We reported the case of a patient referred for a respiratory rehabilitation program (RRP) after intensive care unit stay, who achieved a meaningful functional recovery after 3 wk of RRP, partially carried out in an ad hoc isolation ward.
Keywords: acute respiratory distress syndrome, COVID-19, intensive care unit, muscle weakness, respiratory rehabilitation
Details of the Clinical Case:
A 51-yr-old man underwent a respiratory rehabilitation program (RRP), after being tracheostomized and ventilated due to acute respiratory distress syndrome (ARDS) from coronavirus disease-2019 (COVID-19) infection. Respiratory care, early mobilization, and neuromuscular electrical stimulation were started in the ad hoc isolation ward of our rehabilitation center. At baseline, muscle function was consistent with intensive care unit-acquired weakness and the patient still needed mechanical ventilation (MV) and oxygen support. During the first week of RRP in isolation, the patient was successfully weaned from MV, the tracheal cannula was removed, and the walking capacity was recovered. At the end of the RRP, continued in a standard department, respiratory muscles strength increased by 7% and muscle function improved as indicated by the quadriceps size enlargement of 13% and the change of the Medical Research Council sum score from 48/60 to 58/60.
Discussion:
Providing RRP in patients with severe COVID-19 ARDS involves risks for operators and organizational difficulties, especially in rehabilitation centers; nevertheless, its continuity is important to prevent the development of permanent disabilities in previously healthy subjects. Limited to the experience of only one patient, we were able to carry out a safe RRP during the COVID-19 pandemic, promoting the complete functional recovery of a COVID-19 young patient.
Summary:
Most patients who develop serious consequences of COVID-19 infection risk a reduction in their quality of life. However, by organizing and directing specialized resources, subacute rehabilitation facilities could ensure the continuity of the RRPs even during the COVID-19 pandemic.
Worldwide, a relevant proportion of patients hospitalized for coronavirus disease-2019 (COVID-19) developed a severe acute respiratory distress syndrome (ARDS), requiring intubation and mechanical ventilation (MV) support in the intensive care unit (ICU).1 In Lombardy, the Italian region most affected by COVID-19, 36% of patients admitted to the ICU ranged between 40 and 60 yr, (83% males) and 28% had no comorbidities at the time of hospitalization. Survivors were discharged from the ICU after a median length of stay of 8 d and accounted for 32% of all patients.2
As a result of immobilization and prolonged MV, the recovery of respiratory and physical functions may take a long time after the patient's discharge from the ICU, or sometimes only a partial recovery is achieved, leading to a reduction in quality of life.3 The ICU-acquired weakness affects both peripheral and respiratory skeletal muscles of critical patients and represents one of the most serious consequences of prolonged immobilization, delaying weaning from MV and extending the hospital length of stay.4
Relevance of a respiratory rehabilitation program (RRP) in improving the clinical course of critically ill patients and recovering their functional capacities is well documented5; however, rehabilitation programs must deal with the organizational problems and risks related to COVID-19 emergency.6
In this case report, we described the RRP in a patient with severe COVID-19 ARDS, referred to the tertiary subacute IRCCS Fondazione Don Gnocchi rehabilitation center (Rovato, Italy) in a newly established isolation ward.
CASE DESCRIPTION
A 51-yr old man, resident in Lombardy (Italy), with nonsmoking history and no comorbidities, was referred to our center for rehabilitation from a local hospital, with the diagnosis of COVID-19 severe ARDS.7
On March 15, the patient was admitted in the emergency department with persistent fever, cough, and dyspnea, while the chest x-ray showed bilateral interstitial thickening and consolidation of the lung parenchyma. The following day, the patient was transferred to the ICU for invasive MV and life support due to acute hypoxemic respiratory failure. On March 23, percutaneous tracheostomy was performed for the prolonged necessity of MV.
On March 27, the patient was transferred to our center and placed in the isolation ward set up for COVID-19 infection. On the second day of hospitalization (T0), 2 physiotherapists with ICU and respiratory rehabilitation experience carried out the baseline assessment and the first treatment. Baseline evaluations are detailed in Table 1 and included measures of body composition, muscle function, as well as questionnaires on functionality, dyspnea, and quality of life, while respiratory tests were avoided due to the risk of droplet production. Physiotherapists were allowed to access the isolation ward wearing the appropriate personal protective equipment from Monday to Saturday, and each treatment session took place in the patient's room for 30-45 min, once a day. After 2 consecutive negative swabs for COVID-19 infection, the patient was moved to a COVID-free ward, where he exercised 6 d/wk, 30-45 min twice/d, with the possibility to access a common area temporarily equipped as a gym.
