Abstract
We report a case of bronchial Dieulafoy's disease in the pediatric age. Angio-computed tomography scan and arteriography addressed us to diagnosis. Bronchial endoscopy with biopsy was avoided due to the high risk of developing a life-threatening hemorrhage. Transcatheter embolization of the bleeding bronchial artery was achieved with a MicroPlex® 10 HyperSoft 3D 3.5 mm × 80 mm System (MicroVention, Tustin, CA, USA). Dieulafoy's disease is an extremely rare lesion in the pediatric age, and the small diameter of the bleeding vessels may complicate the percutaneous approach with procedural failure. Currently, the novel thin and soft detachable coils allowed to widen the transcatheter embolization in the pediatric age.
Keywords: Child, Dieulafoy's disease, hemoptysis, percutaneous embolization
In 1898, Dieulafoy defined “exulceration simplex” as a superficial gastric ulcer due to submucosa vascular arterial malformations (then, known as Dieulafoy's disease).[1] The pathognomonic histopathological lesion of Dieulafoy's disease is the presence of large and dysplastic arteries in the submucosa.[2] Dieulafoy's disease usually engages the gastrointestinal submucosa with consequent bleeding. However, this typical histopathological lesion may rarely interest the bronchus with massive hemoptysis. This “bronchial” Dieulafoy's disease is usually an adult disease exacerbated by smoking and hypertension.[3,4] We report a very rare case of bronchial Dieulafoy's disease in a child with recurrent and severe hemoptysis treated with a transcatheter embolization of the bleeding bronchial artery.
Case Report
An 11-year-old male child came to an emergency due to the presence of chest discomfort and massive hemoptysis. A blood transfusion was necessary to achieve the hemodynamic stabilization of the patient. The hemoptysis stopped spontaneously. Oral administration of tranexamic acid was initiated. The anamnestic findings revealed a past massive event of hemoptysis (8 years before), for which the patient underwent percutaneous embolization of a bronchial artery with an Amplatzer Vascular Plug IV 4 mm (Abbott, Plymouth, MN, USA) and a Flipper® PDA Closure detachable coil 3-3 mm (Cook Inc., Bloomington, IN, USA). No comorbidity affected the patient. No significant findings were detected by clinical examination, electrocardiogram, and echocardiography. The angio-computed tomography (CT) scan showed a dilated and tortuous right bronchial artery with diffuse “ground-glass” opacity at the lower lobe of the right lung, suggesting a possible source of bleeding [Figure 1]. The cardiac catheterization was performed immediately. The aortography with selective bronchial arteriography highlighted a common vascular origin of both the right and the left lower bronchial arteries. The right lower bronchial artery was dilated and tortuous with a distal spreading of contrast medium, which suggested an endobronchial bleeding. A thin 0.014” coronary guidewire and a microcatheter were used to cross the small bronchial artery. The effective embolization of both bronchial arteries (right and left) was achieved realizing a MicroPlex® 10 HyperSoft 3D 3.5 mm × 80 mm System (MicroVention, Tustin, CA, USA). The final selective angiography showed complete closure of both the right and the left bronchial arteries, without any other signs of endobronchial bleeding [Figure 2]. Two days later, the patient was discharged. At 1-year follow-up, the patient is asymptomatic and no other hemoptysis arose.
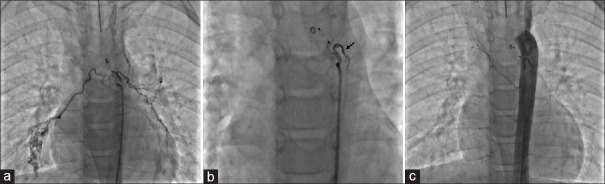
Figure 1.
Angio-computed tomography scan showing a “ground-glass” opacity at the lower lobe of the right lung both in transversal (a) and in frontal (b) view. This finding is suggestive of endobronchial bleeding
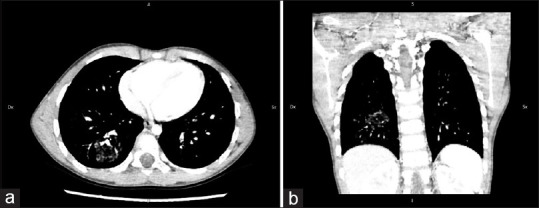
Figure 2.
