Abstract
Objective
To determine whether neighborhood socioeconomic disadvantage, as determined by area deprivation index (ADI), increases 30-day hospital re-observation risk.
Patients and Methods
This retrospective study of 20% Medicare fee-for service beneficiary observation stays from January 1, 2014 to November 30, 2014 included 319,980 stays among 273,308 beneficiaries. We evaluated risk of a 30-day re-observation following an index observation stay for those living in the 15% most compared to the 85% least disadvantaged neighborhoods.
Results
Overall, 4.4% of beneficiaries had index observation stays, which varied by disadvantage (4.3% least; 5.6% most). Patients in the most disadvantaged neighborhoods had higher 30-day re-observation rate (6.8%) compared to least disadvantaged neighborhoods (4.9%) – a 43% increased risk (unadjusted OR 1.43 [1.31–1.55]). After adjustment, this risk remained (1.13 [1.04–1.22]). Discharge to skilled nursing facility reduced 30-day re-observation risk (OR=0.63), while index observation length of stay of four or more days (three midnights) conferred increased risk (OR=1.29); those living in disadvantaged neighborhoods were less likely to discharge to skilled nursing facilities and more likely to have long index stays. Beneficiaries with more than one 30-day re-observation (‘chronic re-observation’) had progressively greater disadvantage by number of stays (adjusted IRR=1.08 [1.02–1.14]). Observation prevalence varied nationally.
Conclusion
Thirty-day re-observation, especially ‘chronic re-observation’, is highly associated with socioeconomic neighborhood disadvantage, even after accounting for factors such as race, disability, and Medicaid eligibility. Beneficiaries least able to pay are potentially most vulnerable to costs from serial re-observations and challenges of Medicare observation policy, which may discourage patients from seeking necessary care.
Introduction
Observation hospitalizations (observation stays) are increasingly common, in contrast to inpatient admissions, in the Medicare program.1 Initially conceived as a billing mechanism for care in short-stay observation units, observation is now commonly encountered on general medical hospital wards.2,3,4 As a result, outpatient services, which include all observation stays, have increased by 43.5% over the last decade, while inpatient admissions have decreased 20.4% over the same time period.5
The designation of observation versus inpatient may hold financial consequences for Medicare beneficiaries because the Medicare billing structure for observation stays is significantly different than for inpatient admissions. Patients hospitalized as inpatients are covered by Medicare Part A and pay a one-time deductible per 60-day benefit period, and Medicare pays for post-hospitalization skilled nursing facility (SNF) coverage following a 3 consecutive inpatient midnight stay.4 Patients hospitalized “under observation” are covered by Medicare Part B and may pay more or less than the inpatient deductible for an individual observation stay because there is no out-of-pocket limit for an individual observation stay. Nor is there a benefit period; thus, patients with frequent observation hospitalizations may bear increased financial risk. Kangovi and colleagues determined that beneficiaries with more than one observation stay in 60 days incurred more than twice the financial out-of-pocket cost compared to those with a single observation stay, with some sustaining out-of-pocket costs three times the Part A inpatient deductible.6 Although the recent Centers for Medicare & Medicaid Services (CMS) Comprehensive Ambulatory Payment Classification (C-APC) 8011 caps financial liability for some individual observation stays, not all observation stays meet C-APC criteria7 and patients may still face cumulative costs from serial C-APC and non-C-APC covered observation stays in excess of the inpatient deductible. Equally important, hospital nights spent under observation, whether billed under C-APC 8011 or otherwise, do not count towards Medicare’s three-midnight requirement for SNF coverage.
It is possible that Medicare’s observation hospitalization policy may disproportionately impact those from marginalized and socioeconomically disadvantaged neighborhoods. While some evidence suggests that African American/Black patients have higher rates of observation stays as compared to Non-Hispanic Whites,8,9 the role of other factors, such as social determinants, have not yet been well studied. Research using the Area Deprivation Index (ADI),10 a validated measure of neighborhood disadvantage, a social determinant of health, demonstrated higher risk of 30-day inpatient readmissions for those living in the 15% most disadvantaged neighborhoods compared to those living in the least disadvantaged neighborhoods.11 It is plausible that a similar phenomenon exists for observation hospitalizations, as these visits may serve as a ‘safety net’ for patients who present to the emergency department (ED) or elsewhere for care and would otherwise discharge home except for lack of fundamental social determinants of health (e.g., housing, transportation), or uncertain access to ambulatory care, medications, and other necessary health care resources. This raises the possibility that those least able to afford unexpected medical costs from serial observation hospitalizations or subsequent uncovered SNF stays are the ones most likely to bear these expenses under Medicare’s current observation policy, which in turn may discourage these patients from seeking needed health care.
We sought to determine the relationship of neighborhood disadvantage and 30-day re-observation. Although there is currently no CMS policy regarding re-observation measurements, we sought to maximize equivalency and relevance to existing policy by studying repeat observation stays within 30 days of an index observation stay to parallel 30-day admission metrics of care quality.
Participants and Methods
Data source and Design
We conducted a national analysis of 2013–2014 Medicare Part A and B national claims data using the nationally representative Medicare 20% random fee-for service beneficiary sample. All qualifying observation stays between January 1, 2014 and November 30, 2014 were evaluated for subsequent 30-day re-observation risk with 2013 serving as the comorbidity baseline year. The term ‘observation stay’ is used to describe index observation encounters and observation events in general, and ‘re-observation’ indicates any observation stay within 30-days of an index observation stay. Observation stays were identified using the comprehensive previously described University of Wisconsin Method.12 Briefly, this includes claims with at least one observation revenue center code including 0760, 0761, 0762, or 0769 appearing in the outpatient revenue center and having no association with an inpatient claim, in addition to inpatient-to-observation ‘status-change’ claims that had some association with an inpatient claim but with observation codes in the outpatient revenue center on or after the discharge date. A review of the observation stays exclusively identified by revenue center code 0761 revealed these stays rarely originated from the emergency department and had a high seven-day cyclical repeat encounter rate indicative of prescheduled planned care. These stays were thus excluded from the final analysis cohort to ensure the most conservative definition of an observation stay. For a list of the full study exclusions see the Supplemental Figure. The final cohort included 319,980 observation stays involving 273,308 unique beneficiaries. The University of Wisconsin Institutional Review Board approved this study.
