Abstract
Background:
We recently demonstrated the ability of a suite of tools embedded in an electronic medical record (EMR) to improve tobacco cessation treatment for adult smokers admitted to the hospital. A randomized controlled trial conducted by our group demonstrated the ability of an EMR-embedded tobacco use disorder treatment tool, the Electronic Support Tool and Orders for the Prevention of Smoking (E-STOPS), to increase the identification and treatment of smokers, but its uptake varied among 126 physicians randomized to the intervention arm. The purpose of this study was to identify facilitators and barriers to using E-STOPS.
Methods:
Semi-structured individual interviews from a purposive sample of 12 hospitalist attending physicians and nine internal medicine residents who were randomized to the E-STOPS intervention were analyzed thematically.
Results:
Three themes shaped E-STOPS use: the inpatient environment, prescriber attitudes and beliefs, and information needs. Overall, participants were pleased with E-STOPS, but had specific suggestions for improvements regarding the timing of the intervention, suppression logic, and additional decision support and training. A few had concerns about the clinical appropriateness of beginning treatment for tobacco dependence during a hospitalization and the proper role of the inpatient team in that treatment.
Conclusions:
Tobacco dependence treatment for hospitalized smokers and facilitated by the EMR is generally acceptable to hospitalists and resident physicians. Improvements in provider training and feedback as well as the timing and content of the electronic tools may increase their utilization by inpatient physicians.
Keywords: Tobacco cessation, smoking/harm reduction, Tobacco dependence, Electronic medical record, Qualitative research
1. Introduction
Hospitals are smoke-free environments and required to identify and offer treatment to smokers who are hospitalized. (Centers for Medicare and Medicaid Services, 2009; Fiore et al., 2012; Williams et al., 2009). Inpatients undergo a period of enforced tobacco abstinence, providing a “teachable moment” (Boudreaux et al., 2012; Buchbinder et al., 2014; Lawson and Flocke, 2009) to initiate treatment and promote long-term abstinence. Furthermore, because many admissions are for tobacco-related conditions, these acute health events may provide sufficient motivation for smokers to quit (Boudreaux et al., 2007).
Health information technology is an accepted tool to identify and treat smokers (Blumentha and Tavenner, 2010). The ubiquity of electronic medical records (EMRs) allows the integration of data from ambulatory, inpatient, and emergency department encounters so that care initiated in one clinical setting can be continued in another. Because tobacco dependence treatment initiated during inpatient stays leads to long-term abstinence if continued for at least 30 days (Rigotti et al., 2012), EMRs can make treatment of tobacco dependence an integrated, systemwide effort. Counseling by clinicians has been demonstrated to increase quit rates for smoking (Stead et al., 2013). EMRs include a variety of functionalities to facilitate the “5 A’s” of tobacco dependence treatment: Ask, Advise, Assess, Assist, Arrange, with most functions focusing on Asking about tobacco use and Assisting with medication prescribing (Schindler-Ruwisch et al., 2017).
Our recent longitudinal, randomized controlled trial demonstrated the ability of an EMR-embedded tobacco use disorder treatment tool, the Electronic Support Tool and Orders for the Prevention of Smoking (E-STOPS), to increase the identification and treatment of smokers (Bernstein et al., 2017). E-STOPS use varied considerably, and we conducted a qualitative sub-study to better understand the potential barriers and facilitators that may shape physician use of E-STOPS and ascertain how to improve its uptake and use.
2. Methods
2.1. Overview of E-STOPS
From 2012–2016 we conducted a randomized trial to compare rates of smoking cessation among medical inpatients who were cared for by physicians randomized to one of two arms: (1) access to the standard EMR that included only the tobacco dependence treatment medications from the hospital formulary or (2) an intervention arm that included a one-hour training session on tobacco dependence treatment and access to E-STOPS (Bernstein et al., 2017). The E-STOPS program consisted of a best practice alert (BPA) that informed physicians of patients’ smoking status and allowed for easy selection from a menu of evidence-based smoking cessation treatment options. These included entering tobacco use disorder (TUD) in the patient’s problem list, a medication order set for nicotine replacement therapy (NRT) in several dosages as well as several other medications (i.e., clonidine, nortriptyline, and bupropion), Connecticut Smokers’ Quitline (QL) referral, and notification of the patient’s primary care provider via EMR messaging that tobacco dependence treatment had been initiated during hospitalization.
