Abstract
Background:
Pulp capping should always be considered as the primary treatment of choice for teeth without irreversible pulpitis in lesions approaching dental pulp. The predictability of vital pulp therapy has improved with the introduction of newer bioceramic materials.
Aim:
The purpose of this randomized controlled trial was to compare the outcomes of mineral trioxide aggregate (MTA) (Angelus, Londrina, Brazil) and a pozzolan-based cement (ENDOCEM-Zr® [Maruchi, Wonju, Korea]) as an indirect pulp capping (IPC) material.
Materials and Methods:
IPC was performed in forty patients who were randomly divided into ENDOCEM-Zr® and MTA groups. The outcome was assessed using clinical and radiographic tests at different time intervals. The prognostic factors on the outcome of IPC were also evaluated.
Results and Conclusions:
The success rate of ENDOCEM-Zr® and MTA groups was 94.7% and 89.4%, respectively. The results were not statistically significant. Binary logical regression showed that the age of the patient and the status of the pulp before treatment were deciding variables for the outcome of the study. Therefore, it was concluded from the study that the evaluated pozzolan-based cement could be used as an alternative to MTA because of its faster setting time and lower discoloration potential. In addition, pulp capping should be performed with caution in individuals above 40 years and in teeth with reversible pulpitis.
Keywords: Calcium silicate cements, ENDOCEM-Zr, indirect pulp capping, mineral trioxide aggregate, pozzolan cement, randomized controlled trial
INTRODUCTION
Retention and maintenance of the pulp is an important aspect in the management of deep carious lesions.[1] Healthy pulp has a crucial role throughout the life of a tooth due to the various responses elicited by the pulp to different stimuli of biological and pathological origin leading to the production of peritubular, secondary, and reparative dentin.[2] Vital pulp therapy should always be the treatment of choice in teeth with healthy or reversibly inflamed dental pulp. The long-term survival rate of any tooth deteriorates after undergoing any nonsurgical or surgical endodontic treatment. Vital pulp therapy reduces or postpones such therapies, thus increasing the tooth's life.[3,4]
Various materials have been used for pulp capping over the ages. Among these, mineral trioxide aggregate (MTA) has proven to be a dependable pulp capping material.[5] However, the disadvantages of MTA include its long setting time, low washout resistance, and tooth discoloration potential.[6] To counter these drawbacks, ENDOCEM-Zr®(Maruchi, Wonju, Korea), a pozzolan cement derived from MTA was developed. The major components of MTA and ENDOCEM are very similar, as both contain oxides of calcium, silicon, and aluminum. However, the radiopacifier in MTA, i.e., bismuth oxide, has been substituted with zirconium oxide in ENDOCEM-Zr.® 7
ENDOCEM was introduced as retrograde filling and repair material, but few studies were done to assess the mineralization and biocompatibility of the cement which gave an insight into whether it can be used for pulp capping. As a direct pulp capping agent, ENDOCEM has shown no significant difference as compared to MTA.[8] As an indirect pulp capping (IPC) material, ENDOCEM has not been evaluated. This study aims to evaluate the long-term outcome of ENDOCEM-Zr® as an IPC material. The secondary objective of the study was also to determine the prognostics factors that can affect the outcome of the IPC procedure.
MATERIALS AND METHODS
The study was approved by the Institutional Ethics Committee (IEC ref. no. 16099) and CTRI with a reference ID 0220083. This prospective, randomized controlled study was conducted as per the CONSORT guidelines. The participants were recruited from a pool of patients who were referred to the department for deep caries management.
Selection criteria
The sample size was calculated based on the article by Leye Benoist et al.[9] Based on an estimated standard deviation of 0.1 units and with a significance level of 0.01 (alpha) and power of 92%, using a two-sided paired t-test, a sample size of 18 was achieved. Considering a drop out of 20%, 22 patients per group was finalized.
Informed consent was obtained from the participants above the age of 18 before enrolling them in the study. The posterior teeth with mature root and healthy periodontium having occlusal or proximal deep carious lesion were included in the study. The radiological depth of the carious lesion was at least two-thirds of the total dentin thickness. Teeth with pulp exposure, spontaneous unprovoked pain, sinus opening, periodontium inflammation, mobility, cracked tooth, furcal radiolucency, internal or external resorption, and periapical lesion were excluded from the study.