Variables
30-day re-observation
We evaluated all-cause re-observation within 30 days of an index observation stay measured from the day of discharge. Qualifying eligibility criteria for the 30-day re-observation measure were aligned with CMS’s existing 30-day inpatient re-hospitalization measure, which does not take into account the competing risk of death within 30 days. Eligible index observation stays were those in which beneficiaries had continuous Medicare part A and B enrollment in the one month post index stay, no death during the index observation stay, and were not discharged against medical advice.13 Chronic re-observation was defined as more than one re-observation within 30 days of an index observation stay.
Neighborhood Disadvantage
Neighborhood disadvantage was measured by the ADI, a validated composite ranked index containing 17 census block group (i.e. “neighborhood-level”) social determinants of health factors encompassing housing, income, employment, transportation and education as captured in the American Community Survey.14 Beneficiary nine-digit zip code were geolinked to their ADI neighborhood ranking matched to the time-period of study.15 ADI rankings range from 1–100 with higher values indicating the most disadvantaged neighborhoods. All ADI scores are freely available through the Neighborhood Atlas (https://www.neighborhoodatlas.medicine.wisc.edu/).15 Using a published threshold definition, the cohort was split into two groupings on the basis of neighborhood disadvantage: patients living in the top 15% most disadvantaged neighborhoods and those living in the bottom 85% least disadvantaged neighborhoods.11
Other covariates
Patient and hospital level covariates were added to isolate the effect of neighborhood disadvantage on 30-day re-observation. They include: comorbidity/illness burden in the 12 months prior (Elixhauser comorbidities, hierarchical condition category score, reason for initial Medicare enrollment/disability), index observation stay factors (indicator for stays originating in ED, length of stay, discharge to SNF), sociodemographic patient factors (age, sex, race, dual Medicare/Medicaid eligibility status, and rurality), and hospital characteristics (discharge volume, teaching/academic affiliation, and for-profit status). Observation length of stay was determined by number of consecutive days of observation revenue center codes. For example, a stay with codes on two consecutive days would be assigned a length of stay of two days. Observation stays were considered to have originated from an ED visit when revenue center codes 450–459 or 0981 were present on the claim16 and occurring one day prior to or on the same day as the first observation revenue center code.
Analysis
In order to be consistent with prior CMS evaluations of 30-day acute care readmissions, we analyzed data at the encounter level. Descriptive statistics were calculated for key baseline characteristics to understand differences by neighborhood disadvantage. To model the impact of neighborhood disadvantage on 30-day re-observation, we employed a generalized linear model approach (logistic regression for any 30-day re-observation; Poisson regression for number of re-observations in 30 days), with statistical inferences based on patient-clustered robust standard errors. Multivariable model adjustments to isolate the effect of neighborhood disadvantage on 30-day re-observation were chosen based on prior work11,17 evaluating 30-day utilization and model considerations when evaluating health disparities.18 To explore interaction effects, we also conducted a series of stratified analyses for variables determined a priori which potentially modify the impact the effect of ADI on re-observation.19 These subgroups are: race, Medicaid status, age 65 or greater, observations originating in the ED, and disability as the reasons for initial Medicare entitlement. Analyses were conducted using StataSE 15 (StataCorp), and R version 3.6.1. Rate of observation prevalent stays were mapped by census block across the United States using ArcGIS 10.7 (Environmental Systems Research Institute) and displayed by quartiles. Per CMS data use agreement requiring cells of less than 10 to be suppressed, data is presented at the county level to reduce gaps in data presentation.
Results
Overall
Across the entire 20% representative sample, there were 319,980 total index observation stays; 5.1% had at least one re-observation within 30 days (Table 1). Of those experiencing an index observation stay, more than half (59.0%) were female and nearly a third (33.1%) were 80 years of age or older. A total of 31.7% were disabled and 27.3% were on Medicaid. Many experienced an observation stay in the year prior (mean = 0.71 (SD = 2.67)). Targeted readmission diagnoses such as chronic obstructive pulmonary disease (COPD) (16.3%) and congestive heart failure (12.7%) were common index observation diagnoses. Clinical Classification Software codes for re-observations can be found in Supplemental Table 1. A total of 4.5% discharged to a SNF (Table 1).
Table 1.