2.2. Study sample
Participants for the qualitative sub-study included hospitalist attending physicians or internal medicine resident physicians who had been randomized to the intervention arm and treated at least 10 patients who were smokers. All participants practiced at one of two teaching hospitals in New Haven, Connecticut that serve much of New Haven County. A total of 46 potential participants were currently on staff at the time of recruitment for the sub-study. They were contacted via email up to three times and invited to participate in the study. Enrollment continued until data saturation was reached; 21 of the 46 potential participants expressed interest in participating in the study (46% response rate) and all 21 enrolled (i.e., none of those who contacted the study declined to participate).
2.3. Procedures
Data for the qualitative sub-study were collected between February and November 2016 and included 21 participants. Using a purposive sampling strategy, approximately equal numbers of internal medicine residents and hospitalists were invited to participate. We continued to interview until thematic saturation had been achieved (Guest et al., 2006). All interviews (except for one) were individually administered in a private setting with the remaining conducted by telephone.
Two experienced qualitative interviewers (LG, DC) conducted the interviews using a semi-structured interview guide developed for this study. Each interview lasted 30–60 minutes, was digitally recorded, and transcribed verbatim. All study procedures and materials were approved by the Yale Human Investigation Committee. Participants provided written informed consent and received a $10 gift certificate upon completion of the interview.
2.4. Data collection and analysis
The interview guide included five domains: (1) history of tobacco cessation training and customary pre-study approach to TUD treatment, (2) description of participants’ typical daily inpatient workflow, opinions about (3) E-STOPS functionality and (4) training they initially received in the main study, and (5) recommendations for program improvement.
The members of the research team responsible for coding and analysis (LG, DC, JW, and TO) met regularly to discuss the transcripts and develop the codebook. Two residents and two hospitalist transcripts were coded independently by each and discussed during codebook development. Coding discrepancies were resolved by consensus. Codebook refinement continued until no new codes were identified and there was acceptable inter-coder reliability. The remaining transcripts were independently coded by one of two coders (TO or JW) and reviewed by the first author when entering the data into ATLAS.ti (Version 7.1.7). The four team members met regularly to analyze the data iteratively and inductively. Thematic analysis (Braun and Clarke, 2006, 2013) and the constant comparison (Kolb, 2012) methods were used to identify common patterns across the codes and interview content. A systematic search for “negative” instances where the data did not fit the existing themes was also included in the analysis.
3. Results
Participants’ positions (i.e., hospitalists or internal medicine residents) and gender were the only descriptive data collected. The sample included 21 physicians, 10 of whom were internal medicine residents; 12 were males.
Three major themes that shaped participants’ E-STOPS use emerged from the 36 codes (Fig. 1). Two themes—E-STOPS in the Inpatient Environment and Personal Attitudes and Beliefs—appeared to directly influence behavior, whereas the Information Needs theme appeared to indirectly affect E-STOPS behavior through its potential impact on participants’ attitudes about E-STOPS or their approach to inpatient care.
Fig. 1.
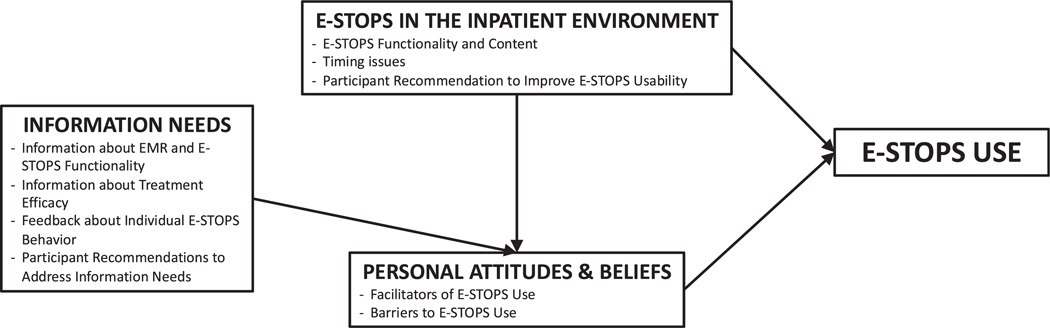
Conceptual Model of the Issues that Shape Physicians’ Use of the Electronic Support Tool and Orders for the Prevention of Smoking (E-STOPS).
The three themes are described below and illustrative quotes for each sub-theme are provided in Table 1.
Table 1.
