Abstract
Objective
Catheter-related bladder discomfort (CRBD) that manifests as agitation and bladder hyperactivity is a common problem in young male patients. Local anaesthetics are typically recommended for this problem. Hence, this study was conducted to determine the effect of intravesical diluted bupivacaine on CRBD in young male patients during postanaesthetic recovery.
Methods
This double-blinded randomised clinical trial included 68 consecutive patients, aged 20–60 years, who underwent urinary catheterisation during surgery and anaesthesia at a university hospital during 2017–2018. Patients were randomly assigned to receive either 50 ml of intravesical diluted (0.2%) bupivacaine (n=37) or normal saline (n=31). The incidence and severity of CRBD were then evaluated in PACU and compared between the two groups.
Results
In this study, 16.2% of patients in the bupivacaine group and 83.9% in the saline group had discomfort at arrival in the recovery room, exhibiting a significant intergroup difference (p=0.0001). Moreover, after 15–20 min, the incidence of CRBD was 16.2% and 90.3% in the bupivacaine and normal saline groups, respectively, which again demonstrated a significant statistical difference (p=0.0001). In addition, the severity of CRBD was lower in the bupivacaine group, during both periods (p=0.005). The saline group reported significantly higher use of pethidine and midazolam (p=0.005).
Conclusion
It may be concluded that intravesical diluted bupivacaine can significantly decrease the incidence and severity of CRBD in young male patients during recovery from anaesthesia. Therefore, the use of this method is highly recommended.
Keywords: Bupivacaine, male, urinary bladder, urinary catheters
Introduction
Urinary catheterisation is commonly performed during various surgeries to control urine output during and after surgery. However, it can cause some severe somatic and mental complications (1–3). The pain and discomfort associated with urethral catheterisation are known as catheter-related bladder discomfort (CRBD) and is the most common cause of agitation during the postoperative phase, especially in young male patients (4). The reported rate of CRBD ranges from 47% to 90% (5). Notably, the contributing factors in this era include male sex, open surgeries, previous urinary catheterisation, and age below 50 years (6–8). Patients experience symptoms akin to overactive bladder, suprapubic pain, urgency, dysuria, incontinence, and agitation because of involuntary contraction of the detrusor muscle (2, 4). CRBD can increase postoperative complications, such as wound dehiscence, bleeding, hemodynamic instability, arrhythmia, and aggravated cardiovascular status leading to prolonged PACU and hospital stay (5, 7). Muscarinic receptors are primarily responsible for the contraction of the detrusor muscle (7), with prostaglandin secretion being another contributing pathway (9). Different preventive and therapeutic modalities including gabapentin (10, 11), tramadol (12), anti-muscarinic agents (13–15), ketamine (16, 17), prostaglandin synthesis blockers (18), alpha-2 agonists (19), and different neural block methods (20–24) have been proposed for treating CRBD. However, these methods provide only partial improvement and not complete resolution. Notably, reduction in pain and discomfort would increase the satisfaction rate among patients and improve their mental status (5, 7). Therefore, local anaesthetics are considered ideal in reducing the CRBD rate and burden by blocking the sensory receptors in the bladder.
Several previous studies have assessed the role of intravesical application of local anaesthetics, such as bupivacaine, in the prevention, diagnosis, and treatment of bladder problems like detrusor muscle hyperreflexia (25, 26), with favourable results. The similarity of CRBD symptoms with that of the aforementioned pathologies led to the hypothesis that intravesical bupivacaine could prevent CRBD incidence as a primary outcome.
Accordingly, this study aimed to compare the effect of intravesical application of diluted bupivacaine with that of the control group (normal saline).