Key patient and hospital characteristics of Medicare observation patients from January 1, 2014 to November 30, 2014 by neighborhood socioeconomic disadvantage.a
| Key Characteristic | Overall (n=319,980) | Least Disadvantaged 85% (n=278,005) | Most Disadvantaged 15% (n=41,975) |
|---|---|---|---|
| Patients | |||
| Age, y — mean ±SD | 73.03±13.66 | 73.73±13.29 | 68.36±15.07 |
| >=65 y — no. (%) | 253,419 (79.2) | 226,397 (81.4) | 27,022 (64.4) |
| >=80 y — no. (%) | 106,023 (33.1) | 96,143 (34.6) | 9,880 (23.5) |
| Female — no. (%) | 188,702 (59.0) | 163,427 (58.8) | 25,275 (60.2) |
| Race — no. (%) | |||
| White | 254,135 (79.4) | 229,517 (82.6) | 24,618 (58.7) |
| African-American | 40,913 (12.8) | 27,726 (10.0) | 13,187 (31.4) |
| Other race | 23,795 (7.4) | 19,704 (7.1) | 4,091 (9.8) |
| Unknown race | 1,137 (0.4) | 1,058 (0.4) | 79 (0.2) |
| Medicaid — no. (%) | 87,302 (27.3) | 66,407 (23.9) | 20,895 (49.8) |
| Disabled — no. (%) | 101,477 (31.7) | 80,764 (29.1) | 20,713 (49.4) |
| Rural-urban commuting area for patient residence — no (%) | |||
| Urban core area | 204,600 (63.9) | 180,431 (64.9) | 24,169 (57.6) |
| Suburban area | 31,721 (9.9) | 29,080 (10.5) | 2,641 (6.3) |
| Large rural area | 42,027 (13.1) | 34,622 (12.5) | 7,405 (17.6) |
| Small town/isolated rural | 41,412 (12.9) | 33,693 (12.1) | 7,719 (18.4) |
| Unknown area | 220 (0.1) | 179 (0.1) | 41 (0.1) |
| Hierarchical condition category score — mean ±SD | 2.28±1.76 | 2.24±1.74 | 2.49±1.90 |
| Observation stays in year prior — mean ±SD | 0.71±2.67 | 0.65±2.20 | 1.07±4.71 |
| Comorbid conditions in year priorb — no. (%) | |||
| Hypertension | 226,490 (70.8) | 194,246 (69.9) | 32,244 (76.8) |
| Uncomplicated diabetes | 102,137 (31.9) | 85,087 (30.6) | 17,050 (40.6) |
| Fluid and electrolyte disorders | 92,721 (29.0) | 78,346 (28.2) | 14,375 (34.3) |
| Chronic pulmonary disease | 90,149 (28.2) | 75,004 (27.0) | 15,145 (36.1) |
| Deficiency Anemia | 87,525 (27.4) | 73,817 (26.6) | 13,708 (32.7) |
| Hypothyroidism | 63,426 (19.8) | 55,756 (20.1) | 7,670 (18.3) |
| Depression | 62,061 (19.4) | 52,226 (18.8) | 9,835 (23.4) |
| Congestive heart failure | 60,045 (18.8) | 50,065 (18.0) | 9,980 (23.8) |
| Renal Failure | 59,971 (18.7) | 50,286 (18.1) | 9,685 (23.1) |
| Other neurologic disorders | 53,895 (16.8) | 45,996 (16.6) | 7,899 (18.8) |
| Peripheral vascular disease | 46,533 (14.5) | 39,603 (14.3) | 6,930 (16.5) |
| Obesity | 44,946 (14.1) | 36,895 (13.3) | 8,051 (19.2) |
| Valvular disease | 36,369 (11.4) | 32,152 (11.6) | 4,217 (10.1) |
| Complicated diabetes | 32,762 (10.2) | 26,657 (9.6) | 6,105 (14.5) |
| Primary diagnosis of index observation stayc — no. (%) | |||
| Congestive heart failure | 40,685 (12.7) | 34,458 (12.4) | 6,227 (14.8) |
| Acute myocardial infarction | 1,276 (0.4) | 1,094 (0.4) | 182 (0.4) |
| Pneumonia | 4,288 (1.3) | 3,646 (1.3) | 642 (1.5) |
| COPD | 52,286 (16.3) | 43,844 (15.8) | 8,442 (20.1) |
| Length of stay of index observation stay, d — mean ±SD | 1.23±0.64 | 1.23±0.64 | 1.24±0.65 |
| 1 d | 267,940 (83.7) | 233,053 (83.8) | 34,887 (83.1) |
| 2 d | 35,811 (11.2) | 31,042 (11.2) | 4,769 (11.4) |
| 3 d | 12,504 (3.9) | 10,742 (3.9) | 1,762 (4.2) |
| >=4 d | 3,725 (1.2) | 3,168 (1.1) | 557 (1.3) |
| Observation stay originated from ED visit — no. (%) | 253,192 (79.1) | 220,424 (79.3) | 32,768 (78.1) |
| Discharged to skilled-nursing facility — no. (%) | 14,265 (4.5) | 12,742 (4.6) | 1,523 (3.6) |
| Index hospital | |||
| Medical school affiliation — no. (%) | |||
| Major medical school | 64,952 (20.3) | 55,204 (19.9) | 9,748 (23.2) |
| Minor medical school | 75,473 (23.6) | 65,276 (23.5) | 10,197 (24.3) |
| No medical school | 179,442 (56.1) | 157,412 (56.6) | 22,030 (52.5) |
| Unknown medical school | 113 (<0.1) | 113 (<0.1) | 0 (0.0) |
| Hospital type — no. (%) | |||
| Nonprofit, public hospital | 280,503 (87.7) | 244,919 (88.1) | 35,584 (84.8) |
| Nonprofit hospital | 229,888 (71.8) | 202,192 (72.7) | 27,696 (66.0) |
| Public hospital | 50,502 (15.8) | 42,614 (15.3) | 7,888 (18.8) |
| For-profit hospital | 38,241 (12.0) | 32,016 (11.5) | 6,225 (14.8) |
| Annual total discharge volumed, n — mean ±SD | 5,399±4,642 | 5,428±4,662 | 5,209±4,508 |
| Highest tertile — no. (%) | 234,514 (73.3) | 205,068 (73.8) | 29,446 (70.2) |
| Middle tertile — no. (%) | 65,077 (20.3) | 55,876 (20.1) | 9,201 (21.9) |
| Lowest tertile — no. (%) | 20,389 (6.4) | 17,061 (6.1) | 3,328 (7.9) |
| 30-d patient outcomes— no. (%) | |||
| 30-day re-observation | 16,400 (5.1) | 13,543 (4.9) | 2,857 (6.8) |
ED: emergency department; COPD: chronic obstructive lung disease; AIDS: Acquired Immune Deficiency Syndrome.
Neighborhood disadvantage as measured by Area Deprivation Index (ADI).
Comorbidities per Elixhauser methods.
Per Medicare readmission measure definitions.
Total number of patient discharges per hospital in 2013 reflects hospital size and census.
Patient characteristics by neighborhood disadvantage
Patients living in the most disadvantaged neighborhoods had a re-observation rate of 6.8%, while those from the least disadvantaged neighborhoods had a rate of 4.9%. Patients with observation stays and who are living in the most disadvantaged 15% of neighborhoods were younger, more likely to be black, be on Medicaid, and be disabled (Table 1). These patients were also more likely to live in rural areas, have more comorbidities, have more observation stays in the prior 12 months, and were more likely to have index observation stays of the targeted conditions heart failure and COPD. They were also more likely to have an initial observation stay at a for-profit hospital, and were less likely to be discharged to a skilled nursing facility. Elixhauser comorbidities occurring in less than 10% of the population (solid tumor without metastasis, psychoses, weight loss, coagulopathy, rheumatoid arthritis/collagen vascular disease, pulmonary circulation disease, drug abuse, liver disease, alcohol abuse, paralysis, metastatic cancer, chronic blood loss anemia, lymphoma, AIDS, and peptic ulcer excluding bleeding) were included as model adjustments but removed from presentation to reduce table size.