Themes and Explicatory Quotes.
| Theme 1: E-STOPS in the Inpatient Environment | |
| E-STOPS Functionality and Content | P12, Hospitalist, male: The thing that has been brought forward in my mind is the fact that the hospital takes smoking cessation seriously and that it’s not just one person trying to do this, the fact that there’s a team and really trying to connect the inpatient and outpatient [care]. |
| Timing Issues | P13, Hospitalist, female: This discussion, while it is important, I don’t think it needs to be done by me in the middle of the night when I only have about twenty minutes or so to see this patient. |
| P6, Internal Medicine, male: I’m not going to order a nicotine patch now because I haven’t even talked to the person yet. | |
| P5, Internal Medicine, male: Their problem list could be very outdated. So I would not do an intervention just based on what [the EMR] says. | |
| Participant Recommendations to Improve E-STOPS Usability | P8, Internal Medicine, male: So perhaps the first time in a day [or]...the first time I enter into the chart after eight a.m. or in the beginning when you start the progress note for the patient. And it could be a reminder that yesterday it was too busy. Today we can discuss this with the patient... and it should continue [to fire] once a day, and only if we haven’t addressed it earlier. |
| P2, Internal Medicine, female: [To] address smoking cessation on discharge may be more helpful for me than every time I go in the chart | |
| P12, Hospitalist, male: So I think if it were something that when you were entering the admission orders, it was just part of that instead of being a best practice alert. Since the study [started], many more best practice alerts have been added, so people sometimes develop muscle memory to just dismiss them. | |
| P15, Hospitalist, male: [The order set] is displayed a little differently than the way we’re used to ordering things that are only available in some of the facilities and not all of them. So [to order something,] I have to think about what building am I in. it’s a little hiccup when you’re trying to do this quickly. | |
| Theme 2: Information Needs | |
| Information about EMR and E-STOPS Functionality | P21, Hospitalist, male: Most of the time I’m not even aware that [TUD has been] added to it until I import the problem list into my notes, and suddenly it’s there. |
| P7, Internal Medicine, female: I remember my very first day as being an intern, the order set popping up and then feeling like I didn’t even know how to use [the EMR] and I didn’t even know how to do anything, and I specifically remember just cancelling out of it so that I could get back to trying to figure everything out, and then never really. And then I think just moving forward, every time it would pop I’ve just gotten accustomed to just trying to get rid of it. | |
| Information about Treatment Efficacy | P4, Internal Medicine, female: What are the long-term impacts on the things that we implement to help patients quit or there’s the medications or it’s the referral, how effective are they? Honestly, I don’t know, but I am curious.is it effective? |
| Feedback about Individual E-STOPS Behavior | P6, Internal Medicine, male: I did like it as a reminder, about the update e-mails that we got about my practices. |
| Participant Recommendations to Address Information Needs | P18, Hospitalist, male: I wouldn’t have minded somebody telling me how effective [the medications listed in the NRT order set were] or where they’re getting this from. |
| P8, Internal Medicine, male: If we can distribute the slides or if we can have every six months a small e-mail that would say, “Here is an online refresher course, ” because we have refresher courses for the hospital. | |
| Theme 3: Personal Attitudes and Beliefs | |
| Facilitators of E-STOPS Use | P9, Internal Medicine, female: I definitely think that while they are already not smoking while in the hospital that that’s a perfect time to bridge them to quitting or cutting back as they leave. |
| P10, Hospitalist, male: These patients may not be regular consumers of healthcare or may not have regular follow-up. So, I think that when they’re hospitalized, it is an opportunity [to intervene]. | |
| Barriers to E-STOPS Use | P17, Hospitalist, male: For a routine patient like somebody who comes in for maybe pneumonia or urinary tract infection, there is no immediate association between the two, so we [wouldn’t talk to the patient about smoking cessation]…it’s only for COPD exacerbations. |
| P1, Internal Medicine, female: I make big differences in primary care that I don’t strive to in the inpatient side…And tobacco cessation, drinking cessation, those things are all outpatient primarily. | |
| P2, Internal Medicine, female: I always try to be cognizant of the amount of information that I give patients during a hospitalization. I do feel like I overwhelm them as it is with just their inpatient [problem]. I just don’t know that they’re ready to take one more thing. | |
| P13, Hospitalist, female: Not all patients really need [NRT patches] in the hospital, so I would never just order a medicine that someone is not asking for...I think it should be their decision. |
3.1. E-STOPS in the inpatient environment theme
3.1.1. E-STOPS functionality and content
Most participants described E-STOPS as “a useful touchpoint,” “comprehensive,” and “easy to use.” They appreciated that it served as a “nice reminder” of patients’ smoking status and as easy access to NRT dosing information and automatic QL referral.One participant noted that E-STOPS served “to raise the level of awareness of providers about that issue of tobacco cessation” (P2, Internal Medicine, female) and reinforced the message of tobacco cessation as a health priority for the organization.
