Abstract
Objective
We explore if there are ways to characterize health systems—not already revealed by secondary data—that could provide new insights into differences in health system performance. We sought to collect rich qualitative data to reveal whether and to what extent health systems vary in important ways across dimensions of structural, functional, and clinical integration.
Data Sources
Interviews with 162 c‐suite executives of 24 health systems in four states conducted through “virtual” site visits between 2017 and 2019.
Study Design
Exploratory study using thematic comparative analysis to describe factors that may lead to high performance.
Data Collection
We used maximum variation sampling to achieve diversity in size and performance. We conducted, transcribed, coded, and analyzed in‐depth, semi‐structured interviews with system executives, covering such topics as market context, health system origin, organizational structure, governance features, and relationship of health system to affiliated hospitals and POs.
Principal Findings
Health systems vary widely in size and ownership type, complexity of organization and governance arrangements, and ability to take on risk. Structural, functional, and clinical integration vary across systems, with considerable activity around centralizing business functions, aligning financial incentives with physicians, establishing enterprise‐wide EHR, and moving toward single signatory contracting. Executives describe clinical integration as more difficult to achieve, but essential. Studies that treat “health system” as a binary variable may be inappropriately aggregating for analysis health systems of very different types, at different degrees of maturity, and at different stages of structural, functional, and clinical integration. As a result, a “signal” indicating performance may be distorted by the “noise.”
Conclusions
Developing ways to account for the complex structures of today's health systems can enhance future efforts to study systems as complex organizations, to assess their performance, and to better understand the effects of payment innovation, care redesign, and other reforms.
Keywords: health care organization, health services research, health system, hospital‐physician affiliation, integrated delivery system, qualitative research, vertical integration
What is Already Known on this Topic
Policymakers believe that integrating separate health care organizations into health systems will improve the coordination, quality, and efficiency of care.
Studies assessing health system performance have found inconsistent outcomes regarding cost, quality, and patient experience.
Most such studies use “health system” as a binary variable (in a system/not in a system) or characterize systems using simple attributes such as size and ownership that are readily available in secondary data.
What this Study Adds
We use in‐depth interview data to examine how contemporary health systems are organized and function.
We find that the systems vary across dimensions of structural, functional, and clinical integration that are linked to performance in empirical literature.
Appropriately characterizing the complexity of health systems—beyond a binary categorization—can support future efforts to measure a broader range of characteristics that may influence health system performance.
1. BACKGROUND
The Affordable Care Act of 2010, with its emphasis on integration and coordination of care, is arguably responsible for the current wave of health care consolidation sweeping through the health care industry. 1 Regulatory changes, rapid technological change, and market dynamics are driving dramatic transformation in the way health care is organized and financed. The introduction of value‐based payment has increased focus on the ability of hospitals and physicians to coordinate care across a range of primary and specialty providers and across settings, and to take on financial risk—pushing hospitals and physicians to consider joining or forming vertically integrated health systems. At the same time, policymakers and payers are pushing to drive improvements in the performance of health systems and to understand what system characteristics are related to performance. Thus far, indicators of greater efficiency and improved quality have lagged behind the promises of consolidation proponents. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12
As Cohen and colleagues point out, we must be able to identify and describe health systems to answer policy‐relevant questions related to their performance. 13 In their discussion, the authors describe multiple secondary data sources that are available to help identify and map hospitals and physician organizations to systems. The majority of studies to date use secondary data to identify hospitals and physicians and apply algorithms to associate them with systems. But health systems are complex organizations. 14 In this analysis, we explore if there are ways to characterize health systems not already revealed by secondary data that could provide new insights into performance differences. Specifically, we argue that qualitative data can be used to craft a rich portrayal of health system diversity on which to base a more nuanced understanding of the characteristics and composition of modern health systems. That knowledge, in turn, can be used to refine measurement approaches to better understand the effects of payment innovation, care redesign, and other reforms.
We have an opportunity to address this complexity in the context of a study initiated by the RAND Center of Excellence on Health System Performance under the Agency for Healthcare Research and Quality's (AHRQ) Comparative Health System Performance Initiative (CHSP). AHRQ funded three Centers of Excellence in 2015 to identify, map, and track health systems and to identify the characteristics of high‐performing systems. 15 As part of the CHSP work, our Center took a “deep dive” into the operations of health systems through extensive interviews with the c‐suite executives who make the strategic and operational decisions. In this paper, we focus on examining health system variation in terms of structural, functional, and clinical integration.
1.1. Conceptual model
In reporting our findings, we use a conceptual framework (Figure 1) developed by our colleagues that identifies five distinct types of integration within and across health care organizations. 16 The framework focuses on how systems are structured and governed, what people who work in the system believe and how they behave, and activities intended to integrate patient care into a single coordinated process within the system. We chose this model because, while there are many different ways to characterize health systems, we wanted to focus on those characteristics that might prove to be meaningful with regard to performance differences.
FIGURE 1.