Table 1. Timeline of Evaluation Measurements and RRP Components.
| Timeline | COVID Ward T0 | COVID-Free Ward | |
|---|---|---|---|
| T1 | T2 | ||
| Measures | BI BID EQ-5D-3L MRC sum score Q girth SPPB |
Repeated T0 MIP/MEP |
Repeated T1 Spirometry |
| RRP | Early mobilization Leg/arm cranking NMES STS training Walking training Weaning from MV |
Aerobic training (cycle ergometer) Resistance training (elastic bands/free weights) Stair climbing |
|
Abbreviations: BI, Barthel index; BID, Barthel index based on dyspnea; COVID, coronavirus disease; EQ-5D-3L, EuroQol questionnaire—5 dimensions, 3 levels; MEP, maximal expiratory pressure; MIP, maximal inspiratory pressure; MRC sum score, Medical Research Council sum score; MV, mechanical ventilation; NMES, neuromuscular electrical stimulation; Q girth, quadriceps size (taken 10 cm above patella); RRP, respiratory rehabilitation program; SPPB, Short Physical Performance Battery; STS, seat-to-stand.
On March 28, under the supervision of the lung specialist and according to previous guidelines,8 physiotherapists started the weaning procedure from MV. However, during the first attempt of spontaneous breathing trial, the patient's Spo2 reduced to <90% and heart rate increased >130 beats/min within 30 min, suggesting excessive respiratory effort and forcing physiotherapists to reintroduce MV. Therefore, on March 30, a second attempt for the spontaneous breathing trial was performed using a threshold positive expiratory pressure device (Philips) set at 10 cm H2O for 20 min, with the aim to increase lung recruitment and improve oxygenation. Then, due to the good compliance of the patient, physiotherapists progressed to the speaking valve with 5 L/min of supplemental oxygen. In addition, the RRP included recovery and maintenance of the sitting position and quadriceps strengthening with neuromuscular electrical stimulation (T-ONE Coach, I-TECH) via squared electrodes (48 × 48 mm) and amplitude between 15 and 20 mA for 30 min.
On March 31, the patient progressed to maintain spontaneous breathing during the whole day, with supplemental oxygen at 3 L/min via nasal cannula (NC). Besides, the training program was integrated with sit-to-stand training and seated leg or arm cranking for 20-30 min.
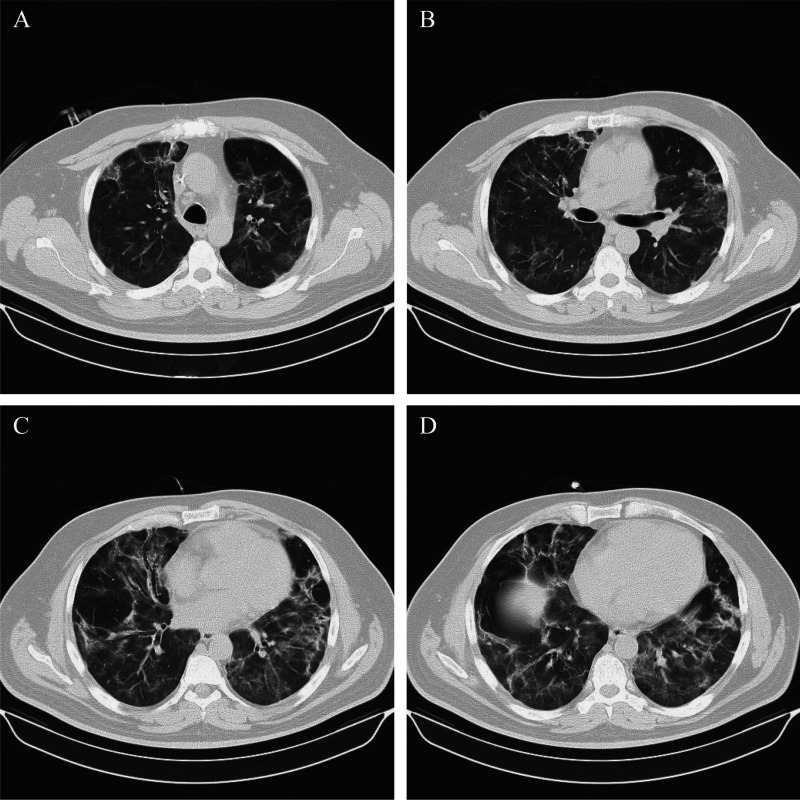
On April 1, despite computed tomography showing parenchymal alterations in both lungs (Figure), the patient was successfully weaned from MV with supplemental oxygen via NC at 1 L/min for rest and 3 L/min for activity. Walking with assistance and balance training, both limited to the patient's room, were added to the RRP and continued until the patient progressed to walk without assistance and independently carried out activities of daily living.