Methods
This randomised, double-blind clinical trial enrolled 68 consecutive patients with ASA physical status I or II and age ranging from 20 to 60 years who were undergoing orthopaedic and cervical spine surgeries in a teaching hospital. Exclusion criteria were patients’ refusal to participate in the study, as well as a history of renal disease, prostatic hyperplasia, overactive bladder, cardiac diseases, central nervous system disorders, morbid obesity, substance use, corticosteroid therapy, and trauma during catheterization. The study was approved by the research ethics committee of the university (reference number: IR.IUMS.FMD.REC.1396.24713-103614) and registered in the Iranian registry of clinical trial (IRCT) (registration code: IRCT2014090111398N6, date: 23/09/2014]. In addition, the study was performed in accordant with the Helsinki Declaration. Informed consent was obtained from the patients after explaining the study protocol in detail. Subsequently, patients were randomly assigned to the following two study groups: normal saline (group S) and bupivacaine (group B). The anaesthesia protocol was identical across the groups, including monitoring (ECG, NIBP, ETCO2, O/I, POM), preoxygenation, and premedication with fentanyl (2 μg kg−1) and midazolam (15 μg kg−1). Anaesthesia was induced using propofol 1.5–2 mg kg−1 and atracurium (0.5 mg kg−1). Tracheal intubation was performed using PVC tube number 8, and then mechanical ventilation was conducted with the same characteristics. The anaesthesia maintenance regimen was executed using propofol 100 to 150 μg kg−1 (with haemodynamic and anaesthesia depth control) and atracurium 0.2 mg kg−1 each 30 min. Morphine 0.1 mg kg−1 was administered initially for all patients, and if required, fentanyl 50 μg was repeated during surgery. After anaesthesia induction, patients underwent urinary catheterisation with number 16 Telefax (made in Malaysia) and lidocaine 2% gel as a lubricant; the catheter balloon was filled with 10 ml still water. Catheterisation was performed without traumatisation by an expert blinded to subjects. Approximately 15 min before termination of the surgery, 50 mL of normal saline (group S) or bupivacaine 0.2% (group B) was injected in the bladder by using a sterile gavage syringe via Foley catheter in the control and intervention groups, respectively. The catheter was then clamped for 30 min. The CRBD incidence and severity were evaluated according to the standard scoring system (Table 1) at the following two timepoints: 1) upon arrival in PACU and 2) after 15–20 minutes (13, 27). Patients who were graded to be in moderate and severe discomfort received meperidine 25 mg and midazolam 1 mg intravenously, and in cases with continued agitation, the catheter was removed.
Table 1.
CRBD severity grading system
| Patient did not complain of any CRBD even on inquiring; | None |
| Reported by patients only on questioning; | Mild |
| Reported by the patients on their own (without questioning and not accompanied by any behavioural responses | Moderate |
| Reported by patients on their own along with behavioural responses. | Severe |
CRBD: catheter-related bladder discomfort
Sample size and statistical analysis
The evaluation of CRBD incidence was the primary outcome of this study. Based on the literature review, the incidence of CRBD was reported to be 30%–85% (mean 57.5%) (4–8). Power analysis was performed using an online calculator, made available by the University of British Columbia (Vancouver, BC, Canada), by assuming alpha at 0.05 with a power of 90% to detect differences in the incidence of CRBD in a range of 0.3–0.7 between the two groups. The calculated minimum sample size in each group was 28 subjects. Overall, 68 patients were ultimately included in the study, considering a 20% dropout rate. The data were analysed using IBM Statistical Package for the Social Sciences version 19.0 (IBM SPSS Corp.; Armonk, NY, USA), and p<0.05 was considered significant. Categorical data were presented as the frequency with percentage and were analysed using the chi-square test. Numerical variables were presented as mean ± standard deviation for normally distributed data and were compared using t-test analysis. The severity of CRBD (secondary outcome) was comparatively analysed between the two groups by using Fisher’s exact test.
Results
This study definitively analysed 68 patients (31 patients in the saline group and 37 in the bupivacaine group). The mean age, weight, duration of operation, volume of intraoperative fluid intake, and urinary output were matched across the groups (Table 2). Lower extremity was the most common surgical site, performed in 51.6% and 40.5% patients of the control and intervention groups, respectively (p>0.05). Furthermore, regarding patients’ ASA physical status, 71% of cases in the saline group, and 75.7% in the intervention group were class I (p>0.05). Furosemide was administered in 6.5% and 8.1% of cases in the control and intervention groups, respectively (p>0.05).
Table 2.
