Highlights
-
•
Teleconsultation is a way to cure patients and limit the spread of COVID-19.
-
•
We conduct a large scale survey and data analysis across four countries.
-
•
Performance expectancy is key for the intention to use teleconsultation.
-
•
Personal traits directly impact effort expectancy.
-
•
Contamination avoidance and availability influence performance expectancy.
Keywords: Teleconsultation, Telemedicine, Acceptance, COVID-19, Pandemic
Abstract
In recent months, humanity has had to deal with a worldwide pandemic called COVID-19, which has caused the death of hundreds of thousands of people and paralyzed the global economy. Struggling to cure infected patients while continuing to care for patients with other pathologies, health authorities have faced the lack of medical staff and infrastructure. This study aimed to investigate the acceptance of teleconsultation solutions by patients, which help to avoid the spread of the disease during this pandemic period. The model was built using some constructs of the technology acceptance model UTAUT2, Personal traits, Availability, and Perceived Risks. A new scale on Contamination Avoidance was developed by the authors. The questionnaire was disseminated in several countries in Europe and Asia and a total sample of 386 respondents was collected. The results emphasize the huge impact of Performance Expectancy, the negative influence of Perceived Risk, and the positive influence of Contamination Avoidance on the adoption of teleconsultation solutions. The findings highlight the moderating effects of Age, Gender, and Country.
1. Introduction
A worldwide pandemic called the Corona Virus Disease, 2019 (COVID-19) first appeared in China and has caused the death of hundreds of thousands of people. Indeed, more than 24 million people worldwide have been infected and more than 830 000 have died.1
According to Yoo and Managi (2020), the governmental interventions applied to reduce the death cases and promote social distancing may cause a loss of 47.28% of the global annual gross domestic product (GDP). Such results were also achieved, as reported by the findings of recent studies, because “people who go out under the state of emergency are stigmatized by society as having inferior ethics because they do not follow the social norms” (Katafuchi et al., 2020, p. 3). The transmission mode of the COVID-19 is mainly due to the spread of droplets by infected individuals when coughing or sneezing. Thus, direct and close interactions over short distances less than 1.5 m and contact with potentially contaminated materials are not recommended. This virus spread rapidly worldwide due to urban development, migrations, and modern transport evolution, thus easily and quickly spreading across boundaries (Jin et al., 2020). According to the World Health Organization, everyone can be infected by COVID-19. Nevertheless, the elderly and individuals with underlying medical conditions represent the population with a higher risk of developing a severe form. The basic reproduction number (R0) indicates the spread of a virus. An R0 below 1 demonstrates a low expansion capacity of a virus, while an R0 above 1 generates immediate actions to limit its diffusion. According to Trilla (2020), the R0 of COVID-19 varies from 1.4 to 2.5. Thus, its impact on health is important and the likelihood of death is high. Governments have tried to contain this disruptive outbreak and to limit its impact. One of the first decisions to restrain COVID-19 infection was the isolation of infected individuals, limiting social interactions, and respecting some rules when going outside, such as wearing masks and washing hands as often as possible. Finally, regular disinfection of all surfaces touched by people, and, then, in some countries, a complete lockdown of citizens was decided. However, the pandemic has highlighted an important issue, that is, the lack of medical staff and infrastructure. Governments have struggled to find ways to cure patients infected by COVID-19 and postponed all non-urgent medical care, but they simultaneously attend to all the other patients with urgent pathologies (Katz et al., 2020). Indeed, the priority was to maximize the capacity in intensive care units by using all the beds available and moving those units into critical care units. The Chinese government has decided to install cabin hospitals to treat patients with a moderate form of COVID-19 to reduce the risk of developing into severe cases (Shu et al., 2020). To contain the pandemic and avoid contamination, patients must avoid, if possible, going to hospitals and, instead, visit their family doctor, and use the available technologies, such as a phone or computers (Bongiovanni et al., 2020) and telemedicine applications, to communicate. Countries could mobilize different approaches to address the lack of physicians, mainly due to the rise of the population or medical deserts. They could increase the number of medical students and/or hire international physicians or use technology. The advent of information and communication technologies (ICTs) in the healthcare area is changing the way health support is provided. According to Gutierrez et al. (2017), e-health can be segmented into six dimensions:
(1) Electronic health records relate to the digitalization of medical information collected, stored, and provided to medical staff to support them in their decision making.
(2) Health information exchange refers to the possibility to aggregate all the data of a patient. It is readily available to authorized people, whichever the country or information system used.
(3) mHealth, based on mobile devices, such as smartphones, can be used by both medical staff and individuals. Nevertheless, mHealth must address some potential issues such as the security and privacy of patient data, differences between standards regarding information treatment, and, finally, the profitability issue of such applications.
(4) Healthcare social media refers to the exchange of information through main forums and online communities sharing experiences, such as chronic or rare diseases. The main risk of using social media is the privacy issue, that is, the exposure of patients’ private information to the public.
(5) Remote care systems are devices designed to collect and communicate data. These devices can be classified as follows (Wen, 2017): i) Health monitoring applications (software) for smartphones and tablets; ii) Electronic devices and apps to capture biological signals (e.g., diabetes); iii) Cloud productivity software tools, for example, COVIDSafe (Australia), Health Code (China), StopCovid (France), COVID Community Alert (Italy), COVID Symptom Study (UK); iv) Monitoring systems such as smartwatches or wristbands.
(6) Telehealth is based on the delivery of services and information through telecommunication solutions. Telehealth empowers patients and the healthcare system and reduces the cost of care for individuals who want to maintain or improve their health. Telehealth includes three concepts: telecare, telemetry, and telemedicine. Telecare offers remote care allowing people, for example, to stay at home. Telemetry allows tracking patients’ health everywhere, including within the hospital using sensors, remoting systems, and wireless networks. Finally, telemedicine reduces the distance barriers between physicians and patients by providing remote consultation (teleconsultation). Telemedicine can improve the quality of medical care, where distance is a critical factor, such as in rural areas, developing countries, and medical deserts (Kolbe et al., 2015). This study focused on the concept of telemedicine. The study aimed to analyze patients’ acceptance of teleconsultation solutions during the COVID-19 pandemic and to cover the two topics raised by the World Economic Forum2 : (1) how does teleconsultation contribute to limiting the infection and spread of disease?; (2) how does teleconsultation contribute to the delivery of healthcare services during a pandemic period? To answer these questions, a quantitative approach was used. A survey was conducted using existing scales and one scale on Contamination Avoidance was developed by the authors. The questionnaire was distributed in several countries in Europe and Asia. A sample of 386 respondents was collected and responses were analyzed using a partial least squares approach with the SmartPLS3.0 software.
This article is organized as follows. The first part presents the theoretical background of telemedicine and teleconsultation. The second part discusses the methodology used, including a presentation of the constructs considered in our research model, the building process of a new scale, the details of data collection, and the sample. The third and fourth parts present and discuss the results. Finally, the article concludes with theoretical and managerial implications, limitations, and suggestion for future research.
