Abstract
Mortality associated with the acute respiratory distress syndrome remains unacceptably high due in part to ventilator-induced lung injury (VILI). Ventilator dyssynchrony is defined as the inappropriate timing and delivery of a mechanical breath in response to patient effort and may cause VILI. Such deleterious patient–ventilator interactions have recently been termed patient self-inflicted lung injury. This narrative review outlines the detection and frequency of several different types of ventilator dyssynchrony, delineates the different mechanisms by which ventilator dyssynchrony may propagate VILI, and reviews the potential clinical impact of ventilator dyssynchrony. Until recently, identifying ventilator dyssynchrony required the manual interpretation of ventilator pressure and flow waveforms. However, computerized interpretation of ventilator waive forms can detect ventilator dyssynchrony with an area under the receiver operating curve of >0.80. Using such algorithms, ventilator dyssynchrony occurs in 3%–34% of all breaths, depending on the patient population. Moreover, two types of ventilator dyssynchrony, double-triggered and flow-limited breaths, are associated with the more frequent delivery of large tidal volumes >10 mL/kg when compared with synchronous breaths (54% [95% confidence interval (CI), 47%–61%] and 11% [95% CI, 7%–15%]) compared with 0.9% (95% CI, 0.0%–1.9%), suggesting a role in propagating VILI. Finally, a recent study associated frequent dyssynchrony-defined as >10% of all breaths-with an increase in hospital mortality (67 vs. 23%, P = 0.04). However, the clinical significance of ventilator dyssynchrony remains an area of active investigation and more research is needed to guide optimal ventilator dyssynchrony management.
Keywords: Acute respiratory distress syndrome, patient self-inflicted lung injury, ventilator dyssynchrony, ventilator-induced lung injury
Despite significant advances in ventilator management, mortality from the acute respiratory distress syndrome (ARDS, see [Supplementary Table] for list of abbreviations) remains unacceptably high.[1] Mechanical ventilation can injure the lung through parenchymal overdistension (volutrauma and barotrauma), cyclic alveolar collapse and reopening (atelectrauma), and inflammatory effects (biotrauma).[2] In at-risk patients, ventilator-induced lung injury (VILI) can increase susceptibility to develop ARDS. In patients with ARDS, VILI increases mortality.[3] Low-tidal-volume mechanical ventilation is one method to reduce VILI, decrease pulmonary complications in those at-risk for ARDS, and improve mortality in patients with ARDS.[4,5,6,7,8] However, low-tidal-volume ventilation alone does not eliminate VILI. Patient interaction with the ventilator, specifically the inappropriate timing and delivery of a mechanical breath in response to patient effort–termed ventilator dyssynchrony (VD) - likely further potentiates VILI.[9] These deleterious patient–ventilator interactions have recently been termed patient self-inflicted lung injury (P-SILI) and reducing such interactions to prevent volutrauma, barotrauma, atelectrauma, and biotrauma has been an active area of research and ventilator design for over 30 years.[10,11]
Supplementary Table
| Abbreviation | Definition |
|---|---|
| APVCMV | Adaptive pressure ventilation continuous mandatory ventilation |
| ARDS | Acute respiratory distress syndrome |
| EIT | Electrical impendence tomography |
| ICU | Intensive care unit |
| IPS | Inspiratory pressure support |
| PAV | Proportional-assist ventilation |
| Paw | Airway pressure |
| PBW | Predicted body weight |
| Pcap | Capillary pressure |
| PCV | Pressure-controlled ventilation |
| PEEP | Positive end-expiratory pressure |
| PL | Transpulmonary pressure |
| Ppl | Pleural pressure |
| Pplat | Plateau pressure |
| P-SILI | Patient self-inflicted lung injury |
| PSV | Pressure support ventilation |
| RASS | Richmond agitation and sedation scale |
| VCV | Volume-controlled ventilation |
| VILI | Ventilator-induced lung injury |
This narrative review defines several different types of ventilator dyssynchrony, outlines the growing ability to detect ventilator dyssynchrony using computerized algorithms, and describes the frequency of ventilator dyssynchrony in different patient populations. We then delineate the different mechanisms by which ventilator dyssynchrony may propagate VILI, reviewing data from both animal and human studies. In addition, we review the potential clinical impact of ventilator dyssynchrony and the efficacy of different interventions to manage ventilator dyssynchrony. Finally, we explore what future studies are necessary to integrate the management of ventilator dyssynchrony into clinical practice to reduce VILI and hopefully improve patient outcomes.
Methods
We performed a narrative review. A literature search of PubMed using the terms “ventilator dyssynchrony,” “ventilator asynchrony,” and “patient-ventilator interactions” was performed. Only English language articles were included. A total of 69 articles were reviewed.
Defining Ventilator Dyssynchrony
There are multiple types of ventilator dyssynchrony (VD) that have been extensively described elsewhere.[9,12,13,14,15,16,17,18] In general, the field is troubled by varying and inconsistent nomenclatures. However, defining the driving mechanism helps categorize the varying types of dyssynchrony. Thus, ventilator dyssynchrony can be divided into triggering dyssynchronies, flow dyssynchronies, and cycling dyssynchronies. Trigger dyssynchronies include double-triggered, reverse-triggered, auto-triggered, and ineffective triggered breaths.[19] Double-triggered breaths occur when high patient inspiratory effort continues into the expiratory cycle of the ventilator and triggers a second breath before complete exhalation. Substantial patient effort and flow limitation may lead to a double-triggered breath. Importantly, other types of ventilator dyssynchrony, such as reverse-triggered or premature cycling dyssynchronies, are subtly different from a double-triggered dyssynchrony. Reverse-triggered breaths are a form of entrainment and result from a mandatory, ventilator-delivered breath triggering a reflexive diaphragmatic contraction resulting in inspiration, typically seen with deep sedation or neurological injury.[20,21] Auto-triggered breaths occur when flow or pressure changes not related to patient effort trigger a breath, as seen with an air leak or the buildup of secretions in the ventilator circuit. Ineffective triggered breaths occur when patient effort is not enough to trigger a ventilator breath. Flow dyssynchronies include flow-limited breaths where the support delivered by the ventilator does not meet the patient's inspiratory demand. Finally, cycling dyssynchronies include premature and delayed cycling. These occur when the patient's and ventilator's inspiratory times do not match, causing alterations at the end of inspiration and the begging of expiration [Figure 1].