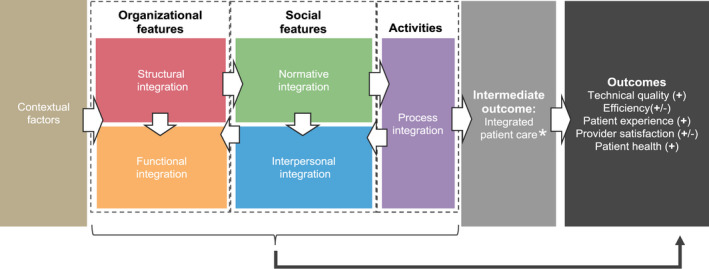
Hypothetical relationships are depicted in the model using arrows that move from left to right. The five types of integration depicted in the model (structural, functional, normative, interpersonal and process integration) are hypothesized to effect intermediate and ultimate outcomes. From Singer SJ, Kerrissey M, Friedberg M, Phillips R. A Comprehensive Theory of Integration. Med Care Res Rev. 2020;77(2):204, Sage Publications, Inc. (used with permission) [Color figure can be viewed at wileyonlinelibrary.com]
We report findings on three types of integration that Singer and colleagues link to performance, based on their review of the empirical literature:
Structural integration (physical, operational, financial, or legal ties among operating units within a system)
Functional integration (formal, written policies, and protocols for activities that coordinate and support accountability and decision making among operating units)
Process (or clinical) integration (actions or activities intended to integrate patient care across people, functions, activities, and operating units within the system). In our discussion, we refer to this as clinical integration.
Structural and functional integration are under the direct control of system executives. Our intent was to understand the kinds of strategic decisions they were making, why they made them, and how they saw their decisions affecting their goals for their systems. Understanding the organizations that make up the systems and the extent to which systems are structurally and functionally integrated is a vital starting point for understanding whether process/clinical integration is happening within systems, how it is happening, or indeed whether it is even possible. Singer's model allows for the possibility that health care organizations may be structurally and functionally integrated and yet not delivering integrated care to patients. 17
Singer's model also identifies two additional types of integration—normative and interpersonal. Normative integration refers to sharing a common culture; interpersonal integration refers to collaboration or teamwork. Executives can speak to these issues, but to appropriately explore normative and interpersonal integration we would want to include information from middle managers and frontline staff. Such an expansion was beyond the study's scope.
1.2. Study objectives
Our objective was to collect data disclosing the contours of multilayered systems; account for their complexity; and reveal how organizational, functional, and clinical integration could affect delivery of care and therefore performance. As Shortell notes, secondary data are needed to track temporal changes in costs, quality, and patient experience, but evidence is also needed about “factors that might be associated with success.” 18
2. METHODS
2.1. Sampling
Using secondary data sources, we identified the system affiliations of all physician organizations (POs) publicly reporting performance data in four states that each host a health care measurement and improvement collaborative. From those states, we selected a purposive sample of 24 health systems to achieve variability on important system attributes (eg, size and performance) (see Appendix S1). If the sampled system had more than one affiliated PO (ie, medical group, independent practice association, faculty practice, or medical foundation), we selected a single PO for data collection.
2.2. Data collection, coding, and analysis
Details of our data collection, coding, and analysis are provided in Appendix S2. Briefly, to study the health systems, we organized “virtual” site visits, comprised of 60‐90 minutes telephone interviews with 5‐8 senior executives in each system. 19 Interview topics were informed by a literature review and modified Delphi panel process. 20 We tailored interview protocols to each executive's sphere of responsibility. Topics included market context; health system origin; organization, governance and management of the system and its hospitals and POs; and the influence of the system on hospital and PO operations.
We coded all interviews thematically using Dedoose, 21 a web platform for analyzing qualitative data that facilitates team‐based data coding. We programmed a codebook (see Appendix S2) based on the main interview questions. After a multistage process of testing, adding, and refining codes, two experienced qualitative researchers independently coded transcripts for the first four site visits (20% of the total interviews) and achieved high interrater reliability (pooled kappa of 0.84). They then independently coded all remaining transcripts, spot checking each other's coding to ensure consistency. The codebook was updated to account for inductively derived codes that illustrate how systems are structured, governed, and operate. 22 We used the coded data to develop detailed memos 23 on each of the 24 systems—and a set of cross‐site memos that incorporated emerging insights—that were used to compare and contrast the organization and governance of health systems and to identify aspects of structural, functional, and clinical integration.
2.3. Limitations
The findings we report may not be generalizable to all US health systems. Our data come from a convenience sample of four states with prior engagement in public reporting and quality improvement collaboratives. The collaboratives in these states are ones that agreed to participate by providing performance data and helping to recruit health systems. Our selection of systems within those states was purposive and nonrandom, based on select attributes such as size and performance.
Our study presents data from the point of view of executives and does not attempt to capture the frontline perspective. We recognize the value of the frontline perspective, but focused our interviews on obtaining high‐level information on organizational dynamics and strategic choices. We did look across respondents within a system for areas of agreement and disagreement.
Finally, we use self‐report data, which may suffer from social desirability bias; however, executives knew that the identities of the systems would be blinded for reporting purposes, so we believe the risk is minimal.
3. RESULTS
3.1. Descriptive data
Table 1 provides key characteristics of the 24 systems in our sample. We identified four basic organizational types: nonprofit; quasi‐public; academic; and a variant of academic health systems that we call academic affiliation agreements (a health system incorporating parts of a university health system and parts of a nonprofit health system, operating under a joint governance arrangement). The systems range from serving a single county to serving multiple counties across three states. Seven of the 24 are multistate systems. Most serve some rural communities along with urban or suburban centers, but a few are almost exclusively rural (eg, Cedar Healthcare, Aspen Health System), comprised of critical access hospitals and associated clinics. Relationships between health systems and their hospitals and POs vary as do the number and types of acute and postacute services associated with each system.
TABLE 1.
