Abstract
Lateral epicondylitis (LE) is a degenerative disease of the tendons, spurred by repetitive microtrauma leading to an attempt by the body to heal by upregulating local angiogenesis and fibroblast proliferation. Prolotherapy (PT) is the injection of dextrose around the injured tissues to stimulate their spontaneous regeneration. Herein, we have described a case of lateral epicondylitis, diagnosed with clinical and ultrasound (US) examination, where local steroid injections provided relief only for a limited time. We treated the patient with US-guided PT, following which the pain disappeared and the tendon was restored.
Keywords: Dextrose, epicondylitis, injection, prolotherapy, regenerative medicine
Introduction
Prolotherapy (PT) has been widely used since it was first performed by Hackett (1) in 1958 with the purpose of stimulating the production of new bone and soft tissue cells. It consists of the injection of dextrose around the affected sites such as tendons, joints, ligaments, and layers (2).
Before the ultrasound (US) era, the injections were performed following the anatomical landmarks and palpation with variable results, whereas the procedures performed with sonographic guidance have allowed a more accurate delivery of the solution to the desired site (2).
Lateral epicondylitis (LE) is a common source of elbow pain, which is associated with repeated and forceful activity; in degenerative tendinopathy, LE consists of the extensor origin of the forearm, most commonly the extensor carpi radialis brevis (ECRB), with the presence of degenerative changes including neovascularity and disorganised collagen fibres or tendon tears (3, 4).
PT, similar to the other local treatments such as corticosteroid, hyaluronic acid, and platelet rich plasma injections, has been used to treat LE; however, thus far, a clear algorithm or flow chart to favour one treatment over another for different patients is not available (3, 4).
Case Presentation
A 70-year-old woman with normal body mass index (BMI) and no relevant medical history presented to our hospital complaining of right LE with a numerical rating score (NRS) of 5, lasting for 10 months. Treatment from her general practitioner comprised ibuprofen, 600 mg twice a day per os for 14 days, and transcutaneous electrical nerve stimulation (TENS) with a transient reduction of pain. Subsequently, she was submitted to 3 local corticosteroid injections, once per week for 3 consecutive weeks. The pain disappeared for 15 days after the last injection, and then recurred (NRS=5). We selected US-guided prolotherapy with 2 mL of 16.5% dextrose. The US scan was performed with a linear transducer 13–6 MHz Mylab One (Esaote, Genova, Italy) and we used an in-plane approach to inject distally to the bone insertion site in the forearm direction, above and below the insertion of the ECRB component of the common extensor tendon (Figure 1). Before the injections, the maximal thickness of ECRB at the proximal insertion was 5 mm compared to 4 mm of the unaffected arm, and the colour Doppler US examination showed a mild vascularization (severity was classified as follows: 0=No vascularization, 1=Mild, 2=Moderate, and 3=Severe), according to Hoksrud et al. (5).
Figure 1.
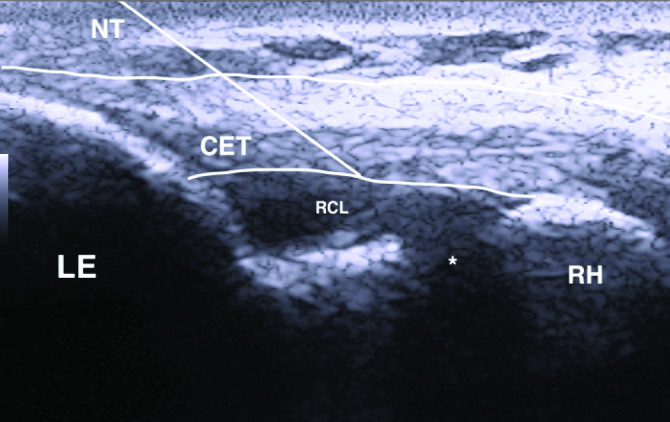
The needle trajectory (NT) in the forearm direction used to deliver the drug above CET and between CET and RCL is shown
*joint space. LE: lateral epicondyle; CET: common extensor tendon; RCL: radial collateral ligament; RH: radial head
We repeated the injection at 15 days interval for two more times; non-steroidal anti-inflammatory drugs (NSAIDs) were forbidden during the treatment period.
The pain intensity decreased slowly and constantly during the following weeks, and after the 3rd injection, it disappeared. The patient was pain free even after 6 months. The US exam showed no vascularization and the maximal thickness of ECRB at the proximal insertion decreased to 4.2 mm. We obtained consent from the patients for the procedure and publication.
Discussion
Regenerative medicine aims to restore and regenerate the injured or diseased tissues and not just reduce the pain and inflammation, as NSAIDs or corticosteroid injections would do.
Local injections of hyaluronic acid, dextrose, whole blood, platelet rich plasma, and other cell based medical devices are being used for the treatment of LE, and can be considered a better option when compared to the conventional corticosteroid injections, with fewer side effects (3, 4).
Conclusion
Prolotherapy is the cheapest option when planning a regenerative medicine treatment for LE, and our experience support its use as the next therapeutic step when conventional treatments fail.
Main Points.
Lateral epicondylitis is a degenerative disease of the tendons.
Prolotherapy is the injection of dextrose around the injured tissues to stimulate their spontaneous regeneration.
A case of lateral epicondylitis is reported wherein the pain disappeared and the tendon was restored upon treatment with US-guided prolotherapy.
Footnotes
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – E.P., G.B.; Design – E.P.; Supervision – E.P., G.B.; Resources – E.P.; Materials – G.B.; Data Collection and/or Processing – E.P.; Analysis and/or Interpretation – E.P., G.B.; Literature Search – G.B.; Writing Manuscript – E.P.; Critical Review – G.B.; Other – E.P., G.B.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Hackett GS. Ligament and tendon relaxation treated by prolotherapy. 3rd edition. Springfield (IL): Charles C Thomas; 1958. [Google Scholar]
- 2.Hauser RA, Lackner JB, Steilen-Matias D, Harris DK. A Systematic Review of Dextrose Prolotherapy for Chronic Musculoskeletal Pain. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:139–59. doi: 10.4137/CMAMD.S39160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabago D, Best TM, Zgierska AE, Zeisig E, Ryan M, Crane D. A systematic review of four injection thera-pies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med. 2009;43:471–81. doi: 10.1136/bjsm.2008.052761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sims SE, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand. 2014;9:419–46. doi: 10.1007/s11552-014-9642-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoksrud A, Ohberg L, Alfredson H, Bahr R. Color Doppler ultrasound findings in patellar tendinopathy (jumper’s knee) Am J Sports Med. 2008;36:1813–20. doi: 10.1177/036354650831989. [DOI] [PubMed] [Google Scholar]