Figure.
Computed tomography scans taken at different levels, from top (A) to bottom (D), shows multiple “ground-glass” areas with increased parenchymal density in both lungs. The main consolidations are in the medium and in the inferior pulmonary lobe of both lungs.
On April 7, after 7 d without MV support, the patient's tracheal cannula was removed by the lung specialist and on April 9, the RRP continued in a COVID-free ward without access restrictions for physiotherapists, as previously reported. The intermediate evaluation (T1) included baseline measurements with MicroRPM (Vyaire Medical) integrated maximal inspiratory and expiratory mouth pressure, while aerobic training with cycle ergometer was included in the RRP, starting from the default resistance of 20 W for 20-30 min. The workload was increased by 10 W if the Borg score was <4, kept equal if the score was between 4 and 6 or reduced by 10 W if the score was >6. In addition, resistance exercises with elastic bands or free weights were performed for 3 sets of 8-10 repetitions with an intensity of 50-70% of 1 repetition maximum.9
However, despite the improvement in exercise tolerance, the patient still required supplemental oxygen via NC at 1 L/min for rest and 2 L/min for activity until April 17, when he was able to train without oxygen support.
On April 21, before the discharge, physiotherapists carried out the final evaluations (T2), including lung function, obtained with a Spiropalm (Cosmed) portable spirometer (Table 2).
Table 2. Principal Variations in Functional Parameters Before, During, and After the RRP.
| Variable | COVID Ward T0 (March 27) | COVID-Free Ward | |
|---|---|---|---|
| T1 (April 9) | T2 (April 21) | ||
| Blood samples | |||
| pH | 7.444 | 7.474 | 7.447 |
| Pao2, mm Hg | 79.9 | 76.3 | 84 |
| Paco2, mm Hg | 33.1 | 46.8 | 34.8 |
| Hb, g/dL | 10.5 | 9.1 | 8.9 |
| MV settings | |||
| Mode | PSV | np | np |
| PEEP, cm H2O | 8 | np | np |
| Fio2, % (activity) | 45 (45) | 24 (28) | 21 (21) |
| Pao2/Fio2 ratio | 177 | 246 | 400 |
| Respiratory function | |||
| BID | 61/100 | 9/100 | 0/100 |
| MIP/MEP, cm H2O (% predicted) | np | 68 (59)/83 (38) | 79 (68)/98 (45) |
| FEV1/FVC, % | np | np | 83.8 |
| FEV1, L (% predicted) | np | np | 2.49 (64) |
| FVC, L (% predicted) | np | np | 2.97 (60) |
| VC, L (% predicted) | np | np | 2.92 (59) |
| Functional capacity | |||
| BI | 19/100 | 99/100 | 100/100 |
| EQ-5D-3L12 | 12/15 | 6/15 | 5/15 |
| SPPB13 | 0/12 | 11/12 | 12/12 |
| Body composition and muscle strength | |||
| BMI, kg/m2 | 27.5 | 27.9 | 28.4 |
| MRC sum score4 | 48/60 | 52/60 | 58/60 |
| Q girth, cm (left/right) | 41.5/42 | 44/44 | 48/49 |
Abbreviations: BI, Barthel index; BID, Barthel index based on dyspnea; BMI, body mass index; COVID, coronavirus disease; EQ-5D-3L, EuroQol questionnaire—5 dimensions, 3 levels; FEV1, forced expired volume in the first second; Fio2, fraction of inspired oxygen; FVC, functional vital capacity; Hb, hemoglobin; MEP, maximal expiratory pressure; MIP, maximal inspiratory pressure; MRC sum score, Medical Research Council sum score; MV, mechanical ventilation; np, not performed; Pao2, arterial pressure of oxygen; Paco2, arterial pressure of carbon dioxide; PEEP, positive end-expiratory pressure; PVS, pressure ventilation support; Q girth, quadriceps size (taken 10 cm above patella); RRP, respiratory rehabilitation program; SPPB, Short Physical Performance Battery; VC, vital capacity.