Although most participants liked having dosing information and several NRT options, some expressed reservations about initiating treatments other than NRT “because [they] didn’t want to start something without having that long conversation” (Participant 3, Internal Medicine, female)—although this participant was willing to continue patients’ existing medications.
3.1.2. Timing issues
Participants discussed the vicissitudes of the inpatient environment, how firing of the E-STOPS components fit with an unpredictable inpatient workflow, patients’ acute versus long-term needs, and providers’ customary practice. The desire was for the firing of E-STOPS to occur at the most appropriate times during patient evaluation, treatment, and discharge. Many suggested preferred times for E-STOPS to fire and for repeat firings to occur. Possible suppression of initial firing until acute medical needs are addressed or the patient has been seen and their desire to receive NRT while hospitalized has been discussed was also frequently mentioned.
Most participants were open to automatic firing of the TUD and QL components upon admission. Objections to automatic firing were primarily based upon participants’ mistrust of the accuracy of the EMR information. Some also thought that repeat firings when accessing a patient’s EMR could engender “alert fatigue” (i.e., becoming inured and not responding to alerts). Participants’ attempts to be proactive and see patients before they were physically brought to the medical unit activated E-STOPS and potentially increased the frequency of popups. This could, in turn, promote alert fatigue and tendencies to dismiss the program.
3.1.3. Recommendations to improve E-STOPS usability
Participants recommended ways to improve E-STOPS functionality and promote its consistent use by providers. These included adjusting the timing of BPAs and modifying the format and content of the tobacco order set.
Given the necessity to first focus on patients’ acute medical problems, participants suggested that E-STOPS should fire multiple times during the inpatient stay. There was no clear consensus, however, about how many times or at what times of the day it should fire. Many recommended that E-STOPS fire at discharge when tobacco use cessation could be part of the conversation about transitioning back to outpatient care. Two participants recommended incorporating E-STOPS into the existing admissions order set to reduce alert fatigue and ensure its consistent use. Participants also recommended improving ease of use by standardizing the E-STOPS format to be consistent with other order sets in use. The difference in physical appearance from that of other existing order sets posed a barrier to its use, particularly when time demands were greatest.
3.2. Information needs theme
Participants identified several types of information deficits that, if addressed, may increase E-STOPS use. These included more information about EMR and E-STOPS functionality, treatment efficacy of the various E-STOPS options, and feedback about individual E-STOPS behavior.
3.2.1. Information about EMR and E-STOPS functionality
Participants believed that providers would make better use of and more informed decisions about E-STOPS with further training about the functionality and navigation of both the EMR and E-STOPS. As participants discussed their E-STOPS use, it also became apparent that many were unclear about how to navigate the alert and order set or about the results of their actions. Participants often inadvertently dismissed alerts and were unable to later retrieve them. Rather than their action being based on any conscious decision, they were often unaware of having ordered QL referrals when they accepted E-STOPS in an attempt to prevent future alerts each time they entered patients’ medical records.
Lack of familiarity with the EMR could influence E-STOPS behaviors and ultimately become habit. These observations raised the question for researchers about whether E-STOPS activation should be delayed until new staff become accustomed to the EMR.
A second issue pertained primarily to hospitalists’ schedules. Residents have regularly scheduled, mandatory meetings and receive weekly emails from chief residents, thereby making it easier to schedule their trainings. Hospitalists have no mandatory meeting requirements. Hence, it is less clear whether extended or ongoing, in-person training is possible for hospitalists. One hospitalist recommended that it could be added to their annual remote training requirements as a “video presentation that you can click on your own at your own leisure” (P17, Hospitalist, male).
3.2.2. Information about treatment efficacy
Inpatient providers have little opportunity to observe the long-term effects of tobacco cessation interventions. Many participants acknowledged their relative lack of knowledge about the efficacy of tobacco cessation interventions such as NRT and QL and their interest in learning more about these subjects.
