO was affiliated or not affiliated with a health system. Beneficiary‐level covariates derived from Medicare enrollment data included age in years and dichotomous indicators for female sex, disability, dual eligibility, and receipt of the low‐income subsidy for Part D costs. Race/ethnicity was imputed using the Medicare Bayesian Improved Surname Geocoding 2.0 methodology, which combines Medicare administrative data with US census data to derive probabilities of membership in each of six racial/ethnic groups for each beneficiary (White, Black, Hispanic, Asian/Pacific Islander, American Indian/Alaska Native, and multiracial). 22 County‐level rurality was defined using the Rural‐Urban Continuum Codes and categorized as metropolitan (metro), nonmetro adjacent to metro, and nonmetro not adjacent to metro. A beneficiary's measure of neighborhood socioeconomic status (SES) was measured using an index constructed at the ZIP code level using six items from the 2011‐2015 pooled American Community Survey. 23 PO‐level covariates included total physicians, total beneficiaries, and the percentage of physicians who were PCPs.
2.5. Propensity score estimation
Because system and nonsystem POs differ on many observed factors, we used propensity score matching to construct a sample of system and nonsystem POs similar on observable characteristics to reduce bias in our estimates of the association between system affiliation and quality of care. 24 The matched sample was constructed by estimating propensity scores for POs using a logistic regression model to estimate the probability of system affiliation, which adjusted for all aforementioned beneficiary characteristics agreed to the PO level (eg, percentage of beneficiaries in the PO who were female) and all aforementioned PO‐level characteristics. We used one‐to‐one matching with a caliper of 0.20 standard deviations of the logit of the propensity score distribution, as recommended by Austin, 25 and required exact matching within HRR. POs were assigned to the HRR where a plurality of beneficiaries lived (median = 92.8%). Matching was based on characteristics of all beneficiaries in POs to ensure the final sample was generalizable to all POs treating FFS Medicare beneficiaries. After generating the matched sample, we excluded beneficiaries who did not have high needs and matched pairs of POs for which one or both POs did not treat beneficiaries who had high needs in order to maintain balance.
2.6. Analytic approach
Using the matched sample of beneficiaries who had high needs, we estimated beneficiary‐level regression models to compare performance of system‐affiliated POs and nonaffiliated POs using Proc GLIMMIX in SAS (Version 9.4). We estimated logistic regression models for dichotomous and binomial dependent variables and negative binomial regression models for count dependent variables. The key explanatory variable was the dichotomous variable indicating that a beneficiary was attributed to a system‐affiliated PO. Models also included PO‐level random effects, and standard errors were clustered at the PO level. To examine the sensitivity of the results to different specifications, we estimated models that adjusted for (a) beneficiary‐level characteristics only, (b) beneficiary‐ and PO‐level characteristics, and (c) beneficiary‐ and PO‐level characteristics and HRR fixed effects (main analysis). We also explored the sensitivity of our results to the exclusion of POs newly affiliated in 2015, hypothesizing that these POs may not yet be fully integrated into systems, and to PO size, which was constructed based on the distribution of the variable (2‐4 physicians [small], 5‐9 physicians [medium], and 10 or more physicians [large]). Additionally, because beneficiaries younger than 65 years are disabled or have another qualifying health condition, we also estimated all models separately for beneficiaries younger than 65 years and beneficiaries aged 65 years and older. For all models, we generated recycled predictions to estimate means for each dependent variable by health system affiliation, using the estimation sample and holding other covariates fixed at their observed values. 26
To examine variation in the quality measures at the system level, we estimated beneficiary‐level regression models, inclusive of beneficiaries who had high needs and received care from system‐affiliated POs, for each performance measure using Proc GLIMMIX in SAS. POs attributed to more than one system (0.01% of the sample) were excluded from this analysis. Models included system‐level random effects and adjusted for all beneficiary‐level variables. We estimated models inclusive of all systems and models stratified by system size. System size was categorized based on the distribution of total physicians: small (less than the 25th percentile, corresponding to <12 physicians), medium (25th to 75th percentile, corresponding to 12 to 179 physicians), and large (greater than the 75th percentile, corresponding to >179 physicians). We generated recycled predictions to estimate predicted mean outcomes for each health system, among systems with at least 30 beneficiaries contributing to a measure, generating a prediction for each beneficiary in the estimation sample and keeping other covariates fixed at their observed values. 26 To compare overall quality across systems, we constructed a standardized composite measure for each health system, a common approach. 27 We did this by calculating z‐scores to standardize all measures, taking the average across measures, and standardizing the composite.