2. Theoretical background
2.1. Telemedicine
Telemedicine solutions, which emerged in the 1960s, were first developed to address the needs of the military and space sectors. The development of ICTs, the individual's adoption rate of devices (computer, tablets, smartphones), the technological advancements of telemedicine tools, and, recently, the worldwide pandemic (COVID-19) were the key drivers of the expansion of healthcare services (Suresh and Nath, 2013). Telemedicine, considered disruptive innovation, proposes interactive solutions and restructures the current health system (Wen, 2017) by providing key benefits such as cost and time efficiencies. Teleconsultation removes the transportation cost and allows the patients to access the relevant physician directly and instantaneously, regardless of location. The use of telemedicine is particularly recommended for patients with pathologies such as diabetes (Banerjee et al., 2020), cancers (Scotté et al., 2020), or asthma and immunodeficiency (Portnoy et al., 2020). Other services include teleradiology consultations and services (Ohannessian et al., 2020); palliative care programs (Calton et al., 2020), and patients waiting for surgery (Sterpetti, 2020). Providing healthcare through telemedicine can reduce the risks of clinicians’ exposure to infections, thanks to better management of their well-being (Patel et al., 2018; Júnior and Pauna, 2020). Patients can connect using their mobile devices or through a Telemedicine Cabin installed in pharmacies, at shopping centers, at work (Baudier et al., 2020). The main benefit of using the Telemedicine Cabin rather than, for example, a connection from home is the availability of measuring devices within the cabin to control blood pressure, weight, temperature, visual acuity, to do an electrocardiogram, or to verify the level of oxygen in the blood. In both cases, the physician provides, after the consultation, accurate advice, including, if necessary, a prescription for drugs or additional analysis. Nevertheless, for successful implementation, telemedicine services need at least infrastructural support, adequate bandwidth availability, technical performance of the communication media, quality audio and video systems, efficient telemedicine software, and sufficient specialized and qualified medical staff, including doctors and nurses. In addition, the sustainability of teleconsultation projects mainly depends on the acceptance of such solutions by both the practitioners and the patients and on the quality of the relationship created. Indeed, some individuals could be attached to the paternalistic model of care where patients and doctors meet face-to-face in the same room and are reluctant to move to another model even if it removes the distance and reduces the level of economic and energy expenses (Bashshur et al., 2009). Several telemedicine solutions, adapted to local needs, have already been implemented worldwide, integrating a combination of technologies such as i) the portable health clinic, including sensors to collect information transmitted via a mobile network (Nohara et al., 2015), ii) the tuberculosis e-health pack using a computer, a digital microscope, and an Internet connection to support the remote diagnosis and therapy proposed to patients (Rachmat et al., 2009), and iii) the mobile diagnosis system using a smartphone with the integration of a telediagnosis system (Namahoot et al., 2015). The main goal of teleconsultation is to improve access to healthcare everywhere, thus reducing inequalities between countries, cities, and social situations and creating a new concept with its own epistemological and therapeutic qualities. Telemedicine solutions are key cases of natural disasters, wars, and pandemics, for example, during the Ebola epidemic outbreak or, more recently, COVID-19.
2.2. COVID-19 and teleconsultation
With the emergence of COVID-19, teleconsultation solutions, already used in previous epidemics such as Ebola or SARS, have boosted (Machado et al., 2020) and gained even more visibility (Greenhalgh et al., 2020; Hollander and Carr, 2020; Pollock et al., 2020). Teleconsultation can solve the main concern of reducing the level of contact among people to prevent cross-contamination and avoid the spreading of the virus. Nevertheless, the goal of teleconsultation is also to continue providing patients (infected by COVID-19 or not) with medical support. Indeed, all individuals with other health pathologies must continue having access to healthcare. Teleconsultation was mainly used to sort COVID-19 patients and identify those infected (Lee et al., 2020; Davarpanah et al., 2020), some of whom have suspect symptoms such as fever, cough, respiratory discomfort, and drowsiness (Scotté et al., 2020). Therefore, the aim is to quickly identify and isolate COVID-19 patients and organize their hospitalization in emergency situations. Health authorities in many countries have implemented telemedicine user guidelines to incentivize people to use such services during the COVID-19 pandemic. In the USA, the use of Skype, Zoom, Google Hangouts, Apple, and telehealth visits is authorized and reimbursed at the same rate as face-to-face visits since March 1, 2020 (Setzen et al., 2020). In Italy, a national strategy for promoting the adoption of teleconsultation is still missing. However, as in Lazio, some regional healthcare institutions offer specific digital services to support patients during the COVID-19 pandemic (https://www.salutelazio.it/lazio-doctor ). In France, patients can be reimbursed when using telemedicine solutions since September 2018. In March 2020, due to the COVID-19 crisis, the French government issued a decree, allowing French Health Insurance to cover any medical teleconsultation.3 In China, public health authorities encourage citizens to embrace remote medical services. The two most popular ones (WeDoctor and haodf.com) propose free-of-charge teleconsultation for patients with COVID-19 and advice regarding the quarantine (Sun et al., 2020). In the UK, telemedicine is free at the point of delivery, and many private health insurance companies include this service in their standard offer.4 Thus, many companies proposing teleconsultation services have emerged, highlighting the potential benefits of such health tools.
2.3. Adoption and acceptability of telemedicine
The adoption and acceptance of telemedicine require the application of one of the technology acceptance models that could explain the factors to predict patients’ behavior. In the personal context of use, the most appropriate and adapted model with predictive power explaining 70 percent of the variance in behavioral intention is the unified theory of acceptance and use of technology (UTAUT) model, also tested in healthcare (Holden and Karsh, 2010; Cimperman et al., 2016). Using UTAUT2 (Venkatesh et al., 2012) is accurate because it was (1) created considering existing models; (2) tested in the healthcare field; (3) and adapted for the measurement of patients’ behavior. The UTAUT2 model consists of seven variables predicting behavioral Intention to Use, Performance Expectancy, Effort Expectancy, Facilitating Conditions, Social Influence, Habit, Hedonic Motivation, and Price Value.
Except for variables of the initial UTAUT2, the model was often extended with additional variables and antecedents depending on the technology and context of use.
The most important predictors of the intention to accept a technological solution in healthcare are: 1) Personal traits, such as Self-Efficacy (Bonsaksen et al., 2013) and Personal Innovativeness (Bloch et al., 2003); 2) Telemedicine benefits such as Availability (Moores, 2012); and 3) Teleconsultation threats, such as Perceived Risks (Ortega-Egea and Roman-Gonzalez, 2011).
2.4. Contamination avoidance
Since diverse diseases appeared in modern society (AIDS, Ebola, etc.), researchers try to understand their social influence on individuals. The law of contagion is one of the most applied theories derived from anthropology and describing magical beliefs in rituals and artifacts in diverse traditional cultures. The law of contagion states that objects, in contact with others, can transfer the power or weakness of the object's owner (Morales et al., 2018). In terms of disease contamination, researchers analyze the negative impact of people's concerns about the danger of being infected through contact with objects or environments that could potentially spread germs, viruses, infections, etc. (Hazée and Van Vaerenbergh, 2020). Thus, contamination fears could negatively influence individuals’ behavior. This negative effect is directly related to the emotion of disgust. Individuals can feel this emotion toward numerous physical contacts with products or objects and in diverse places, such as supermarkets, public transport, or medical establishments (Bezançon et al., 2019; Nakamura and Managi, 2020). Individuals could avoid being in a dangerous situation and take the appropriate action to avoid contamination. Thus, contamination avoidance can be defined as the extent to which consumers tend to avoid contacts or places because of the fear of being contaminated. In the COVID-19 pandemic, obviously, some of the places or situations to raise a high level of contamination concerns are medical establishments. Nevertheless, patients have to continue to consult medical professionals, but, during the COVID-19 pandemic, they might feel that they are in danger (Moroni et al., 2020). In fact, medical staff might also consider that teleconsultation is a suitable option to reduce contacts and infection rates. Thus, the adoption of telemedicine solutions could be an answer for both patients and physicians, maintain patient care, reduce the level of infections, and remove fear.
3. Methodology
3.1. Research model
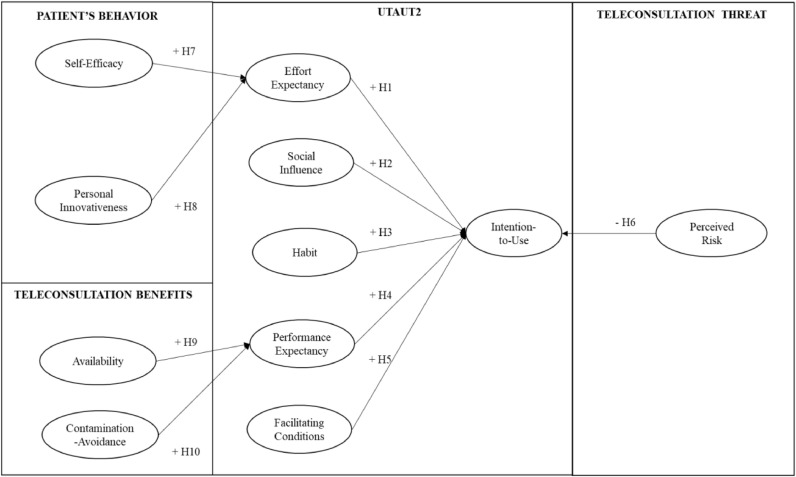
Our research model (Fig. 1 ) was developed using several existing scales obtained from the literature and adapted to analyze the following: (1) the acceptance of teleconsultation solutions during a pandemic period (COVID-19) using five constructs of the UTUAT2 (Venkatesh et al., 2012); (2) the Hedonic Motivation and Price Value variables were removed from the model as not accurate for the study, (3) the patient's behavior using Self-Efficacy (Bonsaksen et al., 2013), and Personal Innovativeness scales (Bloch et al., 2003), (4) the teleconsultation threat mobilizing the scale of Perceived Risks (Ortega-Egea and Roman-Gonzalez, 2011), and finally, (5) the teleconsultation benefits using the Availability scale proposed by Moores (2012) and a scale created to measure one of the perceived advantages of the teleconsultation called Contamination Avoidance:
| Do you think that teleconsultation solutions could prevent you from being contaminated by a virus: |
| 1. On the way to your doctor's office |
| 2. In the waiting room, in contact with other patients |
| 3. In contact with your doctor |
| 4. By touching contaminated objects (door handles, chairs, etc.) |
Fig. 1.
