Abstract
INTRODUCTION:
Although sleep disorders in chronic obstructive pulmonary disease (COPD) are common, no study has comprehensively evaluated sleep disorders in COPD, and there are no screening tools available for COPD patients. Global sleep assessment questionnaire (GSAQ) is one of the best screening tools for the general population.
AIMS AND OBJECTIVES:
The aims and objectives of the study were to find (i) the prevalence of sleep disorders in COPD based on GSAQ score; (ii) if the GSAQ score in COPD is high compared to healthy adult population; (iii) the prevalence of insomnia, obstructive sleep apnea (OSA), restless leg syndrome (RLS), and depression in COPD patients; and (iv) the sensitivity and specificity of GSAQ.
METHODS:
This was a prospective case–control study where GSAQ is administered to 100 stable COPD and 50 healthy individuals. The presence of sleep disorder in COPD was further confirmed based on the diagnostic criteria and polysomnography.
RESULTS:
GSAQ was positive in 68% of the COPD patients compared to 16% of the matched healthy adults (P < 0.001). The sleep disturbance was confirmed in 66 COPD patients. Insomnia, OSA, RLS, depression/anxiety, and overlap of two or more disorder were seen in 39, 13, 30, 22, and 31 patients, respectively. The overall sensitivity/specificity of GSAQ for sleep disturbances in COPD was 90.9%/70.58%, respectively. The sensitivity/specificity of GSAQ for insomnia, OSA, RLS, and anxiety/depression was 87/75%, 77/67%, 90/80%, and 91/65%, respectively.
CONCLUSION:
Sleep disorders in COPD patients are significantly high. GSAQ is a good screening tool for detecting the presence of disturbed sleep in COPD. Overlap of two or more sleep disorders is common in COPD.
Keywords: Chronic obstructive pulmonary disease, depression, global sleep assessment questionnaire, insomnia, obstructive sleep apnea, restless leg syndrome
Chronic obstructive pulmonary disease (COPD) is a chronic debilitating disease characterized by severe morbidity. It has long been recognized that sleep is adversely affected in COPD patients.[1] The estimated prevalence of sleep disturbance in COPD varies from 34% to 78%.[2,3,4] The pathophysiology for disturbed sleep in COPD is complex and multifactorial. It includes interplay between physiological changes, ventilatory disturbances, inflammation, and medications. The presence of sleep disorders may cause a further decline in the quality of life in COPD patients. It also predisposes already suffering COPD population to health problems, functioning, and health-care expenditures.[5,6] Despite these consequences, sleep disorders are not widely detected or treated.[5] There are no studies which have comprehensively evaluated various sleep disorders in COPD patients. Among the disorders described by the International Classification of Sleep Disorders 2014 (III),[7] insomnia and restless leg syndrome (RLS)/periodic limb movement in sleep (PLMS) are seen more commonly in COPD patients than the general population.[8] Obstructive sleep apnea (OSA), though not more common in COPD, can also cause poor sleep quality. The other COPD-related complications like poor cough and dyspnea control could also lead to sleep disturbances.
At present, various numbers of screening tools are available for identifying the presence of disturbed sleep in the general population. These include Berlin Questionnaire,[9] the Sleep Disorders Questionnaire (SDQ),[10] the Pittsburgh Sleep Quality Index (PSQI),[11] and the Global Sleep Assessment Questionnaire (GSAQ).[12] The Berlin Questionnaire selectively screens for OSA. The SDQ is a 175-item questionnaire and is considered too long to be used as a screening tool. The PSQI is a widely used tool; however, it qualitatively differentiates between “good sleepers” and “bad sleepers.” Furthermore, it was not intended to be used as a screening tool.
GSAQ was introduced by Roth et al.[12] in 2002. It is a comprehensive screening tool to assess the presence of sleep disorders in the general population. It comprises 11 items, which are presented in a grid format with responses on a single page.[12] The physical layout of the GSAQ is considered ideal because (1) it utilizes only one page; (2) the header contains pertinent information; (3) the symptom complaints are present in the form of a grid for easy response and interpretation; (4) the symptomatology corresponding to specific sleep disorder is presented in a row; and (5) it also covers daytime impairment.[13] The most important factors, which contribute to the strength of GSAQ, are its effectiveness and comprehensiveness. The sensitivity of GSAQ varies from 79% to 100% in the general population.[12] Due to this high sensitivity, GSAQ is considered as one of the best screening tools for identifying sleep disorders in the general population at the primary care level.[13] Since the GSAQ validity has not been evaluated specifically in COPD patients and the prevalence of sleep disorders in COPD is much higher than that in the healthy adult population, it is essential to find its validity in COPD patients. We undertook this study in a tertiary care center among patients of COPD to find the occurrence of sleep disturbances and sensitivity and specificity of GSAQ.
