The strict lockdown strategy prompted by the Italian government, to hamper severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) spreading, reduced opportunities to perform physical activity. This study quantified an abrupt and statistically significant reduction by 25% of physical activity in patients with implantable defibrillators, during the forced 40-d in-home confinement.
Keywords: cardioverter-defibrillators, COVID-19, physical activity
Purpose:
The coronavirus disease-2019 (COVID-19) pandemic has been spreading rapidly worldwide since late January 2020. The strict lockdown strategy prompted by the Italian government, to hamper severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) spreading, has reduced the possibility of performing either outdoor or gym physical activity (PA). This study investigated and quantified the reduction of PA in patients with automatic implantable cardioverter-defibrillators (ICDs) for primary prevention of sudden death.
Methods:
Daily PA of 24 patients was estimated by processing recorded data from ICD-embedded accelerometric sensors used by the rate-responsive pacing systems.
Results:
During the forced 40-d in-home confinement, a mean 25% reduction of PA was observed as compared with the 40-d confinement-free period (1.2 ± 0.3 vs 1.6 ± 0.5 hr/d, respectively, P = .0001).
Conclusions:
This objective quantification of the impact of the COVID-19 pandemic on PA determined by an ICD device showed an abrupt and statistically significant reduction of PA in primary prevention ICD patients, during the in-home confinement quarantine. To counteract the deleterious effects of physical inactivity during the COVID-19 outbreak, patients should be encouraged to perform indoor exercise-based personalized rehabilitative programs.
The coronavirus disease-2019 (COVID-19) pandemic has prompted many governments to promote strict indoor isolation strategies to hamper the virus spreading by limiting human-to-human transmission. Respect for such necessary, but draconian, recommendations has unavoidably reduced the possibility of performing either outdoor or gym physical activity (PA). Physical inactivity is a major risk factor for cardiovascular disease.1 A large study on 185 000 US subjects reported a steep fall in PA (by 48%) measured by Fitbit trackers since a Federal emergency was declared through April 6.2 However, so far, the literature is sparse regarding precise quantification of a PA decline in cardiac patients during the COVID-19 pandemic. The expected growing prevalence of physical inactivity raises concerns about the maintenance of well-established favorable effects of PA on physical and mental health in such patients.3 The dose-response interaction between the immune system and PA has been described by a J-shaped curve, demonstrating the importance of regular and moderate-intensity exercise to improve the immune system.4,5 Accordingly, there is general agreement in support of keeping physically active during the quarantine, especially for older patients.6
An implantable cardioverter-defibrillator (ICD) is the recommended treatment for either primary or secondary prevention of sudden cardiac death in selected high-risk patients. Light-to-moderate exercise training programs in ICD recipients have resulted in similar benefits as in other cardiac patients.7–10 They also provide potential protective effects against arrhythmic risk through autonomic nervous system balance, metabolic changes, and increasing coronary vascular density and flow. In such patients, an ICD represents a unique tool for continuous monitoring of PA via embedded accelerometric sensors used by the rate-responsive pacing systems.11
The aim of this study was to investigate and quantify changes in PA during the in-home confinement in patients implanted with ICDs.
METHODS
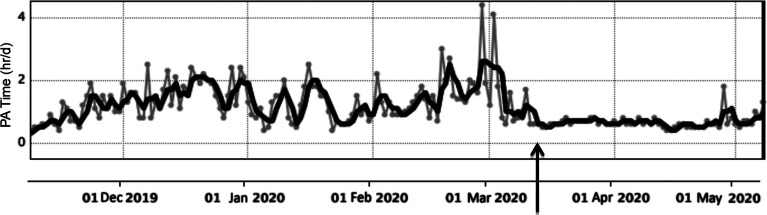
We analyzed data of 24 patients (72 ± 10 yr, 17 males) implanted with ICDs (Boston Scientific) for primary prevention of sudden death and with home-monitoring follow-up. Such ICDs enable a continuous monitoring and recording of PA via embedded accelerometric sensors used by the rate-responsive pacing systems. Recorded data were then processed by a specific algorithm and translated into estimates of time spent in movement, that has been used as surrogate of PA.11 Device-based recordings of patient PA levels were quantified as hr/d and assessed across two timespans: 40 d before and 40 d after the national lockdown began, respectively (Figure).
Figure.
A patient's daily physical activity over time. The fragmented gray curve indicates daily activity in hours, whereas the smooth curve represents mean values by 3-d groups. The arrow indicates the beginning of the in-home confinement quarantine over the whole national Italian territory (March 12, 2020); from this date onward, the curve falls abruptly down and appears flat with little daily variation of physical activity.