Key characteristics of 24 health systems across 4 US States
| Health system (Pseudonyms) | System characteristics | System affiliations | Risk assumption | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Organization type | Region served | HS is a single legal entity | Number of hospitals | Number of POs | PO practice type | Enterprise‐wide EHR | Clinically integrated network | Other services | Health plan | ACO participation | At‐risk contracting | |
| Ash Healthcare | Academic | Single county | No | 2 owned | 1 | Medical foundation (medical group and IPA) | Single instance ‐ one vendor | No | Yes | No | Yes | Yes (small %) |
| Aspen Health System | Nonprofit | Multiple counties within a state | Yes | 7 owned | 0 | Employment | Single instance ‐ one vendor | Yes (all employed physicians are in the CIN) | Yes | No | Yes | Yes (small %) |
| Azalea University Health System | Academic | Multiple counties within a state | No | 3 owned, 1 JV, 7 affiliated | 1 | Faculty practice | Single instance ‐ one vendor | Yes | Yes | No | Yes | Yes (small %) |
| Beech Health | Nonprofit | Multiple counties within a state | No | 5 owned | 1 | Medical foundation (medical group and IPA) | Single instance ‐ one vendor | No | Yes | Yes | Yes | Yes (half) |
| Birch Health | Academic (affiliation agreement) | Multiple counties within a state | No |
3 owned 2 affiliated |
2 | Medical group and faculty practice | Single instance ‐ one vendor | No | Yes | Yes (JV) | Yes | Yes (small %) |
| Cedar Healthcare | Nonprofit | Multiple counties across three states | Yes |
2 owned 1 managed |
0 | Employment | Inpt.. and ambulatory use different vendors | No | Yes | No | Yes | Yes (small %) |
| Chestnut Clinics | Nonprofit | Multiple counties across 3 states | Yes (with subsidiaries) |
49 owned 2 JV |
3 | Medical foundation (medical group and IPA) | Single instance ‐ one vendor | Yes w/partners | Yes | Yes, JV | Yes | Yes |
| Cypress Health System | Nonprofit | Multiple counties across two states | Yes | 8 owned | 1 | Employment | Single instance ‐ one vendor | Yes (all employed physicians are in the CIN) | Yes | Yes, JV | No | Yes (half) |
| Dogwood HealthCare | Nonprofit | Single county | No |
3 owned 2 affiliated |
2 | Medical foundation (medical groups) and IPA | Inpt.. and ambulatory use different vendors | No | Yes | Yes | Yes | Yes (large %) |
| ElmCare | Nonprofit | Multiple counties within a state | Yes (with subsidiaries) |
2 owned 1 JV |
1 | Medical foundation (medical groups) | Single instance ‐ one vendor | Yes w/partners | Yes | No | Yes | Yes (small %) |
| Hickory Healthcare | Nonprofit | Multiple counties within a state | Yes (with subsidiaries) | 4 owned, 1 JV, 3 affiliated | 1 | Employment | Inpt.. and ambulatory use different vendors | No | Yes | Yes | Yes | Yes (small %) |
| Juniper Health | Nonprofit | Multiple counties within a state | No | 2 owned | 0 | Employment | Single instance ‐ one vendor | No | Yes | No | Yes | Yes (small %) |
| Laurel Health System | Nonprofit | Part of one county | No | 3 owned | 2 | Medical group and IPA | Single instance ‐ one vendor | No | Yes | No | No | Yes (half) |
| Linden Health System | Nonprofit | Multiple counties within a state | No | 2 owned | 1 | Medical foundation (medical groups and IPA) | Inpt.. and ambulatory use different vendors | No | Yes | Employees only | No | Yes |
| Magnolia University Health System | Academic | Multiple counties within a state | No | 5 owned | 2 | Faculty practice and medical group | Single instance ‐ one vendor | Yes w/partners | Yes | Employees only | Yes | Yes (small %) |
| Mahogany University Health System | Academic | Multiple counties within a state | No | 1 owned | 1 | Faculty practice and employment | Single instance ‐ one vendor | No | Yes | Yes, JV (but plans to drop nonemployees) | No | Yes (small %) |
| Maple Health System | Nonprofit | Multiple counties within a state | No | 8 owned | 2 | Employment | Single instance ‐ one vendor | Yes | Yes | No | Yes | Yes (small %) |
| Oak Clinics | Academic | Multiple counties across several states | Yes (HS is a subsidiary of academic enterprise) | 17 owned | 0 | Employment | More than one instance (one vendor) | No | Yes (halfway house only) | No | No | Yes (small %) |
| Olive Health | Quasi‐public | Two counties within a state | Yes | 2 owned | 1 | Employment | Multiple EHR vendors within a single setting (inpt.. or ambulatory | Yes w/partners | Yes | No | Yes | Yes (small %) |
| Pine Healthcare | Quasi‐public | Single county | Yes | 1 owned | 0 | Employment | Single instance ‐ one vendor | No | Yes | No | Yes | Yes (small %) |
| Sequoia Health | Academic (affiliation agreement) | Multiple counties within a state | No | 13 owned | 2 | Faculty practice and employment | More than one instance (one vendor) | Yes | Yes | Yes (involves only one of the partners) | Yes | Yes (large %) |
| Spruce Health Care | Nonprofit | Multiple counties across two states | Yes (with subsidiaries) | 12 owned | 1 | Employment | Single instance ‐ one vendor | Yes (all employed physicians are in the CIN) | Yes | Yes, JV (launching) | Yes | Yes (small %) |
| SycamoreCare | Nonprofit | Multiple counties across two states | Yes |
5 owned, 1 affiliated 1 JV |
1 | Employment | Single instance ‐ one vendor | No | Yes | Yes | Yes | Yes (large %) |