Research model.
Items were measured using a five-point Likert scale from “strongly disagree” to “strongly agree.”
3.2. Pre-test
The paradigm of Churchill (1979) was mobilized to check the validity and reliability of the proposed scale. Items measuring the variables were validated by 13 academic experts from business schools or universities before submission (Appendix A). Then, the survey was published on social media to a convenience sample and 87 respondents were collected from April 16 to May 6, 2020. The sample's characteristics are summarized in Table 1 .
Table 1.
Test sample characteristics.
| Gender | |
| Female | 58 |
| Male | 29 |
| Age | |
| 21–25 | 28 |
| 26–35 | 17 |
| 36–45 | 23 |
| Above 45 | 19 |
The Cronbach's alpha (0.900) and the Composite Reliability (0.930) values, all above 0.7, confirmed the reliability of the Contamination Avoidance scales. Reliability was also validated with all loadings above 0.7. The Average Variance Extracted (AVE), at 0.771, confirmed the convergent validity of the Contamination Avoidance variable, above the threshold of 0.5. The discriminant validity was verified by controlling that the indicators of each construct did not load higher with another variable (cross-loadings). Finally, the results were shared with the 13 experts who confirmed the robustness of the Contamination Avoidance scale. Thus, all items proposed to measure this variable were retained.
3.3. Sample and data collection
The survey was translated into four languages (Chinese, English, French, and Italian) by researchers and administered on social media such as LinkedIn, Facebook, and Wenjuanxing, to be as independent and neutral as possible to obtain a fair representation of each age group and anyone without restrictions to biasedness, using hashtags (#Teleconsultation, #Covid19, #Pandemic, #Healthcare) and hyperlinks between June 19 and July 30, 2020. A sample of 386 respondents was collected (Table 2 ). The English version of the survey is available in Appendix B.
Table 2.
Final sample characteristics.
| Gender | Respondents | % |
| Female | 214 | 55% |
| Male | 172 | 45% |
| Total | 386 | 100% |
| Country | ||
| China | 57 | 15% |
| France | 107 | 28% |
| Italy | 82 | 21% |
| UK | 67 | 17% |
| Others | 73 | 19% |
| Total | 386 | 100% |
| Age | ||
| 18–25 | 63 | 16% |
| 26–35 | 118 | 31% |
| 36–55 | 129 | 33% |
| >55 | 76 | 20% |
| Total | 386 | 100% |
4. Results
4.1. Outer and inner model analysis
The reliability of the outer model was first controlled by verifying that the loadings were above 0.700. Second, Cronbach's alpha and Composite Reliability values were analyzed. Except for Facilitating Condition, removed as the Cronbach's alpha (0.676) was below 0.7, all the other constructs were above the recommended thresholds (Cronbach's alpha between 0.776 and 911, and Composite Reliability between 0.865 and 938). Convergent validity was confirmed by the AVE, all above the threshold of 0.5 (minimum 0.616, maximum 814). The discriminant validity was controlled by verifying that the indicators of each variable did not load higher with another variable.
The explained variance (R2), size effect (f2), and predictive relevance (Q2) of the variables were mobilized to validate the inner model. Some parameters were analyzed to study the relationships between variables such as Path Coefficient (β > at 0.200), t-value > at 1.96, and p-value < at 0.05 (Table 3 ). The R2 (0.693) demonstrated that the research model explained a large variance of Intention to Use defined by two variables: Habit and Performance Expectancy, with a huge side effect of Performance Expectancy (0.544) and a negative impact of Perceived Risk (β= −0.067, t-value=2.339, p-value=0.019) as shown in Fig. 1. Thus, hypotheses H3, H4, and H6 were supported. The impact of Effort Expectancy and Social Influence on Intention to Use was not direct or significant. Thus, Hypotheses H1 and H2 were not supported. The model explained 37.5 percent of Effort Expectancy determined by two predictor variables, Self-Efficacy and Personal Innovativeness, with a stronger impact for Self-Efficacy as confirmed by the size effect (f2) at 0.215. Thus, the positive direct and significant impact of Self-Efficacy and Personal Innovativeness were confirmed and H7 and H8 were supported. Finally, the R2 of Performance Expectancy at 44.9 percent was explained by Availability and Contamination Avoidance, thus validating the H9 and H10. The f2 (0.521) confirmed the significant impact of Availability on Performance Expectancy. The blindfolding procedure of SmartPLS3, mobilized to test the predictability of the model (Q2) with all values above 0, confirmed the predictive relevance of Effort Expectancy (0.291), Intention to Use (0.556) and Performance Expectancy (0.330). The quality of the hypothetical model was validated by analyzing the goodness-of-fit (GOF). The results (at 0.6) confirmed the good quality of the model. The Standardized Root Mean Square Residual (at 0.067, that is, below the recommended threshold of 0.1) reinforced the quality of the research model. The collinearity statistics were controlled and the findings assured that the model was free of common method bias. All inner and outer Variance Inflation Factors were below the recommended threshold of 3.3. Finally, as indicated in Table 3, on ten hypotheses postulated, seven were supported (H3, H4, H6, H7, H8, H9, and H10), two were not supported (H1 and H2), and one was removed (H5: Impact of Facilitating Condition on Intention to Use).
Table 3.
Test of hypotheses (X=Supported, O Not Supported).
| Variable | Predictor construct | R2 | f2 | β | t-Value | p-Value | Q2 | H |
| Effort Expectancy | 0.375 | 0.291 | ||||||
| Self-Efficacy | 0.215 | 0.423 | 6.611 | 0.000 | X | |||
| Personal Innovativeness | 0.093 | 0.279 | 4.723 | 0.000 | X | |||
| Intention to Use | 0.693 | 0.556 | ||||||
| Effort Expectancy | 0.009 | 0.080 | 1.473 | 0.141 | O | |||
| Habit | 0.018 | 0.119 | 2.472 | 0.013 | X | |||
| Performance Expectancy | 0.544 | 0.634 | 12.616 | 0.000 | X | |||
| Perceived Risk | 0.012 | (−0.067) | 2.339 | 0.019 | X | |||
| Social Influence | 0.001 | (−0.022) | 0.709 | 0.478 | O | |||
| Performance Expectancy | 0.449 | 0.330 | ||||||
| Availability | 0.521 | 0.577 | 13.487 | 0.000 | X | |||
| Contamination Avoidance | 0.055 | 0.188 | 3.839 | 0.000 | X | |||
4.2. Moderating effects
The Multi-Group Analysis procedure of SmartPLS3 was mobilized to check the moderating effects of age, country, and gender on all the research model constructs by analyzing the Path Coefficients and the t and p-values, using the bootstrapping procedure.
Four relationships of the model were moderated by age within the four countries analyzed (Table 4 ).
Table 4.