Means and comparison of background variables across two groups
| Group | Group | Mean | SD | p |
|---|---|---|---|---|
|
| ||||
| Age (years) | S | 37.94 | 10.36 | 0.956 |
| B | 37.78 | 11.95 | ||
| Weight (kg) | S | 81.39 | 11.27 | 0.965 |
| B | 81.51 | 12.24 | ||
| Duration of operation (h) | S | 3.10 | 0.972 | 0.640 |
| B | 3.20 | 0.759 | ||
| Fluid Volume (L) | S | 2.35 | 0.68 | 0.310 |
| B | 2.54 | 0.75 | ||
| Urine Output (mL) | S | 431.61 | 198.53 | 0.460 |
| B | 473.51 | 255.95 | ||
SD: standard deviation
Immediately after the patients’ entry into the recovery, the incidence of CRBD was reported as 83.87% and 16.22% in the normal saline and bupivacaine groups, respectively. After 15–20 minutes of entry into recovery, the CRBD incidence was reported as 91.32% and 16.22% in the saline and bupivacaine groups, respectively. A statistically significant intergroup difference was observed (p=0.0001). The severity of CRBD in the two groups after clamp removal is illustrated in Figure 1. As demonstrated in Figure 1, a milder form of CRBD symptoms was reported in 16.22% of patients of the group (B). By contrast, 41.94% of patients belonging to the group (S) exhibited medium or severe CRBD symptoms. The difference was statistically significant (p=0.0001). CRBD severity after 15–20 minutes is demonstrated in Figure 2. At both time points, a significant intergroup difference was observed (p=0.0001).
Figure 1.
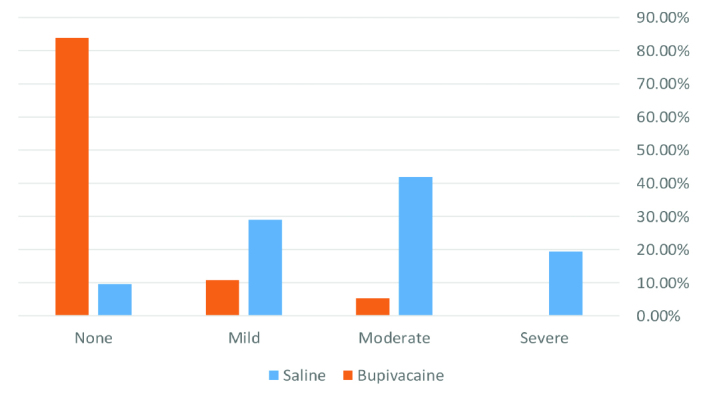
Incidence and severity of CRBD immediately after clamp release in the groups
CRBD: catheter-related bladder discomfort
Figure 2.
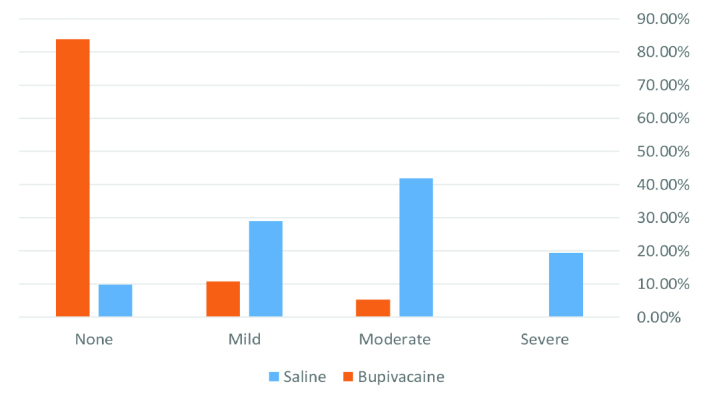
Incidence and severity of CRBD 15–20 min after clamp release in the groups
CRBD: catheter-related bladder discomfort
The mean dosage of meperidine was 17.9±12.4 mg in the group (S), and 7.9±11.8 mg in the group (B) with significant difference (p=0.001). Moreover, midazolam was not administered in the bupivacaine group, but in six cases of the control group (S) at a mean dose of 0.19±0.4 mg (p=0.005).
Discussion
The results of the present study demonstrated that compared with normal saline injection, a 50 ml injection of diluted (0.2%) bupivacaine into the bladder during the final stage of surgery prevented the incidence of CRBD to a large extent and reduced the intensity of bladder pain and discomfort caused by urinary catheterisation, thereby causing a 67.7% decrease (16.2% vs. 83.9%) in CRBD incidence in young and middle-aged male patients upon regaining consciousness. This modality is more effective than the use of sedatives and systemic analgesics, as noted in other studies (10–19), to decrease the incidence and intensity of the unrest at the time of emergence. Approximately 15 to 20 min after clamp removal, when patients were fully conscious and oriented, only 16.2% of patients in the bupivacaine group reported mild to median intensity CRBD. In contrast, this proportion rose to 90.3% in the saline (placebo) group, exhibiting significant statistical difference (p=0.0001). Notably, no case of severe unrest and agitation was reported in the bupivacaine group.
Furthermore, another significant finding of the study is the substantial decrease of sedative (midazolam) and analgesic (meperidine) use in the bupivacaine group compared with the saline group, which further corroborates the positive effect of intravesical bupivacaine on pain and agitation.