| Willow Clinics | Nonprofit | Multiple counties across two states | No | 2 owned | 0 | Employment | Single instance ‐ one vendor | Yes w/partners (all employed physicians are in the CIN) | Yes | Yes, JV (launching) | Yes | Yes (small %) |
HS refers to health system. A quasi‐public corporation is a private company that is supported by the government with a public mandate (and public funding) to provide a given service. Many quasi‐public corporations began as government entities (eg, safety net providers) but have since become nonprofit entities. Academic affiliation agreement refers to a health system that incorporates parts of a university health system and a nonprofit health system operated under a joint governance arrangement. Hospitals are a count of acute, general hospitals and exclude behavioral health faculties. Owned refers to hospitals owned and operated by the HS. Affiliated refers to hospitals managed by the HS under affiliation agreements (such as MOUs, management contracts, joint provision of service agreements). JV refers to jointly owned and operated or managed. PO refers to physician organizations such as medical groups, IPAs, medical foundations and faculty practices. Medical foundation refers to 1206(l) foundations in California. A mark of "0" in the PO column indicates that the HS is a single legal entity providing ambulatory physician services without separate, identifiable PO entities. EHR refers to electronic health record. Enterprise‐wide refers to an EHR that all (or almost all) affiliated providers use. Single instance means that there is a single copy of content that the multiple users or computers share. More than one instance refers to a situation in which the health system uses a single vendor EHR but not a single instance of the content. CIN refers to whether the health system offers a clinically integrated network to payers or participates with another HS or hospital to offer a CIN to payers. CIN w/partners refer to participation in a CIN sponsored by two or more HS. Other services refer to acute care facilities (such as ambulatory surgery centers), diagnostic and medical services (such as imaging, laboratories, pharmacy), and postacute care services (such as SNF, home health, and hospice) that are owned, operated or provided through a joint venture. Health plan is a health insurance company either owned by a health system or through a JV. Employees only refer to a self‐insured health plan. ACO refers to whether the health system offers an ACO product to payers or participates in an ACO network offered by another entity. At‐risk contracting is defined as percent of book of business at global (professional, hospital, and pharmacy), full (professional and hospital), or partial (professional services only) risk. Source: health system interview and survey data collected by authors. Information is current as of the date of the site visit (2017‐2019).
The systems also differ in maturity. At one end of the continuum is a system that has not onboarded a new hospital acquisition for 30 years (Dogwood HealthCare); at the other end are systems that were mid‐merger/acquisition at the time of data collection (eg, Juniper Health). (We use pseudonyms here and throughout the paper, in keeping with IRB requirements).
3.2. Key findings
3.2.1. Structural Integration
Below we describe the organizational, legal, financial, and informational ties among operating units within the system, starting with organizational structures.
Organizational/legal structures
Single versus multi‐entity structures: If complexity exists on a continuum, at one end is Cedar Healthcare, a single legal organization that operates hospitals and clinics (See Figure 2). At the other end are complex systems such as Cypress Health System, which operates multiple hospitals (a flagship hospital and multiple critical access hospitals) and a postacute care division; it provides its ambulatory care through a clinically integrated network (CIN) 24 comprised of its own employed physicians (practicing in Cypress‐owned clinics) as well as an additional 100 specialty physicians practicing in small medical groups in the community (see Figure 3). There are multiple systems in our sample with complexity that rivals Cypress Health System. We expected complexity in our sample, but the amount of complexity within systems and lack of pattern across systems was surprising.
FIGURE 2.
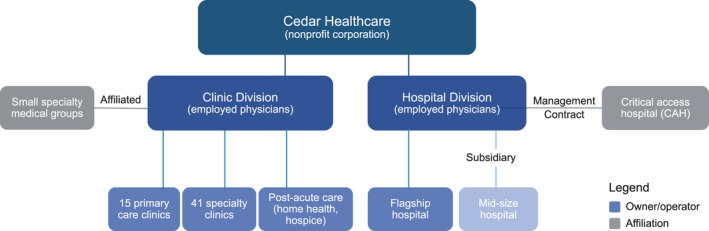
Simple Health System Organizational Structure [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 3.
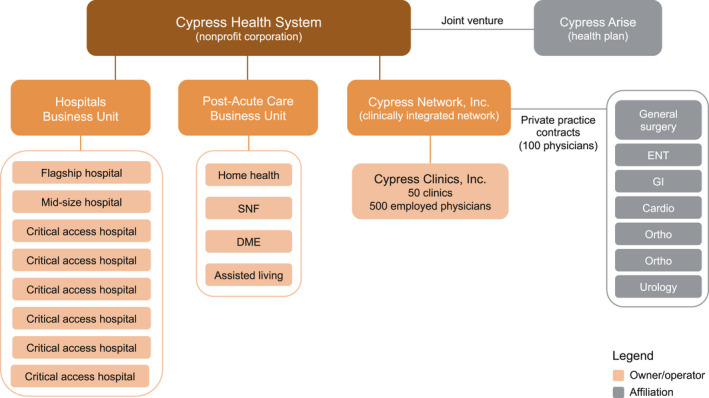
More Complex Health System Organizational Structure [Color figure can be viewed at wileyonlinelibrary.com]
Hospitals: The number of hospitals associated with systems ranges from 1 to 51; the relationships between systems and their hospitals vary, including ownership (alone or through joint venture), management, and affiliations under a wide variety of contractual relationships. Ownership, however, does not always indicate an intention or the ability to integrate. Some executives report having greater influence over affiliates that have been in the system longer, but time was not the only factor. For example, Oak Clinics acquired hospitals in the 1990s but operated as a “holding company” until they decided to move toward system integration and standardization in 2010. By contrast, Dogwood's managed hospitals are integrated into their system in similar ways as their owned hospitals.