Methods
It was a prospective case–control study carried out in a tertiary care center from January 2017 to July 2019. The study was carried out after obtaining ethical clearance in adherence to the guidelines of the Declaration of Helsinki from the institutional ethical committee and written informed consent from the patients. The aims and objectives were to (1) find the prevalence of sleep disorders in COPD based on GSAQ score; (2) compare the GSAQ score in COPD with healthy adult population; (3) find the prevalence of insomnia, OSA, RLS, and depression in COPD patients, and (4) find the sensitivity and specificity of GSAQ score in COPD patients.
COPD patients were diagnosed according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD)[14] definition. Clinically, stable and optimally treated COPD patients were included in the study after obtaining their consent. Their age, sex, detailed history, clinical examination, and investigations were noted down in the proforma. Spirometry was conducted for all the patients. All the patients were on their regular inhalers and none of the patients were on oral corticosteroids. All the patients were initially asked if they had disturbed sleep. The patients were asked, “Do you have disturbed sleep?” and the answer for this was noted in form of “yes” or “no.”
All the patients were then subjected for GSAQ. GSAQ covers mood, daytime activities, and medical issues related to sleep and sleep disorders.[12] Description of GSAQ and sleep disorder related to individual question is given in Table 1. The response to GSAQ is considered positive if any of the sleep disorders was present in the past 1 month. It is considered as negative if the answer to all 11 questions was “Never.” Among these patients, giving a positive reply to question (Q) 1, 2, 3, 5, 6, 7, 8, 10, and 11 was evaluated further, as the corresponding disorders are commonly associated with COPD (i.e., insomnia, OSA, RLS/PLMS, nocturnal cough/dyspnea, and anxiety/depression).[8] Q4 and Q9 correspond to the disorder of shift worker disease and parasomnia, respectively, and were not evaluated further.
Table 1.
Description of global sleep assessment questionnaire and inference of individual question
| Question number | Symptoms | Sleep disorder |
|---|---|---|
| Q1 | Difficulty initiating and maintaining sleep | Insomnia |
| Q2 | Excessive day time sleepiness | OSA, insomnia |
| Q3 | Activity limitation due to inadequate sleep | Insomnia, OSA |
| Q4 | Working conditions causing inadequate sleep | Shift workers disease |
| Q5 | Presence of snoring | OSA |
| Q6 | Nocturnal choking or witnessed apnea in sleep | OSA |
| Q7 | Unpleasant sensation in legs relieved on movement | RLS, PLMS |
| Q8 | Involuntary leg jerks and twitches in sleep | RLS, PLMS |
| Q9 | Involuntary movements in sleep including scream, punch, and nightmares | Parasomnia |
| Q10 | Other causes leading to disturbed sleep like nocturnal cough, nocturnal dyspnea, etc | Causes secondary to systemic disease |
| Q11 | Sadness or anxiousness | Anxiety/depression |
OSA=Obstructive sleep apnea, RLS=Restless leg syndrome, PLMS=Periodic limb movement in sleep, COPD=Chronic obstructive pulmonary disease
All the patients were then subjected to individual disorder-based questionnaire or polysomnography (PSG). The study was a part of a larger study in which all the patients were subjected to nocturnal pulse oximetry. Patients suspected of having OSA based on the history of snoring and presence of either body mass index (BMI) ≥25 kg/mm2 or sawtooth pattern on nocturnal pulse oximetry[15] were subjected to Level 1 PSG using Philips Alice 5 Polysomnograph® as per the American Academy of Sleep Medicine (AASM)[16] guidelines. OSA was defined as per the AASM definition: Presence of five or more scoreable respiratory events, i.e., apnea, hypopneas, or respiratory effort-related arousal (RERA) per hour of sleep along with daytime or nocturnal symptoms or 15 or more scoreable respiratory events (i.e., apneas, hypopneas, or RERAs) per hour of sleep.[16]
RLS was diagnosed based on the “URGE” criteria. The causes of secondary RLS were ruled out before labeling it as RLS due to COPD. RLS was diagnosed when all the following criteria were satisfied:[17](1) an urge to move the legs, usually associated with unpleasant leg sensations, (2) exacerbation of symptoms by rest, (3) gets relieved on activity, and (4) symptoms worse in the evening and at night.