Age as a moderator.
| 18–25 | 26–35 | 36–55 | More than 55 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | t-Value | p-Value | β | t-Value | p-Value | β | t-Value | p-Value | β | t-Value | p-Value | |
| CA->PE | 0.349 | 2.852 | 0.004 | 0.132 | 1.303 | 0.193 | 0.252 | 2.871 | 0.004 | 0.135 | 1.624 | 0.104 |
| HT->ITU | 0.175 | 1.271 | 0.204 | (−0.001) | 0.006 | 0.994 | 0.139 | 1.495 | 0.135 | 0.262 | 3.068 | 0.002 |
| PI->EE | 0.131 | 0.948 | 0.343 | 0.263 | 2.705 | 0.007 | 0.353 | 3.620 | 0.000 | 0.293 | 2.214 | 0.027 |
| PR->ITU | (−0.204) | 2.337 | 0.019 | (−0.044) | 0.517 | 0.604 | 0.034 | 0.710 | 0.477 | (−0.090) | 1.448 | 0.148 |
The impact of:
-
•
Contamination Avoidance (CA) on Performance Expectancy (PE) was supported for the 18–25 years old and 36–55 years old groups and rejected for the 26–35 years old and more than 55 years old groups.
-
•
Habit (HT) on Intention to Use (ITU) was validated only by the respondents who were more than 55 years old.
-
•
Personal Innovativeness (PI) on Effort Expectancy (EE) was rejected by the 18–25 years old group only.
-
•
Perceived Risk (PR) on Intention to Use was validated by the 18–25 years old group and rejected by the respondents who were more than 25 years old.
One of the goals of this study was to analyze the differences highlighted by the country regarding the acceptability of teleconsultation solutions during the COVID-19 pandemic (Table 5 ). On the five relationships identified as different, Chinese respondents rejected all of them. The UK respondents also rejected almost all relationships except for the impact of Contamination Avoidance on Performance Expectancy (β=0.373, t-value=3.664, p-value=0.000). French respondents validated the positive, direct, and significant impact of Contamination Avoidance on Performance Expectancy and of Habit on Intention to Use and the negative impact of Perceived Risk on Intention to Use. The relationships between Personal Innovativeness on Effort Expectancy and Social Influence on Intention to Use were rejected. Findings in Italy were the complete opposite of the French results. The influence of Contamination Avoidance on Performance Expectancy, Habit on Intention to Use and the negative influence of Perceived Risk on Intention to Use were rejected and the relationships between the influence of Personal Innovativeness on Effort Expectancy and Social Influence on Intention to Use were supported.
Table 5.
Country as a moderator.
| China | France | Italy | UK | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Β | t-Value | p-Value | β | t-Value | p-Value | β | t-Value | p-Value | β | t-Value | p-Value | |
| CA->PE | 0.232 | 1.616 | 0.106 | 0.147 | 2.003 | 0.045 | 0.214 | 1.570 | 0.116 | 0.373 | 3.664 | 0.000 |
| HT->ITU | 0.276 | 1.646 | 0.099 | 0.190 | 2.277 | 0.022 | (−0.016) | 0.191 | 0.848 | 0.222 | 1.635 | 0.102 |
| PI->EE | 0.073 | 0.438 | 0.661 | 0.170 | 1.587 | 0.112 | 0.233 | 2.311 | 0.020 | 0.133 | 1.181 | 0.237 |
| PR->ITU | (−0.044) | 0.380 | 0.703 | (−0.112) | 2.074 | 0.038 | (−0.134) | 1.381 | 0.167 | (−0.099) | 0.941 | 0.346 |
| SI->ITU | 0.214 | 1.547 | 0.121 | 0.018 | 0.339 | 0.734 | 0.160 | 2.032 | 0.042 | 0.062 | 0.839 | 0.401 |
Finally, the moderating effect of gender on the two relationships of the influence of Habit and Perceived Risk on Intention to Use was confirmed. Indeed, both relationships were rejected by females and validated by males (Table 6 ).
Table 6.
Gender as a moderator.
| Male | Female | |||||
|---|---|---|---|---|---|---|
| β | t-Value | p-Value | β | t-Value | p-Value | |
| HT->ITU | 0.168 | 2.514 | 0.011 | 0.050 | 0.724 | 0.468 |
| PR->ITU | (−0.143) | 3.373 | 0.000 | 0.022 | 0.550 | 0.582 |
5. Discussion
This paper studied the research model using five constructs of the UTAUT2, two patient's traits (Innovativeness, Self-Efficacy), and the two perceived benefits of teleconsultation during the pandemic (Availability and Contamination Avoidance).
The findings highlight the huge influence of Performance Expectancy on the Intention to Use teleconsultation solutions, especially during the COVID-19 period. In a healthcare context, Performance Expectancy is often a significant predictor of Intention to Use, and the results are aligned with several previous studies (Baudier et al., 2020; de Veer et al., 2015; Cimperman et al., 2016), in terms of the adoption of health information systems (Hsu et al., 2013), mHealth (Hoque and Sorwar, 2017), health-related wearable devices (Gao et al., 2015; Wang et al., 2020), or electronic health records (Tavares et al., 2018). Another positive relationship emphasizes the value of Habit in adopting medical teleconsultation. Other health-related technology researchers validated these results in previous studies (Duarte and Pinho, 2019; Ravangard et al., 2017; Dhiman et al., 2019). Videoconferences became part of people's daily life, especially during the COVID-19 pandemic and the isolation period. Therefore, Habit is one of the predictors of teleconsultation. The relationship between Effort Expectancy and Intention to Use was not validated. Even if Effort Expectancy is often important for the individual use context, this finding is consistent with other studies in the health sector. Alaiad and Zhou (2014) found that Effort Expectancy is low for home healthcare robots by users, for whom these robots are not new. A similar assumption confirmed that the Effort Expectancy is not significant for the experienced users of health-related wearable devices compared with new users or non-users of this technology (Gao et al., 2015). mHealth and eHealth require less effort to adopt if this technology is familiar to patients (Duarte and Pinho, 2019; Jewer, 2018). Finally, the adoption of the Telemedicine Cabin by the younger generation is not influenced by Effort Expectancy, as the “digital natives” are used to technology (Baudier et al., 2020). Thus, medical teleconsultation is organized as a simple videoconference and the influence of Effort Expectancy on Intention to Use is certainly considered less important. This study did not support the direct relationship between Intention to Use and Social Influence for medical teleconsultations. In most of the studies about technology adoption in healthcare, Social Influence is significant and is an important predictor for professionals (Baudier et al., 2019; Alazzam et al., 2019) or individuals (Wang et al., 2020; Gao et al., 2015; Duarte and Pinho, 2019). Nevertheless, we can assume that Social Influence has a greater influence on the acceptance of innovative solutions. De Veer et al. (2015) did not validate the effect of Social Influence on Intention to Use e-health solutions. Thus, the Internet as a technology is not new to patients. Medical users can perceive teleconsultation as a videoconference. Additionally, the findings confirmed the negative influence of Perceived Risk on the Intention to Use teleconsultation that is significant and direct, although the significance is low. Perceived Risk is often a negative predictor of technology adoption, especially in the data-sensitive fields such as e-banking, e-shopping (Alalwan et al., 2018), or healthcare (Gao et al., 2015; Kim and Song, 2017). The medical data disclosure is not possible without the total agreement of the patient. Patients should understand and trust the process of data collection and storage. Thus, it may require a level of technical knowledge and understanding of the related laws. Hence, people estimate that the potential risk of data misuse is low but it exists when they use medical teleconsultation. The research model tested antecedents of two variables of UTAUT2: 1) Personal Innovativeness and Self-Efficacy on Effort Expectancy and 2) Availability and Contamination Avoidance on Performance Expectancy.