Physician organizations: The structural relationships between health systems and POs are highly complex. We identified nine types of physician groupings in an earlier analysis. 19 Many of the systems incorporate multiple approaches, and the operational ties between the systems and their POs vary (see Table 1). A number of systems have both affiliated medical groups that employ physicians and IPAs (independent practice associations) that may operate under different governance arrangements (eg, Laurel Health System, Ash Healthcare). Aspen Health System physically co‐locates some of its POs with its hospitals. AMC‐based systems (eg, Azalea, Magnolia University Health System) staff their hospitals with a combination of university medical school faculty, employed physicians, and affiliated community‐based physicians. The systems also vary in the extent to which affiliated POs are exclusive to the system. Differences in system/physician relationships often relate more to history, mission, and market realities than to the optimal organizational structure executives might have chosen had they begun building their systems today.
Acute and postacute care services: All 24 systems own, operate, or manage acute and postacute care services. These range from a single halfway house (Oak) to systems with numerous health care entities, including ambulatory surgery centers; home health agencies; rehabilitation, hospice, skilled nursing facilities; and behavioral health services. In many cases, these ancillary services are fully owned, but some are joint ventures.
Health plans: Thirteen of the 24 systems have, or were preparing to launch, a health insurance product. Some of these exist to self‐insure employees, but the majority are products offered to the larger market—either by the system alone or in partnership with another entity (an insurer or another system). Some are re‐entering the insurance arena after previous insurance offerings were closed (Spruce Health Care, Willow Clinics).
Single signature contracting
As Casalino 25 points out, the ability for systems to take on risk is not an end in itself but indicative that a provider network is sufficiently integrated to achieve significant efficiencies. Financial integration across hospitals and POs within a system gives physicians incentives to cooperate in controlling costs and improving quality. According to the executives in our systems, key to financial integration is establishing a common contracting signatory (eg, Sequoia Health, Maple Health System, Linden Health System, Cedar, Aspen, Cypress, Dogwood). Contracting on behalf of the entire system increases leverage with payers and reduces the need for each acquired or affiliated entity to negotiate and manage its own contracts (also reducing payer burden). A system's larger scale, incorporating multiple care settings, better positions it to take on risk‐based contracts. Executives in our systems discussed variability in how contracting works in their organizations. In only one system (Cypress) are all physicians included under a single contracting signature for its entire book of business. “A lot of payers didn't want to deal with us because we had so many players and they all had to have separate contracts…we found if we had one signature, one contract…we'd be much more efficient and friendly to the marketplace (Cypress Health System, CFO).
Executives reflect the need to grow their systems, increase contracts, and perform under risk‐based contracting, but taking on risk is largely aspirational. All of the executives report that their system has experience with value‐based payment; however, the majority also report that fee‐for‐service remains, by far, the predominant payment model (see Table 1). This is true in spite of state‐level efforts at health reform, in spite of changes borne of the ACA, and in contradiction of proclamations heralding the advent of the value‐based payment world.
Health IT infrastructure
Chief information officers describe an enterprise‐wide EHR using a single instance of a vendor product as the “gold standard” for EHRs. Enterprise‐wide refers to an EHR that all (or almost all) system providers use. Single instance means that there is a single copy of content that the multiple users or computers share. Executives in 17 of the systems report that they have such a system for hospitals and employed physicians (see Table 1), except in the case of a fairly recent merger/acquisition that has extended the system to a new geographic base (Juniper). Other executives report that they have not yet been able to move all hospitals or physicians to the same EHR system. For affiliated private physician practices, such as those in CINs, many systems offer assistance with purchasing and technical support, but do not mandate purchase or use of the system's EHR. In other cases, they require affiliating practices to use the system's EHR or acquire and use an interoperable system (ElmCare).
Observations on structural integration
Five observations about structural integration emerged from our analyses of the interviews.
First, structure is often historically driven rather than purposive. Systems adapt to current and anticipated future needs based on their pre‐existing organizational structures.
Second, “owned” does not necessarily mean operating like a system. Structural integration is a process; and it is important to understand that most systems are on a glide path toward integration. One CEO (ElmCare) calls his system a federated model. He describes concentric circles with fully owned facilities and a medical foundation at the core and joint ventures and independent physician practices at the periphery. He also reports that the system is investing in health IT (to help ensure continuity of care) and in patient‐facing IT applications (to keep patients engaged).
Third, multiple organizational models for physicians continue to exist (medical groups, IPAs, PSAs) because each model offers advantages and disadvantages for systems and physicians. Less control may be an issue for systems, but they need physicians to fill out their networks and many physicians “fiercely” guard their independence. Systems have other ways to influence physician practice, such as compensation structures and performance reporting.
Fourth, increased market competition (or the perception of competition) motivates executives to rapidly build, buy, or affiliate to preserve or increase their market share. A dominate strategy post‐ACA is to bring private practice physicians into the system through development of CINs. 24 As described by the CEO of one of the academic medical systems, “We're not doing their billing, we're not recording their revenue, we're not running their practices, we're really just affiliating with them to provide a network of physicians to our patients“ (Azalea University Health System, CFO). These relationships, which are a significant aspect of system development, are largely undetectable in secondary data because they are not ownership/management relationships.
Fifth, involvement in (or planning future involvement in) value‐based payment arrangements is motivating system leaders to move toward approaches that allow them to fully “own” lives. As one executive summarized: “It's not about ‘heads in beds’ anymore, it's about how many lives do you control for the continuity or continuum of care in the market?” (Laurel Health System, President, and CEO).