For all models, results are presented as percentages for dichotomous and binomial dependent variables and as rates for count dependent variables. This study was approved by the corresponding author's Institutional Review Board.
3. RESULTS
Among 18 844 619 Medicare beneficiaries who received care from POs eligible for this analysis, 12.6% had high needs (N = 2 323 301). More than half (52.3%) of Medicare beneficiaries who have high needs received care from POs affiliated with health systems (Table 1), which was similar to the percentage observed among all beneficiaries (50.8%). These beneficiaries had more than three times the expected spending of an average Medicare beneficiary (mean HCC score = 3.3). On average, beneficiaries with high needs receiving care from system‐affiliated POs were less likely to be Hispanic (5.3% vs 8.1%) and live in metro areas (64.4% vs 82.5%) than beneficiaries receiving care from nonaffiliated POs. On average, POs affiliated with health systems were larger (89 vs 12 physicians) and had a lower percentage of physicians providing primary care (52.2% vs 76.5%) than nonaffiliated POs.
TABLE 1.
Characteristics of physician organizations (POs) and Medicare beneficiaries who have high needs, full sample before matching, by system affiliation status in 2015
| System‐affiliated POs | Nonaffiliated POs | |
|---|---|---|
| Characteristics of beneficiaries | ||
| Age in years, mean | 70.2 | 70.2 |
| HCC score, mean | 3.3 | 3.3 |
| Female, % | 56.4 | 56.5 |
| Disabled, % | 30.4 | 28.9 |
| Dually eligible, % | 27.0 | 27.7 |
| Received low‐income subsidy for Part D costs, % | 3.0 | 2.8 |
| Race/ethnicity, % | ||
| White | 79.5 | 73.5 |
| Black | 9.7 | 11.3 |
| Hispanic | 5.3 | 8.1 |
| Asian or Pacific Islander | 1.9 | 3.6 |
| American Indian or Alaskan Native | 0.7 | 0.9 |
| Multiracial | 2.9 | 2.6 |
| County rurality, % | ||
| Metropolitan (metro) | 64.4 | 82.5 |
| Nonmetro, adjacent to metro | 21.9 | 12.3 |
| Nonmetro, not adjacent to metro | 13.7 | 5.2 |
| Neighborhood SES index, mean | 0.1 | 0.1 |
| Census Division, % a | ||
| New England | 8.1 | 6.1 |
| Middle Atlantic | 12.1 | 14.4 |
| East North Central | 19.8 | 14.9 |
| West North Central | 10.3 | 5.5 |
| South Atlantic | 18.5 | 26.3 |
| East South Central | 6.3 | 7.5 |
| West South Central | 9.8 | 10.0 |
| Mountain | 5.2 | 4.9 |
| Pacific | 9.9 | 10.4 |
| Characteristics of physician organizations | ||
| Total physicians, mean | 89 | 12 |
| Total beneficiaries, mean | 3677 | 815 |
| Physicians providing primary care, % | 52.2 | 76.5 |
| Total beneficiaries | 1 214 201 | 1 109 100 |
| Total POs | 2552 | 11 128 |
Table describes POs providing primary care to Medicare beneficiaries who have high needs and characteristics of those beneficiaries in 2015.
Abbreviations: HCC, Hierarchical Condition Categories; PO, physician organization; SES, socioeconomic status.
Census divisions include the following states: New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont); Mid‐Atlantic (New Jersey, New York, and Pennsylvania); East North Central (Illinois, Indiana, Michigan, Ohio, and Wisconsin); West North Central (Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota); South Atlantic (Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, District of Columbia, and West Virginia); East South Central (Alabama, Kentucky, Mississippi, and Tennessee); West South Central (Arkansas, Louisiana, Oklahoma, and Texas); Mountain (Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, and Wyoming); and Pacific (Alaska, California, Hawaii, Oregon, and Washington).
Following propensity score matching, we identified 3254 POs (1627 matched pairs) treating 414 618 beneficiaries with high needs. Affiliated and nonaffiliated POs were more similar following matching, as measured by smaller standardized differences on observable characteristics (Table A.1 in Appendix S1), and evidenced by overlap in the range and density of propensity scores after matching (Figure A.1 in Appendix S1). The ten most common conditions among beneficiaries with high needs in the matched sample are listed in Figure A.2 in Appendix S1. Nearly half (48.8%) of beneficiaries had congestive heart failure, and 43.9% had chronic obstructive pulmonary disease (COPD). Additionally, 50.0% of beneficiaries had diabetes, with or without complications.
