The coronavirus disease-2019 (COVID-19) pandemic containment and mitigation strategies may lead to excessive physical inactivity and sedentary behavior, drastically impacting cardiorespiratory fitness and overall health. It is urgent to safely find ways to sit less and move more.
Keywords: cardiorespiratory fitness, coronavirus, physical activity, sedentary time
Abstract
The coronavirus disease-2019 (COVID-19) pandemic containment and mitigation strategies may lead to excessive physical inactivity and sedentary behavior, drastically impacting cardiorespiratory fitness and overall health. It is urgent to safely find ways to sit less and move more.
As the coronavirus disease-2019 (COVID-19) pandemic continues to spread and have a global impact, a combination of critically important containment and mitigation strategies have been implemented worldwide, such as closure of schools and business, shelter in place, and social distancing strategies.
While these strategies are imperative to public health, they may lead to important unintended consequences for health, which include excessive physical inactivity (PI) and sedentary behavior (SB). The activity restrictions and routine disruption imposed by the COVID-19 pandemic have already led to concern that individuals and families are reducing their exercise habits and daily physical activity (PA) in different contexts (occupational, transportation, and leisure), while increasing their sedentary activities (increased time using mobile devices, television, etc).1 In fact, evidence has already emerged to support these concerns—demonstrating a significant reduction in PA, paralleled by a significant increase in SB, during the COVID-19 pandemic.2,3 Physical inactivity and SB are among the leading modifiable risk factors for cardiovascular disease and all-cause mortality, and are contributing causes to ≥35 unhealthy conditions.4 Moreover, while there is no current evidence of a direct protective effect of PA on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, the overwhelming body of established evidence builds a strong rationale for promoting PA during the COVID-19 pandemic.5 Specifically, among the countless benefits of avoiding excessive PI and SB, the positive effects of exercise on the immune system are particularly noteworthy during the COVID-19 pandemic,6 in addition to preventing/managing chronic conditions, reducing anxiety/depression risk, and improving sleep and quality of life. This is especially true for patients with cardiopulmonary diseases,7,8 as their access to rehabilitation programs has been compromised as part of the response to the pandemic.
If in fact the world is moving much less and sitting much more during the COVID-19 pandemic, the timing could not be any worse, given PI and SB have already themselves been defined as a pandemic with catastrophic health consequences. The COVID-19 pandemic may be creating an “imposed physical inactivity model,” which has been used to demonstrate the impact of PI and SB on human health, whereby individuals experimentally transition from high/normal to an imposed low daily ambulatory PA and/or increased sedentary time.9 Evidence has shown that, among a group of young healthy men, a reduction of their normal daily steps from approximately 6000 to 10 000 to approximately 1 400 steps, during only 3 to 5 d, was enough to negatively alter insulin sensitivity, glycemic control, and endothelial function. Longer duration (2-3 wk) resulted in more robust and clinically significant metabolic and functional impairments, with a 7% reduction in maximal oxygen consumption (Vo2max), 17% reduction in peripheral insulin sensitivity, attenuation of post-prandial lipid metabolism, 1.2-kg decrease in total fat-free mass (0.5 kg of it in the leg musculature), and a 7% increase in visceral adipose tissue.9 The rapidity by which Vo2max, a gold standard measure of cardiorespiratory fitness (CRF),10 declines during “imposed physical inactivity models” is particularly disconcerting. Recently, the American Heart Association referred to CRF as a “clinical vital sign, potentially a stronger predictor of mortality than established risk factors such as smoking, hypertension, high cholesterol, and type 2 diabetes mellitus.”11 Simply stated, individuals with a higher CRF, regardless of other health characteristics, have a far better health trajectory while those with a low CRF do far worse. As such, maintaining CRF throughout the lifespan is of paramount importance.12 Moreover, a 7% reduction in Vo2max found after 2–3 wk of reduced physical activity, which would be expected to occur, under normal conditions, after only 10 yr of aging, is particularly troubling.13 In this context, there is significant concern over the long-term consequences of a significant and lasting global increase in PI and SB leading to a decline in CRF post-COVID-19.
Efforts are underway to promote PA during this time. Both the World Health Organization and the American College of Sports Medicine have provided useful and reliable resources to help individuals and families to avoid excessive PI and SB, and to safely maintain their PA.14,15 During (and after) the COVID-19 pandemic, it is imperative, perhaps now more than ever, that the world finds a way to sit less and move more.
In summary:
The COVID-19 pandemic may lead to important unintended consequences for health, such as excessive PI and SB.
Physical inactivity and SB are leading health risk factors, and the current “imposed physical inactivity” can have a drastic impact on CRF and overall health.