3.2.3. Feedback about individual E-STOPS behavior
Participants believed that periodically receiving information (e.g., quarterly reports) about how much (or little) they used E-STOPS was useful and could encourage them to use the program. They appeared genuinely interested in feedback about their own E-STOPS behavior over time and relative to that of other providers with access to the electronic support tool.
3.2.4. Recommendations to address information needs
To address information needs, participants primarily recommended methods to improve information dissemination and supplemental training, particularly with respect to scientific evidence about tobacco cessation interventions. Additional training, refresher courses, and updates on advances in treatment of tobacco use disorder were commonly recommended.
Participants primarily discussed tobacco cessation with patients with pulmonary or cardiovascular diagnoses and appeared unaware of the potential negative impact of smoking on other health problems (Ford and Shilliday, 2006; Silverstein, 1992). This “negative instance” suggests the need to increase awareness of the deleterious effects of smoking on other conditions and could further reinforce the need to address tobacco cessation with all patients who smoke.
3.3. Personal attitudes and beliefs theme
Participants provided both direct and indirect evidence of how attitudes and beliefs about program functionality, smoking cessation interventions, and preferred approach to inpatient care shaped E-STOPS behavior. E-STOPS use appeared to be linked to the belief that an intervention requiring minimal time or effort that can improve patients’ health was well worth doing and “certainly made it a lot easier to do the right thing” (P15, Hospitalist, male).
3.3.1. Facilitators of E-STOPS use
E-STOPS use appeared more likely to occur when providers believed that inpatient settings are an appropriate environment in which to encourage patients to quit or try new approaches to smoking cessation—particularly for patients who lacked access to ambulatory healthcare services and may have never thought about quitting.
3.3.2. Barriers to E-STOPS use
Aside from timing issues and the need to address acute medical problems, three beliefs also appeared to discourage E-STOPS use. The first was the belief that inpatient treatment for tobacco use was only appropriate for specific admitting diagnoses, most often identified as chronic obstructive pulmonary disease or cardiac problems. A second barrier concerned the belief that, with little or no opportunity for patient follow-up once discharged, the issue of tobacco cessation was more appropriately within the purview of outpatient primary care. Finally, participants often rationalized their reluctance to use E-STOPS based on their expectations about patients or (less frequently) the belief that the patient should always initiate the request for treatment.
4. Discussion
E-STOPS was generally well-received. We identified three themes among the 21 interviews with internal medicine residents and hospitalists. Apart from the challenge of scheduling in-person training sessions for the latter group, no between-group differences in content were discernible.
Our findings were generally consistent with previous studies (Jensen and Bossen, 2016; Koskela et al., 2016; Taft et al., 2017). Alerts were viewed as useful reminders, but provider workload and workflow often impeded E-STOPS use. The timing of reminders to be consistent with clinicians’ workflow (Bates et al., 2003; Jenssen et al., 2016; Militello et al., 2004; Patterson et al., 2005, 2004; Saleem et al., 2005) and reducing the overall number of alerts (Saleem et al., 2005) were thought to facilitate E-STOPS use. The number and frequency of alerts is critical to the successful implementation of EMR-based programs (Bates et al., 2003), as most alerts are dismissed (van der Sijs et al., 2006), and response attenuates over time (Saleem et al., 2005). Participants’ stated suggestions of limiting firing to daytime hours (after placing the initial and most urgent orders), continuing to fire until the provider responds, firing again at discharge, and permitting access to other staff with discharge responsibilities were thought to be ways to promote E-STOPS use. These strategies could potentially be less intrusive, reduce the number of alerts received by any given provider, and be tested in future studies to determine which are most effective in increasing E-STOPS use.
Although providers’ decision-making process and treatment approach can vary considerably (Forsvik et al., 2017; Neri et al., 2015) and be influenced by local policies and environmental factors, a review concluded that decision-support systems improve prescribing practices and preventive care referrals. However, few studies have examined the effect of these systems on clinical, workload, or efficiency outcomes (Bright et al., 2012). Hence, we recommend that computer-based health promotion interventions consider not only providers’ information needs, workflow, and usability issues but also seek to design programs to be sufficiently flexible to individual treatment approaches and decision-making styles (Rizvi et al., 2016; Van Engen-Verheul et al., 2016). For example, alerts for a given provider could be suppressed until after meeting the patient and submitting initial orders. They could also be suppressed within designated units wherein patients may have acute medical needs or need for emergent stabilization (e.g., intensive care, delivery wards). Another possible strategy for promoting E-STOPS use and reducing risk of alert fatigue would be to permit access to E-STOPS to other staff (e.g., nursing, social work, health psychology, respiratory therapy, pharmacy) or in conjunction with discharge activities and plans. Feedback to program designers about usability issues also facilitates program use (Saleem et al., 2005), and based upon the many suggestions from participants on how to improve E-STOPS usability, we further recommend including a feedback option for users to voice concerns about E-STOPS functionality and usability to encourage user “buy-in” and provide the software developers with valuable information about how to further improve E-STOPS.