30-day re-observation and neighborhood disadvantage
Living in the most disadvantaged neighborhoods was associated with a 43% increased risk of 30-day re-observation compared to those residing in the least disadvantaged 85% of neighborhoods (unadjusted OR 1.43 [1.31–1.55]). Table 2 displays the impact on the effect of neighborhood disadvantage after adjusting for a series of factors. Adjusting for comorbidities, illness burden, and prior disability, the odds ratio of re-observations was 1.20 [1.10–1.30]. After fully accounting for all factors (including race), living in a disadvantaged neighborhood continued to be associated with re-observation within 30 days (1.13 [1.04–1.22]). Discharge to skilled nursing facility reduced risk of 30 day re-observation (0.63 [0.57–0.69]), while index observation length of stay of four or more days (three or more midnights) conferred increased risk of 30-day re-observation (1.29 [1.09–1.52]). The impact of all individual unadjusted and adjusted variables can be found in the Supplemental Table 2. Results of the stratified analysis failed to suggest evidence for a modified effect for any of the pre-specified subgroups, including Medicaid status.
Table 2.
Unadjusted and adjusted 30-day re-observation risk within the most disadvantaged neighborhoods by variable block adjustments.a
| Unadjusted OR (95% CI) | +Comorbidity block | +Factors during observation stay block | +Hospital characteristics block | +Demographics block | +Race and Medicaid status block | |
|---|---|---|---|---|---|---|
| Additive Model | 1.43 (1.31 – 1.55) | 1.20 (1.10 – 1.30) | 1.18 (1.09 – 1.28) | 1.17 (1.08 – 1.27) | 1.16 (1.07 – 1.26) | 1.13 (1.04–1.22) |
| ADI + Race and Medicaid status | 1.20 (1.11 – 1.31) | |||||
| ADI + Demographics | 1.26 (1.16 – 1.38) | |||||
| ADI + Hospital characteristics | 1.40 (1.29 – 1.53) | |||||
| ADI + Observation stay factors | 1.42 (1.30 – 1.54) | |||||
| ADI + Comorbidities | 1.20 (1.10 – 1.30) |
ADI, Area Deprivation Index; CI, Confidence Internals; OR, Odds Ratio.
Variable block categories. Comorbidities: Hierarchical Condition Category (HCC) score, Elixhauser index variables, disabled; Observation Stay Factors: index observation length of stay, discharge to skilled nursing facility, stay originating from emergency department; Hospital Characteristics: medical school affiliation, nonprofit status, hospital discharge volume; Demographics: age, gender, rural-urban commuting code (RUCA); Race and Medicaid Status: race, Medicaid status.
Chronic re-observation and ADI
Of the 16,400 (5.1%) stays with a re-observation within 30 days, approximately 1 in 7 had more than one re-observation within the same 30 day period. Although more than one re-observation within 30 days of an index observation stay was not common, those with ‘chronic re-observations’ had progressively greater disadvantage by number of observation stays in the 30-day window (Unadjusted Incident Rate Ratio =1.28 [1.21–1.34] and Adjusted Incident Rate Ratio=1.08 [1.02–1.14]) (Figure 1).
Figure 1. Chronic re-observation by patient-level number of re-observations within 30 days of initial index observation stay.
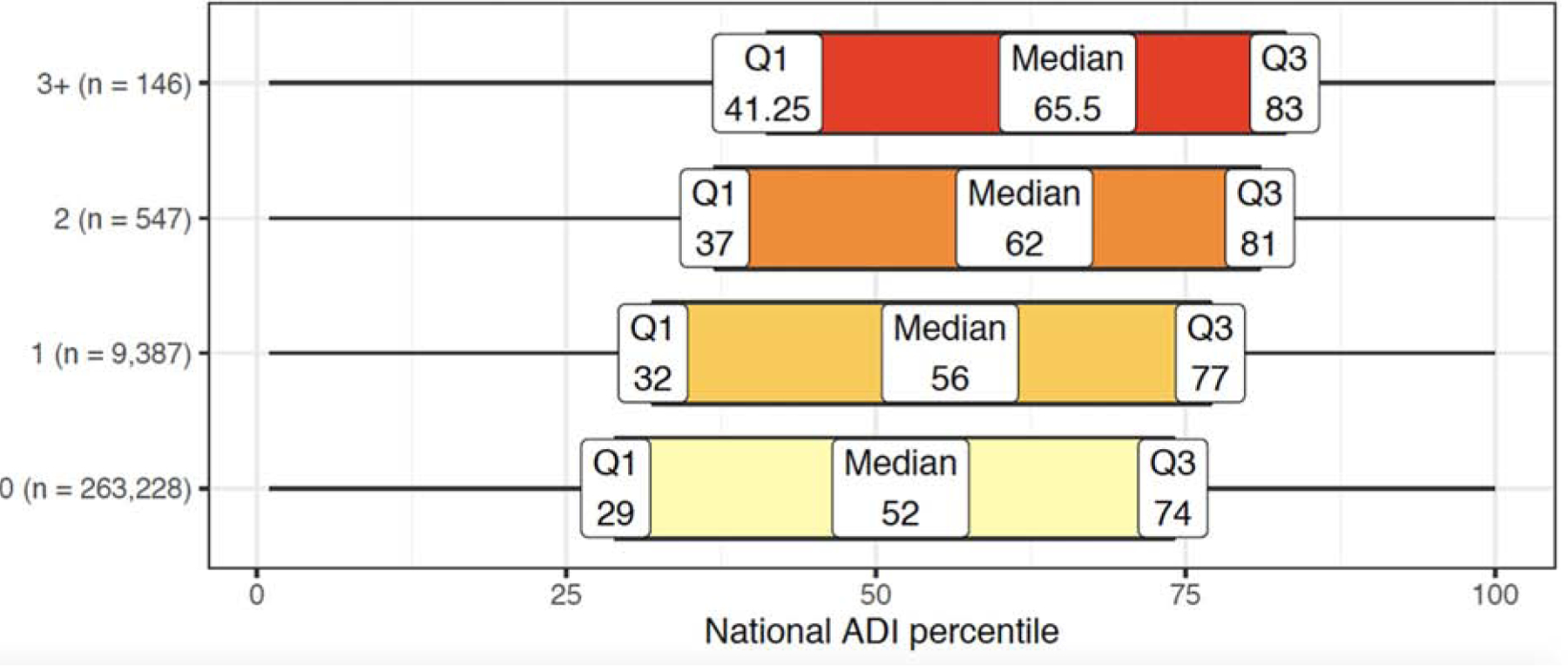
Number of re-observations within 30 days. Median national Area Deprivation Index (ADI) rank with 25–75th interquartile range.