CRBD is one of the most common problems in surgeries involving male patients, which may cause severe unrest and agitation during emergence and postanaesthetic recovery, reported in 30% to 85% of male patients who underwent urinary catheterisation (4–8). Several treatment techniques and medications have been used to prevent and resolve this problem, with all being relatively effective, albeit not completely successful. Various studies have examined methods, such as caudal neural block (20, 21), pudendal nerve block (24), dorsal penile nerve block (22), systemic ketamine prescription (16, 17), prostaglandin inhibitors (18), dexmedetomidine (19), and muscarinic receptor inhibitors (13–15). A recent meta-analysis study (2019) undertaken by Hur et al. (28) that was published in the Journal of Anaesthesia compared the effectiveness of these methods and reported Gabapentin to be the most effective in reducing CRBD incidence generally and Tolterodine in lowering its intensity. However, it is impossible to draw a precise conclusion because the studies had relatively small sample sizes and heterogenic designs.
After carefully searching various sources, to the best of our knowledge, no controlled study has been conducted regarding local anaesthetic application using intravesical methods to prevent CRBD. However, the application of topical anaesthetics, in the form of gels or ointments, to the urethra has been reported to have positive effects by Mu et al. (23). Therefore, the present study is unique in this regard. Moreover, this study differs from similar studies based on the fact that most studies primarily enrolled patients who underwent various urologic surgeries, whereas such patients were excluded from this study to avoid interference from factors like cystic inflammation because of surgery and to examine the net effect of catheterisation.
Demographic variables, such as patients’ age and weight of the two study groups, are compared in Table 1, along with the comparison of surgery types and duration and ASA classes, accounting for homogeneity and stochastic selection of patients in the two groups. Thus, interfering factors were eliminated to a large extent.
As discussed earlier, because of the absence of studies that used this method, comparison of this study with other studies is challenging. In a study conducted by Mu et al. (23) in China, 146 young male patients who underwent urinary catheterisation for surgery were divided into two groups of topical prilocaine and lidocaine combination recipients and lidocaine gel recipients, and CRBD was observed to be significantly lower in the mixed anaesthetic group, which is concordant with our findings related to the acceptable functionality of topical anaesthetics.
A study conducted by Li et al. (22) in 2016, coextensively with the present study’s results, examined 48 young male patients, aged between 18 and 60 years, placed into two groups of dorsal penile nerve block with ropivacaine and intravenous Tramadol recipients, and observed that CRBD intensity at various times after the surgery was significantly lower in the dorsal penile nerve block group, besides lower incidence of conditions like nausea, vomiting, and dry mouth.
Prajapati et al. (20) conducted a study in 2018 on 99 patients who underwent PCNL surgery and were placed into three groups that received caudal block using bupivacaine alone, bupivacaine plus Fentanyl, and bupivacaine plus Nalbuphine, respectively, to control CRBD. The results revealed that CRBD was significantly lower in the two groups that received a mixed anaesthetic regimen. In another study conducted by Li and Liao (24) in 2016, the bilateral pudendal block was observed to decrease both the incidence and intensity of CRBD in patients (63% vs. 84%). Nonetheless, we should note that despite the statistically significant difference, it is less effective compared with the present study. In conclusion, the results of the present study, as well as previous studies have revealed that topical anaesthetic use is more effective than other methods like systemic drug prescriptions in preventing and decreasing the intensity of CRBD-a highly unpleasant condition. Notably, intravesical injection of diluted bupivacaine is one of the most effective methods among these interventions.
Study limitations
One of the limitations of the present study is the short reporting and registration times of the primary outcome of the study. It would have been advisable to monitor the outcome at multiple time points during the later stages of recovery. The other limitation is related to the difficulty of CRBD intensity examination using the scale used for the study, as some patients were not sufficiently conscious (immediately after clamp removal) to report with accuracy. Therefore, it is encouraged to undertake studies with larger sample size, more frequent patient monitoring (especially in later stages), and the use of other local anaesthetics like ropivacaine or combinations with adjutant drugs, and to compare them with other existing treatment methods.
Conclusion
In general, based on the results of the present study, it can be concluded that injection of diluted bupivacaine (0.2%) into the bladder and clamping the catheter for 30 minutes to prevent the solution from being discharged is highly effective in decreasing the incidence and intensity of CRBD during post anaesthetic recovery of young and middle-aged male patients. Therefore, the application of this treatment modality is strongly recommended to treat CRBD and improve the recovery quality of young male patients’ after urinary catheterisation.