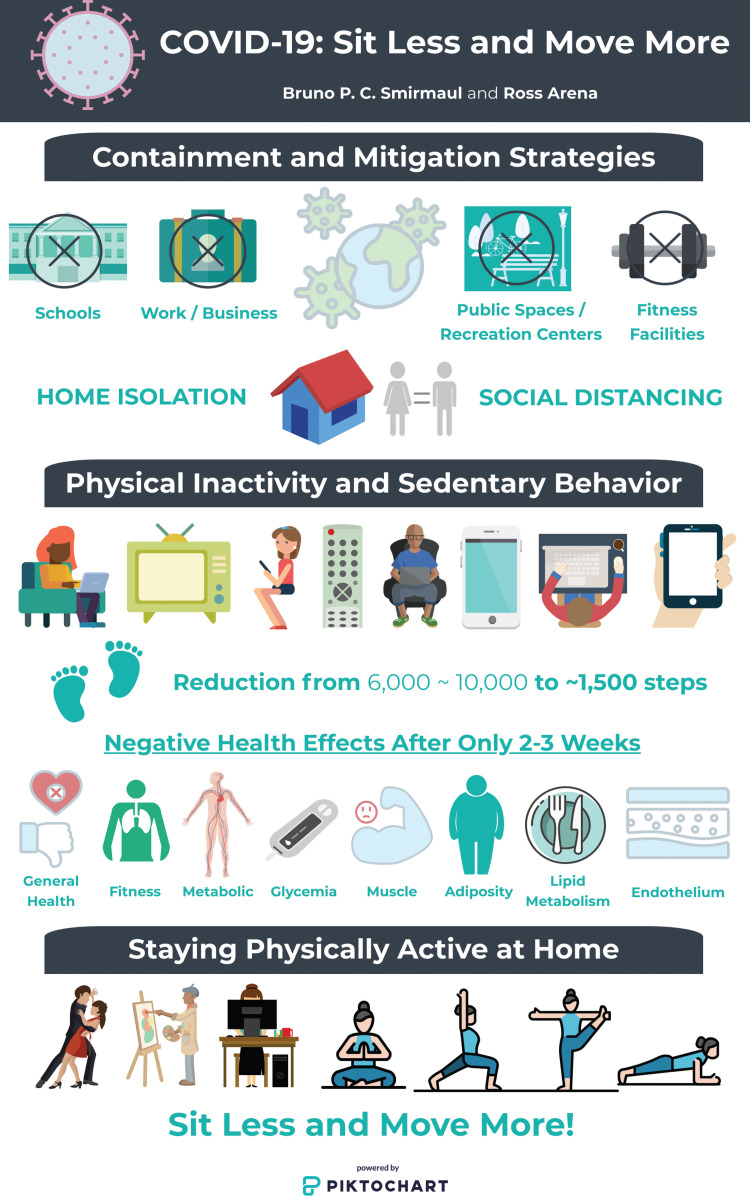
Sitting less and moving more is of paramount importance, now more than ever (Figure).
Figure.
Illustrative summary of the potential effects of the coronavirus disease-2019 (COVID-19) pandemic on physical inactivity (PI) and sedentary behavior (SB), its negative health consequences, and a call to sit less and move more. This figure is available in color online (www.jcrpjournal.com).
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: how will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another [published online ahead of print April 8, 2020]? Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected [published online ahead of print April 30, 2020]. Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyer J, McDowell C, Lansing J, et al. Changes in physical activity and sedentary behaviour due to the COVID-19 outbreak and associations with mental health in 3,052 US adults [published online ahead of print May 6, 2020]. Cambridge Open Engage. doi:10.33774/coe-2020-h0b8g. [Google Scholar]
- 4.Booth FW, Roberts CK, Thyfault JP, Ruegsegger GN, Toedebusch RG. Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Physiol Rev. 2017;97:1351–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laddu DR, Lavie CJ, Phillips SA, Arena R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic [published online ahead of print April 9, 2020]. Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nieman DC, Wentz LM. The compelling link between physical activity and the body's defense system. J Sport Health Sci. 2019;8:201–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlin BW. The Journal of Cardiopulmonary Rehabilitation and prevention at 40 years and its role in the evolution of pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2020;40(2):65–69. [DOI] [PubMed] [Google Scholar]
- 8.Ades PA, Balady GJ, Berra K, et al. The Journal of Cardiopulmonary Rehabilitation and prevention at 40 years and its role in the evolution of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2020;40(1):2–8. [DOI] [PubMed] [Google Scholar]
- 9.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2:1143–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harber MP, Kaminsky LA, Arena R, et al. Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis. 2017;60(1):11–20. [DOI] [PubMed] [Google Scholar]
- 11.Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134(24):e653–e699. [DOI] [PubMed] [Google Scholar]
- 12.Franklin BA, Brubaker PH, Harber MP, Lavie CJ, Myers J, Kaminsky LA. The Journal of Cardiopulmonary Rehabilitation and Prevention at 40 years and its role in promoting lifestyle medicine for prevention of cardiovascular diseases: part 1. J Cardiopulm Rehabil Prev. 2020;40(3):131–137. [DOI] [PubMed] [Google Scholar]
- 13.Kaminsky LA, Arena R, Ellingsen O, et al. Cardiorespiratory fitness and cardiovascular disease—the past, present, and future. Prog Cardiovasc Dis. 2019;62(2):86–93. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization—Regional Office for Europe. Stay physically active during self-quarantine. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/technical-guidance/stay-physically-active-during-self-quarantine. Accessed June 11, 2020.
- 15.American College of Sports Medicine. Staying Physically Active During the COVID-19 Pandemic. https://www.acsm.org/read-research/newsroom/news-releases/news-detail/2020/03/16/staying-physically-active-during-covid-19-pandemic. Accessed June 11, 2020.