Insomnia was diagnosed as per the Diagnostic and Statistical Manual of Mental Disorders (V).[18] It defines insomnia as dissatisfaction with sleep quantity or quality associated with one (or more) of the following symptoms for at least three times/week in the past 3 months with daytime consequences: (1) difficulty initiating sleep; (2) difficulty maintaining sleep, characterized by frequent awakenings or problems returning to sleep after awakenings; and (3) early-morning awakening with inability to return to sleep. This excludes sleep–wake disorders, drug or medication abuse, and coexisting medical comorbidity causing insomnia.
The patients underwent screening with two-question depression screen, the Patient Health Questionnaire-2 (PHQ-2), and the three-question anxiety screen, the PHQ-3, from the Primary Care Evaluation of Mental Disorders (PRIME-MD).[19] PHQ-2 is an ultra-brief, two-item measure questionnaire with three possible answers. The questionnaire finds out the frequency of mood change per week over the past 1 month. Scores of ≥3 have been recommended to identify cases of major depressive disorder. The PHQ-3 score is used for screening anxiety disorder. It is a 3-point questionnaire with a similar framework. Due to its high sensitivity and specificity, it is considered as one of the best diagnostic tools.[20] Patients were sent to psychiatry evaluation after that.
Fifty randomly selected healthy adults were taken as control. These controls were attendants and relatives of the patients who used to accompany them to the hospital. The healthy adults were age and sex matched with the COPD patients. Those who gave their consent were included in the study. The exclusion criteria were i) active smoking, ii) presence of any respiratory symptoms/ disease, iii) presence of unstable comorbid conditions, iv) ongoing medications affecting sleep. They were all screened for the presence of sleep disorder using GSAQ. Participants giving a positive reply to any of the questions were considered as GSAQ positive. They were not subjected for further evaluation.
Statistical analysis
The sample size was calculated by formula: n = Z21-α/2 × p(1 − p)/d2. Assuming a prevalence (p) of sleep disorders of 40% in COPD patients[21] and a precision of 10%, the sample size obtained was 100. The data was tabulated on MS-Excel®(2010), and statistical analysis for mean, standard deviation, sensitivity, and specificity was done using “open EPI” software®(OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version 3.01). The positive and negative likelihood ratios were calculated using sensitivity and specificity using standard formulae. The “p” value was calculated using t-test, “ANOVA,” and “Chi-square test” wherever applicable.
Results
One hundred clinically stable COPD patients were enrolled in the study. On initial inquiry, 40% of the patients reported presence of disturbed sleep, which means 40 patients gave answer “yes” to the question – “do you have disturbed sleep?” On subjecting the patients for GSAQ, we found that 68 patients had the presence of one or other sleep disorders. These 68 included all the 40 patients who had reported the presence of disturbed sleep on initial history taking. Their characteristics including age, sex, comorbidities, and severity in terms of forced expiratory volume in 1 second (FEV1) are depicted in Table 2.
Table 2.
Characteristics of chronic obstructive pulmonary disease patients enrolled in the study
| GSAQ positive | GSAQ negative | P | |
|---|---|---|---|
| n | 68 | 32 | |
| Mean age (years) | 59.35±8.48 | 60.17±6.02 | 0.61 |
| Male-to-female | 56:10 | 33:1 | 0.06 |
| Mean smoking index* | 202.87±71.74 | 210±67.68 | 0.61 |
| Mean FEV1 (ml) | 958.18±302.07 | 890.85±390.05 | 0.34 |
| Mean FEV1 (percentage predicted) | 47.93±15.04 | 44.54±19.7 | 0.34 |
| GOLD | |||
| Stage I | 0 (0) | 2 (5.8) | |
| Stage II | 29 (43.39) | 9 (26.47) | |
| Stage III | 28 (42.42) | 13 (38.23) | |
| Stage IV | 9 (13.63) | 10 (29.41) | |
| Diabetes mellitus | 16 (24.24) | 7 (20.58) | 0.34 |
| Hypertension | 26 (39.4) | 17 (50) | 0.15 |
| Ischemic heart disease | 10 (15.15) | 6 (17.64) | 0.10 |
| Hypothyroidism | 4 (6.06) | 1 (2.9) | 0.24 |
*Smoking index=Cigarettes smoked per day multiplied by number of years. FEV1=Forced expiratory volume in 1 second, GSAQ=Global sleep assessment questionnaire, GOLD=Global initiative for chronic obstructive lung disease
The COPD patients were compared for the presence of sleep disorders using GSAQ with 50 age/sex-matched healthy adults. The average age of healthy adult population was 60.9 ± 3.9 years, among which 40 were men and 10 were women. Eight of fifty (16%) patients had a positive GSAQ score. Among these eight patients who reported disturbed sleep, six patients gave a positive answer for Q11. This suggested that anxiety/depression could be a cause of disturbed sleep in them.