Figure 1.
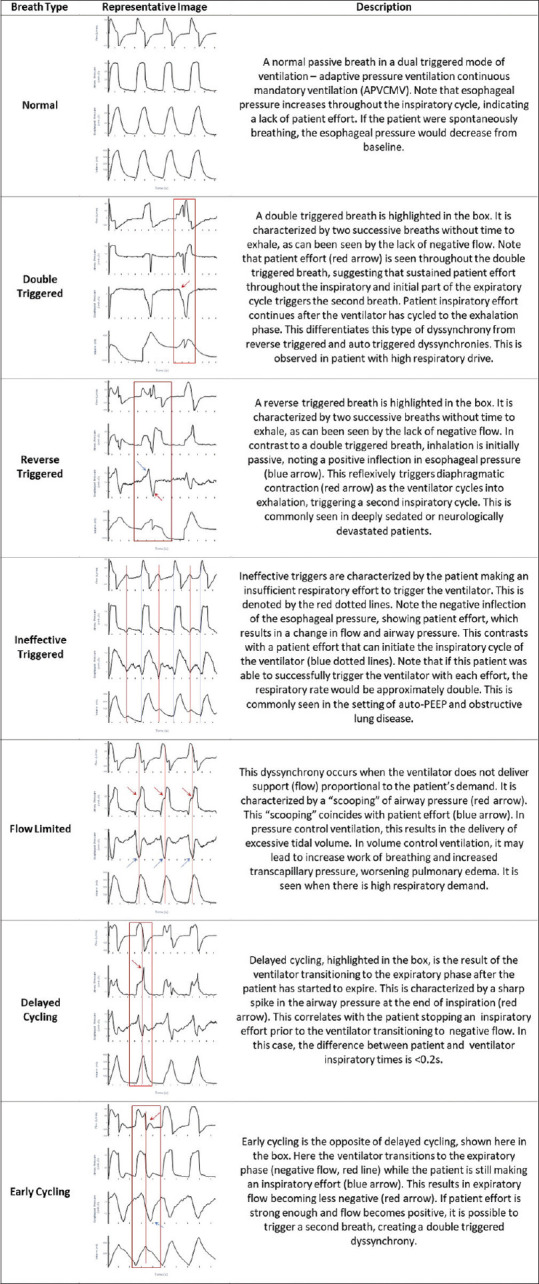
Representative types of ventilator dyssynchrony – Examples of some types of commonly observed ventilator dyssynchronies. All examples demonstrate flow (L/min), airway pressure (cm H2O), esophageal pressure (cm H2O), and volume (ml)
Detecting Ventilator Dyssynchrony
Until recently, ventilator dyssynchrony was difficult to monitor and required the manual interpretation of ventilator pressure and flow waveforms. In clinical practice, ventilator waveforms are often underutilized to monitor patient–ventilator interactions.[22,23,24,25] Moreover, manual review of standard pressure and flow waveforms at bedside is fraught with inaccuracies. Waveform interpretation is complicated by noisy signals, complex combinations of ventilator dyssynchrony, and multiple modes of ventilation. Moreover, a patient's clinical status is continuously changing, resulting in varying types and frequency of ventilator dyssynchrony over time. In one study, physicians identified ventilator dyssynchrony with only 16%–28% sensitivity.[26] Like physicians, nurses and respiratory therapists also face challenges with bedside waveform analysis to detect ventilator dyssynchrony.[27,28] Experts in the field are considered the gold standard at detecting ventilator dyssynchrony in these studies, but even so, the manual analysis of over 20,000 breaths per day for a single patient is simply too time intensive for systematic analysis and routine clinical utility.
Consequently, computerized algorithms to identify ventilator dyssynchrony from flow and pressure waveforms have been developed. Gutierrez et al. initially showed that differences between synchronous and dyssynchronous breaths could be detected by spectral analysis, but did not utilize this technique to detect differed types of ventilator dyssynchrony.[29] Blanch et.al., later validated a computerized model to detect ineffective triggered breaths with a sensitivity of 65.2% and specificity of 73.9%, demonstrating that computers could accurately detect specific types of ventilator dyssynchrony.[30,31] Building on the work of Gholami[32] and Mulqueeny,[33] Sottile et al. utilized machine learning to accurately detect three types of ventilator dyssynchrony, building a frame work that is easily expanded to detect additional types of ventilator dyssynchrony.[34] Using this framework, the authors were able to detect double-triggered, flow-limited, ineffective triggered, and synchronous breaths with an area under the receiver operating curve of >0.80, a similar or better accuracy to that reported by Blanch.[30,31] These computerized detection methods, though, are still limited in detecting ventilator dyssynchrony as they utilize only pressure and flow waveforms generated from the ventilator. Consequently, accurate detection is still limited for some types of ventilator dyssynchrony, such as auto-triggered, reverse-triggered, and cycling dyssynchronies that require additional forms of monitoring, either esophageal manometry or electrical monitoring of diaphragmatic activity, for accurate identification [Figure 1].[18,35]
Frequency of Ventilator Dyssynchrony
Despite these limitations, computerized detection of ventilator dyssynchrony has allowed for the systematic study of ventilator dyssynchrony to determine its prevalence in various disease states and modes of ventilation. At least seven studies have described the prevalence of ventilator dyssynchrony in different patient cohorts and various modes of ventilation over varying lengths of time [Table 1]. Initial studies evaluated patients for limited periods of time and concluded that ventilator dyssynchrony was common, seen in 4%–40% of all breaths, and is present in all patients.[36,37,38,39,40] Ineffective trigged breaths and double-triggered breaths were the most commonly observed types of ventilator dyssynchrony.
Table 1.