The study confirmed the importance of Personal Innovativeness on Effort Expectancy, confirming previous findings. Users with higher Personal Innovativeness tend to use technology despite its perceived complexity and without effort (Wu et al., 2011; Fan et al., 2018). Another examined personal characteristic of users is the influence of Self-Efficacy as an antecedent of Effort Expectancy. Self-Efficacy, in a technology use context, is often limited to the Computer Self-Efficacy (Compeau and Higgins, 1995). It was deleted from the initial UTAUT because of its little direct effect on Intention to Use (Venkatesh et al., 2003). Nevertheless, it has significance as a moderator or antecedent. In the health context, the Patient Self-Efficacy includes personal characteristics such as previous experiences with technology, ease of learning how to use technology (Hofstede et al., 2014), or Patient Self-Management (Hofstede et al., 2014). Previous studies validated the impact of Self-Efficacy on Effort Expectancy in the healthcare context (Hsiao et al., 2011; Kohnke et al., 2014). By using technology, patients rely on their own capacity to adopt it; in the case of teleconsultation, the patients with higher Self-Efficacy will perceive it as less complicated. The results of this study confirmed that availability is a strong predictor of Performance Expectancy regarding teleconsultation adoption by patients, and they are consistent with other studies (Baudier et al., 2020; Moores, 2012). Finally, Contamination Avoidance was regarded as a positive factor reinforcing the adoption of teleconsulting in the COVID-19 pandemic context. This construct has been created for this study and validated in the pre-test using the Churchill paradigm. It impacted positively on Performance Expectancy. The limitation of movement, lockdowns, and strict sanitarian rules changes the business models of the service companies (Kabadayi et al., 2020), giving distant solutions an advantage. Contamination concerns about the COVID-19 pandemic resulted in changes in consumers’ behavior, including the avoidance of certain places (Hazée, and Van Vaerenbergh, 2020). Thus, patients are expected to use teleconsultation to avoid being contaminated. Additionally, in medical literature, Moroni et al. (2020) confirmed that the threat to get contaminated by COVID-19 could result in medical care avoidance that could affect patients’ health, or even life. Therefore, Contamination Avoidance has strong predictive power for teleconsultation adoption in the case of COVID-19.
5.1. Moderating effects
5.1.1. Age and gender
Contamination Avoidance had a direct influence on Performance Expectancy for the respondents in the 18–25 and 36–55 years old age groups. This finding could be explained by the fact that these age groups are both worried about their relatives. The youngest group could be concerned about infecting their parents because they are still at home and the second group because their parents are considered a population at risk. Nevertheless, the results were surprising, as COVID-19 can have lethal consequences for the older generation. Older people probably take self-protection measures more often and still prefer to have personal contact with their physicians, which is confirmed by the greater effect of Habit on Intention to Use by the oldest age group. The results confirmed the moderation influence of age and gender on the Habit of using medical teleconsultation; thus, it has a greater impact on older men. This finding is in line with previous studies (Venkatesh et al., 2012; Tavares et al., 2018). Additionally, Perceived Risk also had a stronger effect on men than on women, highlighting the different attitudes toward the use of personal data and security by technology (Lee and Rho, 2013). Notably, Perceived Risk is strong for the youngest users (18–25 years old) and has no significance for older patients (Zhu et al., 2018). We have observed that younger men often use information technology. They are more aware of their personal data threats than older people, who use technology occasionally or for some simple tasks (Zhao et al., 2018). Finally, the impact of Personal Innovativeness on Effort Expectancy has more importance for users above 25 years old than for the youngest users (18–25 years old). The finding is consistent with other research results (Jackson et al., 2013; Baudier et al., 2020).
5.1.2. Country
The sample collected helped to analyze four countries regarding potential differences in the adoption of medical teleconsultation. Teleconsultation exists to some extent in all the countries studied and it has become important in the COVID-19 crisis. Nevertheless, the factors that could predict the adoption of such services are not similar. First, only the Italian respondents confirmed the effect of Social Influence on Intention to Use and that of Personal Innovativeness on Effort Expectancy, rejected by the model. Social Influence is a key predictor for using digital technologies in Italy, such as e-commerce (Guzzo et al., 2016) or mobile phone (Basaglia et al., 2009). Phan and Daim (2011) confirmed the impact of innovativeness on the ease of use of mobile technologies in Italy. Even if this effect was smaller than other tested antecedents, the users with higher innovativeness perceived less technology complexity.
One year before COVID-19, teleconsultation was implemented and reimbursed in France. The pandemic has just brought to light the existing remote medical services. Therefore, many patients have had medical teleconsultation experiences before the sanitarian crisis, explaining why Habit has an impact on French respondents’ Intention to Use (Baudier et al., 2020). Nevertheless, only the French respondents considered Perceived Risks as influencing Intention to Use, confirming previous studies on the adoption of health-related mobile applications (Currie, 2016) and the Telemedicine Cabin (Kondrateva et al., 2020).
For the UK, the use of the national health service and local medical services means that there is a preference to consult medical doctors and staff in person. The use of teleconsultation is not available to some patients. When patients develop symptoms, they are only allowed to be checked for COVID-19. In China, they experienced COVID-19 at the earliest time. They adopted the stringent approach of lockdowns, set up temporary hospitals, and conducted personal quarantine measures through medical doctors and staff, with effective controls of COVID-19 transmission. Therefore, the majority of Chinese respondents may not accept the implementation of teleconsultation.
Finally, one of the Performance Expectancy of teleconsultation, in the UK and France, is Contamination Avoidance. This relationship cannot be discussed based on existing literature as the Contamination Avoidance scale was built for the purposes of this study. However, these findings confirmed that patients from those two countries are more concerned about this topic than the Italian and Chinese respondents. Perhaps cultural differences and how governments handle COVID-19 between these groups of countries can also explain these variations.
6. Conclusion
This study addresses the critical question of healthcare delivery during the COVID-19 pandemic and the perception of teleconsultation by individuals. The technology acceptance models are often tested in the medical context for both medical professionals (Alazzam et al., 2019) and individuals (Baudier et al., 2020; Duarte and Pinho, 2019). The results of the study are important for both theory and practice.
6.1. Theoretical implications
This paper applied the UTAUT2 model to the medical teleconsultation context. The findings provide several theoretical contributions: 1) two out of the four UTAUT2 factors analyzed directly influence Intention to Use (Performance Expectancy and Habit), and two relationships were rejected (Social Influence and Effort Expectancy); 2) the analysis confirmed the moderating effects of age, gender, and country in the healthcare context; 3) a new scale for the construct of Contamination Avoidance was developed, tested, and validated based on the concept of contamination concerns. Previous studies focused on the negative impact of the fear of contagion on consumer behavior. People could be scared of getting infected through physical contact with other people or objects. Thus, this factor plays a central role in the acceptance of remote solutions and can be applied not only in a medical context, but also for the adoption of other technologies, which help to avoid direct physical contact, such as contactless payments, online shopping, working videoconferences, and online education.
6.2. Managerial implications
Due to COVID-19, the sanitarian crisis has impacted the global healthcare system (public or private hospital, retirement home, doctor's or nurse's office, etc.). The capacities of medical establishments, especially at the high point of the COVID-19 crisis, are limited. As the second/third waves of the crisis are announced, teleconsultation should be implemented rapidly to provide benefits for both the professionals and the patients to maintain healthcare services. The first audience of this study would be the healthcare authorities and governments, who are searching for efficient solutions in case of a second sanitarian crisis of the ongoing pandemic. They should encourage the launch of such technologies, communicate all the benefits of using such services for patients, and convince physicians to adopt teleconsultation solutions. Remote medical consultations exist already, but they are underused for many reasons. Second, the providers of appropriate platforms can focus on the functionalities of technology regarding patients’ profiles (age, gender, culture) and greatly improve their positioning and communication strategy. Third, as the second group of users, physicians could use the results of this study to understand the behavior of their patients. Finally, the international community could also be a target audience of this study. Today, even within Europe (France, Italy, and the UK), differences regarding technology acceptance are highlighted. Nevertheless, the experience exchange and respect of cultural differences can help the international community to define effective technology.
6.3. Limitations and future research
Despite various contributions, this study has its limitation that can provide the pathway for future studies. First, the sample, strong enough to run Partial Least Analysis, was still relatively low because of the short period for data collection and the specific context (COVID-19). Furthermore, data selection biasedness can happen due to the limitation of sources seeking data or when the questionnaire is put at a particular place and time, such as specific social media (Delgado-Rodriguez and Llorca, 2004). Moreover, only four countries were analyzed. Thus, future research could extend the study to other regions and test the new Contamination Avoidance on other technologies such as contactless payment in other fields of research (retail, finance). A longitudinal study could also better understand the evolution of teleconsultation acceptance (for example, after the pandemic).