Geographic distribution of observation hospitalizations
A total of 4.4% of all beneficiaries in the 20% fee-for-service enrolled Medicare population had at least one observation stay during the study period (4.3% in the least disadvantaged 85% compared to 5.6% in the most disadvantaged 15%). Figure 2 illustrates the geographic variation across the United States. There was marked variation in observation stay prevalence across the country, with lower rates overall on the west coast and higher rates in the Ohio River Valley area, central Midwest, and parts of the South.
Figure 2. Rate of Medicare beneficiary prevalent observation stays by county, 2014.
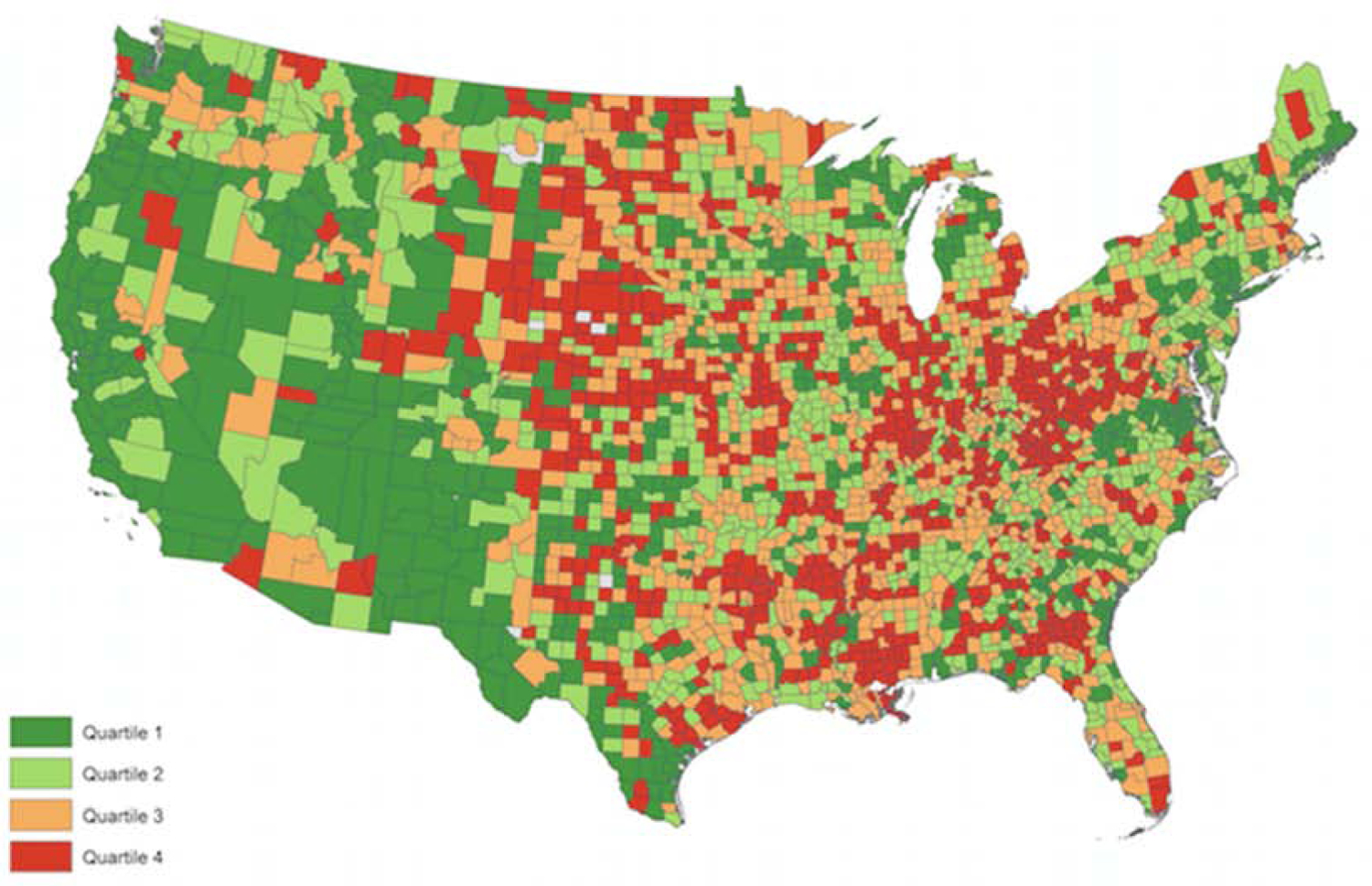
United States mapped by beneficiary nine-digit zip code. Per Centers for Medicare & Medicaid Services data use agreement requiring cells of less than 10 to be suppressed, data is presented at the county level to reduce gaps in data presentation. Quartile 1: 3.43% and below; Quartile 2: 3.44–4.59%; Quartile 3: 4.60–5.84%; Quartile 4: 5.85% and above.