Frequency of ventilator dyssynchrony in reported literature
| Author | Patient type | Mode of ventilation | Types of VD | Frequency (%) |
|---|---|---|---|---|
| Fabry 1996 | Respiratory failure 5 min samples 11 patients |
IPS | IEE | 20.0 (0.0-40) |
| Thille 2006 | Respiratory failure 30 min samples 62 patients |
Any | All | 2.1 (0.7-8.6) |
| VCV | All | 4.3±4.8 | ||
| IEE | 3.0±4.9 | |||
| Double triggered | 1.2±2.3 | |||
| PSV | All | 1.9±3.8 | ||
| IEE | 1.8±3.7 | |||
| Doubled triggered | 0.1±0.4 | |||
| Pohlman 2008 | ARDS 5 min samples 20 patients |
VCV | Double triggered | 9.7±15.2 |
| De Wit 2009 | Respiratory failure 15 min samples 35 observations |
Any | All | 11±14 |
| IEE | 9±12 | |||
| Double triggered | 5.8 | |||
| Short cycled | 5.6 | |||
| Mellot 2014 | Respiratory failure 90 min samples 30 patients |
Any | All | 23.3 |
| IEE | 14.7 | |||
| Double triggered | 0.17 | |||
| Flow limited | 0.20 | |||
| Premature cycling | 2.14 | |||
| Delayed cycling | 0.02 | |||
| Blanch 2015 | Respiratory failure Continuous samples 50 patients |
Any | All | 3.41 (1.95-5.77) |
| VCV | All | 1.49 (0.32-4.68) | ||
| IEE | 0.91 (0.15-3.36) | |||
| Double triggered | 0.06 (0.00-0.29) | |||
| PCV | All | 1.69 (0.54-4.37) | ||
| IEE | 0.98 (0.23-3.32) | |||
| Double triggered | 0.11 (0.00-0.44) | |||
| PSV | All | 2.15 (0.90-4.74) | ||
| IEE | 1.18 (0.49-2.96) | |||
| Double triggered | 0.12 (0.00-0.32) | |||
| Sottile 2018 | Acute hypoxic respiratory failure Continuous samples 62 patients |
APVCMV/PCV | All | 34.4 (34.4-34.5) |
| IEE | 24.8 (24.2-25.0) | |||
| Double triggered | 3.12 (3.1-3.14) | |||
| Flow limited | 13.6 (13.56-13.64) |
The measured frequency of all ventilator dyssynchrony and specific sub-types of ventilator dyssynchrony in the landmark studies today, as a function of ventilator mode. IPS=Inspiratory pressure support, VCV=Volume-controlled ventilation, PCV=Pressure-controlled ventilation, PSV=Pressure support ventilation, APVCMV=Adaptive pressure ventilation continuous mandatory ventilation
More recent studies have utilized the ability to analyze continuous ventilator waveforms. In one study of 50 patients, over 8 million breaths were recorded and analyzed for the presence of ineffective triggered breaths and double-triggered breaths in volume-controlled, pressure-controlled, and pressure support modes of mechanical ventilation.[31] The authors confirmed that ventilator dyssynchrony occurred in all patients and was frequent, occurring in over 3% of breaths. Ineffective triggered breaths were the most common type of ventilator dyssynchrony in all modes of ventilation. While the rate of ventilator dyssynchrony was similar between pressure-controlled and volume-controlled modes of ventilation, ineffective triggered breaths were observed more frequently in pressure support ventilation (PSV) than in other modes of ventilation. Consequently, PSV was associated with a significant increase in the overall rate of ventilator dyssynchrony when compared to control modes of ventilation. Moreover, Blanch, etal. detected significant diurnal variation in the frequency of ventilator dyssynchrony, with ventilator dyssynchrony being more frequent at night.
Finally, in a study of 62 patients with ARDS or ARDS risk factors, ventilator dyssynchrony was seen in all patients and in 34.4% of breaths. Ineffective triggered breaths remained the most common type of dyssynchrony, seen in 24% of all breaths. Flow-limited breaths were the second most common, seen in 13% of breaths. Double-triggered breaths accounted for 3% of all breaths. Overall ventilator dyssynchrony was seen far more frequently than in prior studies. Patients in this study were generally quite ill, with an average PaO2-to-FiO2(P: F) ratio of 139 ± 68, perhaps explaining the increase frequency of ventilator dyssynchrony. Interestingly, most patients were ventilated in a proprietary dual-triggered mode of ventilation, adaptive pressure ventilation continuous mandatory ventilation, followed by pressure-controlled ventilation and volume-controlled modes of ventilation. Such dual-triggered modes of ventilation were previously hypothesized to improve patient comfort and potentially decrease some types of ventilator dyssynchrony, yet ventilator dyssynchrony was still frequently observed.
Pathophysiology of Ventilator Dyssynchrony
In practice, ventilator dyssynchrony is assumed to cause P-SILI, increase respiratory muscle work, increase patient discomfort, and delay extubation.[18,41] However, the mechanisms by which ventilator dyssynchrony propagates lung injury and the relative potential of each type of ventilator dyssynchrony to generate P-SILI remain unknown. Initial human and animal studies have started to shed light on these issues.
Indeed, some types of ventilator dyssynchrony are associated with the delivery of large-tidal-volume breaths that, in the context of VILI, are linked to worse outcomes.[4] Pohlman etal. showed that double-triggered breaths were associated with a significant increase in delivered tidal volume – 10.1 (8.8–10.7) ml/kg of predicted body weight (PBW) in double-triggered breaths versus 5.9 (5.7–6.2) ml/kg PBW in synchronous breaths.[40] Similarly, Beitler found in 33 patients with ARDS receiving low-tidal-volume ventilation that double-triggered breaths were associated with tidal volumes of 11.3 (9.7–13.3) ml/kg PBW.[42] Sottile et al. have shown that double-triggered and flow-limited breaths were associated with larger than expected tidal volumes in patients with ARDS or ARDS risk factors receiving low-tidal-volume ventilation (11.95 [11.06–12.85] ml/kg PBW and 7.44 [7.0–7.8] ml/kg PBW vs. 6.2 ml/kg PBW, respectively). Moreover, double-triggered and flow-limited breaths were associated with the more frequent delivery of large tidal volumes >10 mL/kg when compared with synchronous breaths (54% [95% confidence interval (CI), 47%–61%] and 11% [95% CI, 7%–15%] compared with 0.9% [95% CI, 0.0%–1.9%]).[34] Unique to this study, most patients were ventilated in a dual-triggered mode of ventilation, where variable patient effort can result in varying delivered tidal volumes, explaining how flow-limited breaths could result in the delivery of excessive tidal volumes. In aggregate, these data suggest a mechanism whereby multiple types of ventilator dyssynchrony, not only double-triggered breaths, may deliver large tidal volumes and cause P-SILI.