Clinical examination
The status of the pulp was tested by performing thermal and electric pulp tests. Teeth with response suggestive of normal pulp or reversible pulpitis were included in the study.
Radiographic examination
Intra-oral periapical radiographs were taken in the paralleling technique for all the patients after the clinical examination. Teeth in which the lesion involved two-thirds or more of the dentin were included in the study. Periodontal health of the teeth was assessed using the Periapical Index system (PAI) by Orstavik et al.[10] Teeth having a score of 1 were included in the study.
Caries excavation and pulp capping
Once the tooth was anesthetized and a rubber dam applied, caries removal was performed. Caries removal at high speed using a round diamond bur (BR-31 Mani Diamond Bur, Tochigi, Japan) was restricted to the peripheral walls to avoid pulp exposure. Thus, a layer of caries-affected dentin was left on the cavity floor adjacent to the pulpal/axial wall. A caries detecting dye (Caries Detector, Kuraray, Japan) was used to check the presence of remaining infected dentin that was manually removed with the help of spoon excavators (#EXC817 GDC, Hoshiarpur, India).
Restorative procedure
The investigator's colleague performed coin toss just before the treatment process. Hence, the dentist was not aware of the material used until the restoration process, thus eliminating the allocation bias. ENDOCEM-Zr was allotted to “Heads” and MTA was allotted to “Tails.” The allocation was done until there were 22 teeth in both groups.
MTA (MTA Angelus™, Londrina, Brazil) and ENDOCEM-Zr®(Maruchi, Wonju, Korea) were mixed according to the manufacturer's instructions until a homogenous wet sand consistency mix was obtained. For MTA, the mixed cement was placed on the selected site with the help of a plastic filling instrument and a moist cotton pellet was placed on the cement and left for 15 min as per the manufacturer's instruction. For ENDOCEM-Zr®, the mix was applied on the selected site. Using an absorbent pellet, the mixture was condensed. Once the cement hardened in about 4 min, the cavity was given an interim restoration of RMGIC (GC Fuji II LC, Tokyo, Japan). During the recall visit, the RMGIC was reduced to a base and composite resin restoration (Filtek Z350 XT, 3M ESPE, St. Paul, USA) was placed using the incremental technique.
Recall and data entry
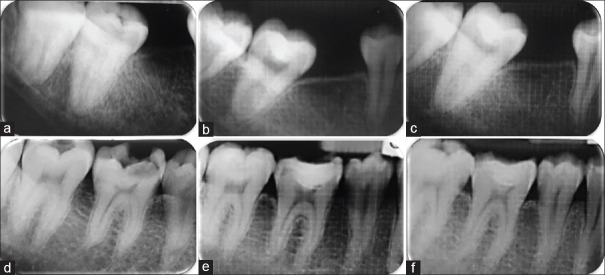
The patients were recalled after 1 week, 3 months, 6 months, and 12 months. The clinical and the radiographic tests were repeated at every visit, and readings were entered in the data entry sheet. The clinical and radiographic outcomes were assessed for all the patients by a single experienced endodontist, who was blinded. The teeth were checked for tenderness on percussion and palpation and were entered as 0 if absent and 1 if present. Pulp sensibility test was done for each tooth. Teeth giving an exaggerated and lingering response, or no response were considered as failures. The radiographical success of the procedure was evaluated based on the absence of; furcal radiolucency and/or root resorption and/or PAI score of >2 [Figure 1].
Figure 1.
Radiographs at baseline, 3 months, and 12 months recall visit for mineral trioxide aggregate group (a-c) and for ENDOCEM-Zr group (d-f)
Statistical analysis
All the patients' data were collected, tabulated, and subjected to statistical analysis using the SPSS v20.0 software (IBM Corp, Somers, NY, USA). Per-protocol analysis was followed in this study. The results of ENDOCEM-Zr® and MTA for the pulp capping procedure were compared using Pearson's Chi-square test with a significance value kept at 0.05. The relationship of the independent variables in deciding the outcome of the IPC procedure was analyzed using binary logistic regression.