Discussion
Living in a disadvantaged neighborhood impacts a patient’s risk for re-observation, even after accounting for other factors such as race, dual Medicare/Medicaid eligibility, and disability. Neighborhood disadvantage carries similar re-observation risk as several chronic medical conditions, including congestive heart failure and peripheral vascular disease, and carries greater risk than chronic lung disease. Other than ADI, the most predictive covariates for re-observation included dual Medicaid/Medicare eligibility, age, disability, race, and comorbid drug abuse. Importantly, those with ‘chronic re-observations’ within the 30-day follow-up period had progressively greater disadvantage as the number of re-observations increased. These findings strongly suggest that a comprehensive definition of disadvantage including social determinants of health is important to adequately quantify re-observation burden for the most vulnerable Medicare beneficiaries.15,20
Our findings raise several additional critical concerns. First, those living in the most disadvantaged neighborhoods were more likely to have long (four days/three midnights or longer) index observation stays, despite Medicare’s two-midnight rule that directs physicians to order inpatient status when there is a two-midnight expectation.4,21 This is particularly concerning as long observation stays have been shown to be associated with higher out-of-pocket cost,22,23 and these are the patients who can likely least afford such an additional expense. We also found that a long index observation length of stay conferred increased risk of re-observation, demonstrating a cascade effect from a single, long index observation stay.
Disadvantaged patients were also less likely to discharge to a SNF following their index observation stay. Because SNF stays are not covered by Medicare after observation stays, it is not surprising that disadvantaged patients may choose other discharge options. Goldstein and colleagues found that of patients recommended for SNF following an observation hospitalization, only 20% actually discharged to a SNF, many citing cost concerns.24 Importantly, we found that discharge to SNF significantly reduced risk of re-observation after an index observation stay. This finding is of greatest concern for disadvantaged patients staying 3 or more nights under observation who would have been entitled to their SNF benefit if those nights had been considered inpatient nights, adding to the cascade effect from a single, long index observation stay (Figure 3). Our findings also add import and urgency to the recent Health and Human Services Office of Inspector General report directing CMS to study the impact of including observation nights towards the three-midnight requirement for purposes of skilled nursing facility coverage, citing this as one of the Inspector General’s “Top 25 Unimplemented Recommendations” of 2019.25
Figure 3. Cascading effect of long index observation stay and decreased skilled nursing facility discharges on risk of re-observation for beneficiaries residing in the most disadvantaged 15% of neighborhoods.
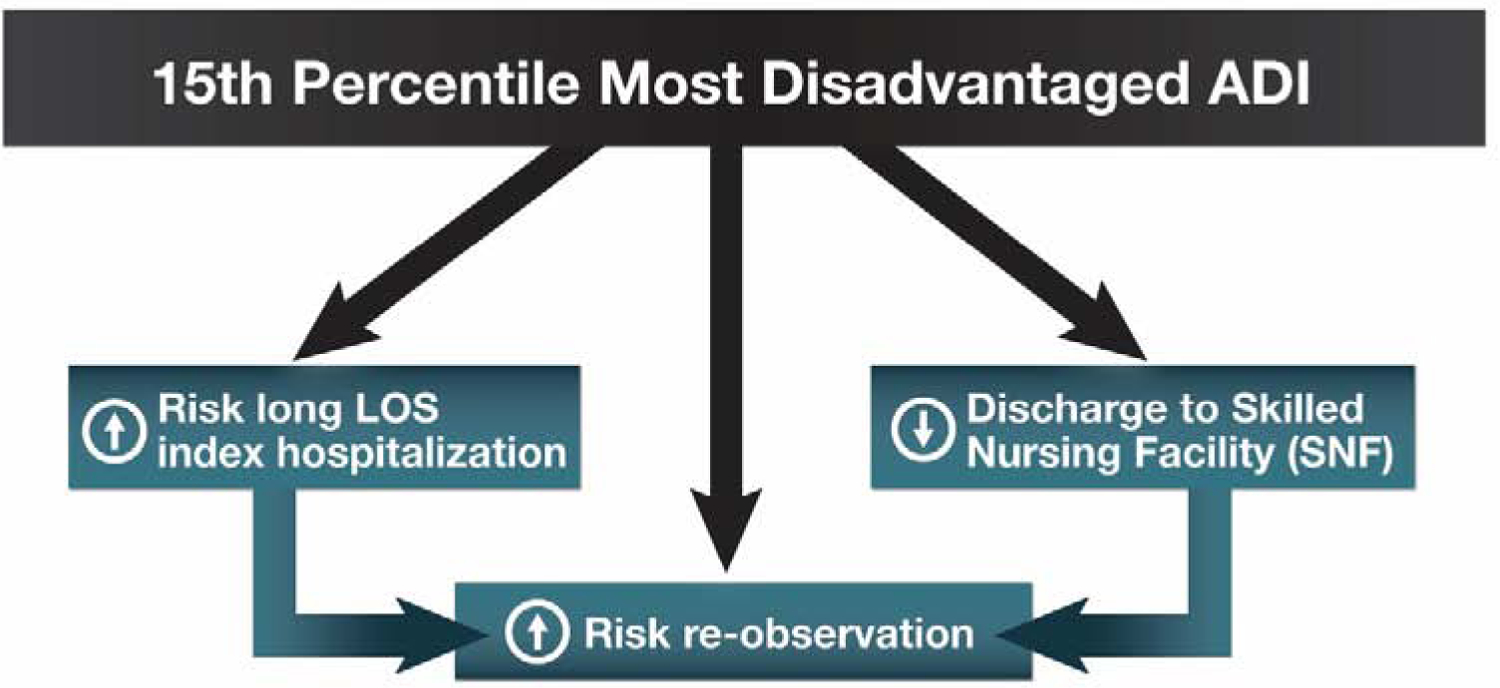
ADI: Area Deprivation Index; LOS: length of stay.
Although one would expect that Medicare policy would be applied consistently across the country, we found that use of observation hospitalizations varied nationally. Patients living in areas with rates significantly above the national average, like those in the Ohio River Valley, Midwest and parts of the South, may be particularly vulnerable to adverse financial consequences of this policy. This geographical variation adds complexity to the observation discussion and merits further study to determine cause of these regional differences.
Importantly, our collective findings may have financial consequences for Medicare beneficiaries. Medical debt accounts for more than half of all debt in the United States, with a mean per capita amount of $579 for those with debt.26 In comparison, the average out-of-pocket cost for a single observation hospitalization in 2012 was $528, which is similar to the published 2019 bundled C-APC 8011 out-of-pocket observation cost of $477.27 Thus, even a single observation stay can prove financially overwhelming for many Americans, not to mention the additive burden on those who experience re-observation, or those who incur SNF costs following observation hospitalizations. These uncovered SNF costs averaged $10,503 in 2012.28 Further, our finding that re-observation, and especially ‘chronic re-observation,’ is highly associated with neighborhood disadvantage means those least able to pay are the most vulnerable to high out-of-pocket risk from serial observation hospitalizations for which there is no cumulative out-of-pocket financial cap.