Simple or minor changes in formatting, such as having the intervention appear on a single screen and providing citations for or links to seminal articles and guidelines, can also improve program use (Bates et al., 2003; Teich et al., 1993; Van Engen-Verheul et al., 2016) and were noted by participants in this study. In addition, although only one participant recommended standardizing the order set format to be consistent with all other order sets within the same EMR system, this recommendation seems relatively easy to implement and could greatly improve E-STOPS usability in that the time to mentally process the information would be reduced. Notwithstanding, format does not appear to be as important as EMR data validity (Jensen and Bossen, 2016). As providers noted and consistent with the literature, inaccuracies can result in false-positive alerts, mistrust of the system, and inefficient use of clinicians’ time (Koskela et al., 2016). Strategies to improve the validity of EMR data could greatly improve use of EMR-embedded tools such as E-STOPS. This could be accomplished through routine and frequent updates of patients’ EMR and periodic reporting on improvements made to the EMR system and statistics concerning data accuracy. Through these actions, it is hoped that confidence in data accuracy would gradually improve over time.
The difficulties noted by many participants in navigating the program also suggested the need for more detailed training about program navigation and functionality. The importance of this training has been associated with increased user satisfaction and decreased perceived level of stress (Ghahramani et al., 2009; Patterson et al., 2005). Therefore, it is important to ensure that clinicians—particularly those who are new to EMR and/or E-STOPS—meet a designated minimum standard of competence in navigating these system(s). It may also help to implement the trainings in a stepwise fashion with EMR training occurring first and allowing for time to get used to that system before initiating E-STOPS training and use.
Consistent with a review article on reminders and feedback (Bennett and Glasziou, 2003), many participants were interested in information about treatment efficacy for various tobacco cessation interventions, feedback about their E-STOPS behavior, and access to brief online courses. These points could improve provider receptiveness to E-STOPS and could be customized for all staff positions that may contribute to the treatment of tobacco dependence.
It could be inferred from the interviews that an inpatient “culture” appeared to exist in which discussions about smoking cessation with inpatients were limited to a circumscribed set of diagnoses (e.g., COPD). One unique finding from this study was the “negative instance” was that of participants not recognizing how smoking has far-reaching negative consequences (e.g., complicates healing of wounds or management of chronic illnesses such as diabetes). Offering empirical evidence about the potential deleterious effects of smoking on many health problems may increase discussions about tobacco cessation with all patients who smoke. And while the concept that patients, not providers, should decide whether to initiate NRT seems consistent with a patient-centered culture, it also suggests a reactive rather than proactive approach to the treatment of tobacco dependence. We recommend disseminating information about the far-reaching deleterious effects of smoking and, as previously noted, empirical evidence of the effectiveness of smoking cessation interventions. We also support efforts to make tobacco dependence treatment the default (i.e., requiring patients who decline treatment to “opt out”) as another strategy to increase access to tobacco cessation treatment within the inpatient setting (Richter and Ellerbeck, 2015).
Several study limitations should be noted. First, the study occurred within one hospital system. The EMR systems and the environment in which they are used vary, and hence, the results of the current study may have limited transferability and should be verified and adapted according to the local needs of other healthcare environments. Second, recall and social desirability biases may have influenced the findings. Finally, although the issue of leaving requests for tobacco pharmacotherapy entirely to the patient was not suggested by many, the frequency of this belief should be assessed in future studies to determine whether an “opt out” approach would further promote E-STOPS use (Richter and Ellerbeck, 2015).
In conclusion, EMR-facilitated tobacco dependence treatment for hospitalized smokers is feasible and generally acceptable to hospitalist and internal medicine resident physicians. Improving provider training and feedback, the timing and content of the electronic tools, and considering providers’ decision-making and treatment approach may increase utilization by providers.
Acknowledgements
The authors wish to thank the participants for sharing their experiences and recommendations with our research team.