Main Points
“CRBD” is a very common problem in young males.
It is the most common cause of emergence agitation.
Previous efforts result in partial improvement and not complete resolution.
Intravesical diluted bupivacaine can significantly decrease the incidence and severity of CRBD.
Acknowledgements
We warmly thank all who helped conduct this study. In addition, we express our gratitude towards Dr. Ali Tajik for providing statistical assistance.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Iran University of Medical Sciences (reference number: IR.IUMS.FMD.REC.1396.24713-103614).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – M.R.G., A.P.; Design – M.R.G., S.S., M.G.; Supervision – A.P., M.R.G.; Resources – F.R., A.K.; Materials – F.R., A.K.; Data Collection and/or Processing – S.S., S.T., M.G.; Analysis and/or Interpretation – M.R.G., A.P., F.R.; Literature Search – S.S., S.T., M.G., A.K.; Writing Manuscript – S.S., M.R.G., A.P.; Critical Review – A.P., M.R.G., A.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Feneley RC, Hopley IB, Wells PN. Urinary catheters: history, current status, adverse events and research agenda. J Med Eng Technol. 2015;39:459–70. doi: 10.3109/03091902.2015.1085600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah J. Catheterisation. Ann R Coll Surg Engl. 2012;94:5–7. doi: 10.1308/003588412X13171221500303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawrence EL, Turner IG. Materials for urinary catheters: a review of their history and development in the UK. Med Eng Phys. 2005;27:443–53. doi: 10.1016/j.medengphy.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010;57:843–8. doi: 10.1007/s12630-010-9338-9. [DOI] [PubMed] [Google Scholar]
- 5.Bai Y, Wang X, Li X, Pu C, Yuan H, Tang Y, et al. Management of Catheter-Related Bladder Discomfort in Patients Who Underwent Elective Surgery. J Endourol. 2015;29:640–9. doi: 10.1089/end.2014.0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li C, Liu Z, Yang F. Predictors of catheter-related bladder discomfort after urological surgery. J Huazhong Univ Sci Technolog Med Sci. 2014;34:559–62. doi: 10.1007/s11596-014-1315-z. [DOI] [PubMed] [Google Scholar]
- 7.Binhas M, Motamed C, Hawajri N, Yiou R, Marty J. Predictors of catheter-related bladder discomfort in the post-anaesthesia care unit. Ann Fr Anesth Reanim. 2011;30:122–5. doi: 10.1016/j.annfar.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Lim N, Yoon H. Factors Predicting Catheter-Related Bladder Discomfort in Surgical Patients. J Perianesth Nurs. 2017;32:400–8. doi: 10.1016/j.jopan.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Antunes-Lopes T, Carvalho-Barros S, Cruz CD, Cruz F, Martins-Silva C. Biomarkers in overactive bladder: a new objective and noninvasive tool? Adv Urol. 2011;2011 doi: 10.1155/2011/382431. 382431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodarzi D, Cyrus A, Aghamohammadi J, Sadeghi B. Efficacy of Gabapentin for Prevention of Postoperative Catheter-related Bladder Discomfort in Patients Undergoing open prostatectomy. J Iran Clin Res. 2015;1:67–74. [Google Scholar]
- 11.Bala I, Bharti N, Chaubey VK, Mandal AK. Efficacy of gabapentin for prevention of postoperative catheter-related bladder discomfort in patients undergoing transurethral resection of bladder tumor. Urology. 2012;79:853–7. doi: 10.1016/j.urology.2011.11.050. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal A, Yadav G, Gupta D, Singh PK, Singh U. Evaluation of intra-operative tramadol for prevention of catheter-related bladder discomfort: A prospective, randomized, double-blind study. Br J Anaesth. 2008;101:506–10. doi: 10.1093/bja/aen217. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal A, Dhiraaj S, Singhal V, Kapoor R, Tandon M. Comparison of efficacy of Oxybutynin and Tolterodine for prevention of catheter related bladder discomfort: a prospective randomized, placebo-controlled, double-blind study. Br J Anaesth. 2006;96:377–80. doi: 10.1093/bja/ael003. [DOI] [PubMed] [Google Scholar]
- 14.Srivastava VK, Nigam R, Agrawal S, Kumar S, Rambadh S, Kanaskar J. Evaluation of the efficacy of solifenacin and darifenacin for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Minerva Anestesiol. 2016;82:867–73. [PubMed] [Google Scholar]