GSAQ in COPD patients pointed toward insomnia in 49 patients (Q1/Q2/Q3), OSA in 39 (Q2/5/6), RLS/PLMS in 41 (Q7/Q8), and anxiety/depression in 47 (Q11). Sixteen patients had disturbed sleep due to causes attributable to COPD like nocturnal cough, nocturnal dyspnea, and pain (Q10). Sleep disorders unrelated to COPD, i.e., parasomnia (Q9), were suspected in 14 and shift work disorder was suspected in 12 patients (Q4). One patient gave positive answer to more than one question frequently. A confirmed diagnosis of disturbed sleep due to various disorders related to COPD was obtained in 66 patients using disease-specific questionnaire and PSG. Based on the respective questionnaires, 39 had insomnia and 30 had RLS. PHQ-2 and PHQ-3 for depression/anxiety was positive in 22 patients. Although 39 patients were suspected to have OSA based on GSAQ Q2/5/6 (i.e., excessive daytime sleepiness, snoring, or choking), only 16 among them had BMI ≥25 Kg/mm2 or sawtooth pattern on nocturnal pulse oximetry. On subjecting these 16 for PSG, 13 patients were diagnosed OSA. Thirty-one patients had an overlap of two or more disorders.
The patients diagnosed to have sleep disorders with the respective questionnaires and PSG were taken as true positive and those found not having any sleep disorder were taken as true negative. Using these data, we calculated the sensitivity and specificity of GSAQ for detecting the presence of various sleep disorders related to COPD. The sensitivity, specificity, and positive and negative likelihood ratios of GSAQ for detecting the presence of sleep-related disorder are given in Table 3.
Table 3.
Sensitivity, specificity, and positive likelihood ratio and negative likelihood ratio of the global sleep assessment questionnaire for detecting the presence of any sleep disorder and presence of individual disorder
| Based on GSAQ | Based on questionnaire/PSG | Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio | |
|---|---|---|---|---|---|---|
| Presence of sleep disorder | 68 | 66 | 90.9% | 70.58% | 3.08 | 0.12 |
| Insomnia | 49 | 39 | 87% | 75% | 3.48 | 0.17 |
| OSA | 39 | 13 | 77% | 67% | 2.33 | 0.34 |
| RLS | 41 | 30 | 90% | 80% | 4.5 | 0.12 |
| Anxiety/depression | 47 | 22 | 91% | 65% | 2.6 | 0.138 |
The total number of enrolled patients is 100; hence, the number of patients will be same as percentage. GSAQ=Global sleep assessment questionnaire, PSG=Polysomnography, OSA=Obstructive sleep apnea, RLS=Restless leg syndrome
The patients of COPD having sleep disorder were compared with those not having any sleep disorder in terms of age, FEV1(absolute and % predicted), and comorbidities. There was no statistically significant difference among the two [Table 1]. On classifying the patients based on GOLD stages, we found that only two patients belonged to GOLD Stage I. Hence, patients having GOLD Stages I and II were clubbed and GOLD Stages III and IV were clubbed. We compared patients in Stage I and II, i.e., FEV1≥50% with those in Stage III and IV, i.e., FEV1< 50%. The group having FEV1< 50% had a significantly higher likelihood of developing any of the sleep disorders (P < 0.05). This group with FEV1< 50% also had a significantly higher probability of developing RLS (P < 0.05). There was no statistically significant difference in patients having OSA, insomnia, or anxiety/depression among the two groups [Table 4].
Table 4.