When comparing quality of care in affiliated and nonaffiliated POs, we found small differences in quality for beneficiaries receiving care from affiliated and nonaffiliated POs. In our main analysis (Table 2 and Table A.2 in Appendix S1), we observed that rates of ED visits were higher among beneficiaries in affiliated POs (117.5 per 100) than nonaffiliated POs (106.8 per 100). Additionally, we observed a small, but statistically significant difference in rates of hospitalizations for ACS chronic conditions between beneficiaries in affiliated POs (8.7%) and nonaffiliated POs (8.3%). Results were largely similar in models that adjusted for fewer covariates (Table A.2 in Appendix S1), as well as in models stratified by age (Table A.3 in Appendix S1). Among beneficiaries aged 65 years and older, we also observed a small difference in rates of follow‐up visits within 30 days of hospitalization among system‐affiliated POs (89.5%) and nonaffiliated POs (89.3%); however, this difference was less than 0.5 percentage points.
TABLE 2.
Quality of care for Medicare beneficiaries who have high needs in matched sample receiving care from system‐affiliated and nonaffiliated POs, 2015
| All POs | POs with 2‐4 physicians | POs with 5‐9 physicians | POs with ≥10 physicians | |||||
|---|---|---|---|---|---|---|---|---|
| System‐affiliated POs | Nonaffiliated POs | System‐affiliated POs | Nonaffiliated POs | System‐affiliated POs | Nonaffiliated POs | System‐affiliated POs | Nonaffiliated POs | |
| ED visits per 100 beneficiaries a | 117.5 | 106.8*** | 127.7 | 117.1*** | 137.8 | 119.3* | 115.4 | 106.4*** |
| All‐cause readmission rate a | 22.8 | 22.4 | 22.7 | 22.3 | 25.3 | 22.1 | 22.8 | 22.6 |
| Hospitalizations for ACS chronic conditions a | 8.7 | 8.3* | 9.5 | 9.2 | 11.0 | 9.1 | 8.6 | 8.2** |
| Follow‐up visit within 14 d of ED visit | 65.9 | 66.2 | 64.1 | 66.5* | 67.0 | 64.3** | 66.0 | 66.5* |
| Follow‐up visit within 30 d of hospitalization | 88.0 | 87.6 | 85.9 | 87.4 | 81.3 | 81.3 | 88.1 | 87.3** |
| Continuity of care | 80.4 | 80.7 | 76.7 | 80.7*** | 78.1 | 78.7 | 80.8 | 81.0* |
The table presents mean predicted outcomes for each dependent variable, by health system affiliation, using the results from regression models for the estimation sample of propensity score matched POs and their attributed fee‐for‐service Medicare beneficiaries who have high needs in 2015.
Abbreviations: ACS, ambulatory care‐sensitive; ED, emergency department; PO, physician organization.
Lower rates indicate better quality of care for these measures.
P < .05, **P < .01, ***P < .001.
When examining results stratified by PO size (Table 2 and Table A.4 in Appendix S1), we continued to observe slightly higher rates of ED visits in affiliated POs than nonaffiliated POs. Among small POs, we also observed better performance among nonaffiliated POs than affiliated POs in continuity of care (80.7% vs 76.7%) and follow‐up after ED visits (66.5% vs 64.1%). Among medium POs, system‐affiliated POs also had higher rates of follow‐up after ED visits (67.0% vs 64.3%). Among large POs, we observed differences of less than one percentage point for four measures.
In models comparing nonsystem POs and POs affiliated with systems for more than one year, we observed higher rates of ED visits in affiliated POs than nonaffiliated POs (Table A.5 in Appendix S1). We also observed small, statistically significant differences in rates of follow‐up after ED visits (66.2% vs 65.5%) and hospitalizations (87.9% vs 87.2%), indicating better performance among affiliated POs.