3.2.2. Functional integration
Functional integration is the extent to which the system is characterized by centralized control versus autonomy for hospitals and POs within the system. Functional integration can be effectuated through “hard” (centralized decision making) or “soft” (incentives, branding) mechanisms. We found that systems that directly own entities are not necessarily more functionally integrated than those that affiliate with other organizations and private practice physicians to fill out their networks.
Business functions
Executives in all 24 systems cite integration of business functions as a way to promote system integration while increasing economies of scale. Merging back‐office functions (regulatory compliance, accounting, human resources, IT support, procurement/supply chain) are first steps. Executives also see creating data warehouses and centralizing data analytic capabilities as key. Having access to EHR data for all patients allows systems to conduct population health management centrally (ie, stratifying patients into groups to link them to appropriate care). Some systems have completely centralized this function (eg, Azalea, Spruce), and others are transitioning to it (eg, Hickory Healthcare).
Planning and budgeting
A second aspect of functional integration is centralizing decisions about planning and budgeting at the system level. Systems vary in how much autonomy individual hospitals or other provider groups retain in making capital planning decisions, and executives note the need to balance the system's goal for centralization with local needs. Many systems maintain strong central control over entities within the system (eg, Mahogany University Health System, Willow, SycamoreCare). Recent mergers and acquisitions have required some systems to redesign their decision making processes to permit more local control (Juniper, Maple). Some executives maintain that local control allows individual hospitals to react to local market conditions or to incorporate local cultural norms (Pine Healthcare, Chestnut Clinics, Aspen).
Physician employment and compensation
A key factor in pursuing functional integration is employing physicians or establishing other compensation methods to enlist provider cooperation in controlling costs and improving quality. All systems employed some physicians either directly or through medical foundations. Roughly three‐quarters have affiliated providers as well. But not all systems are able to or wish to employ all physicians. Rather, systems have pursued affiliation approaches such as contracting with IPAs and sponsoring CINs. The general goal is to capture referral pathways and enforce clinical performance metrics. Compensation for physicians in CINs may include some risk‐based payments for meeting quality benchmarks or quality incentive payments (eg, ElmCare).
Branding
The few executives who mentioned branding emphasized its importance to integration. This includes harmonizing the physical appearance of clinic locations, changing clinic names, and using common advertising platforms (Dogwood, Cypress, Spruce). Two system executives describe this effort as a way to synchronize the look and feel of various care environments for patients (Chestnut, Pine). Some systems try to promote system integration behind the scenes (SycamoreCare) while allowing acquired hospitals to retain aspects of their original brand.
Observations on functional integration
Executives had differing views on centralized versus decentralized decision making. Most reported that they had centralized back‐office functions fairly early and most were (at least) aspirational about the need for reducing variation in clinical care across their hospitals and POs; not all agreed on how and to what extent there should be any “local” control over decision making. The CEO of one of the quasi‐public systems explained, “we try to push as much of the decision making down to the frontline as possible…[consistent with organizational goals], we allow a considerable amount of discretion and freedom to determine where the dollars are pinpointed" (Pine Healthcare CEO). Others described the prioritization of some issues over others as coming from “the bottom up” (Magnolia University Health System).
Health system executives do not agree on the benefits of functional integration or ways to get there. Some saw it as potentially curtailing the ability to act independently when necessary and were concerned about the “inordinate amount of time and effort” that would be involved (Aspirus). A system may adopt one strategy for functional integration but carry it out very differently across the system's hospitals and POs. Several executives highlighted the amount of time, labor, and commitment it takes to functionally integrate: “We have grown exponentially… but we're now stabilizing and trying to grow into our skin” (Olive Health CFO). System leaders consistently report that taking on risk‐sharing accelerates functional integration.
3.2.3. Clinical Integration
Singer and colleagues define clinical integration as a set of activities the system initiates to integrate patient care across settings. Casalino (2006) 25 explains that clinical integration could be evidenced by the presence of organized processes to control costs and improve quality and by the significant investment of monetary and human capital in these processes. Based on our interviews, we identify four ways that systems are improving the consistency of care across operating units, building on capacity developed through structural or functional integration.
“Hard‐wiring” clinical processes
Health systems in our sample are promoting care integration through EHRs. Most systems viewed a single EHR as a way to “hard wire” critical clinical processes into the system. Executives report using the EHR to standardize care and reduce errors through clinical workflows, order sets, clinical care protocols, and decision support algorithms. An enterprise‐wide EHR allows systems to integrate new evidence into practice uniformly and to reduce variation in care.
Standardizing service lines
Executives cite establishing standardized service lines as a way to integrate patient care across settings. One executive (Cypress) described this effort as “bottom up,” starting with one or two service lines (eg, cardiology and orthopedics); the system is now trying to replicate the process across other service lines and then to standardize clinical services across all settings. For other systems, the process was a “top down” push to reorganize care delivery (eg, Hickory). Some executives noted that they were moving to create “centers of excellence” within their system for certain care lines, so that most of the volume for the particular service line (eg, oncology or cardiology) would be directed to only one of the system's hospitals (eg, Birch Health, Olive Health).
Redesigning care delivery
Some systems are changing care delivery in more profound ways. For example, executives in some systems (eg, Aspen, Oak, Linden, Magnolia) said they are moving toward the delivery of primary care through teams, which may comprise only physicians or include other health professionals (eg, nurses, pharmacists). Team‐based care often requires changing guidelines for providing and supervising care.