Comparison of chronic obstructive pulmonary disease patients based on forced expiratory volume in 1 second
| Severity in terms of FEV1 | FEV1 <50% (n=60) | FEV1 ≥50% (n=40) | P |
|---|---|---|---|
| All sleep disorders | 35 (58.3) | 25 (62.5) | 0.02 |
| Insomnia | 23 (38.3) | 16 (40) | 0.41 |
| RLS | 25 (41.6) | 4 (10) | <0.05 |
| Anxiety/depression | 11 (18.3) | 11 (27.5) | 0.11 |
| OSA | 6 (10) | 7 (17.5) | 0.12 |
FEV1=Forced expiratory volume in 1 second, RLS=Restless leg syndrome, OSA=Obstructive sleep apnea
Discussion
The prevalence of disturbed sleep in COPD patients is estimated to be about 34%–78% in various studies.[2,3,22] We found that the prevalence of sleep disorders in COPD was 66%, of which 31% had an overlap of two or more disorders. The prevalence in COPD patients was significantly higher than the healthy adults (P < 0.001). Insomnia was found to be the most common sleep disorder in COPD, whereas GSAQ showed that a healthy population may have disturbed sleep commonly due to anxiety/depression. In a study on a healthy population from South India,[23] the prevalence of disturbed sleep varied between 20.0% and 34.2%; in our study, it was 16%.
Although sleep disorders in COPD are common, they are not identified or treated. Thus, there is a need to identify tools that can be implemented at the primary care level.[13] The data of presence or absence of sleep disorders are based on individual studies evaluating individual disorders. To the best of our knowledge, no study has comprehensively evaluated sleep in COPD. Our study is the first study to find out that the presence of two or more sleep disorders is common in COPD. Furthermore, we could not find any study, which has directly compared the prevalence of disturbed sleep in COPD patients to the general population.
Our study also shows that merely asking about the presence of sleep problems is not sufficient. A detailed questionnaire-based evaluation is needed to evaluate sleep in COPD patients. It is the first study to evaluate the sensitivity and specificity of GSAQ in COPD patients. Although GSAQ had high false-positive rate, i.e., specificity of only 70.58%, the sensitivity for detecting the presence of sleep disorder related to COPD was very high, i.e., 90.9%. We also found that the GSAQ had a high positive likelihood ratio of >1 for sleep disorders. This suggests that a positive GSAQ is strongly associated with the presence of sleep disorder. GSAQ thus can be used as a screening tool at primary care level for detecting sleep disorders in COPD. The COPD patients if screened at a primary care level using GSAQ, it can reduce the burden of a specialist. The further analysis of GSAQ-positive patients can be best done by a pulmonologist with knowledge of sleep disorders. An algorithm useful for primary care physicians has been depicted in Figure 1.
Figure 1.
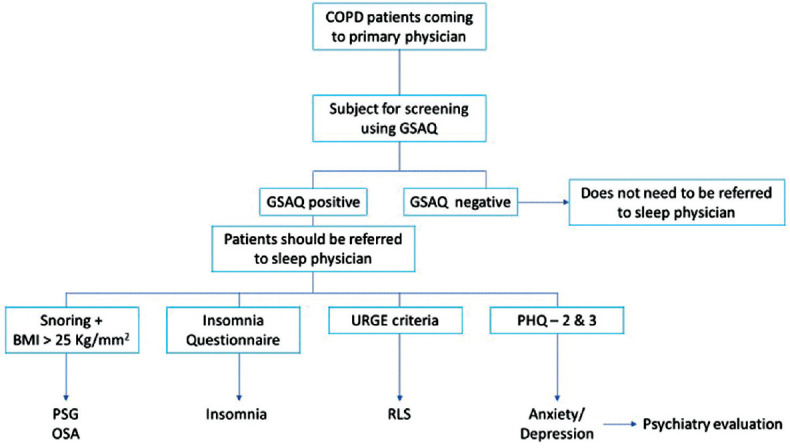
An algorithm useful for primary care physicians for the screening of chronic obstructive pulmonary disease patients for the presence of sleep disorders
The most common disorder seen in our study was insomnia. The prevalence of insomnia has been reported between 23% and 53%;[22] in our study, it was 39%. Although insomnia prevalence varies in various studies, it is definitely high when compared with those without COPD.[24] The presence of depression, anxiety, and current tobacco use, however, has shown a consistently higher prevalence of insomnia in COPD.[7,25] In our study, there was an overlap of insomnia in 16% with RLS, 13% with anxiety/depression, and 7% with cough/breathlessness at night. This indicates that it is important to find the cause of insomnia in COPD patients.