Substantial variation in quality of care for beneficiaries who have high needs was observed across health systems (Figure 1). An average of 794 health systems (range = 705 to 842) were examined for each measure. System‐level rates of continuity of care exhibited substantial variation with rates between 69.3% and 89.7% for 90% of systems (median = 81.5%), and 3.5% of systems had extremely low rates (ie, outliers less than 67.8%). Substantial variation was also observed in rates of follow‐up after ED visits, as 90% of systems had rates between 56.9% and 73.5% (median = 66.2%) and 1.8% of systems had extremely low rates less than 52.3%. When examining variation in quality of care by system size, rates of continuity of care and follow‐up after ED visits remained the measures exhibiting the greatest variation across systems (Figure 2). Median rates of measures were similar across small, medium, and large systems. A notable difference was observed for ED visits. Small systems had the highest median rate of ED visits (158.5 per 100) and the greatest variation in rates of ED visits, as 90% of small systems had rates between 99 and 254 per 100. When examining the composite measures of quality, we found evidence of mixed performance within a system, as systems were unlikely to be consistently high or low performing. Among 211 systems in the top quartile of overall performance, only 13 systems had scores in the top quartile for at least five of six measures, suggesting there is not a consistent pattern of high performance. Similarly, among 211 systems in the bottom quartile of overall performance, only 27 systems had scores in the bottom quartile for at least five of six measures, illustrating no consistent pattern of low performance.
FIGURE 1.
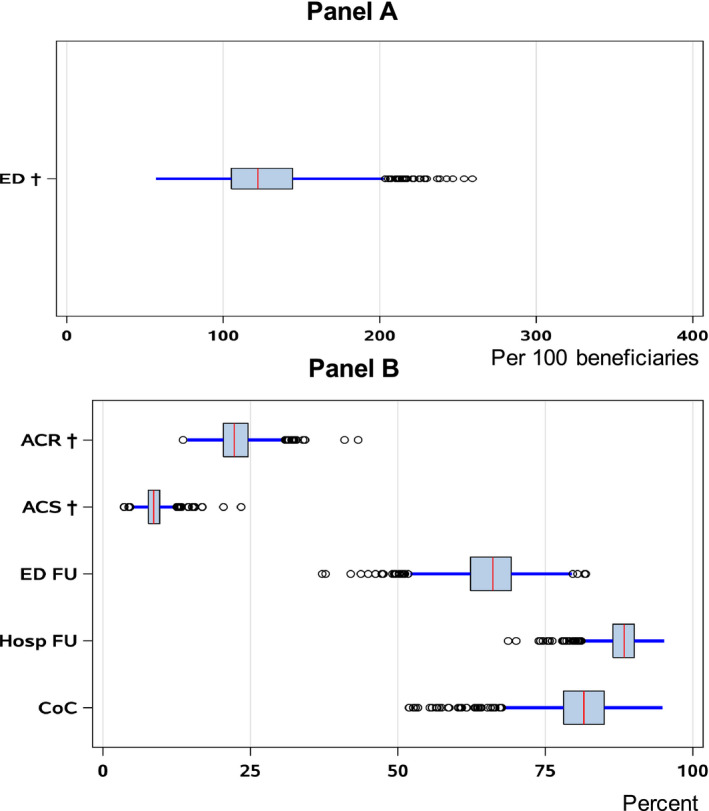
System‐level variation in quality of care for beneficiaries who have high needs, 2015. Figure presents mean predicted outcomes for each performance measure for each health system, among systems with at least 30 beneficiaries contributing to a measure. Predictions are based on results from regression models that include all POs in systems treating fee‐for‐service Medicare beneficiaries who have high needs in 2015. The red line indicates the median health system, the box indicates the middle 50% of systems, and the blue line indicates values between the first quartile and the first quartile minus 1.5 times the interquartile range (IQR) (ie, the “lower fence”) and values between the third quartile and the third quartile plus 1.5 times the IQR (ie, the “upper fence”). The circles indicate values that exceed the upper fence or are less than the lower fence. †Lower rates indicate better quality of care for these measures. Abbreviations include ACR, all‐cause readmission rate; ACS, hospitalizations for ambulatory care‐sensitive chronic conditions; CoC, continuity of care; ED, ED visit rate; ED FU, follow‐up visit 14 d after ED visit; Hosp FU, follow‐up visit 30 d after hospitalization [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
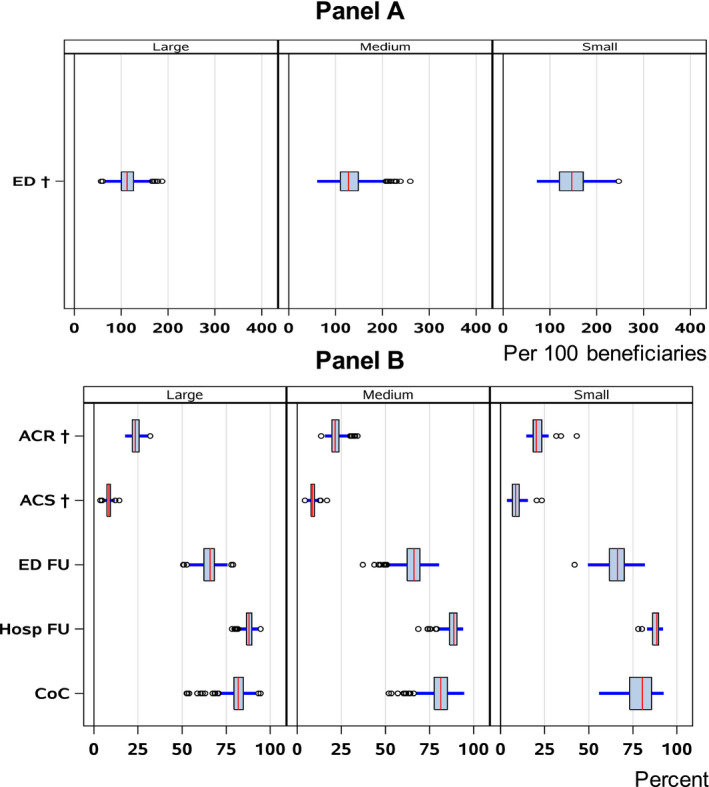
System‐level variation in quality of care for beneficiaries who have high needs, by system size, 2015. Figure presents mean predicted outcomes for each performance measure for each health system, among systems with at least 30 beneficiaries contributing to a measure. Predictions are based on results from regression models that includes all POs in systems treating fee‐for‐service Medicare beneficiaries who have high needs in 2015. System size was categorized based on the distribution of total physicians: small (less than the 25th percentile, corresponding to <12 physicians), medium (25th to 75th percentile, corresponding to 12 to 179 physicians), and large (greater than the 75th percentile, corresponding to >179 physicians). The red line indicates the median health