CRediT authorship contribution statement
Patricia Baudier: Writing - original draft, Writing - review & editing, Supervision, Visualization, Project administration, Conceptualization, Methodology. Galina Kondrateva: Writing - original draft, Writing - review & editing, Conceptualization. Chantal Ammi: Writing - original draft, Writing - review & editing, Conceptualization. Victor Chang: Writing - original draft, Writing - review & editing. Francesco Schiavone: Writing - original draft, Writing - review & editing.
acknowledgement
Prof. Chang's work was partly supported by VC Research (VCR 0000107).
Biographies
Patricia Baudier is an Associate Professor of Marketing at EM Normandie Business School (France). Her research focuses on new technologies acceptance. She spent 28 years within major American companies such as Apple and Kodak and prepared her PhD within the Institute Mines Telecom Business School (Paris-Saclay). She has authored several papers in leading journals of innovation, management and marketing. Patricia is a program co-chair of the FEMIB an international conference and a member of the Research Network on Innovation. She is, within her school, the head of a research axis on International Business Network.
Galina Kondrateva has a Ph.D. in Business Management obtained at Paris-Saclay University. Today Dr. Kondrateva is an Associate Professor at EDC Paris Business School (France), a member of OCRE (Observatoire et center de Recherche en Entrepreneuriat). Her research interests are in the marketing and the adoption of technologies, with a big part of cross-cultural comparison. The topics of her research comprise analysis of users’ behavior in the usage of mobile applications, telemedicine, blockchain, and Artificial Intelligence including comparison across cultures. Before starting her academic career, she has been working for ten years as an executive director in a marketing agency in Russia.
Chantal Ammi is a Full Professor of Marketing at Institute Mines Telecom Business School (France). Her research focuses on new technologies, consumers behavioral, usage and acceptability, information systems and innovation. She was the director of a Doctoral Program and a laboratory of research (Litem) for many years. She supervised many PhD students and managed several European and industrial contracts of research in the fields of innovation and technologies (Automation, robotics…). She has authored several papers in leading journals of innovation, management and marketing.
Victor Chang is currently a Full Professor of Data Science and Information Systems at the School of Computing, Engineering and Digital Technologies, Teesside University (UK). He was previously a Senior Associate Professor, at the International Business School Suzhou, Xi'an Jiaotong-Liverpool University (China). He is the Associate Editor of IEEE TII, IFFU and IDD journals and Editor-in-Chief of IJOCI and OJBD journals, and hold or lead guest editor roles in prestigious journals. He has published 3 books as sole authors. He is the founding conference chair for IoTBDS, COMPLEXIS, FEMIB and IIoTBDSC to build up and foster active research communities globally with positive impacts.
Francesco Schiavone is Associate Professor in management at University Parthenope, Naples, Italy. He received the Ph.D. degree in network economics and knowledge management from the Ca’ Foscari University of Venice (Italy) in 2006. He is also an Affiliated Professor in innovation management at Paris School of Business and Em Lyon (France). In April 2017 Prof. Schiavone has been habilitated as Full Professor in management by MIUR (Italian Ministry of Education and Research). Currently, his main research areas are technology management, strategic innovation, communities of practice, and healthcare management and innovation.
Footnotes
Figures retrieved on August 27 https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1?
Appendices
Appendix A: List of experts
| Institution | Country | Position | Field of research | Years of experience as a researcher | |
|---|---|---|---|---|---|
| Expert1 | University of Naples Parthenope | Italy | Associate Professor | Management | 13 |
| Expert2 | College of Business and Economics, West Virginia | USA | Associate Professor | Finance | 16 |
| Expert3 | University of Stuttgart | Germany | Full Professor | Management of Innovation | 12 |
| Expert4 | University of Nantes | France | Full Professor | Management of Innovation | 30 |
| Expert5 | Teesside University | UK | Full Professor | Data Science and IS | 20 |
| Expert6 | Catholic University of Louvain | Belgium | Associate Professor | Management of Innovation | 7 |
| Expert7 | Business School, Beijing Normal University | China | Associate Professor | Management of Innovation | 12 |
| Expert8 | Peter The Great St Petersburg Polytechnic University | Russia | Associate Professor | Management of Innovation | 26 |
| Expert9 | Pardis Ltd | Austria | PhD; MD | Management of Innovation | 32 |
| Expert10 | ISC Paris Business School | France | Associate Professor | Finance | 10 |
| Expert11 | University and IAE of Bordeaux | France | Full Professor | Marketing | 35 |
| Expert12 | EDC Business School | France | Full Professor | Marketing | 46 |
| Expert13 | EMLV Business School | France | Associate Professor | Digital Marketing | 6 |
Appendix B: Survey
| In the recent isolation situation: |
| [ITU1.You think it is a good idea to use teleconsultation] |
| [ITU2.You will always use teleconsultation in the near future to access healthcare professionals] |
| [ITU3.You plan to use teleconsultation] |
| You think that: |
| [PE1.Using a teleconsultation would be useful] |
| [PE2.Teleconsultation would allow you to access healthcare faster] |
| [PE3.Using teleconsultation would increase your productivity] |
| [PE4.Teleconsultation would increase your chances of achieving healthcare] |
| You get the impression that: |
| [EE1.Learning how to use teleconsultation is easy for you] |
| [EE2.Your interaction with teleconsultation is clear and understandable] |
| [EE3.You find teleconsultation easy to use] |
| [EE4.It is easy for you to become skillful at using teleconsultation] |
| You could use teleconsultation if: |
| [SI1.People who are important to you think that you should use it] |
| [SI2.Your environment (family, friends) influences your intention to use it] |
| [SI3.This gives you higher status than those who do not use teleconsultation] |
| [SI4.Healthcare staff encourage the use of teleconsultation] |
| Regarding teleconsultation, you think that: |
| [FC1.You have IT knowledge to use this solution] |
| [FC2.You can get help around in case of difficulties] |
| [FC3.Teleconsultation is compatible with other technologies you use] |
| [FC4.You have the necessary training to use this solution] |
| You would say: |
| [HA1.Using teleconsultation could become a habit for you] |
| [HA2.You could become “addicted” to the use of teleconsultation] |
| [HA3.You could use teleconsultation often] |
| [HA4.Using teleconsultation could become natural to you] |
| You think that: |
| [PR1.The use of teleconsultation would result in a loss of confidentiality, because the information could be used without your knowledge] |
| [PR2.Using a teleconsultation would not correspond to your personal values or your self-image] |
| [PR3.To learn how to use and adapt teleconsultation would be a significant waste of time] |
| [PR4.The use of teleconsultation would cause risks for the treatment and diagnosis of patients] |
| You would say about you that: |
| [PI1.You like to experiment with technological innovations] |
| [PI2.If you hear about a new technology, you want to try it] |
| [PI3.In your entourage, you are usually the first to try new technology] |
| You are convinced that you can: |
| [SE1.use teleconsultation if you can call someone in case of problems] |
| [SE2.deal with most of the problems you might encounter while using teleconsultation] |
| [SE3.stay calm when you face difficulties in teleconsultation use because you can count on your skills] |
| Thanks to the teleconsultation available 24/7: |
| [AV1.You can get the care you need on time] |
| [AV2.You can consult when you are available] |
| [AV3.Teleconsultation will always be available when you need it] |