RESULTS
Forty-four patients were initially included in the study. Out of the 44 patients, four patients were later excluded because three of them were not meeting the inclusion criteria (pulp exposure and isolation difficulty) and one of them declined to participate in the study. The baseline characteristics of the participants randomly allocated into MTA and ENDOCEM-Zr groups did not show statistically significant difference [Table 1]. One patient each was lost at follow-up in the MTA and ENDOCEM-Zr® group during the 3rd month and 6th month recall, respectively. A total of 38 patients were analyzed at the end of 1 year. The follow-up rate was 95%. At the 3-month follow-up period, one tooth failed due to irreversible pulpitis in the MTA group. At the 6-month follow-up, one tooth each from both the groups failed due to symptomatic irreversible pulpitis. However, there were no failures in both the groups at 1-year follow-up. The overall success rate of IPC according to this study was 92.1% at the end of 12 months. The overall success rate in ENDOCEM and MTA groups at the end of 12 months was 94.7% and 89.5%, respectively. There was no statistically significant difference between both the groups (P = 0.547) as shown in Table 2. The recruitment of the participants and the sequence of events from initiation to 12 months are depicted in Figure 2.
Table 1.
Baseline characteristics of the participants included in the study
| Variable | Subgroup | ENDOCEM Zr®, n (%) | MTA, n (%) | χ2 | P |
|---|---|---|---|---|---|
| Age (years) | <40 | 17 (85) | 16 (80) | 0.173 | 0.677 |
| >40 | 3 (15) | 4 (20) | |||
| Sex | Male | 11 (55) | 8 (40) | 0.902 | 0.342 |
| Female | 9 (45) | 12 (60) | |||
| Tooth | Premolar | 8 (40) | 9 (45) | 0.102 | 0.749 |
| Molar | 12 (60) | 11 (55) | |||
| Site of lesion | Occlusal | 6 (30) | 6 (30) | 0.000 | 0.000 |
| Proximal | 14 (70) | 14 (70) | |||
| Pulp status | Normal | 9 (45) | 8 (40) | 0.102 | 0.749 |
| Reversible | 11 (55) | 12 (60) |
MTA: Mineral trioxide aggregate
Table 2.
Univariate analysis between outcome at 12 months to dependent variables
| Variables | Subgroups | Frequency | Success, n (%) | Failure, n (%) | χ2 | P |
|---|---|---|---|---|---|---|
| Type of material | ENDOCEM Zr® | 19 | 18 (94.7) | 1 (5.3) | 0.362 | 0.547 |
| MTA | 19 | 17 (89.5) | 2 (10.5) | |||
| Gender | Male | 18 | 16 (88.9) | 2 (11.1) | 0.487 | 0.485 |
| Female | 20 | 19 (95) | 1 (5) | |||
| Age (years) | <40 | 33 | 33 (100) | 0 | 21.497 | <0.001 |
| >40 | 5 | 2 (40) | 3 (60) | |||
| Tooth | Premolar | 16 | 14 (87.5) | 2 (12.5) | 0.806 | 0.369 |
| Molar | 22 | 21 (95.4) | 1 (4.6) | |||
| Site of lesion | Occlusal | 10 | 10 (100) | 0 | 1.163 | 0.280 |
| Proximal | 28 | 25 (89.3) | 3 (10.7) | |||
| Pulpal status | Normal | 20 | 20 (100) | 0 | 3.083 | 0.079 |
| Reversible pulpitis | 18 | 15 (83.3) | 3 (16.7) |
MTA: Mineral trioxide aggregate
Figure 2.