Ventilator dyssynchrony is associated with additional mechanisms that propagate lung injury in addition to delivering large tidal volumes. The stress applied to the lung tissue is the pressure distending the lung or the transpulmonary pressure (PL). Transpulmonary pressure is the difference between airway pressure (Paw) and the pressure in the pleural space (Ppl). Assuming normal chest wall compliance during positive-pressure ventilation in the absence of patient effort, Paw constitutes the majority of PL. PL is, therefore, often clinically estimated as the Paw at the end of inspiration, more commonly referred to as the plateau pressure (Pplat). However, during spontaneous effort, Ppl may be strongly negative and thus contribute significantly to PL, resulting in barotrauma.[43] However, human data are lacking. Yoshida et al. demonstrated that esophageal pressure, a clinical surrogate for Ppl, was more negative when rabbits made spontaneous effort during both volume- and pressure-controlled ventilation. This respiratory effort consequently resulted in increased PL in pressure-controlled ventilation [Figure 2].[44,45] Moreover, strong respiratory effort in rabbits receiving moderate-tidal-volume ventilation was associated with PL>33 cm H2O, despite observing “safe” plateau pressures <30 cm H2O. These animals had worse histopathological findings of ARDS on necropsy.[46] Since some types of ventilator dyssynchrony are associated with vigorous patient effort, we can infer from animal studies that ventilator dyssynchrony may generate large and potentially damaging PL in patients as well. Moreover, the clinical importance of patient effort and ventilator dyssynchrony may be closely intertwined with the degree of lung injury, such that ventilator dyssynchrony only causes P-SILI if the lung is already severely injured.
Figure 2.
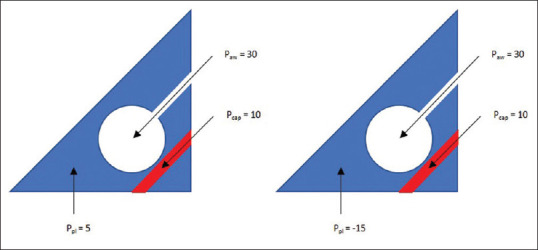
Examples of transpulmonary pressures with and without spontaneous effort – During a pressure- or volume-controlled mechanical breath in a paralyzed patient (left), the transpulmonary pressure is the difference between the airway pressure and pleural pressures (25 = 30 - 5) and transvascular pressure is the difference between the capillary pressure and pleural pressures (5=10-5). In a spontaneously breathing mechanically ventilated patient (right), airway pressure is constant but pleural pressure is negative. This results in both increased transpulmonary pressure (45 = 30--15) and transvascular pressures (25=10--15), which may worsen lung injury and pulmonary edema. Paw: Airway pressure, Ppl: Pleural pressure, Pcap: Capillary pressure, PL: Transpulmonary pressure
Finally, the pressure distribution in the injured lung is heterogeneous, contributing to regional VILI. In animal models using electrical impendence tomography, spontaneous breaths resulted in hyperinflation and potential volutrauma in dependent lung regions. Hyperinflation may be caused by a pendelluft phenomenon, as they noted a decrease in volume in the nondependent portions of the lung when total lung volume remained constant. This phenomenon increased linearly with increasing spontaneous effort and was reduced two-fold by neuromuscular blockade and paralysis.[44,47,48] Similar pathophysiology has been observed in humans as a consequence of reverse triggering dyssynchrony.[49] In addition, vigorous patient effort may be associated with increased pulmonary edema and lead to increasing lung injury. This observation may be explained by a strongly negative Ppl resulting in strongly negative transvascular pressure that promotes fluid exudation into the alveolar space [Figure 2].[50]
Clinical Impact of Ventilator Dyssynchrony
The clinical impact of ventilator dyssynchrony and its potential to worsen lung injury and patient outcomes remains poorly defined. Ventilator dyssynchrony has been associated with increased length of stay and worse mortality. However, in a study of 103 patients, Rolland-Debord et al. found no difference in ventilator days, intensive care unit (ICU) days, hospital days, or mortality between patients with >10% or <10% dyssynchronous breaths during weaning.[35] However, these observations occurred later in the course of critical illness. When studied earlier in a patient's course, ventilator dyssynchrony is associated with worse clinical outcomes. de Wit etal. evaluated the presence of ineffective triggered breaths in 60 patients within 24 h of intubation. In patients with >10% dyssynchronous breaths, ventilator dyssynchrony was associated with increased duration of mechanical ventilation, ICU stay, and hospital stay, as well as a lower likelihood of being discharged home despite having similar mortality.[51] Similarly, both Thille et al. and Gogineni et al. confirmed that frequent ventilator dyssynchrony early in the course of mechanical ventilation was associated with longer duration of mechanical ventilation.[36,52] Thille et al. also noted a greater incidence of tracheostomy, but no difference in mortality in patients with frequent ventilator dyssynchrony.[36] Finally, Blanch studied the presence of ventilator dyssynchrony in 50 patients for their entire hospital course and found that >10% of dyssynchronous breaths was associated with an increase in hospital mortality (67% vs. 23%, P = 0.04), while there was no difference in reintubation, tracheostomy, or duration of mechanical ventilation.[31]
Management of Ventilator Dyssynchrony
The optimum management of ventilator dyssynchrony is debated. Potential interventions include altering ventilator parameters, changing the mode of ventilation, optimizing sedation, or utilizing neuromuscular blockade.