Flenley[26] in 1985 coined the term “overlap syndrome” for the co-occurrence of COPD and OSA in the same patient. The exact relationship between OSA and COPD is not fully established and may be influenced by many factors. Studies show that copresence of COPD and OSA leads to cor-pulmonale and severe exacerbations.[27] The prevalence of co-occurrence in our study was 13%. Thus, though the prevalence is not very high, it is important to treat the treatable cause to prevent the adverse outcome. A higher number of patients (39) were suspected to have OSA by GSAQ. On detail analysis this high false positive rate of GSAQ for OSA was due to coexistence of other disorders like insomnia. Thus, sensitivity and specificity for detecting OSA with GSAQ were lower compared to other disorders.
RLS, also known as Willis–Ekbom disease, is still a poorly recognized disorder in COPD.[28] The exact cause of the increased prevalence of RLS in COPD is not known but is thought to be hypoxia.[27] The prevalence of RLS in the general population ranges from 2.9% to 15%.[27,28] The prevalence of RLS in COPD is reported to be 36.8%,[28] it was 30% in our study. RLS may lead to insomnia and anxiety/depression. In our study, there was an overlap in 20%. RLS was associated with poorer lung function in our study, similar to previously reported studies.[29]
Another important aspect, which significantly affects sleep and overall quality of life, is anxiety/depression. Anxiety and depression contribute to a substantial burden of COPD-related morbidity. In a longitudinal study conducted by Schneider etal.[30] among 35,000 COPD patients followed up over a period of 10 years, the incidence of depression was 16.2 cases/1000 person-years in the COPD group. In addition, those with severe COPD were twice as likely to develop depression compared with patients having mild COPD.[31] We found the prevalence of anxiety/depression in 22% of our COPD patients. The PHQ-2 and the PHQ-3 from the PRIME MD[19] are screening tools for depression and anxiety, respectively. The overall sensitivity, specificity, and the accuracy were 83%, 88%, and 86%, respectively.[19] Due to this, the diagnosis made using these questionnaires was reliable at the level of sleep physician/pulmonologist. As the management of depression/anxiety is a prerogative of psychiatrists, we identified patients having depression/anxiety and then referred them to psychiatrist.
Besides these, COPD patients also report disturbed sleep because of nocturnal cough, dyspnea, wheeze, and pain.[13] We utilized Q10 in GSAQ for asking the COPD patients about these problems. We found that 16% had disturbed sleep either because of nocturnal cough, nocturnal dyspnea, or pain. Klink and Quan[3] found that nocturnal cough or wheezing was responsible for difficulty in initiating and maintaining of sleep in 39% of COPD patients. These problems are attributed to the underlying COPD and are generally not seen in the healthy population.
We grouped all the COPD patients enrolled as per the GOLD stages. There was a high likelihood of developing any of the sleep disorders in the group having FEV1< 50%. This finding can suggest that patients having a lower FEV1have a higher likelihood of developing sleep disorder. Some previous studies have also found that patients having more severe COPD have worse sleep.[8,32] Seeing individually, we found that patients having FEV1< 50% had a higher probability of developing RLS. There was no statistically significant difference among the patients having insomnia, OSA, and anxiety/depression.
Some patients had features of parasomnia or had unfavorable working hours. These factors also cause disturbed sleep. The common sleep disorders associated with COPD are insomnia, RLS, OSA, and anxiety/depression.[8] Epidemiological studies of parasomnia and shift worker disease have not shown any association with COPD.[33,34] Hence, both these seem to be unrelated to the presence of COPD in them. We propose a “modified GSAQ for COPD,” in which items pertaining to parasomnia and circadian rhythm disturbance [Box 1] may be deleted to make GSAQ more specific for identifying sleep disorders related to COPD. COPD patients suspected of having sleep disorders based on “modified GSAQ for COPD” can be referred to a pulmonologist dealing with sleep rather than only sleep a specialist. The sensitivity, specificity, and validity of this modified GSAQ for COPD remain an area of research.
Box 1.