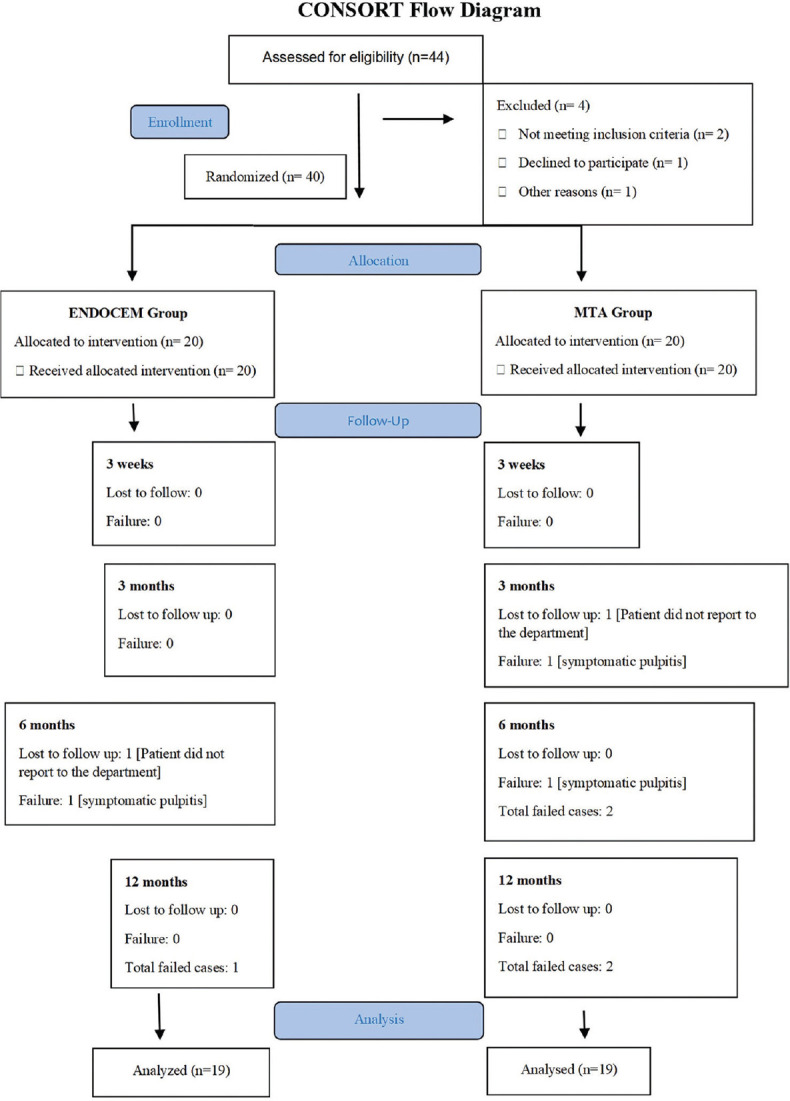
The CONSORT diagram of reporting of participant flow
The three cases that failed were seen in patients above the age of 40, with proximal caries, and teeth exhibiting symptoms of reversible pulpitis during the baseline investigation [Table 2]. The outcome of the pulp capping procedure was predicted using logistic regression analysis. Nagelkerke R2 of 0.754 indicated a moderately strong relationship between the predictors. The analysis showed that the age of the patient (P = 0.002) and pulpal status (P = 0.002) were the parameters that affected the outcome of the pulp capping procedure significantly [Table 3].
Table 3.
Binary logistic regression analysis depicting relationship between final outcome to independent variables
| Variables | B | Standard error | P | 95% confidence interval | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| ENDOCEM Zr®
(Mineral trioxide aggregate)# |
0.536 | 8.386 | 0.611 | −16.578 | 28.260 |
| Male (Female)# |
0.393 | 8.160 | 0.690 | −14.551 | 21.174 |
| <40 years (>40 years)# |
−38.698 | 5.390 | 0.002* | −46.702 | −21.280 |
| Premolar (Molar)# |
1.156 | 11.526 | 0.427 | −12.146 | 34.507 |
| Occlusal surface (Proximal surface)# |
0.233 | 9.97 | 0.868 | −14.642 | 33.602 |
| Normal pulp (Reversible pulpitis)# |
−36.341 | 14.584 | 0.002* | −37.331 | −1.224 |
| Constant | 16.850 | 18.917 | 0.200 | −43.459 | 23.131 |
#Reference category mention in parentheses; *Statistically significant.