- 15.Nam K, Seo JH, Ryu JH, Oh AY, Lee T, Park HP, et al. Randomized, clinical trial on the preventive effects of butyl-scopolamine on early postoperative catheter-related bladder discomfort. Surgery. 2015;157:396–401. doi: 10.1016/j.surg.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 16.Shariat Moharari R, Lajevardi M, Khajavi M, Najafi A, Shariat Moharari G, Etezadi F. Effects of intra-operative ketamine administration on postoperative catheter-related bladder discomfort: a double-blind clinical trial. Pain Pract. 2014;14:146–50. doi: 10.1111/papr.12055. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal A, Gupta D, Kumar M, Dhiraaj S, Tandon M, Singh PK. Ketamine for treatment of catheter related bladder discomfort: a prospective, randomized, placebo controlled and double blind study. Br J Anaesth. 2006;96:587–9. doi: 10.1093/bja/ael003. [DOI] [PubMed] [Google Scholar]
- 18.Ergenoglu P, Akin S, Yalcin Cok O, Eker E, Kuzgunbay B, Turunc T, et al. Effect of intraoperative paracetamol on catheter-related bladder discomfort: A prospective randomized, double-blind study. Curr Ther Res Clin Exp. 2012;73:186–94. doi: 10.1016/j.curtheres.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim HC, Lee YH, Jeon YT, Hwang JW, Lim YJ, Park JE, et al. The effect of intraoperative dexmedetomidine on postoperative catheter-related bladder discomfort in patients undergoing transurethral bladder tumor resection: A double-blind randomized study. Eur J Anaesthesiol. 2015;32:596–601. doi: 10.1097/EJA.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 20.Prajapati D, Patel M, Patel P, Mistry D. Effect of caudal bupivacaine alone and with adjuvant fentanyl and nalbuphine to minimize the catheter-related bladder discomfort after tubeless percutaneous nephrolithotomy: A prospective randomized study. World Congress on regional anesthesia and pain medicine; United States. 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsuchiya M, Kyoh Y, Mizutani K, Yamashita J, Hamada T. Ultrasound-guided single shot caudal block anesthesia reduces postoperative urinary catheter-induced discomfort. Minerva Anestesiologica. 2013;79:1381–8. [PubMed] [Google Scholar]
- 22.Li JY, Yi ML, Liao R. Dorsal Penile Nerve Block With Ropivacaine-Reduced Postoperative Catheter-Related Bladder Discomfort in Male Patients After Emergence of General Anesthesia: A Prospective, Randomized, Controlled Study. Medicine (Baltimore) 2016;95:e3409. doi: 10.1097/MD.0000000000003409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mu L, Geng LC, Xu H, Luo M, Geng JM, Li L. Lidocaine-prilocaine cream reduces catheter-related bladder discomfort in male patients during the general anesthesia recovery period: A prospective, randomized, case-control STROBE study. Medicine (Baltimore) 2017;96:e6494. doi: 10.1097/MD.0000000000006494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Jing-yi, Liao Ren. Prevention of catheter-related bladder discomfort - pudendal nerve block with ropivacaine versus intravenous tramadol: study protocol for a randomized controlled trial. Trials. 2016;17:448. doi: 10.1186/s13063-016-1575-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McInerney PD, Grant A, Chawla J, Stephenson TP. The effect of intravesical Marcaine instillation on hyperreflexic detrusor contractions. Paraplegia. 1992;30:127–30. doi: 10.1038/sc.1992.40. [DOI] [PubMed] [Google Scholar]
- 26.Moldwin R. North Shore Long Island Jewish Health Sytem Smith Institute For Urology Standard/Policy/Procedure. Guidelines for Intravesical Drug Instillation. 2009. https://www.painfulbladder.org/pdf/guidelinesforintravesicaldruginstillation_smithinstitute.pdf.
- 27.Srivastava VK, Agrawal S, Kadiyala VN, Ahmed M, Sharma S, Kumar R. The efficacy of pregabalin for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled double-blind study. J Anesth. 2015;29:212–6. doi: 10.1007/s00540-014-1911-x. [DOI] [PubMed] [Google Scholar]
- 28.Hur M, Park SK, Yoon HK, Yoo S, Lee HC, Kim WH, et al. Comparative effectiveness of interventions for managing postoperative catheter-related bladder discomfort: a systematic review and network meta-analysis. J Anesth. 2019;33:197–208. doi: 10.1007/s00540-018-2597-2. [DOI] [PubMed] [Google Scholar]