RESULTS
During the forced 40-d in-home confinement, a 25% mean reduction of PA was observed as compared to the 40-d confinement-free period (mean 1.6 ± 0.5 vs 1.2 ± 0.3 hr/d, respectively, P = .0001). Since left ventricular systolic dysfunction is not uncommon in primary prevention ICD patients, baseline exercise performance is expected to be low12 and this may account for the relatively shallow decline in PA of our patients. Thus, data were reanalyzed after excluding very inactive patients (ie, PA <1 hr/d), but results did not change showing a significant decrease in PA after lockdown began (2.0 ± 0.6 vs 1.5 ± 0.4 hr/d, respectively, P = .0001).
DISCUSSION
This may be the first objective quantification of the impact of the COVID-19 pandemic on PA determined by an ICD device. An abrupt cessation of physical exercise has been associated with rapid loss of PA-related benefits. A mild reduction by even 25% of daily PA in poorly trained ICD patients may underlie a clinically significant worsening of frailty (eg, increasing fall risk) and loss of metabolic, cardiovascular, and musculoskeletal conditioning within just two weeks. To counteract the deleterious effects of physical inactivity during the COVID-19 outbreak, patients should be encouraged to perform indoor exercise-based personalized rehabilitative programs.13–15
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Kaminsky LA, Brubaker PH, Guazzi M, et al. Assessing Physical Activity as a Core Component in Cardiac Rehabilitation: A Position statement of the American Association of Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehabil Prev. 2016;36(4):217–229. [DOI] [PubMed] [Google Scholar]
- 2.Evidation Health, Inc. COVID-19 pulse: delivering regular insights on the pandemic from a 150,000+ person connected cohort. https://evidation.com/news/covid-19-pulse-first-data-evidation/. Updated April 15, 2020.
- 3.Lippi G, Henry BM, Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19) [published online ahead of print April 9, 2020]. Eur J Prev Cardiol. doi:10.1177/2047487320916823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kakanis MW, Peake J, Brenu EW, et al. The open window of susceptibility to infection after acute exercise in healthy young male elite athletes. Exerc Immunol Rev. 2010;16:119–137. [PubMed] [Google Scholar]
- 5.Rahmati-Ahmadabad S, Hosseini F. Exercise against SARS-CoV-2 (COVID-19): does workout intensity matter? (A mini review of some indirect evidence related to obesity). Obes Med. 2020;19;100245. doi:10.1016/j.obmed.2020.100245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pavon DJ, Baeza AC, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people [published online ahead of print March 24, 2020]. Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vanhees L, Kornaat M, Defoor J, et al. Effect of exercise training in patients with an implantable cardioverter defibrillator. Eur Heart J. 2004;25(13):1120–1126. [DOI] [PubMed] [Google Scholar]
- 8.Alswyan AH, Sauer Liberato AC, Dougherty CM. A systematic review of exercise training in patients with cardiac implantable devices. J Cardiopulm Rehabil Prev. 2018;38(2):70–84. [DOI] [PubMed] [Google Scholar]
- 9.Dougherty CM, Burr RL, Kudenchuk PJ, Glenny RW. Aerobic exercise effects on quality of life and psychological distress after an implantable cardioverter defibrillator. J Cardiopulm Rehabil Prev. 2020;40(2):94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinhaus DA, Lubitz SA, Noseworthy PA, Kramer DB. Exercise interventions in patients with implantable cardioverter-defibrillators and cardiac resynchronization therapy. J Cardiopulm Rehabil Prev. 2019;39(5):308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puppala VK, Hofeld BC, Anger A, et al. Pacemaker detected active minutes are superior to pedometer-based step counts in measuring the response to physical activity counseling in sedentary older adults. BMC Geriatr. 2020;20(1):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kramer DB, Tsai T, Natarajan P, et al. Frailty, physical activity, and mobility in patients with cardiac implantable electrical devices. J Am Heart Assoc. 2017;6(2):e004659. doi:10.1161/JAHA.116.004659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Cardiopulm Rehabil Prev. 2019;39(4):208–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berry R, Brawner CA, Kipa SG, Stevens C, Bloom C, Keteyian SJ. Telemedicine home-based cardiac rehabilitation: a case series. J Cardiopulm Rehabil Prev. 2020;40(4):245–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeo TJ, Wang YL, Low TT. Have a heart during the COVID-19 crisis: making the case for cardiac rehabilitation in the face of an ongoing pandemic. Eur J Prev Cardiol. 2020;27(9):903–905. [DOI] [PMC free article] [PubMed] [Google Scholar]