DISCUSSION
The overall success rate of IPC in the present study was 94% at the end of 12 months. This result is consistent with the studies conducted in the recent past, which have shown high success for IPC as a treatment option for deep carious lesions, ranging from 92% to 97%.[11,12] There was no significant difference in the outcome between the MTA and ENDOCEM-Zr® groups, suggesting that both the materials are equally effective as an IPC agent. This result is comparable with the study by Jang et al., which demonstrated similar cumulative successes of MTA and ENDOCEM as pulp capping materials up to 1 year.[8] Another study by Park et al. that evaluated the formation of dentin bridge histologically in rat teeth detected no statistically significant difference between ENDOCEM and MTA.[13]
In the current study, it was seen that lesser time was required for the setting of ENDOCEM-Zr® as compared to MTA. Li et al. in 2013 stated that the addition of nano-sized particles of zirconium oxide fastens the setting reaction of Portland cement, thereby reducing the setting time.[14] This decrease in the setting time of ENDOCEM-Zr® leads to an increased strength of the material during the early phase and increased resistance toward washout.[15] Another disadvantage of MTA is the discoloration potential of the material, which can be overcome with the use of ENDOCEM-Zr®.[16] This was substantiated in the study by Kang SH et al., where they proved lower discoloration with ENDOCEM-Zr® than MTA.[17]
The logistic regression in this study identified the age and status of the pulp as the predictive factor in the outcome of the pulp therapy. All the failures were present in patients above the age of 40. This result was consistent with the study conducted by Cho et al., in which all the failures were seen in patients 40 years and older.[18] The probable reason for this could be the reduction in pulp vascularity and cumulated pulpal stresses with age.[19] The other factor which decided the outcome in this study was the dental pulp status at the baseline investigation. All the teeth that failed in this study had reversible pulpitis before initiating the pulp capping procedure. This result is in accordance with a review by Rodd et al., where they have concluded that the status of the pulp determines the outcome of the pulp capping procedure.[20]
Although in the present study, the site of the lesion showed no significant effect on the treatment outcome of IPC, all the failures occurred in teeth where the pulp capping was performed in the proximal aspect. As per the study conducted by Cho et al., it was concluded that the teeth with carious lesions at the axial side had less survival rate compared to lesions on the occlusal side.[18] This may be attributed to the increased marginal leakage of proximal cavities compared to occlusal cavities due to inadequate visual access, which makes isolation, placement of capping material, and complete removal of caries more difficult, leading to marginal leakage.[18] However, further studies must be done with a larger sample size and for a longer duration to substantiate the results of the present study.
CONCLUSIONS
This study has shown that ENDOCEM-Zr® is equally effective in IPC when compared to MTA and has a faster setting time and no discoloration, unlike MTA. Factors such as the patient's age and status of the pulp can be considered as prognostic factors in the IPC procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hilton TJ. Keys to clinical success with pulp capping: A review of the literature. Oper Dent. 2009;34:615–25. doi: 10.2341/09-132-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stockton LW. Vital pulp capping: A worthwhile procedure. J Can Dent Assoc. 1999;65:328–31. [PubMed] [Google Scholar]
- 3.Caplan DJ, Cai J, Yin G, White BA. Root canal filled versus non-root canal filled teeth: A retrospective comparison of survival times. J Public Health Dent. 2005;65:90–6. doi: 10.1111/j.1752-7325.2005.tb02792.x. [DOI] [PubMed] [Google Scholar]