| Do you think that teleconsultation solutions can prevent you from being contaminated by viruses: |
| [CA1.On the way to your doctor's office] |
| [CA2.In the waiting room in contact with other patients] |
| [CA3.In contact with your doctor] |
| [CA4.By touching contaminated objects (door handles, chairs, etc.)] |
References
- Alaiad A., Zhou L. The determinants of home healthcare robots adoption: an empirical investigation. Int. J. Med. Inform. 2014;83(11):825–840. doi: 10.1016/j.ijmedinf.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Alalwan A.A., Dwivedi Y.K., Rana N.P., Algharabat R. Examining factors influencing Jordanian customers’ intentions and adoption of internet banking: extending UTAUT2 with risk. J. Retail. Consum. Serv. 2018;40:125–138. [Google Scholar]
- Alazzam M.B., Basari A.S.H., Sibghatullah A.S., Ibrahim Y.M., Ramli M.R., Naim M.H. Trust in stored data in EHRs acceptance of medical staff: using UTAUT2. Int. J. Appl. Eng. Res. 2019;11(4):2737–2748. [Google Scholar]
- Banerjee M., Chakraborty S., Pal R. Diabetes self-management amid COVID-19 pandemic. Diabete. Metabolic Syndrome. 2020;14(4):351–354. doi: 10.1016/j.dsx.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashshur R.L., Shannon G.W., Krupinski E.A., Grigsby J., Kvedar J.C., Weinstein R.S., Merrell R.C. National telemedicine initiatives: essential to healthcare reform. Telemedicine and e-Health. 2009;15(6):600–610. doi: 10.1089/tmj.2009.9960. [DOI] [PubMed] [Google Scholar]
- Basaglia S., Caporarello L., Magni M., Pennarola F. Individual adoption of convergent mobile phone in Italy. Rev. Manag. Sci. 2009;3:1–18. [Google Scholar]
- Baudier P., Ammi C., Lecouteux A. Employees’ acceptance of the healthcare internet of things: a source of innovation in corporate human resource policies. J. Innovat. Econ. Manag. 2019;3:89–111. [Google Scholar]
- Baudier P., Kondrateva G., Ammi C. The future of telemedicine Cabin? Futures. 2020;122 doi: 10.1016/j.futures.2020.102595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezançon M., Guiot D., Le Nagard E. The role of negative physical contagion in the online purchase of second-hand products. Recherche et Appl. en Market. 2019;34(4):2–28. [Google Scholar]
- Bloch P.H., Brunel F.F., Arnold T.J. Individual differences in the centrality of visual product aesthetics: concept and measurement. J. Consum. Res. 2003;29(4):551–565. [Google Scholar]
- Bongiovanni A., Mercatali L., Fausti V., Ibrahim T. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey. Eur. J. Cancer. 2020;134:3–5. doi: 10.1016/j.ejca.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonsaksen T., Kottorp A., Gay C., Fagermoen M.S., Lerdal A. Rasch analysis of the general self-efficacy scale in a sample of persons with morbid obesity. Health Qual. Life Outcomes. 2013;11(1):202–213. doi: 10.1186/1477-7525-11-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calton B., Abedini N., Fratkin M. Telemedicine in the time of coronavirus. J. Pain. Symptom. Manage. 2020;60(1):12–14. doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchill G.A., Jr A paradigm for developing better measures of marketing constructs. J. Market. Res. 1979;16:64–73. [Google Scholar]
- Cimperman M., Brenčič M.M., Trkman P. Analyzing older users’ home telehealth services acceptance behavior-applying an extended UTAUT model. Int. J. Med. Inform. 2016;90:22–31. doi: 10.1016/j.ijmedinf.2016.03.002. [DOI] [PubMed] [Google Scholar]
- Compeau D.R., Higgins C.A. Computer self-efficacy: development of a measure and initial test. MIS Q. 1995:189–211. [Google Scholar]
- Currie W. Health organizations’ adoption and use of mobile technology in France, the USA and UK. Procedia Comput. Sci. 2016;98:413–418. [Google Scholar]
- Davarpanah A.H., Mahdavi A., Sabri A., Langroudi T.F., Kahkouee S.…Tuchayi A.M. Novel screening and triage strategy in Iran during deadly Coronavirus disease 2019 epidemic: Value of humanitarian teleconsultation service. J. Am. College Radiol. 2020;17(6):734–738. doi: 10.1016/j.jacr.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado-Rodriguez M., Llorca J. Bias. J. Epidemiol. Commun. Health. 2004;58(8):635–641. doi: 10.1136/jech.2003.008466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Veer A.J., Peeters J.M., Brabers A.E., Schellevis F.G., Rademakers J.J.J., Francke A.L. Determinants of the intention to use e-Health by community dwelling older people. BMC Health Serv. Res. 2015;15(1):103. doi: 10.1186/s12913-015-0765-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhiman N., Arora N., Dogra N., Gupta A. Consumer adoption of smartphone fitness apps: an extended UTAUT2 perspective. J. Indian Bus. Res. 2019;12(3):363–388. [Google Scholar]
- Duarte P., Pinho J.C. A mixed methods UTAUT2-based approach to assess mobile health adoption. J. Bus. Res. 2019;102:140–150. [Google Scholar]
- Fan W., Liu J., Zhu S., Pardalos P.M. Investigating the impacting factors for the healthcare professionals to adopt artificial intelligence-based medical diagnosis support system (AIMDSS) Ann. Oper. Res. 2018:1–26. [Google Scholar]
- Gao Y., Li H., Luo Y. An empirical study of wearable technology acceptance in healthcare. Ind. Manag. Data Syst. 2015;115(9):1704–1723. [Google Scholar]
- Greenhalgh T., Wherton J., Shaw S., Morrison C. Video consultations for covid-19. BMJ 2020. 2020:368. doi: 10.1136/bmj.m998. [DOI] [PubMed] [Google Scholar]
- Gutierrez M.A., Moreno R.A., Rebelo M.S.… . In: In Global health Informatics. De Fatima Marin H., Massad E, Sigulem D, editors. Academic Press; pp.: 2017. Information and communication technologies and global health challenges; pp. 50–93. [Google Scholar]
- Guzzo T., Ferri F., Grifoni P. A model of e-commerce adoption: consumer’s perceptions and behaviours. Behav. Inf. Technol. 2016;35(3):196–209. [Google Scholar]
- Hazée S., Van Vaerenbergh Y. Customers’ contamination concerns: an integrative framework and future prospects for service management. J. Serv. Manag. 2020 doi: 10.1108/JOSM-04-2020-0129. [DOI] [Google Scholar]
- Hofstede J., de Bie J., Van Wijngaarden B., Heijmans M. Knowledge, use and attitude toward eHealth among patients with chronic lung diseases. Int. J. Med. Inform. 2014;83(12):967–974. doi: 10.1016/j.ijmedinf.2014.08.011. [DOI] [PubMed] [Google Scholar]
- Holden R.J., Karsh B.T. The technology acceptance model: its past and its future in health care. J. Biomed. Inform. 2010;43(1):159–172. doi: 10.1016/j.jbi.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander J.E., Carr B.G. Virtually perfect?: telemedicine for COVID-19. New Engl. J. Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- Hoque R., Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: an extension of the UTAUT model. Int. J. Med. Inform. 2017;101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002. [DOI] [PubMed] [Google Scholar]
- Hsiao J.L., Chang H.C., Chen R.F. A study of factors affecting acceptance of hospital information systems: a nursing perspective. J. Nurs. Res. 2011;19(2):150–160. doi: 10.1097/JNR.0b013e31821cbb25. [DOI] [PubMed] [Google Scholar]
- Hsu C.L., Lee M.R., Su C.H. The role of privacy protection in healthcare information systems adoption. J. Med. Syst. 2013;37(5):9966. doi: 10.1007/s10916-013-9966-z. [DOI] [PubMed] [Google Scholar]
- Jackson J.D., Mun Y.Y., Park J.S. An empirical test of three mediation models for the relationship between personal innovativeness and user acceptance of technology. Inf. Manag. 2013;50(4):154–161. [Google Scholar]
- Jewer J. Patients’ intention to use online postings of ED wait times: a modified UTAUT model. Int. J. Med. Inform. 2018;112:34–39. doi: 10.1016/j.ijmedinf.2018.01.008. [DOI] [PubMed] [Google Scholar]
- Jin H., Lu L., Liu J., Cui M. Complex emergencies of COVID-19: management and experience in Zhuhai. Int. J. Antimicrob. Agents. 2020;55(5) doi: 10.1016/j.ijantimicag.2020.105961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Júnior A.J.M., Pauna H.F. Distance learning and telemedicine in the area of Otorhinolaryngology: lessons in times of pandemic. Braz. J. Otorhinolaryngol. 2020;86(3):271–272. doi: 10.1016/j.bjorl.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabadayi S., O’Connor G.E., Tuzovic S. Viewpoint: the impact of coronavirus on service ecosystems as service mega-disruptions. J. Serv. Market. 2020 doi: 10.1108/JSM-03-2020-0090. [DOI] [Google Scholar]