Optimizing ventilator settings would appear to be the safest method to decrease ventilator dyssynchrony. Indeed, Pohlman etal. demonstrated that increasing tidal volume by 1 ml/kg PBW decreased the odds of double-triggered breaths by 60% in 20 patients with ARDS receiving low-tidal-volume ventilation and deep sedation.[40] An observational study of 30 patients by Chanques etal. identified that increasing inspiratory time was independently associated with almost eliminating double-triggered breaths.[53] Similarly, MacIntyre etal. showed that increasing ventilator flow decreased flow-limited dyssynchrony in 16 patients.[54] Moreover, positive end-expiratory pressure (PEEP) is known to decrease ineffective triggered breaths when there is significant auto-PEEP from obstructive lung disease.[55,56] In practice, though, identifying the optimal ventilator settings requires systematic evaluation of patient-ventilator interactions. The combination of ventilator parameters that optimally reduces ventilator dyssynchrony when balancing potentially deleterious changes, such as an increase in tidal volume, remains unknown and is likely different for each patient. Finally, ventilator changes that reduce one type of ventilator dyssynchrony may inadvertently increase other types of ventilator dyssynchrony. For example, decreasing flow rate to lengthen the inspiratory time, thereby improving cycling dyssynchronies, may increase flow dyssynchronies. This decision is additionally challenging because it is not currently known which types of ventilator dyssynchrony are more injurious.
Moreover, in the last several decades, a plethora of ventilator modes have been developed to try and reduce ventilator dyssynchrony. Chanques etal. demonstrated that changing to PSV was independently associated with near elimination of double-triggered breaths. However, changing the ventilator mode to PSV was also associated with a median increase of 4 ml/kg PBW in tidal volume, which may further drive lung injury via volutrauma.[53] In addition, Blanch demonstrated that ineffective triggered breaths were seen most commonly in PSV when compared to other modes of ventilation. Several studies have evaluated the effective of dual control modes of ventilation (i.e., proprietary modes such as pressure-regulated volume control). MacIntyre etal. demonstrated that changing to a dual-triggered mode of ventilation decreased, but did not eliminate, flow-limited dyssynchrony in 16 patients.[54] Similarly, Figueroa-Casasand Montoya investigated the utility of switching from traditional volume-controlled modes of ventilation to a dual-triggered mode of ventilation to reduce ventilator dyssynchrony in 19 patients. For the same tidal volume, patients ventilated with a dual-triggered mode of ventilation manifest less ventilator dyssynchrony. In addition, in either mode of ventilation, patients ventilated with larger tidal volumes had less ventilator dyssynchrony.[57] However, such modes of ventilation allow for the delivery of large-tidal-volume breaths with increased respiratory drive so that additional P-SILI may negate the benefit of reduced ventilator dyssynchrony.[34] Finally, newer mode of ventilation such as proportional-assist ventilation (PAV) has theoretical benefits that may reduce ventilator dyssynchrony, but in small studies to date, similar rate of ventilator dyssynchrony has been seen between PSV and PAV.[58,59] Thus, there is no clear optimal mode of ventilation to manage ventilator dyssynchrony.
The effects of sedation on ventilator dyssynchrony are similarly complex. Chanques etal. found that increasing sedation was associated with an absolute reduction of 14% in double-triggered breaths.[53] However, de Witt etal. investigated the frequency of ineffective triggered breaths as related to sedation score and demonstrated that increasing sedation was associated with an increased frequency of ineffective triggered breaths.[37] Sottile etal. evaluated the effect of Richmond Agitation and Sedation Scale score and neuromuscular blockade on the frequency of ventilator dyssynchrony in 62 patients. Double-triggered, flow-limited, and ineffective triggered breaths were all reduced with deep sedation compared to patients with lighter sedation. Moreover, neuromuscular blockade effectively eliminated all types of ventilator dyssynchrony.[34,43] However, the use of deep sedation and neuromuscular blockade to reduce or eliminate ventilator dyssynchrony must be balanced against the deleterious side effects of sedation and neuromuscular blockade, such as diaphragmatic weakness and generalized deconditioning. Deep sedation has been associated with longer duration of mechanical ventilation.[60] Moreover, the type of neuromuscular blockade agent may have impact on patient outcomes. In patients who required neuromuscular blockade, Sottile etal. reported that cisatracurium when compared to vecuronium was associated with fewer ventilator days, shorter hospitalization, and greater odds of being discharged to home.[61] However, even when using cisatracurium, patients treated with 48 h of neuromuscular blockade had no difference in 120 days mortality.[62] Consequently, the optimal use of sedation and neuromuscular blockade to minimize ventilator dyssynchrony and improve overall patient outcomes remains unknown.
Future Directions
Ventilator dyssynchrony is common, has multiple mechanisms, and is correlated with worse patient outcomes. The first step in improving management of ventilator dyssynchrony is the development of reliable and simple means of monitoring the dyssynchrony patterns illustrated in Figure 1 and integrating this technology into clinical ventilators. These systems for identifying ventilator dyssynchrony may need to incorporate esophageal manometry or electrical monitoring of diaphragmatic activity to provide sufficient fidelity to identify additional types of ventilator dyssynchrony. These monitors require specialized knowledge and integration with ventilator data, so this is an ideal opportunity to apply computerized methods to detect ventilator dyssynchrony.[63]
In addition, more data are needed to delineate the relative importance of each type of ventilator dyssynchrony to propagate P-SILI. This is similar to the concept of an injury cost function in VILI that quantifies the amount of damage caused by the mechanical ventilator.[64,65] Developing a P-SILI cost function that describes injury resulting from ventilator dyssynchrony will guide decisions to balance the prevention of ventilator dyssynchrony against the potential cost of interventions, such as VILI resulting from increased tidal volume.[65,66,67] Because data from animal models and clinical trials suggest that spontaneous effort may only been harmful in moderate-to-severe ARDS, the P-SILI cost function should be based on the underlying lung physiology to allow personalized predictions of the threshold for ventilator dyssynchrony intervention.[68]
Finally, many of the potential interventions can decrease one type of ventilator dyssynchrony while increasing others. In the case of sedation and neuromuscular blockade, there intervention may even have systemic effects beyond the lungs. Balancing the potential negative side effects of these interventions compared to the benefit of reducing P-SILI requires a careful cost–benefit analysis. To make this decision, it will be necessary to understand the patient's clinical trajectory, the degree of underlying lung injury, and the amount of injury caused by ventilator dyssynchrony (the P-SILI cost function) to determine when and which interventions are necessary to optimize an individual patient's treatment. It is likely that computer algorithms will be necessary to balance these conflicting requirements for each patient in real time and guide the clinical team to optimize patient management. Once developed, this computer-guided care can then be compared to usual care in large randomized controlled trials powered to reduce mortality in ARDS. Such a system has the potential to improve mechanical ventilation by advancing the tenants of low-tidal-volume ventilation and lung-protective ventilations initially developed by the ARDS network in a personalized manner.