- 4.Wegner PK, Freitag S, Kern M. Survival rate of endodontically treated teeth with posts after prosthetic restoration. J Endod. 2006;32:928–31. doi: 10.1016/j.joen.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Hegde S, Sowmya B, Mathew S, Bhandi SH, Nagaraja S, Dinesh K. Clinical evaluation of mineral trioxide aggregate and biodentine as direct pulp capping agents in carious teeth. J Conserv Dent. 2017;20:91–5. doi: 10.4103/0972-0707.212243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bakland LK, Andreasen JO. Will mineral trioxide aggregate replace calcium hydroxide in treating pulpal and periodontal healing complications subsequent to dental trauma.A review? Dent Traumatol. 2012;28:25–32. doi: 10.1111/j.1600-9657.2011.01049.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee M, Kang CM, Song JS, Shin Y, Kim S, Kim SO, et al. Biological efficacy of two mineral trioxide aggregate (MTA)-based materials in a canine model of pulpotomy. Dent Mater J. 2017;36:41–7. doi: 10.4012/dmj.2016-121. [DOI] [PubMed] [Google Scholar]
- 8.Jang Y, Song M, Yoo IS, Song Y, Roh BD, Kim E. A randomized controlled study of the use of proroot mineral trioxide aggregate and endocem as direct pulp capping Materials: 3-month versus 1-year Outcomes. J Endod. 2015;41:1201–6. doi: 10.1016/j.joen.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Leye Benoist F, Gaye Ndiaye F, Kane AW, Benoist HM, Farge P. Evaluation of mineral trioxide aggregate (MTA) versus calcium hydroxide cement (Dycal(®)) in the formation of a dentine bridge: A randomised controlled trial. Int Dent J. 2012;62:33–9. doi: 10.1111/j.1875-595X.2011.00084.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orstavik D, Kerekes K, Eriksen HM. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2:20–34. doi: 10.1111/j.1600-9657.1986.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 11.Farooq NS, Coll JA, Kuwabara A, Shelton P. Success rates of formocresol pulpotomy and indirect pulp therapy in the treatment of deep dentinal caries in primary teeth. Pediatr Dent. 2000;22:278–86. [PubMed] [Google Scholar]
- 12.Petrou MA, Alhamoui FA, Welk A, Altarabulsi MB, Alkilzy M, H Splieth C. A randomized clinical trial on the use of medical Portland cement, MTA and calcium hydroxide in indirect pulp treatment. Clin Oral Investig. 2014;18:1383–9. doi: 10.1007/s00784-013-1107-z. [DOI] [PubMed] [Google Scholar]
- 13.Park SJ, Heo SM, Hong SO, Hwang YC, Lee KW, Min KS. Odontogenic effect of a fast-setting pozzolan-based pulp capping material. J Endod. 2014;40:1124–31. doi: 10.1016/j.joen.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Li Q, Deacon AD, Coleman NJ. The impact of zirconium oxide nanoparticles on the hydration chemistry and biocompatibility of white Portland cement. Dent Mater J. 2013;32:808–15. doi: 10.4012/dmj.2013-113. [DOI] [PubMed] [Google Scholar]
- 15.Choi Y, Park SJ, Lee SH, Hwang YC, Yu MK, Min KS. Biological effects and washout resistance of a newly developed fast-setting pozzolan cement. J Endod. 2013;39:467–72. doi: 10.1016/j.joen.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 16.Berger T, Baratz AZ, Gutmann JL. In vitro investigations into the etiology of mineral trioxide tooth staining. J Conserv Dent. 2014;17:526–30. doi: 10.4103/0972-0707.144584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang SH, Shin YS, Lee HS, Kim SO, Shin Y, Jung IY, et al. Color changes of teeth after treatment with various mineral trioxide aggregate-based materials: An ex vivo study. J Endod. 2015;41:737–41. doi: 10.1016/j.joen.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 18.Cho SY, Seo DG, Lee SJ, Lee J, Lee SJ, Jung IY. Prognostic factors for clinical outcomes according to time after direct pulp capping. J Endod. 2013;39:327–31. doi: 10.1016/j.joen.2012.11.034. [DOI] [PubMed] [Google Scholar]
- 19.Lipski M, Nowicka A, Kot K, Postek-Stefa-ska L, Wysocza-ska-Jankowicz I, Borkowski L, et al. Factors affecting the outcomes of direct pulp capping using Biodentine. Clin Oral Investig. 2018;22:2021–9. doi: 10.1007/s00784-017-2296-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodd HD, Waterhouse PJ, Fuks AB, Fayle SA, Moffat MA British Society of Paediatric Dentistry. Pulp therapy for primary molars. Int J Paediatr Dent. 2006;16(Suppl 1):15–23. doi: 10.1111/j.1365-263X.2006.00774.x. [DOI] [PubMed] [Google Scholar]