system, the box indicates the middle 50% of systems, and the blue line indicates values between the first quartile and the first quartile minus 1.5 times the interquartile range (IQR) (ie, the “lower fence”) and values between the third quartile and the third quartile plus 1.5 times the IQR (ie, the “upper fence”). The circles beyond the upper fence indicate outliers (a value greater than 1.5 times IQR). †Lower rates indicate better quality of care for these measures. Abbreviations include ACR, all‐cause readmission rate; ACS, hospitalizations for ambulatory care‐sensitive chronic conditions; CoC, continuity of care; ED, ED visit rate; ED FU, follow‐up visit 14 d after ED visit; Hosp FU, follow‐up visit 30 d after hospitalization [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
With a growing number of POs affiliating with health systems, 1 we sought to examine quality of care received in health system‐affiliated POs and nonaffiliated POs by Medicare beneficiaries who have high needs. We found that about half of Medicare beneficiaries who have high needs received care from health systems in 2015. Additionally, we found that rates of ED visits were higher among beneficiaries in system‐affiliated POs than nonaffiliated POs, and small differences in other quality measures across sensitivity analyses. Finally, we found that performance on quality‐of‐care measures varied substantially across health systems—even within strata defined by health system size—and that most systems were not consistently achieving high (or low) performance on most measures.
Our findings of small but higher rates of ED visits in system‐affiliated POs than nonaffiliated POs align with most prior research. A recent systematic review of vertical integration reported mostly null and negative results for measures of utilization. 2 A non–peer‐reviewed study by Wagner reported no differences in ED visits in affiliated POs and nonaffiliated POs among beneficiaries who have chronic conditions 13 ; however, this study differs from ours in that it was limited to a few states and used a different definition of high needs. Although most prior studies were not limited to patients with high needs, they provide evidence about the challenge of increasing follow‐up visits and reducing inefficient care. Across all models, regardless of PO size or longer system affiliation, we failed to find a benefit of system affiliation in reducing ED visits. Our results and evidence from the literature suggest that ownership relationships of hospitals and POs have not led to more coordinated or efficient use of care for patients with high needs.
We hypothesized that health system affiliation would confer advantages to beneficiaries who have high needs, in part because of better care management. We found some evidence of advantages of systems for follow‐up visits among medium and large POs and POs affiliated with systems for more than one year. However, these differences were small, about one percentage point on average, and may not be clinically meaningful. These findings may indicate that nonaffiliated POs may have structures and processes in place that are similar to those in health systems. Care management is a widely recommended and studied intervention for patients who have high needs, 9 , 10 , 11 and both affiliated and nonaffiliated POs report increased use of care management processes over time. 8 Similarly, electronic health record (EHR) adoption is widespread, with 85.9% of office‐based physicians reporting use of an EHR in 2017, 28 and there is evidence that hospital acquisition does not increase POs’ health IT functionality. 7 Thus, affiliated and nonaffiliated POs may have similar capabilities of delivering care to beneficiaries who have high needs and systems may not confer meaningful benefits related to care management to patients who have high needs.