Financial support and sponsorship
NIH K23 5K23HL145011.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 2.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis. 1974;110:556–65. doi: 10.1164/arrd.1974.110.5.556. [DOI] [PubMed] [Google Scholar]
- 3.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369:2126–36. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 4.Acute Respiratory Distress Syndrome Network. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 5.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 6.Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37. doi: 10.1056/NEJMoa1301082. [DOI] [PubMed] [Google Scholar]
- 7.Guay J, Ochroch EA. Intraoperative use of low volume ventilation to decrease postoperative mortality, mechanical ventilation, lengths of stay and lung injury in patients without acute lung injury. Cochrane Database Syst Rev. 2018;9:7. doi: 10.1002/14651858.CD011151.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Determann RM, Royakkers A, Wolthuis EK, Vlaar AP, Choi G, Paulus F, et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: A preventive randomized controlled trial. Crit Care. 2010;14:R1. doi: 10.1186/cc8230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilstrap D, MacIntyre N. Patient-ventilator interactions. Implications for clinical management. Am J Respir Crit Care Med. 2013;188:1058–68. doi: 10.1164/rccm.201212-2214CI. [DOI] [PubMed] [Google Scholar]
- 10.MacIntyre N, Nishimura M, Usada Y, Tokioka H, Takezawa J, Shimada Y. The Nagoya conference on system design and patient-ventilator interactions during pressure support ventilation. Chest. 1990;97:1463–6. doi: 10.1378/chest.97.6.1463. [DOI] [PubMed] [Google Scholar]
- 11.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–42. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 12.Dres M, Rittayamai N, Brochard L. Monitoring patient-ventilator asynchrony. Curr Opin Crit Care. 2016;22:246–53. doi: 10.1097/MCC.0000000000000307. [DOI] [PubMed] [Google Scholar]
- 13.Branson RD, Blakeman TC, Robinson BR. Asynchrony and dyspnea. Respir Care. 2013;58:973–89. doi: 10.4187/respcare.02507. [DOI] [PubMed] [Google Scholar]
- 14.Murias G, Lucangelo U, Blanch L. Patient-ventilator asynchrony. Curr Opin Crit Care. 2016;22:53–9. doi: 10.1097/MCC.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 15.Pham T, Telias I, Piraino T, Yoshida T, Brochard LJ. Asynchrony consequences and management. Crit Care Clin. 2018;34:325–41. doi: 10.1016/j.ccc.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Tobin MJ, Jubran A, Laghi F. Patient-ventilator interaction. Am J Respir Crit Care Med. 2001;163:1059–63. doi: 10.1164/ajrccm.163.5.2005125. [DOI] [PubMed] [Google Scholar]
- 17.Murias G, Villagra A, Blanch L. Patient-ventilator dyssynchrony during assisted invasive mechanical ventilation. Minerva Anestesiol. 2013;79:434–44. [PubMed] [Google Scholar]
- 18.Epstein SK. How often does patient-ventilator asynchrony occur and what are the consequences? Respir Care. 2011;56:25–38. doi: 10.4187/respcare.01009. [DOI] [PubMed] [Google Scholar]
- 19.Sassoon CS. Triggering of the ventilator in patient-ventilator interactions. Respir Care. 2011;56:39–51. doi: 10.4187/respcare.01006. [DOI] [PubMed] [Google Scholar]
- 20.Delisle S, Charbonney E, Albert M, Ouellet P, Marsolais P, Rigollot M, et al. Patient-ventilator asynchrony due to reverse triggering occurring in brain-dead patients: clinical implications and physiological meaning. Am J Respir Crit Care Med. 2016;194:1166–8. doi: 10.1164/rccm.201603-0483LE. [DOI] [PubMed] [Google Scholar]
- 21.Akoumianaki E, Lyazidi A, Rey N, Matamis D, Perez-Martinez N, Giraud R, et al. Mechanical ventilation-induced reverse-triggered breaths: A frequently unrecognized form of neuromechanical coupling. Chest. 2013;143:927–38. doi: 10.1378/chest.12-1817. [DOI] [PubMed] [Google Scholar]
- 22.Nilsestuen JO, Hargett KD. Using ventilator graphics to identify patient-ventilator asynchrony. Respir Care. 2005;50:202–34. [PubMed] [Google Scholar]
- 23.Kondili E, Xirouchaki N, Georgopoulos D. Modulation and treatment of patient-ventilator dyssynchrony. Curr Opin Crit Care. 2007;13:84–9. doi: 10.1097/MCC.0b013e328011278d. [DOI] [PubMed] [Google Scholar]
- 24.Hess DR. Ventilator waveforms and the physiology of pressure support ventilation. Respir Care. 2005;50:166–86. [PubMed] [Google Scholar]
- 25.Georgopoulos D, Prinianakis G, Kondili E. Bedside waveforms interpretation as a tool to identify patient-ventilator asynchronies. Intensive Care Med. 2006;32:34–47. doi: 10.1007/s00134-005-2828-5. [DOI] [PubMed] [Google Scholar]
- 26.Colombo D, Cammarota G, Alemani M, Carenzo L, Barra FL, Vaschetto R, et al. Efficacy of ventilator waveforms observation in detecting patient-ventilator asynchrony. Crit Care Med. 2011;39:2452–7. doi: 10.1097/CCM.0b013e318225753c. [DOI] [PubMed] [Google Scholar]
- 27.Ramirez II, Arellano DH, Adasme RS, Landeros JM, Salinas FA, Vargas AG, et al. Ability of ICU health-care professionals to identify patient-ventilator asynchrony using waveform analysis. Respir Care. 2017;62:144–9. doi: 10.4187/respcare.04750. [DOI] [PubMed] [Google Scholar]