Funding
This study was supported by grant R18HL108788 from the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Footnotes
Conflict of interest
No authors have any competing interests.
References
- Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, Spurr C, Khorasani R, Tanasijevic M, Middleton B, 2003. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J. Am. Med. Inform. Assoc. 10, 523–530. 10.1197/jamaia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett JW, Glasziou PP, 2003. Computerized reminders and feedback in medication management: a systematic review of randomized controlled trials. Med. J. Aust. 178, 217–222. [DOI] [PubMed] [Google Scholar]
- Bernstein SL, Rosner J, DeWitt M, Tetrault J, Hsiao AL, Dziura J, Sussman S, O’Connor P, Toll B, 2017. Design and implementation of decision support for tobacco dependence treatment in an inpatient electronic health record. Transl. Behav. Med. 7, 185–195. 10.1007/s13142-017-0470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumentha l D., Tavenner M, 2010. The “meaningful use” regulation for electronic health records. N. Engl. J. Med. 363, 501–504. 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Baumann BM, Camargo CA Jr., O’Hea E, Ziedonis DM, 2007. Changes in smoking associated with an acute health event: theoretical and practical implications. Ann. Behav. Med. 33, 189–199. 10.1080/0883661070131003. [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Bock B, O’Hea E, 2012. When an event sparks behavior change: an introduction to the sentinel event method of dynamic model building and its application to emergency medicine. Acad. Emerg. Med. 19, 329–335. 10.1111/j.1553-2712.2012.01291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V, 2006. Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Braun V, Clarke V, 2013. Successful Qualitative Research: A Practical Guide for Beginners. SAGE Publications Ltd, Thousand Oaks, CA. [Google Scholar]
- Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, Samsa G, Hasselblad V, Williams JW, Musty MD, Wing L, Kendrick AS, 2012. Effect of clinical decision-support systems. A systematic review. Ann. Intern. Med. 157, 29–43. 10.73326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- Buchbinder M, Wilbur R, Zuskov D, McLean S, Sleath B, 2014. Teachable moments and missed opportunities for smoking cessation counseling in a hospital emergency department: a mixed-methods study of patient-provider communication. BMC Health Serv. Res. 14, 651 10.1186/s12913-014-0651-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services, 2009. Medicare and Smoking Cessation. http://www.scdhec.gov/Health/docs/Medicare_SmkgCessation2009.pdf. [PubMed]
- Fiore MC, Gopelrud E, Schroeder SA, 2012. The Joint Commision’s new tobacco-cessation measures-will hospitals do the right thing? N. Engl. J. Med. 366, 1172–1174. 10.1056/NEJMp1115176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford SK, Shilliday BB, 2006. Smoking and diabetes: helping patients quit. Clin. Diabetes 24, 133–137. 10.2337/diaclin.24.3.233. [DOI] [Google Scholar]
- Forsvik H, Voipio V, Lamminen J, Doupi P, Hypponen H, Vuokko R, 2017. Literature review of patient record structures from the physician’s perspective. J. Med. Syst. 41 (29). 10.1007/s10916-016-0677-0. [DOI] [PubMed] [Google Scholar]
- Ghahramani N, Lendel I, Haque R, Sawruk K, 2009. User satisfaction with computerized order entry system and its effect on workplace level of stress. J. Med. Syst. 33, 199–205. 10.1007/s109166-008-9180-6. [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, Johnson L, 2006. How many interviews are enough? An experiment with data saturation and variability. Field Meth. 18, 59–82. . [DOI] [Google Scholar]
- Jensen LG, Bossen C, 2016. Factors affecting physicians’ use of a dedicated overview interface in an electron helath record: the importance of standard information and standard documentation. Int. J. Med. Inform. 87, 44–53. 10.1016/j/ijmedinf.2015.12.009. [DOI] [PubMed] [Google Scholar]
- Jenssen BP, Bryant-Stephens T, Leone FT, Grundmeier RW, Fiks AG, 2016. Clinical decisions support tool for parental tobacco treatment in primary care. Pediatrics 137, e20154185. 10.1542/peds.2015-4185. [DOI] [PubMed] [Google Scholar]