Across systems, even when stratified by size, we observed significant variation in quality performance on a number of the measures. We also found that most systems do not consistently achieve high (or low) performance on most measures examined. A few systems, however, had consistently high quality across multiple measures. Better understanding the mechanisms leading to higher performance in these systems could be informative to strengthening performance among lower performing systems. Findings from a recent literature review and technical expert panel focused on attributes of health system performance highlighted the role of care delivery processes, health information technology, and quality improvement activities and infrastructure. 29 Although larger systems report having more health IT functionalities than smaller systems, 12 with evidence suggesting that health IT functionalities may promote quality, 30 we found little differences in quality across the categories of system size that we examined. Additional research that explores attributes such as culture, leadership, and size can help to identify the factors contributing to high quality in these systems.
Our results are relevant to policy makers considering strategies for improving care for patients who have high needs. Integrating care across multiple settings and providers is encouraged as a strategy for addressing the needs of patients who have high needs 4 , 31 and our findings suggest this integration may occur outside of formal ownership relationships. Additionally, our results, taken within the context of existing evidence that consolidation leads to higher prices, 2 , 3 , 32 highlights the need for enacting policies that emphasize delivery of value‐based care. Of note, a new “direct‐contracting” value‐based payment model from the Centers for Medicare & Medicaid Services (CMS), described as the next phase for accountable care organizations, includes a focus on Medicare beneficiaries who have high needs. 33 Further, our results are relevant to POs who may be considering affiliating with health systems. Although affiliation may be attractive to POs due to the potential to increase profits through increased market share and higher prices, it has been argued that this relationship may be less than ideal for POs in the context of risk‐sharing arrangements and population‐based payment models if health systems put few resources toward improving quality in ambulatory care settings. 2
This study has a number of limitations. Our propensity score model included a variety of covariates and matched POs within the same HRR; however, the underlying assumption of conditional independence (ie, that the propensity score model includes all possible confounders of the association between the treatment and the outcome, including unmeasured factors) may not hold. This limitation is common to propensity score techniques and traditional regression modeling, and highlights our inability to make causal conclusions about whether these results are due to health system affiliation or other features of POs or their patients. For example, if more proactive patients seek out POs in systems because they anticipate needing more coordinated care, this may bias our estimates and lead us to find a positive impact of system affiliation. On the other hand, if sicker patients seek out POs in systems because they anticipate needing more coordinated care, this may lead us to find a negative or null impact of system affiliation. While our use of matching is intended to reduce bias in our estimates, overall these limitations motivate the need for future analyses that utilize longitudinal data and can isolate the causal effect of system affiliation.
Further limitations include our inability to determine the mechanisms impacting performance of the POs studied, some of which cannot be measured in claims data, such as organizational culture and leadership. 34 While we observed some small differences in quality among affiliated and nonaffiliated POs when stratifying by size, systems also differ in their use of advanced practice clinicians, complexity, and mission, among other factors, factors that warrant further exploration. Additionally, our sample did not include non‐FFS Medicare beneficiaries, physicians in solo practice, and POs in HRRs with very high and very low concentrations of POs affiliated in systems, and our findings may have limited generalizability to these beneficiaries and providers. There is no single definition of “high‐need” patients and different definitions may produce different results, but we note that our findings align with much of the existing literature exploring health systems and quality of care. 4 Finally, although we examined a rich set of performance measures that are frequently reported in the literature and used to assess provider performance, future research should consider a broader set of measures to more fully assess whether quality of care differs between affiliated POs and nonaffiliated POs.
As the health care delivery system evolves with different organizational affiliations and relationships, it is important to understand the role of health systems in delivering care to patients who have high needs. This analysis of 2015 Medicare claims data found that system‐affiliated POs do not provide better care than nonaffiliated POs to Medicare beneficiaries who have high needs. Although a minority of health systems consistently achieved high quality on several measures, overall findings suggest that health systems may not confer hypothesized advantages of care management to patients who have high needs.