- 28.Chacón E, Estruga A, Murias G, Sales B, Montanya J, Lucangelo U, et al. Nurses' detection of ineffective inspiratory efforts during mechanical ventilation. Am J Crit Care. 2012;21:e89–93. doi: 10.4037/ajcc2012108. [DOI] [PubMed] [Google Scholar]
- 29.Gutierrez G, Ballarino GJ, Turkan H, Abril J, de La Cruz L, Edsall C, et al. Automatic detection of patient-ventilator asynchrony by spectral analysis of airway flow. Crit Care. 2011;15:R167. doi: 10.1186/cc10309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blanch L, Sales B, Montanya J, Lucangelo U, Garcia-Esquirol O, Villagra A, et al. Validation of the Better Care® system to detect ineffective efforts during expiration in mechanically ventilated patients: A pilot study. Intensive Care Med. 2012;38:772–80. doi: 10.1007/s00134-012-2493-4. [DOI] [PubMed] [Google Scholar]
- 31.Blanch L, Villagra A, Sales B, Montanya J, Lucangelo U, Luján M, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015;41:633–41. doi: 10.1007/s00134-015-3692-6. [DOI] [PubMed] [Google Scholar]
- 32.Gholami B, Phan TS, Haddad WM, Cason A, Mullis J, Price L, et al. Replicating human expertise of mechanical ventilation waveform analysis in detecting patient-ventilator cycling asynchrony using machine learning. Comput Biol Med. 2018;97:137–44. doi: 10.1016/j.compbiomed.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 33.Mulqueeny Q, Redmond SJ, Tassaux D, Vignaux L, Jolliet P, Ceriana P, et al. Automated detection of asynchrony in patient-ventilator interaction. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:5324–7. doi: 10.1109/IEMBS.2009.5332684. [DOI] [PubMed] [Google Scholar]
- 34.Sottile PD, Albers D, Higgins C, Mckeehan J, Moss MM. The association between ventilator dyssynchrony, delivered tidal volume, and sedation using a novel automated ventilator dyssynchrony detection algorithm. Crit Care Med. 2018;46:e151–7. doi: 10.1097/CCM.0000000000002849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rolland-Debord C, Bureau C, Poitou T, Belin L, Clavel M, Perbet S, et al. Prevalence and prognosis impact of patient-ventilator asynchrony in early phase of weaning according to two detection methods. Anesthesiology. 2017;127:989–97. doi: 10.1097/ALN.0000000000001886. [DOI] [PubMed] [Google Scholar]
- 36.Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32:1515–22. doi: 10.1007/s00134-006-0301-8. [DOI] [PubMed] [Google Scholar]
- 37.de Wit M, Pedram S, Best AM, Epstein SK. Observational study of patient-ventilator asynchrony and relationship to sedation level. J Crit Care. 2009;24:74–80. doi: 10.1016/j.jcrc.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mellott KG, Grap MJ, Munro CL, Sessler CN, Wetzel PA, Nilsestuen JO, et al. Patient ventilator asynchrony in critically ill adults: Frequency and types. Heart Lung. 2014;43:231–43. doi: 10.1016/j.hrtlng.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fabry B, Guttmann J, Eberhard L, Bauer T, Haberthür C, Wolff G. An analysis of desynchronization between the spontaneously breathing patient and ventilator during inspiratory pressure support. Chest. 1995;107:1387–94. doi: 10.1378/chest.107.5.1387. [DOI] [PubMed] [Google Scholar]
- 40.Pohlman MC, McCallister KE, Schweickert WD, Pohlman AS, Nigos CP, Krishnan JA, et al. Excessive tidal volume from breath stacking during lung-protective ventilation for acute lung injury. Crit Care Med. 2008;36:3019–23. doi: 10.1097/CCM.0b013e31818b308b. [DOI] [PubMed] [Google Scholar]
- 41.Mellott KG, Grap MJ, Munro CL, Sessler CN, Wetzel PA. Patient-ventilator dyssynchrony: Clinical significance and implications for practice. Crit Care Nurse. 2009;29:41–55. doi: 10.4037/ccn2009612. quiz 1 P following 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beitler JR, Sands SA, Loring SH, Owens RL, Malhotra A, Spragg RG, et al. Quantifying unintended exposure to high tidal volumes from breath stacking dyssynchrony in ARDS: The BREATHE criteria. Intensive Care Med. 2016;42:1427–36. doi: 10.1007/s00134-016-4423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoshida T, Fujino Y, Amato MB, Kavanagh BP. Fifty years of research in ARDS. Spontaneous breathing during mechanical ventilation. Risks, mechanisms, and management. Am J Respir Crit Care Med. 2017;195:985–92. doi: 10.1164/rccm.201604-0748CP. [DOI] [PubMed] [Google Scholar]
- 44.Yoshida T, Nakahashi S, Nakamura MA, Koyama Y, Roldan R, Torsani V, et al. Volume-controlled ventilation does not prevent injurious inflation during spontaneous effort. Am J Respir Crit Care Med. 2017;196:590–601. doi: 10.1164/rccm.201610-1972OC. [DOI] [PubMed] [Google Scholar]
- 45.Yoshida T, Amato MB, Kavanagh BP. Understanding spontaneous vs. ventilator breaths: Impact and monitoring. Intensive Care Med. 2018;44:2235–8. doi: 10.1007/s00134-018-5145-5. [DOI] [PubMed] [Google Scholar]
- 46.Yoshida T, Uchiyama A, Matsuura N, Mashimo T, Fujino Y. Spontaneous breathing during lung-protective ventilation in an experimental acute lung injury model: High transpulmonary pressure associated with strong spontaneous breathing effort may worsen lung injury. Crit Care Med. 2012;40:1578–85. doi: 10.1097/CCM.0b013e3182451c40. [DOI] [PubMed] [Google Scholar]
- 47.Yoshida T, Torsani V, Gomes S, de Santis RR, Beraldo MA, Costa EL, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188:1420–7. doi: 10.1164/rccm.201303-0539OC. [DOI] [PubMed] [Google Scholar]