In addition to impacts on the most disadvantaged individual Medicare beneficiaries, our results also have implications at the systems level, particularly for hospitals and for CMS. Because observation hospitalizations do not count as hospital stays under CMS’ Readmissions Reduction Program, designations of ‘observation status’ for initial and/or recurrent stays may alter hospital quality metrics, hospital reimbursement, readmission metrics, and other measurements and outcomes in intended or unintended ways.29,30 Using 2007–2015 Medicare data, Zuckerman and colleagues concluded that the rise in observation hospital stays did not explain the observed reduction in inpatient readmissions.31 However, the targeted conditions congestive heart failure, chronic obstructive pulmonary disease, pneumonia, and to a lesser degree, myocardial infarction, were fairly common primary diagnoses in our observation and re-observation cohort; these hospitalizations fall outside the Readmissions Reduction Program by virtue of being hospital stays classified as observation. Recently, Figueroa and colleagues found that the decreased inpatient hospitalization rate for ambulatory care-sensitive conditions could largely be accounted for (75%) by the increased use of observation hospitalizations from 2011 to 2015.32 Regardless of Readmission Reduction Program outcomes and impact, this growing number of outpatient hospital stays excluded from many quality metrics29,30 should be considered in utilization measures33–39 and studies of patient out-of-pocket risk, particularly for disadvantaged patients.
Our findings merit additional methodological considerations. Methods for identifying observation stay utilization in Medicare claims varies greatly in the medical literature. We previously reported our validated and reproducible methods for observation stay case finding, including that observation claims identified exclusively with revenue center code 0761 were potentially a different type of service experience for individual patients in that they likely reflect planned care interventions. In this study, we found that 0761-only observation encounters almost never originated with an ED visit and had a high cyclical seven day re-observation rate suggestive of prescheduled visits. We conservatively excluded these visits to avoid elevating our re-observation rate on pre-planned care, but believe 0761-only cases merit future investigation.
Despite strengths of our study including a geo-linked nationally representative sample and robust observation definition, we acknowledge limitations. First, our study was limited to traditional fee-for-service Medicare beneficiaries, so we cannot conclude that commercial payor or Medicare Advantage plans would have similar results. Additionally, our study was limited to the year 2014, and it is possible other years may vary. However, Medicare’s Two-Midnight rule has been in effect since October 1, 2013, so our data reflect current Medicare policy considerations. Our methods also cannot provide statistical analysis between individual and neighborhood effects, given the lack of markers in a nationwide Medicare claims sample available for research. Finally, as the first study linking ADI and observation stays, we chose to exclusively study observation instead of also including inpatient stays. This not only allowed us to analyze unique observation policy issues such as SNF access, length of stay, and risk of repeat stays, but is consistent and parallel to prior work focused exclusively on 30-day inpatient readmissions.11 Future studies using ADI may consider including all types of hospital visits over intervals extending beyond 30 days.
Conclusion
In summary, living in a disadvantaged neighborhood impacts re-observation risk at a rate similar to many chronic medical conditions. Disadvantaged patients may be at risk of higher out of pocket costs through re-observation, chronic re-observation, and reduced SNF access, the latter of which by itself is a risk factor for re-observation. Hospitals and providers might consider using neighborhood disadvantage measured by ADI in initiatives to identify patients needing assistance to help prevent repeat observation hospitalizations. Ultimately, policymakers should consider these equity considerations in future Medicare regulatory decisions.
Supplementary Material
Acknowledgements
We gratefully acknowledge the assistance of Carol Hermann, whose leadership and technical assistance has been invaluable to the production of this manuscript. We also acknowledge the critical efforts of Casey Wagner in assisting with manuscript production.
Funding: This project was supported by a National Institute on Minority Health and Health Disparities Award (R01MD010243 [PI Kind]). This material is the result of work also supported with the resources and the use of facilities at the University of Wisconsin Department of Medicine Health Services and Care Research Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding source had no role in study design, collection, analysis and interpretation of the data, nor in writing of the report or the decision to submit the article for publication.
Abbreviations
- ADI
Area Deprivation Index
- CMS
Centers for Medicare & Medicaid Services
- C-APC
Comprehensive Ambulatory Payment Classification
- ED
Emergency Department
- SNF
Skilled nursing facility
Footnotes
Conflict of interest: Dr. Sheehy served as pro-bono expert witness for the plaintiffs in Alexander v Azar, United States District Court of Connecticut, regarding beneficiary rights to appeal to Medicare when placed under observation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1).Medicare Payment Advisory Commission, Report to the Congress: Medicare and the Health Care Delivery System, Chapter 7—Hospital short-stay policy issues. June 2015. Available at: http://medpac.gov/docs/default-source/reports/june-2015-report-to-the-congress-medicare-and-the-health-care-delivery-system.pdf?sfvrsn=0. Accessed March 14, 2020.
- 2).Sheehy A, Graf B, Gangireddy S, et al. Hospitalized but not admitted: characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med 2013;173(21):1991–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Wachter R Observation status for hospitalized patients: A maddening policy begging for revision. JAMA Intern Med 2013;173(21):1999–2000. [DOI] [PubMed] [Google Scholar]
- 4).Are you a hospital inpatient or outpatient? If you have Medicare--ask! Available at: https://www.medicare.gov/Pubs/pdf/11435-Are-You-an-Inpatient-or-Outpatient.pdf. Accessed March 14, 2020.
- 5).Medicare Payment Advisory Commission, Report to the Congress: Medicare Payment Policy, Chapter 3--Hospital inpatient and outpatient services. March 2019. Available at: http://medpac.gov/docs/default-source/reports/mar19_medpac_entirereport_sec.pdf?sfvrsn=0. Accessed March 14, 2020.