Cardiac catheterization. The selective arteriography (a) highlights a common vascular trunk from which both the left and the right bronchial arteries arise. The right bronchial artery is tortuous and dilated with the significant spreading of contrast medium distally. The coil (arrow) is deployed in the distal part of the common vascular trunk achieving a complete embolization of both bronchial arteries (b). The final aortography (c) shows the success of the procedure without the opacification of the embolized bronchial arteries
Discussion
Bronchial Dieulafoy's disease is a rare cause of hemoptysis characterized by the presence of large and dysplastic arteries in the bronchial submucosa. The spontaneous rupture of these dysplastic vessels produces an endobronchial bleeding with consequent massive hemoptysis. The mean age of diagnosis is 47 years, and the right lower lobe is the most affected.[3,4,5] Chronic inflammation of the airways, respiratory tract injury, and long-term smoking are considered triggers for the bleeding events. The diagnostic “gold standard” is the histopathological examination, which may demonstrate the arterial malformation in the bronchial submucosa. However, this examination requires a bronchial/lung sample that should be obtained by an autopsy, a pneumonectomy, or an endobronchial biopsy. The latter is burdened by a high risk of fatal hemorrhages, so the clinicians are discouraged to perform it.[5] The angio-CT scan and the angiography are useful imaging tools for diagnosis with typical signs of disease: tortuous and dilated bronchial arteries with endobronchial bleeding.[3,4]
In the literature, only three cases describe Dieulafoy's disease in the pediatric age.[6,7,8] In our case, the symptoms (recurrent and massive hemoptysis) and the angio-CT scan gave enough findings to suspect this rare disease. Bronchoscopy was not performed as judged useless both to confirm the diagnosis and to plan the therapeutic strategy. Moreover, the suspected Dieulafoy's disease addressed us toward the decision to avoid biopsies of endobronchial lesions or nodules. Both the angio-CT scan and the arteriography suggested us the diagnosis of Dieulafoy's disease. The transcatheter approach was a feasible and effective strategy to close the bleeding vessel avoiding surgery. In our experience, this is the first case of successful percutaneous treatment of Dieulafoy's disease in the pediatric age. In fact, the previous reports[6,7,8] recorded failure of percutaneous attempt with consequent surgical approach to stop the bleeding. Conversely, in our case, the use of novel thin and soft detachable coils (MicroPlex® 10 HyperSoft 3D; MicroVention, Tustin, CA, USA) allowed an effective treatment of the young patient. The development of these novel soft coils permitted to widen the percutaneous approach also to the pediatric population, in which the small diameter of the bleeding vessels may complicate the procedure with a higher risk of failure.
Conclusion
Bronchial Dieulafoy's lesion is a rare disease that often begins with massive hemoptysis in adult age. However, the onset of the disease in the pediatric age must not be neglected. “Sine causa” massive and recurrent hemoptysis should address the clinicians to suspect a Dieulafoy's disease. The suspicion is crucial to allow an early management. The endobronchial biopsy should be avoided due to the risk of fatal hemorrhage. Currently, transcatheter embolization of the bleeding vessels is the “ first-line” therapy, since the novel thin and soft embolization coils allow a high success rate also in children.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient's parents have given consent for images and other clinical information to be reported in the journal. The patient's parents understand that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We gratefully acknowledge Agnese Fontana, LD for her invaluable help in reviewing and improving the chapter.
References
- 1.Dieulafoy G. Exulceratio simplex. L'intervention chirurgicale dans les hématémèses foudroyantes consécutives à l'exulcération simple del'estomac. Bull Acad Méd. 1898;39:49–84. [Google Scholar]
- 2.Parrot A, Antoine M, Khalil A, Théodore J, Mangiapan G, Bazelly B, et al. Approach to diagnosis and pathological examination in bronchial Dieulafoy disease: A case series. Respir Res. 2008;9:58. doi: 10.1186/1465-9921-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qian X, Du Q, Wei N, Wang M, Wang H, Tang Y. Bronchial Dieulafoy's disease: A retrospective analysis of 73 cases. BMC Pulm Med. 2019;19:104. doi: 10.1186/s12890-019-0863-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen W, Chen P, Li X, Gao X, Li J. Clinical characteristics and treatments for bronchial Dieulafoy's disease. Respir Med Case Rep. 2019;26:229–35. doi: 10.1016/j.rmcr.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Werf TS, Timmer A, Zijlstra JG. Fatal haemorrhage from Dieulafoy's disease of the bronchus. Thorax. 1999;54:184–5. doi: 10.1136/thx.54.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niu HL, Yi P, Wang H, Wang FH, Liu W, Gao Q, et al. Infantile Dieulafoy's disease of bronchus: Report of a case. Chin J Pathol. 2017;46:731–2. doi: 10.3760/cma.j.issn.0529-5807.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 7.Ganganah O, Guo S, Chiniah M, Sah SK, Wu J. Endobronchial ultrasound and bronchial artery embolization for Dieulafoy's disease of the bronchus in a teenager: A case report. Respir Med Case Rep. 2015;16:20–3. doi: 10.1016/j.rmcr.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang Y, Wu QC, Wang B. Dieulafoy's disease of the bronchus: Report of a case and review of the literature. J Cardiothorac Surg. 2014;9:191. doi: 10.1186/s13019-014-0191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]