Onboarding clinicians
Some systems have developed specific “onboarding” protocols to more effectively integrate hospitals and POs they acquire. Oak Clinics has centralized onboarding—all physicians joining the system are employees, they participate in a standardized orientation, and return for updates early in their tenure. Dogwood executives estimate that a hospital onboarding takes 18 months to 3 years. Executives explained that a lack of cultural integration of the new providers, particularly with different hospitals purchased over time, can make aligning system goals difficult (eg, Aspen, Juniper, Spruce). Some executives focus on managing care tightly; others emphasized the need for balance—mindful that their systems need to attract and retain physicians to fill out their networks.
Observations on clinical integration
For most of the executives, standardizing care remains the next frontier. In the words of one CQO (Sequoia Health), “to know that a patient is going to get the same level of care at any touch point in our organization—we don't have that and that would be the ultimate goal.” Executives were particularly concerned about care across physicians in IPAs or CINs. As health systems populate their networks with private practice physicians, they cede substantial control over providers who are not exclusive to their system.
Academic medical systems that host both faculty physician groups and other medical groups and/or IPAs face a similar challenge: how to integrate the academic side of medicine (with its own rules and procedures) with community physicians so that neither group feels like the other took over the practice of medicine (Sequoia Health). Cultural change is difficult especially when physicians are moving from a “physician‐controlled climate to one [in which] physicians have a great deal of input, but not necessarily control” (Hickory Healthcare CMO).
4. DISCUSSION
In our sample of 24 systems, we found many types of structural integration, including a variety of ownership and management arrangements, joint ventures, and affiliation agreements. There are many ways to legally structure these arrangements, but the goal is to create a centralized structure capable of managing patients across the continuum of care.
One of the most important aspects of functional integration is employing physicians and controlling compensation to align financial incentives with the system for quality and efficiency goals. We found a wide variety of arrangements between health systems and physicians. Centralizing business functions, providing for an enterprise‐wide health IT system, and having a single contracting signatory were viewed as foundational. Building economies of scale on centralized business functions, providing “fingertip” access to a complete clinical record, and centralizing contracting generate efficiencies for the system and allow physicians and other clinicians to spend more time “practicing at the top of their license” and less time managing the business of providing care.
Executives describe clinical integration as more difficult to achieve but essential for competing in the world of value‐based payment. Currently, risk‐based contracts represent only a small portion of the total book of business for most systems, but all executives view risk‐based contracting as the future. Many noted that they are trying to build infrastructure to take on risk‐based contracts. Managing the continuum of care and managing population health require tools such as an enterprise‐wide EHR or, at the least, interoperability across existing EHR platforms.
Executives in several systems cautioned that there are constraints to integration. For example, they felt there were limits to how far variation could be reduced without negatively impacting cultural diversity. Some emphasized a trade‐off between standardization and provider autonomy.
4.1. Implications
Building from Singer's conceptual framework, we examined structural, functional, and clinical integration across a sample of 24 health systems. Some of the aspects of integration we discuss have already received attention in the literature—others (such as balancing the need for centralized versus decentralized decision making, the role of branding and organizational identity, and cultural integration of new providers) deserve further exploration.
We found important variation across health systems that can and should be documented and measured systematically. Studies that treat “health system” as a binary variable (in a system/not in a system) may be inappropriately “lumping together” for analysis health systems of very different types; at different levels of maturity; and at different stages of structural, functional, and clinical integration. As a result, a “signal” indicating outcomes from these systems may be distorted by the “noise.”
Our observations are in keeping with those of commentators for BMC Medicine who note that “complexity is much talked about, but sub‐optimally studied in health services research.” 14 They argue that because complexity is a feature of health systems (not just a feature of interventions), and because systems are dynamic, conventional ways of study need to give way to a more pluralistic approach—appreciating the detail rather than attempting to strip away the layers of complexity to get to artificial simplifications. In their words, “there are no universal solutions to the challenges of complex systems, nor is there a set of universal methods that will bring us closer to the truth.”
Qualitative work is useful in looking at the how and why of phenomena, to explore unstudied areas, and to unpack assumptions to see how well they fit the current research models and practices. But to operationalize these observations for purposes of analysis will require collaboration with those who have expertise in variable development and measurement. That may be the next logical step to further this type of analysis.
It might also be useful to be able to classify health systems in some simple way that indicates their degree of integration. However, the results of our deep dive into health system operations underscores our concern that development of such a classification system may not be realistic. We have documented variation among systems, not just in ownership type, but in aspects of “system‐ness” that “matter” for the production of care. We have identified intra‐system as well as cross‐system variability—variability that matters in terms of whether good care in one part of the system predicts good care across the entire system. The question of intent also surfaces: do all systems intend to integrate or are some content to be holding companies? Maturity is also a factor: how long after a merger/acquisition could one expect to see clinical integration? Is there such a thing as “too big to succeed”? While size may be positively associated with access to capital and additional resources, how much of those additional resources will need to be spent on administering a sprawling system, including those that cross state lines?
Do health systems perform better on meaningful measures than health care organizations that are unaffiliated? There is not enough evidence at this stage to answer that question. There is even less evidence to determine whether particular types of systems are more likely to perform well. As our analysis illustrates, addressing the performance issue requires more detailed information about health system integration than is often readily available. Simplistic conceptualizations of health systems, using dimensions such as ownership and size, do not capture the diversity of structural, functional, and clinical integration that we identified. A more nuanced conceptualization is necessary, as are research designs that are likely to generate meaningful findings about what drives performance.
CONFLICTS OF INTEREST
The authors report no conflicts of interest.
Supporting information
Supplementary Material
Appendix S1
Appendix S2
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: This work was supported through the RAND Center of Excellence on Health System Performance, which is funded through a cooperative agreement (1U19HS024067‐01) between the RAND Corporation and the Agency for Healthcare Research and Quality. The content and opinions expressed in this publication are solely the responsibility of the authors and do not reflect the official position of the Agency or the US Department of Health and Human Services.