DISCUSSION
COVID-19 survivors, particularly those who developed severe respiratory symptoms and had prolonged ICU stay, may benefit from respiratory and functional rehabilitation in the subacute phase of the disease.10 However, in the early stage of the emergency, the area of postacute rehabilitation has been used to unload the collapsed hospitals and therefore reorganized for a less specialized activity. For this reason, together with the high risk of contagion during an RRP, rehabilitation activity in critical patients may have been seriously reduced, leading to a worsening of long-term functional outcomes and quality of life in COVID-19 survivors. In addition, the discontinuation of MV in critical patients is a time-consuming part of the rehabilitation process. Therefore, the need to unload territorial ICUs requires experienced physiotherapists in the subacute rehabilitation centers to be able to perform this procedure effectively and safely for the patient.
We reported the case of a young patient without comorbidities who developed severe ARDS due to COVID-19 infection and arrived to our rehabilitation center with tracheostomy and MV support, after an ICU length of stay of 12 d. The RRP performed in the COVID-ward, with the lack of continuous feedback between physiotherapists, lung specialist and patient, and the limited setting and evaluation tools, could have delayed the patient's progress. Nevertheless, we promoted a spontaneous breathing trial, breathing exercises, and early mobilization of the patient also in the COVID ward. As a result, after 5 d from ICU discharge, the patient had been completely weaned from MV and after 12 d since the arrival in our center, the tracheal cannula had been removed. Furthermore, the muscle function of the patient was initially consistent with ICU-acquired weakness diagnosis, as previously seen in >30% of subjects recovering from ARDS.11 Nevertheless, the patient achieved autonomous walking within 1 wk from ICU discharge, and he showed at the intermediate evaluation (T1) an almost normal functional capacity. The rehabilitation program was improved after the transition to a COVID-free ward; however, some essential parts of the pre-COVID RRP such as the 6-min walk test, useful to define the workload for the patient, remained unavailable. At T2, after 26 d from ICU discharge and 38 d of hospitalization overall, the patient showed a recovered muscle function and increased quadriceps size (13%) from the baseline assessment. Maximal inspiratory pressure and maximal expiratory pressure results showed a 7% improvement, although remained under normal values compared with age-matched subjects. In contrast, the lung function was consistent with a pulmonary restrictive pathology, even if comparisons with pre-COVID or initial values are not possible.
To our knowledge, this is the first report describing the subacute rehabilitation program and its outcomes, after a severe form of ARDS due to COVID-19 infection. Because of the recent outbreak of the virus, in the scientific literature there are no available data for comparison with our results. In general, young patients developing ARDS due to various conditions have an average hospitalization length of stay of 48 d, while the functional capacity at 3 mo post-ICU discharge is poor, as well as the number of previously active patients who returned to work. Recovery of pulmonary function is also incomplete among ARDS patients, showing mean forced expiratory volume in 1 sec and forced vital capacity results at 75% and 72% of predicted values, respectively.11
Our findings are related exclusively to the reported case and this is the main limitation of this investigation. A second limitation is derived from the necessity to carry out the patient's assessment with simple tests and minimum or no equipment, with the baseline assessment performed in isolation more limited than the final evaluation.
In conclusion, despite the risk of contagion, the personal protective equipment consumption and the rehabilitative setting limitation, targeting rehabilitation resources such as physiotherapists and health care professionals with experience of critical patients, could improve functional outcomes in those patients with severe consequences of COVID-19 infection who are at high risk of developing disabilities. We hope that the continuity of rehabilitation treatments will be maintained by the specialized subacute rehabilitation facilities during the COVID-19 pandemic, despite considerable organizational difficulties.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance V 1.2. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Published 2020. Accessed April 10, 2020.
- 2.Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herridge MS. Recovery and long-term outcome in acute respiratory distress syndrome. Crit Care Clin. 2011;27(3):685–704. [DOI] [PubMed] [Google Scholar]
- 4.Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(17):1626–1635. [DOI] [PubMed] [Google Scholar]
- 5.Connolly B, Salisbury L, O'Neill B, et al. Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst Rev. 2015;2015(6):CD008632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedersini P, Corbellini C, Villafane JH. Italian physical therapists' response to the novel COVID-19 emergency [published online ahead of print April 13, 2020]. Phys Ther. doi:10.1093/ptj/pzaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. [DOI] [PubMed] [Google Scholar]
- 8.Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29(5):1033–1056. [DOI] [PubMed] [Google Scholar]
- 9.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. [DOI] [PubMed] [Google Scholar]
- 10.Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–693. [DOI] [PubMed] [Google Scholar]
- 12.Scalone L, Cortesi PA, Ciampichini R, et al. Italian population-based values of EQ-5D health states. Value Health. 2013;16(5):814–822. [DOI] [PubMed] [Google Scholar]
- 13.Bakhru RN, Davidson JF, Bookstaver RE, et al. Physical function impairment in survivors of critical illness in an ICU recovery clinic. J Crit Care. 2018;45:163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]