Supporting information
Author matrix
Appendix S1
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: The authors thank Denis Agniel, Linda Cottrell, Lesley Baseman, and Aaron Kofner from the RAND Corporation for their help preparing of the databases required for the analysis. This work was supported by the RAND Center of Excellence on Health System Performance, which is funded through a cooperative agreement with the Agency for Healthcare Research and Quality (AHRQ) (Agreement No. 1U19HS024067‐01). The content and opinions expressed in this article are solely the responsibility of the authors and do not reflect the views or official positions of AHRQ, the Department of Health and Human Services, or the US government.
Kranz AM, DeYoreo M, Eshete‐Roesler B, et al. Health system affiliation of physician organizations and quality of care for Medicare beneficiaries who have high needs. Health Serv Res 2020;55:1118–1128. 10.1111/1475-6773.13570
REFERENCES
- 1. Physicians Advocacy Institute . Updated physician practice Acquisition Study: National and Regional Changes in Physician Employment 2012–2018. 2019. http://www.physiciansadvocacyinstitute.org/Portals/0/assets/docs/021919‐Avalere‐PAI‐Physician‐Employment‐Trends‐Study‐2018‐Update.pdf?ver=2019‐02‐19‐162735‐117. Accessed March 5, 2020.
- 2. Machta RM, Maurer KA, Jones DJ, Furukawa MF, Rich EC. A systematic review of vertical integration and quality of care, efficiency, and patient‐centered outcomes. Health Care Manage Rev. 2019;44(2):159‐173. [DOI] [PubMed] [Google Scholar]
- 3. Hwang W, Chang J, LaClair M, Paz H. Effects of integrated delivery system on cost and quality. Am J Manag Care. 2013;19(5):e175‐e184. [PubMed] [Google Scholar]
- 4. Chapter 2. key characteristics of high‐need patients In:Long P, Abrams M, Milstein A, et al., eds. Effective Care for High‐need Patients: Opportunities for Improving Outcomes, Value, and Health. Washington, DC: National Academy of Medicine; 2017. [PubMed] [Google Scholar]
- 5. Bleich SN, Sherrod C, Chiang A, et al. Peer reviewed: systematic review of programs treating high‐need and high‐cost people with multiple chronic diseases or disabilities in the United States, 2008–2014. Prev Chronic Dis. 2015;12:E197 10.5888/pcd12.150275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Casalino LP, Wu FM, Ryan AM, et al. Independent practice associations and physician‐hospital organizations can improve care management for smaller practices. Health Aff. 2013;32(8):1376‐1382. [DOI] [PubMed] [Google Scholar]
- 7. Bishop TF, Shortell SM, Ramsay PP, Copeland KR, Casalino LP. Trends in hospital‐ownership of physician practices and the effect on processes to improve quality. Am J Accountable Care. 2016;22(3):172. [PMC free article] [PubMed] [Google Scholar]
- 8. Rodriguez HP, McClellan SR, Bibi S, Casalino LP, Ramsay PP, Shortell SM. Increased use of care management processes and expanded health information technology functions by practice ownership and Medicaid revenue. Med Care Res Rev. 2016;73(3):308‐328. [DOI] [PubMed] [Google Scholar]
- 9. Bodenheimer T, Berry‐Millett R.Care management of patients with complex health care needs. 2009. https://www.rwjf.org/en/library/research/2009/12/care‐management‐of‐patients‐with‐complex‐health‐care‐needs.html. Accessed March 4, 2020. [PubMed]
- 10. Section 8: The Care Management Evidence Base. Agency for Healthcare Research and Quality, Rockville, MD. 2014. https://www.ahrq.gov/patient‐safety/settings/long‐term‐care/resource/hcbs/medicaidmgmt/mm8.html. Accessed March 4, 2020.
- 11. Farrell T, Tomoaia‐Cotisel A, Scammon D, Day J, Day R, Magill M.Care management: implications for medical practice, health policy, and health services research. 2015. https://www.rwjf.org/en/library/research/2009/12/care‐management‐of‐patients‐with‐complex‐health‐care‐needs.html. Accessed March 4, 2020.
- 12. Shi Y, Amill‐Rosario A, Rudin RS, et al. Health information technology for ambulatory care in health systems. Am J Manag Care. 2020;26(1):32‐38. [DOI] [PubMed] [Google Scholar]
- 13. Wagner AR.Effect of physician‐hospital financial integration on health outcomes and spending (Job Market Paper). 2016. https://pdfs.semanticscholar.org/f7de/61ed6e726c824e9a2ebae320a40398b258a2.pdf?_ga=2.8442870.211374152.1583334650‐1898796475.1583334650. Accessed March 4, 2020.