- Kolb SM, 2012. Grounded theory and the constant comparative method: valid research strategies for educators. J. Emerging Trends Educ. Res. Policy Stud. 3, 83–86. [Google Scholar]
- Koskela T, Sandstrom S, Makinen J, Liira H, 2016. User perspectives on an electronic decision-support tool performing comprehensive medication review – a focus group study with physicians and nurses. BMC Med. Inform. Decis. Mak. 16, 6 10.1186/s12911-016-0245-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson PJ, Flocke SA, 2009. Teachable moments for health behavior change: a concept analysis. Patient Educ. Couns. 76, 25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Militello L, Patterson ES, Tripp-Reimer T, Asch SM, Fung CH, Glassman P, Anders S, Doebbeling B, 2004. Clinical reminders: why don’t they use them? Proc. Hum. Factors Ergon. Soc. Annu. Meet. 48, 1651–1655. 10.1177/154193120404801505. [DOI] [Google Scholar]
- Neri PM, Redden L, Poole S, Pozner CN, Horsky J, Raja AS, Poon E, Schiff G, Landman A, 2015. Emergency medicine resident physicians’ perceptions of electronic documentation and workflow. A mixed methods study. Appl. Clin. Inform. 6, 27–41. 10.4338/ACI-2014-08-RA-0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson ES, Doebbeling BN, Fung CH, Militello L, Anders S, Asch SM, 2005. Identifying barriers to the effective use of the effective use of clinical reminders: bootstrapping multiple methods. J. Biomed. Inform. 38, 189–199. 10.1016/j.jbi.2004.11.015. [DOI] [PubMed] [Google Scholar]
- Patterson ES, Nguyen AD, Halloran JP, Asch SM, 2004. Human factors barriers to the effective use often HIV clinical reminders. J. Am. Med. Inform. Assoc. 11, 50–59. 10.1197/jamia.M1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter KP, Ellerbeck EF, 2015. It’s time to change the default for tobacco treatment. Addiction 110, 381–386. 10.1111/add/12734. [DOI] [PubMed] [Google Scholar]
- Rigotti NA, Clair C, Munafo MR, Stead LF, 2012. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst. Rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi RF, Harder KA, Hultman GM, Adam TJ, Kim M, Pakhomov SVS, Melton GB, 2016. A comparative observational study of inpatient clinical note-entry and reading/retrieval styles adopted by physicians. Int. J. Med. Inform. 90, 1–11. 10.1016/j.ijmedinf.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleem JJ, Patterson ES, Militello L, Render ML, Orshansky G, Asch SM, 2005. Exploring barriers and facilitators to the use of computerized clinical reminders. J. Am. Med. Inform. Assoc. 12, 438–447. 10.1197/jamia.M1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schindler-Ruwisch JM, Abroms LC, Bernstein SL, Heminger CL, 2017. A content analysis of electronic health record (EHR) functionality to support tobacco treatment. Transl. Behav. Med. 7, 148–156. 10.1007/s13142-016-0446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein P, 1992. Smoking and wound healing. Am. J. Med. 93, S22–S24. 10.1016/0002-9343(92)90623-J. [DOI] [PubMed] [Google Scholar]
- Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T, 2013. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taft T, Staes C, Slager S, Weir C, 2017. Adapting Nielsen’s design heuristics to dual processing for clinical decision support. AMIA Annu. Symp. Proc. 2016, 1179–1188. [PMC free article] [PubMed] [Google Scholar]
- Teich JM, Spurr CD, Flammini SJ, Schmiz J, Beckley RF, Hurley JF, Aranow M, Glaser JP, 1993. Response to a trial of physician-based inpatient order entry. Proc. Annu. Symp. Comput. Appl. Med. Care 316–320. [PMC free article] [PubMed] [Google Scholar]
- van der Sijs H, Aarts J, Vulto A, Berg M, 2006. Overriding of drug safety alerts in computerized physician order entry. J. Am. Med. Inform. Assoc. 13, 138–147. 10.1197/jamia.M1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Engen-Verheul MM, Peute LWP, de Keizer NF, Peek N, Jaspers MWM, 2016. Optimizing the user interface of a data entry module for an electronic patient record for cardiac rehabilitation: a mixed method usability approach. Int. J. Med. Inform. 87, 15–26. 10.1016/j.ijmedinf.2015.12.007. [DOI] [PubMed] [Google Scholar]
- Williams SC, Hafner JM, Morton DJ, Holm AL, Milberger SM, Koss RG, Loeb JM, 2009. The adoption of smoke-free hospital campuses in the United States. Tob. Control 18, 451–458. 10.1136/tc.2009.030494. [DOI] [PubMed] [Google Scholar]