- 48.Yoshida T, Roldan R, Beraldo MA, Torsani V, Gomes S, de Santis RR, et al. Spontaneous effort during mechanical ventilation: Maximal injury with less positive end-expiratory pressure. Crit Care Med. 2016;44:e678–88. doi: 10.1097/CCM.0000000000001649. [DOI] [PubMed] [Google Scholar]
- 49.Yoshida T, Nakamura MA, Morais CC, Amato MB, Kavanagh BP. Reverse triggering causes an injurious inflation pattern during mechanical ventilation. Am J Respir Crit Care Med. 2018;198:1096–9. doi: 10.1164/rccm.201804-0649LE. [DOI] [PubMed] [Google Scholar]
- 50.Kallet RH, Alonso JA, Luce JM, Matthay MA. Exacerbation of acute pulmonary edema during assisted mechanical ventilation using a low-tidal volume, lung-protective ventilator strategy. Chest. 1999;116:1826–32. doi: 10.1378/chest.116.6.1826. [DOI] [PubMed] [Google Scholar]
- 51.de Wit M, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK. Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med. 2009;37:2740–5. doi: 10.1097/ccm.0b013e3181a98a05. [DOI] [PubMed] [Google Scholar]
- 52.Gogineni VK, Brimeyer R, Modrykamien A. Patterns of patient-ventilator asynchrony as predictors of prolonged mechanical ventilation. Anaesth Intensive Care. 2012;40:964–70. doi: 10.1177/0310057X1204000607. [DOI] [PubMed] [Google Scholar]
- 53.Chanques G, Kress JP, Pohlman A, Patel S, Poston J, Jaber S, et al. Impact of ventilator adjustment and sedation-analgesia practices on severe asynchrony in patients ventilated in assist-control mode. Crit Care Med. 2013;41:2177–87. doi: 10.1097/CCM.0b013e31828c2d7a. [DOI] [PubMed] [Google Scholar]
- 54.MacIntyre NR, McConnell R, Cheng KC, Sane A. Patient-ventilator flow dyssynchrony: Flow-limited versus pressure-limited breaths. Crit Care Med. 1997;25:1671–7. doi: 10.1097/00003246-199710000-00016. [DOI] [PubMed] [Google Scholar]
- 55.MacIntyre NR. Patient-ventilator interactions: Optimizing conventional ventilation modes. Respir Care. 2011;56:73–84. doi: 10.4187/respcare.00953. [DOI] [PubMed] [Google Scholar]
- 56.Thille AW, Cabello B, Galia F, Lyazidi A, Brochard L. Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med. 2008;34:1477–86. doi: 10.1007/s00134-008-1121-9. [DOI] [PubMed] [Google Scholar]
- 57.Figueroa-Casas JB, Montoya R. Effect of Tidal Volume Size and Its Delivery Mode on Patient-Ventilator Dyssynchrony. Ann Am Thorac Soc. 2016;13:2207–14. doi: 10.1513/AnnalsATS.201605-362OC. [DOI] [PubMed] [Google Scholar]
- 58.Gautam PL, Kaur G, Katyal S, Gupta R, Sandhu P, Gautam N. Comparison of patient-ventilator asynchrony during pressure support ventilation and proportional assist ventilation modes in surgical intensive care unit: A randomized crossover study. Indian J Crit Care Med. 2016;20:689–94. doi: 10.4103/0972-5229.195701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vasconcelos RS, Sales RP, de Melo LH, Marinho LS, Pd Bastos V, da Nc Nogueira A, et al. Influences of duration of inspiratory effort, respiratory mechanics, and ventilator type on asynchrony with pressure support and proportional assist ventilation. Respir Care. 2017;62:550–7. doi: 10.4187/respcare.05025. [DOI] [PubMed] [Google Scholar]
- 60.Kress JP, Pohlman AS, O'Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–7. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 61.Sottile PD, Kiser TH, Burnham EL, Ho PM, Allen RR, Vandivier RW, et al. An observational study of the efficacy of cisatracurium compared with vecuronium in patients with or at risk for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2018;197:897–904. doi: 10.1164/rccm.201706-1132OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Moss M, Ulysse CA, Angus DC. National Heart, Lung, and Blood Institute PETAL Clinical Trials Network. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 2019;380:1997–2008. doi: 10.1056/NEJMoa1901686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Unroe M, MacIntyre N. Evolving approaches to assessing and monitoring patient-ventilator interactions. Curr Opin Crit Care. 2010;16:261–8. doi: 10.1097/MCC.0b013e328338661e. [DOI] [PubMed] [Google Scholar]
- 64.Mellenthin MM, Seong SA, Roy GS, Bartolák-Suki E, Hamlington KL, Bates JH, et al. Using injury cost functions from a predictive single compartment model to assess the severity of mechanical ventilator induced lung injuries. J Appl Physiol. 2019;127:58–70. doi: 10.1152/japplphysiol.00770.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hamlington KL, Smith BJ, Allen GB, Bates JH. Predicting ventilator-induced lung injury using a lung injury cost function. J Appl Physiol (1985) 2016;121:106–14. doi: 10.1152/japplphysiol.00096.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hamlington KL, Smith BJ, Dunn CM, Charlebois CM, Roy GS, Bates JH. Linking lung function to structural damage of alveolar epithelium in ventilator-induced lung injury. Respir Physiol Neurobiol. 2018;255:22–9. doi: 10.1016/j.resp.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith BJ, Grant KA, Bates JH. Linking the development of ventilator-induced injury to mechanical function in the lung. Ann Biomed Eng. 2013;41:527–36. doi: 10.1007/s10439-012-0693-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–16. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]