The proposed modified global sleep assessment questionnaire
| Global sleep assessment questionnaire |
| 1. Do you have difficulty falling asleep, staying asleep, or do you feel poorly rested in the morning? |
| Never Sometimes Usually always |
| 2. Do you fall asleep unintentionally or fight to stay awake during the day? |
| Never Sometimes Usually always |
| 3. Do sleep difficulties or daytime sleepiness interfere with your daily activities? |
| Never Sometimes Usually always |
| 4.*Do work or other activities prevent you from getting enough sleep? |
| Never Sometimes Usually always |
| 5. Do you snore loudly? |
| Never Sometimes Usually always |
| 6. Do you hold your breath, have breathing pauses, or stop breathing in your sleep? |
| Never Sometimes Usually always |
| 7. Do you have restless or “crawling” feelings in your legs at night that go away if you move your legs? |
| Never Sometimes Usually always |
| 8. Do you have repeated rhythmic leg jerks or leg twitches during your sleep? |
| Never Sometimes Usually always |
| 9. *Do you have nightmares or do you scream, walk, punch or kick in your sleep? |
| Never Sometimes Usually always |
| 10. Do the following things disturb you in your sleep: Nocturnal cough, nocturnal dyspnea, chest pain/tightness, or wheezing? |
| Never Sometimes Usually always |
| 11. Do you feel sad or anxious? |
| Never Sometimes Usually always |
*Question pertaining to shift work disease (n=4) and parasomnia (n=9) which are unrelated to COPD can be deleted. COPD=Chronic obstructive pulmonary disease
There were few limitations to our study. The study had a small sample size. Inclusion of a larger sample would have better confirmed our findings. Nocturnal oxygen desaturation and hypoventilation were not evaluated in our study. Both of them can predispose to the disorders described. A study that comprehensively evaluates all sleep disorders in COPD and correlation with nocturnal oxygen desaturation and hypoventilation would be worthwhile. Another factor for sleep disturbance is nicotine use and withdrawal. Both these factors were also not evaluated in our study. Patients of depression/anxiety were diagnosed on PHQ-2 and PHQ-3, which is a useful diagnostic tool. Although the exact diagnosis is made by a psychiatrist, this was the best method we, as pulmonologists, could have used. The healthy individuals were not subjected to further evaluation because of logistic issues.
Conclusion
The presence of sleep disorders and disturbed sleep is significantly high in COPD patients. GSAQ has a good sensitivity for finding out the presence of disturbed sleep in COPD patients. Primary care physicians can easily use this questionnaire to rule out the presence of sleep disorders. Those who have a positive answer for any of the question should be referred to a specialist dealing with COPD and sleep. Those having a negative GSAQ score can be reasonably considered as not having any sleep disorders and need not be referred to a specialist.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fleetham JA. Is chronic obstructive pulmonary disease related to sleep apnea–hypopnea syndrome? AJRCCM. 2003;167:3–4. doi: 10.1164/rccm.2211003. [DOI] [PubMed] [Google Scholar]
- 2.Sleep Quality in COPD. [Last accessed on 2019 May 31]. Available from: http://www.thoracic.org/copd-guidelines/for-health-professionals/management-of-stable-copd/sleep/sleep-problems-in-copd.php .
- 3.Klink M, Quan SF. Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airway diseases. Chest. 1987;91:540–6. doi: 10.1378/chest.91.4.540. [DOI] [PubMed] [Google Scholar]
- 4.Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington DC: National Academies Press; 2006. pp. 67–209. [PubMed] [Google Scholar]
- 5.Kuppermann M, Lubeck DP, Mazonson PD, Patrick DL, Stewart AL, Buesching DP, et al. Sleep problems and their correlates in a working population. J Gen Intern Med. 1995;10:25–32. doi: 10.1007/BF02599573. [DOI] [PubMed] [Google Scholar]
- 6.Hatoum HT, Kong SX, Kania CM, Wong JM, Mendelson WB. Insomnia, health-related quality of life and healthcare resource consumption. A study of managed-care organisation enrollees. Pharmacoeconomics. 1998;14:629–37. doi: 10.2165/00019053-199814060-00004. [DOI] [PubMed] [Google Scholar]
- 7.Sateia MJ. International classification of sleep disorders-third edition: Highlights and modifications. Chest. 2014;146:1387–94. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 8.Budhiraja R, Siddiqi TA, Quan SF. Sleep disorders in chronic obstructive pulmonary disease: Etiology, impact, and management. J Clin Sleep Med. 2015;11:259–70. doi: 10.5664/jcsm.4540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 10.Douglass AB, Bornstein R, Nino-Murcia G, Keenan S, Miles L, Zarcone VP, Jr, et al. The Sleep Disorders Questionnaire. I: Creation and multivariate structure of SDQ. Sleep. 1994;17:160–7. doi: 10.1093/sleep/17.2.160. [DOI] [PubMed] [Google Scholar]
- 11.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 12.Roth T, Zammit G, Kushida C, Doghramji K, Mathias SD, Wong JM, et al. A new questionnaire to detect sleep disorders. Sleep Med. 2002;3:99–108. doi: 10.1016/s1389-9457(01)00131-9. [DOI] [PubMed] [Google Scholar]
- 13.Klingman KJ, Jungquist CR, Perlis ML. Questionnaires that screen for multiple sleep disorders. Sleep Med Rev. 2017;32:37–44. doi: 10.1016/j.smrv.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Global Strategy for Diagnosis, Management, and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017. [Last accessed on 2019 Sep 28]. Available from: http://goldcopd.org .