- 14. Defining Health Systems. Rockville, MD: Agency for Healthcare Research and Quality; 2017. https://www.ahrq.gov/chsp/chsp‐reports/resources‐for‐understanding‐health‐systems/defining‐health‐systems.html. Accessed August 1, 2020. [Google Scholar]
- 15. Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS‐HCC model. Health Care Financ Rev. 2004;25(4):119. [PMC free article] [PubMed] [Google Scholar]
- 16. McWilliams JM, Chernew ME, Landon BE. Medicare ACO program savings not tied to preventable hospitalizations or concentrated among high‐risk patients. Health Aff. 2017;36(12):2085‐2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Colla CH, Lewis VA, Kao L‐S, O’Malley AJ, Chang C‐H, Fisher ES. Association between Medicare accountable care organization implementation and spending among clinically vulnerable beneficiaries. JAMA Intern Med. 2016;176(8):1167‐1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chapter 4. Care models that deliver In:Long P, Abrams M, Milstein A, et al., eds. Effective Care for High‐need Patients: Opportunities for Improving Outcomes, Value, and Health. Washington, DC: National Academy of Medicine; 2017. [PubMed] [Google Scholar]
- 19. McCarthy D, Ryan J, Klein S. Models of Care for High‐need, High‐cost Patients: An Evidence Synthesis. New York, NY: The Commonwealth Fund; 2015. https://www.commonwealthfund.org/publications/issue-briefs/2015/oct/models-care-high-need-high-cost-patients-evidence-synthesis [PubMed] [Google Scholar]
- 20. 2015 Measure Information about the Hospital Admissions for Acute and Chronic Ambulatory Care‐sensitive Condition. Baltimore, MD: Centers for Medicare and Medicaid Services; 2017. https://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/PhysicianFeedbackProgram/Downloads/2015‐ACSC‐MIF.pdf. Accessed March 10, 2020. [Google Scholar]
- 21. Breslau N, Haug MR. Service delivery structure and continuity of care: a case study of a pediatric practice in process of reorganization. J Health Soc Behav. 1976;17(4):339‐352. [PubMed] [Google Scholar]
- 22. Elliott MN, Morrison PA, Fremont A, McCaffrey DF, Pantoja P, Lurie N. Using the Census Bureau’s surname list to improve estimates of race/ethnicity and associated disparities. Health Serv Outcomes Res Methodol. 2009;9(2):69. [Google Scholar]
- 23. Dubowitz T, Heron M, Bird CE, et al. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. Am J Clin Nutr. 2008;87(6):1883‐1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non‐randomized control group. Stat Med. 1998;17(19):2265‐2281. [DOI] [PubMed] [Google Scholar]
- 25. Austin PC. Optimal caliper widths for propensity‐score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150‐161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005;6(1):93‐109. [DOI] [PubMed] [Google Scholar]
- 27. Shwartz M, Restuccia JD, Rosen AK. Composite measures of health care provider performance: a description of approaches. Milbank Q. 2015;93(4):788‐825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Office of the National Coordinator for Health Information Technology . Office‐based physician electronic health record adoption, health IT quick‐stat #50. https://dashboard.healthit.gov/quickstats/pages/physician‐ehr‐adoption‐trends.php. Published January 2019. Accessed April 8, 2020.
- 29. Ridgely MS, Ahluwalia SC, Tom A, et al. What are the determinants of health system performance? Findings from the literature and a technical expert panel. Joint Comm J Qual Patient Saf. 2020;46(2):87‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160(1):48‐54. [DOI] [PubMed] [Google Scholar]
- 31. Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high‐need, high‐cost patients—an urgent priority. N Engl J Med. 2016;375(10):909‐911. [DOI] [PubMed] [Google Scholar]
- 32. Post B, Buchmueller T, Ryan AM. Vertical integration of hospitals and physicians: Economic theory and empirical evidence on spending and quality. Med Care Res Rev. 2018;75(4):399‐433. [DOI] [PubMed] [Google Scholar]
- 33. Direct Contracting Model Options. Baltimore, MD: Centers for Medicare & Medicaid Services; 2020. https://innovation.cms.gov/innovation‐models/direct‐contracting‐model‐options. Accessed April 8, 2020. [Google Scholar]
- 34. Ridgely MS, Duffy E, Wolf L, et al. Understanding US health systems: Using mixed methods to unpack organizational complexity. eGEMs. 2019;7(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author matrix
Appendix S1