- 6).Kangovi S, Cafardi SG, Smith RA, Kulkarni R, Grande D. Patient financial liability for observation care. J Hosp Med 2015;10(11):718–723. [DOI] [PubMed] [Google Scholar]
- 7).Centers for Medicare & Medicaid Services. Part B Hospital, Chapter 4, section 290.5.3. Available at https://www.cms.gov/files/document/chapter-4-part-b-hospital-including-inpatient-hospital-part-b-and-opps-0. Accessed March 14, 2020.
- 8).Feng Z, Wright B, Mor V. Sharp rise in Medicare Enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Affairs. 2012;31(6):1251–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Wright B, Zhang X, Rahman M, Abir M, Ayyagari P, Kocher K. Evidence of racial and geographic disparities in the use of Medicare observation stays and subsequent patient outcomes relative to short-stay hospitalizations. Health Equity. 2018;21:45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Singh G Area deprivation and widening inequalities in U.S. mortality, 1969–1998. Am J Public Health. 2003;93:1137–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Kind AJH, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann Intern Med 2014;161(11):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Sheehy A, Shi F, Kind A. Identifying observation stays in Medicare data: Policy implications of a definition. J Hosp Med 2019;14(2):96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Centers for Medicare & Medicaid Services. Measures Inventory Tool: Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure. Available at: https://cmit.cms.gov/CMIT_public/ListMeasures?q=Claims-Based%20Hospital-Wide%20All-Cause%20Unplanned%20Readmission%20Measure. Accessed March 14, 2020.
- 14).United States Census. American Community Survey. Available at: https://www.census.gov/programs-surveys/acs/. Accessed March 14, 2020.
- 15).Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible—The Neighborhood Atlas. N Engl J Med 2018; 378:2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Venkatesh AK, Mei H, Kocher KE, et al. Identification of Emergency Department Visits in Medicare Administrative Claims: Approaches and Implications. Acad Emerg Med 2017;24(4): 422–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Joynt Maddox K, Reidhead M, Hu J, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. HSR 2019;54(2): 327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Cook BL, McGuire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care: methods and practical issues. HSR 2012;47:1232–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003; 326(7382):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Office of Disease Prevention and Health Promotion. Healthy People 2020. Social Determinants of Health; https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed January 16, 2020. [Google Scholar]
- 21).Office of Inspector General. Vulnerabilities Remain Under Medicare’s 2-Midnight Hospital Policy. December 2016. Available at: https://oig.hhs.gov/oei/reports/oei-02-15-00020.asp. Accessed March 12, 2020.
- 22).Hockenberry JM, Mutter R, Barrett M, Parlato J, Ross M. Factors associated with prolonged observation services stays and the impact of long stays on patient cost. HSR 2014;49(3):893–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).Baugh C, Schuur J. Observation Care. N Engl J Med 2013;369:1474–1475. [DOI] [PubMed] [Google Scholar]
- 24).Goldstein J, Schwartz J, McGraw P, Banks T, Hicks L. The unmet need for postacute rehabilitation among Medicare observation patients: a single center study. J Hosp Med 2017;12:168–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).July 2019: Solutions to reduce fraud, waste, and abuse in HHS programs: OIG’s top recommendations. Available at: https://oig.hhs.gov/reports-and-publications/compendium/files/compendium2019.pdf. Accessed March 12, 2020.
- 26).Consumer Financial Protection Bureau. Consumer credit reports: a study of medical and non-medical collections. Available at: https://files.consumerfinance.gov/f/201412_cfpb_reports_consumer-credit-medical-and-non-medical-collections.pdf. Accessed March 14, 2020.
- 27).LogixHealth. 2019. Outpatient Payment System Update. Available at: https://www.logixhealth.com/uploads/PDF/LogixHealth-2019%20OPPS%20Update.pdf. Accessed March 14, 2020.
- 28).Office of Inspector General. Hospitals’ use of observation stays and short inpatient stays for Medicare beneficiaries. Available at: https://oig.hhs.gov/oei/reports/oei-02-12-00040.asp. Accessed March 14, 2020.
- 29).Sabbatini A, Wright B. Excluding observation stays from readmission rates—what quality measures are missing. N Engl J Med 2018;378:2062–2065. [DOI] [PubMed] [Google Scholar]
- 30).Wadhera R, Yeh R, Joynt Maddox K. The Hospital Readmissions Reduction Program—time for a reboot. N Engl J Med 2019;380(24):2289–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31).Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med 2016;374:1543–51. [DOI] [PubMed] [Google Scholar]
- 32).Figueroa JF, Burke LG, Zheng J, Orav EJ, Jha AK. Trends in Hospitalization vs Observation Stay for Ambulatory Care-Sensitive Conditions. JAMA Intern Med 2019;179(12):1714–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33).Cerasale M, Watson P. Use of observation stays in calculating hospitalizations among Medicare beneficiaries. JAMA 2015;314(4):355–365. [DOI] [PubMed] [Google Scholar]
- 34).Horowitz LI, Wang Y, Altaf FK, et al. Hospital characteristics associated with postdischarge hospital readmission, observation and emergency department utilization. Med Care. 2018;56:281–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35).Nuckels TK, Fingar KR, Barrett ML, et al. Returns to emergency department, observation, or inpatient care within 30 days after hospitalization in 4 states, 2009 and 2010 versus 2013 and 2014. J Hosp Med 2018;13:296–303. [DOI] [PubMed] [Google Scholar]
- 36).Nuckels TK, FIngar KR, Barrett M, Steiner CA, Stocks C, Owens PL. The shifting landscape in utilization of inpatient, observation, and emergency department services across payors. J Hosp Med 2017;12:443–446. [DOI] [PubMed] [Google Scholar]
- 37).Dharmarajan K, Qin L, Bierlein M, et al. Outcomes after observation stays among older adult Medicare beneficiaries in the USA: retrospective cohort study. BMJ. 2017;357: j2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38).Venkatesh AK, Wang C, Ross JS, et al. Hospital use of observation stays: cross sectional study of the impact on readmission rates. Med Care. 2016;54:1070–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39).Albritton J, Belnap T, Savitz L. The effect of the hospital readmission reduction program on the duration of observation stays: using regression discontinuity to estimate causal effects. eGEMS 2017;5(3):6,1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