Ridgely MS, Buttorff C, Wolf LJ, et al. The importance of understanding and measuring health system structural, functional, and clinical integration. Health Serv Res. 2020;55:1049–1061. 10.1111/1475-6773.13582
REFERENCES
- 1. Swisher AW, Gordon CH. The importance of clinical integration to provider networks under the affordable care act. J Health Life Sci Law. 2014;8(1):1‐28. [Google Scholar]
- 2. Baker LC, Bundorf MK, Kessler DP. Vertical integration: hospital ownership of physician practices is associated with higher prices and spending. Health Aff (Millwood). 2014;33(5):756‐763. [DOI] [PubMed] [Google Scholar]
- 3. Beaulieu ND, Dafny LS, Landon BE, Dalton JB, Kuye I, McWilliams JM. Changes in quality of care after hospital mergers and acquisitions. N Engl J Med. 2020;382(1):51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Casalino LP, Ramsay P, Baker LC, Pesko MF, Shortell SM. Medical group characteristics and the cost and quality of care for Medicare beneficiaries. Health Serv Res. 2018;53(6):4970‐4996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gaynor M, Town R.The impact of hospital consolidation. Robert Wood Johnson Foundation. https://www.rwjf.org/en/library/research/2012/06/the‐impact‐of‐hospital‐consolidation.html. Published 2012. Accessed April 9, 2020
- 6. Kacik A.Monopolized healthcare market reduces quality, increases costs. Modern Healthcare. https://www.modernhealthcare.com/article/20170413/NEWS/170419935/monopolized‐healthcare‐market‐reduces‐quality‐increases‐costs. Published 2017. Accessed April 9, 200
- 7. Kaul A, Prabha KR, Katragadda S.Size should matter: Five ways to help healthcare systems realize the benefits of scale. PricewaterhouseCoopers, Strategy&. https://www.strategyand.pwc.com/media/file/Size‐should‐matter.pdf. Published 2016. Accessed April 9, 2020
- 8. Machta RM, Maurer KA, Jones DJ, Furukawa MF, Rich EC. A systematic review of vertical integration and quality of care, efficiency, and patient‐centered outcomes. Health Care Manage Rev. 2019;44(2):159‐173. [DOI] [PubMed] [Google Scholar]
- 9. National Council on Compensation Insurance (NCCI) . The impact of hospital consolidation on medical costs. National Council on Compensation Insurance. https://www.ncci.com/Articles/Pages/II_Insights_QEB_Impact-of-Hospital-Consolidation-on-Medical-Costs.aspx. Published 2018. Accessed April 9, 2020
- 10. Scott KW, Orav EJ, Cutler DM, Jha AK. Changes in hospital‐physician affiliations in U.S. hospitals and their effect on quality of care. Ann Intern Med. 2017;166(1):1‐8. [DOI] [PubMed] [Google Scholar]
- 11. Short MN, Ho V. Weighing the effects of vertical integration versus market concentration on hospital quality. Med Care Res Rev. 2019. 538–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tsai TC, Jha AK. Hospital consolidation, competition, and quality: is bigger necessarily better? JAMA. 2014;312(1):29‐30. [DOI] [PubMed] [Google Scholar]
- 13. Cohen GR, Jones DJ, Heeringa J, et al. Leveraging diverse data sources to identify and describe U.S. Health Care Delivery Systems. EGEMS (Wash DC). 2017;5(3):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med. 2018;16(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Agency for Healthcare Research and Quality . Comparative Health System Performance (CHSP) Initiative. Agency for Healthcare Research and Quality. https://www.ahrq.gov/chsp/index.html. Published 2018. Accessed November 1, 2018
- 16. Singer SJ, Kerrissey M, Friedberg M, Phillips R. A comprehensive theory of integration. Med Care Res Rev. 2020;77(2):196‐207. [DOI] [PubMed] [Google Scholar]
- 17. Kerrissey MJ, Clark JR, Friedberg MW, et al. Medical group structural integration may not ensure that care is integrated. From the patient's perspective. Health Aff (Millwood). 2017;36(5):885‐892. [DOI] [PubMed] [Google Scholar]
- 18. Shortell SM. Themed issue: accountable care organizations and vertical integration. Health Care Manage Rev. 2019;44(2):91‐92. [DOI] [PubMed] [Google Scholar]
- 19. Ridgely MS, Duffy E, Wolf L, et al. Understanding U.S. Health systems: using mixed methods to unpack organizational complexity. EGEMS (Wash DC). 2019;7(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ridgely M, Ahluwalia S, Tom A, et al. What are the determinants of health system performance? Findings from the literature and a technical expert panel. Jt Comm J Qual Patient Saf. 2019;46(2):87‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dedoose . Features. https://www.dedoose.com/home/features. Published 2018. Accessed November 1, 2018.
- 22. Bradley EA, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758‐1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Birks M, Chapman Y, Francis K. Memoing in qualitative research: Probing data and processes. J Nurs. 2008;13(1):68‐75. [Google Scholar]
- 24. Ridgely MS, Timbie JW, Wolf LJ, et al. Consolidation by Any Other Name: The Emergence of Clinically Integrated Networks, Research Report A370–1. Santa Monica, CA: RAND Corporation; 2020. [Google Scholar]
- 25. Casalino LP. The Federal Trade Commission, clinical integration, and the organization of physician practice. J Health Polit Policy Law. 2006;31(3):569‐585. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Appendix S1
Appendix S2