- Katafuchi Y., Kurita K., Managi S. COVID-19 with stigma: theory and evidence from mobility data. Econ. Disaster. Climate Change. 2020 doi: 10.1007/s41885-020-00077-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J.N., Sinha S.S., Alviar C.L., Dudzinski D.M.…van Diepen S. COVID-19 and disruptive modifications to cardiac critical care delivery. Journal of the American College of Cardiology. 2020;76(1):72–84. doi: 10.1016/j.jacc.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim C.W., Song H.R. Structural relationships among public’s risk characteristics, trust, risk perception and preventive behavioral intention: the case of MERS in Korea. Crisisnomy. 2017;13:85–95. [Google Scholar]
- Kolbe N., Killu K., Coba V., Neri L., Garcia K.M., McCulloch M., Dulchavsky S. Point of care ultrasound (POCUS) telemedicine project in rural Nicaragua and its impact on patient management. J. Ultrasound. 2015;18(2):179–185. doi: 10.1007/s40477-014-0126-1. ... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondrateva G., Baudier P., Ammi C. International Marketing Trends Conference; Paris: 2020. The Digital Natives’ Paradox: Adoption of Telemedicine Cabin; pp. 16–18. January 2020. [Google Scholar]
- Kohnke A., Cole M.L., Bush R. Incorporating UTAUT predictors for understanding home care patients' and clinician's acceptance of healthcare telemedicine equipment. J. Technol. Manag. Innovat. 2014;9(2):29–41. [Google Scholar]
- Lee I., Kovarik C., Tejasvi T., Pizarro M., Lipoff J.B. Telehealth: helping your patients and practice survive and thrive during the COVID-19 crisis with rapid quality implementation. J. Am. Acad. Dermatol. 2020;82(5):1213. doi: 10.1016/j.jaad.2020.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Rho M.J. Perception of influencing factors on acceptance of mobile health monitoring service: a comparison between users and non-users. Healthc. Inform. Res. 2013;19(3):167–176. doi: 10.4258/hir.2013.19.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado R.A., de Souza N.L., Oliveira R.M., Júnior H.M., Bonan P.R.F. Social media and telemedicine for oral diagnosis and counselling in the COVID-19 era. Oral Oncol. 2020;105 doi: 10.1016/j.oraloncology.2020.104685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moores T.T. Towards an integrated model of IT acceptance in healthcare. Decis. Support Syst. 2012;53(3):507–516. [Google Scholar]
- Morales A.C., Dahl D.W., Argo J.J. Amending the law of contagion: a general theory of property transference. J. Assoc. Consum. Res. 2018;3(4):555–565. [Google Scholar]
- Moroni F., Gramegna M., Ajello S., Beneduce A., Baldetti L., Azzalini L. Collateral damage: medical care avoidance behavior among patients with acute coronary syndrome during the COVID-19 pandemic. JACC: Case Reports. 2020;2(10) doi: 10.1016/j.jaccas.2020.04.010. ... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura H., Managi S. Airport risk of importation and exportation of the COVID-19 pandemic. Transp. Policy (Oxf.) 2020;96:40–47. doi: 10.1016/j.tranpol.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namahoot C.S., Brückner M., Nuntawong C. Mobile diagnosis system with emergency telecare in Thailand. Procedia Comput. Sci. 2015;69:86–95. [Google Scholar]
- Nohara Y., Kai E., Ghosh P.P., Islam R., Ahmed A., Kuroda M., Kobayashi K. Health checkup and telemedical intervention program for preventive medicine in developing countries: verification study. J. Med. Internet Res. 2015;17(1):e2. doi: 10.2196/jmir.3705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohannessian R., Duong T.A., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveillance. 2020;6(2):e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega-Egea J.M., Roman-Gonzales M.V. Explaining physicians’ acceptance of EHCR systems: an extension of the TAM with trust and risk factors. Comput. Human. Behav. 2011;27:319–332. [Google Scholar]
- Patel R.S., Bachu R., Adikey A., Malik M., Shah M. Factors related to physician burnout and its consequences: a review. Behav. Sci. 2018;8(11):98. doi: 10.3390/bs8110098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan K., Daim T.U. Exploring technology acceptance for mobile services. J. Ind. Eng. Manag. 2011;4(2):339–360. [Google Scholar]
- Pollock K., Setzen M., Svider P.F. Embracing telemedicine into your otolaryngology practice amid the COVID-19 crisis: an invited commentary. Am. J. Otolaryngol. 2020 doi: 10.1016/j.amjoto.2020.102490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portnoy J., Waller M., Elliott T. Telemedicine in the Era of COVID-19. J. Allergy Clin. Immunol. 2020;8(5):1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachmat H.H., Octovia L.I., Soegijoko S. Development of a simple e-health system for tuberculosis management at community health center level in Indonesia. Med-e-Tel 2009 Proc. 2009:366–369. [Google Scholar]
- Ravangard R., Kazemi Z., Abbasali S.Z., Sharifian R., Monem H. Development of the UTAUT2 model to measure the acceptance of medical laboratory portals by patients in Shiraz. Electron. Physician. 2017;9(2):3862. doi: 10.19082/3862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scotté F., Minvielle E., Mir O., André F., Barlesi F., Soria J.C. A patient reported outcome platform, a useful tool to improve monitoring and effective management of Covid-19–positive patients with cancer. Eur. J. Cancer. 2020;132:1. doi: 10.1016/j.ejca.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setzen M., Svider P.F., Pollock K. COVID-19 and rhinology: a look at the future. Am. J. Otolaryngol. 2020 doi: 10.1016/j.amjoto.2020.102491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu L., Ji N., Chen X., Feng G. Ark of life and hope: role of cabin hospital in facing COVID-19. J. Hosp. Infect. 2020;105(2):351–352. doi: 10.1016/j.jhin.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterpetti A.V. Lessons learned during the COVID-19 virus pandemic. J. Am. Coll. Surg. 2020;230(6):1092–1093. doi: 10.1016/j.jamcollsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., Yu K., Xie Z., Pan X. China empowers Internet hospital to fight against COVID-19. J. Infect. 2020;81(1):67–68. doi: 10.1016/j.jinf.2020.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suresh S., Nath L. Challenges in managing telemedicine centers in remote tribal hilly areas of Uttarakhand. Indian J. Community Health. 2013;25(4):372–380. [Google Scholar]
- Tavares J., Goulao A., Oliveira T. Electronic health record portals adoption: empirical model based on UTAUT2. Inform. Health Soc. Care. 2018;43(2):109–125. doi: 10.1080/17538157.2017.1363759. [DOI] [PubMed] [Google Scholar]
- Trilla A. One world, one health: the novel coronavirus COVID-19 epidemic. Med. Clin. (Barc.) 2020;154(5):175. doi: 10.1016/j.medcli.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh V., Morris M.G., Davis G.B., Davis F.D. User acceptance of information technology: toward a unified view. MIS Q. 2003:425–478. [Google Scholar]
- Venkatesh V., Thong J.Y., Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q. 2012;36(1):157–178. [Google Scholar]
- Wang H., Tao D., Yu N., Qu X. Understanding consumer acceptance of healthcare wearable devices: an integrated model of UTAUT and TTF. Int. J. Med. Inform. 2020 doi: 10.1016/j.ijmedinf.2020.104156. [DOI] [PubMed] [Google Scholar]
- Wen C.L.… . In: In Global Health Informatics. De Fatima Marin H., Massad E, Sigulem D, editors. Academic Press; Eds: 2017. Telemedicine, ehealth and remote care systems; pp. 168–194. [Google Scholar]
- Wu L., Li J.Y., Fu C.Y. The adoption of mobile healthcare by hospital’s professionals: an integrative perspective. Decis. Support Syst. 2011;51(3):587–596. [Google Scholar]
- Yoo S., Managi S. Global mortality benefits of COVID-19 action. Technol Forecast Soc Change. 2020;160 doi: 10.1016/j.techfore.2020.120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Ni Q., Zhou R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manage. 2018;43:342–350. [Google Scholar]
- Zhu Z., Liu Y., Che X., Chen X. Moderating factors influencing adoption of a mobile chronic disease management system in China. Inform. Health Social Care. 2018;43(1):22–41. doi: 10.1080/17538157.2016.1255631. [DOI] [PubMed] [Google Scholar]