- 15.Netzer N, Eliasson AH, Netzer C, Kristo DA. Overnight pulse oximetry for sleep-disordered breathing in adults: A review. Chest. 2001;120:625–33. doi: 10.1378/chest.120.2.625. [DOI] [PubMed] [Google Scholar]
- 16.Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 17.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J, et al. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 19.Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 21.McNicholas WT, Verbraecken J, Marin JM. Sleep disorders in COPD: The forgotten dimension. Eur Respir Rev. 2013;22:365–75. doi: 10.1183/09059180.00003213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gothi D. Sleep disorders in chronic obstructive pulmonary disease. Indian J Sleep Med. 2015;10:11–21. [Google Scholar]
- 23.Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India. 2012;60:68–74. doi: 10.4103/0028-3886.93601. [DOI] [PubMed] [Google Scholar]
- 24.Pronzato C. Chronic obstructive pulmonary disease and obstructive sleep apnea. Association, consequences and treatment. Monaldi Arch Chest Dis. 2010;73:155–61. doi: 10.4081/monaldi.2010.285. [DOI] [PubMed] [Google Scholar]
- 25.Ohayon MM, O'Hara R, Vitiello MV. Epidemiology of restless legs syndrome: A synthesis of the literature. Sleep Med Rev. 2012;16:283–95. doi: 10.1016/j.smrv.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flenley DC. Sleep in chronic obstructive lung disease. Clin Chest Med. 1985;6:651–61. [PubMed] [Google Scholar]
- 27.Fleetham J, West P, Mezon B, Conway W, Roth T, Kryger M. Sleep, arousals, and oxygen desaturation in chronic obstructive pulmonary disease. The effect of oxygen therapy. Am Rev Respir Dis. 1982;126:429–33. doi: 10.1164/arrd.1982.126.3.429. [DOI] [PubMed] [Google Scholar]
- 28.Lo Coco D, Mattaliano A, Lo Coco A, Randisi B. Increased frequency of restless legs syndrome in chronic obstructive pulmonary disease patients. Sleep Med. 2009;10:572–6. doi: 10.1016/j.sleep.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 29.İn E, Turgut T, Özdemir C. Impact of restless legs syndrome on the sleep quality in chronic obstructive pulmonary disease. Eurasian J Pulmonol. 2016;18:18–23. [Google Scholar]
- 30.Schneider C, Jick SS, Bothner U, Meier CR. COPD and the risk of depression. Chest. 2010;137:341–7. doi: 10.1378/chest.09-0614. [DOI] [PubMed] [Google Scholar]
- 31.Atlantis E, Fahey P, Cochrane B, Smith S. Bidirectional associations between clinically relevant depression or anxiety and COPD: A systematic review and meta-analysis. Chest. 2013;144:766–77. doi: 10.1378/chest.12-1911. [DOI] [PubMed] [Google Scholar]
- 32.Vaidya S, Sah RB, Teotiya A, Gothi D. Evaluation of sleep disorders in chronic obstructive sleep disease patients by subjective questionnaire and their correlation with FEV1, PaO2 and PaCO2. Indian J Sleep Med. 2017;12:60–3. [Google Scholar]
- 33.Avidan AY, Kaplish N. The parasomnias: Epidemiology, clinical features, and diagnostic approach. Clin Chest Med. 2010;31:353–70. doi: 10.1016/j.ccm.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 34.Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC. Shift work and chronic disease: The epidemiological evidence. Occupational Med. 2011;61:78–89. doi: 10.1093/occmed/kqr001. [DOI] [PMC free article] [PubMed] [Google Scholar]


