Abstract
The metabolic syndrome (MS) is a set of metabolic disturbances, represented by various cardiovascular risk factors which are generally associated with the central accumulation of fat and the resistance to insulin. Inadequate changes in eating behaviours and weight loss, which are associated to taking part in regular physical activity, are considered to be primary and first choice therapies for the treatment of MS, as they assist in the reduction of the abdominal girth and visceral fat, improve the sensibility to insulin and reduce the plasmatic concentrations of glucose and triglycerides, raise the values of high density lipoproteins and, consequently decrease the risk factors which contribute to the development of type 2 diabetes. The MS is a current discussion theme in the health field as it is related to illnesses/diseases, which not only cause a worldwide high mortality rate but show increasing incidence. Type 2 diabetes is characterised by a deregulation of the carbohydrates, lipids and proteins found in the metabolism and result in diminished secretion of insulin, resistance to insulin or a combination of both. Type 2 diabetes is the most form of diabetes of the first 3 types of diabetes, representing 90% of all cases. Diabetes is a chronic and complex disease which requires a strict medical follow-up so as to reduce the risks and obtain strategies for its control. The fast-epidemiological global evolution which has been registered in the last few years, leads to it being considered one of the pandemics of the 21st century. In this non-systematic and advanced review of the MS in type 2 diabetic patients, several articles were consulted, and some recently published studies were analysed.
Keywords: metabolic syndrome, type 2 diabetic
Introduction
In the 9th edition of the International Diabetes Federation (IDF) Diabetes Atlas, the prevalence of diabetes is estimated in 2019 and projected for 2030 and 2045. It is estimated that there are 463.0 million cases of diabetes among adults between the ages of 20 and 79 including both type 1 and type 2 worldwide1 (Fig. 1).
Figure 1.
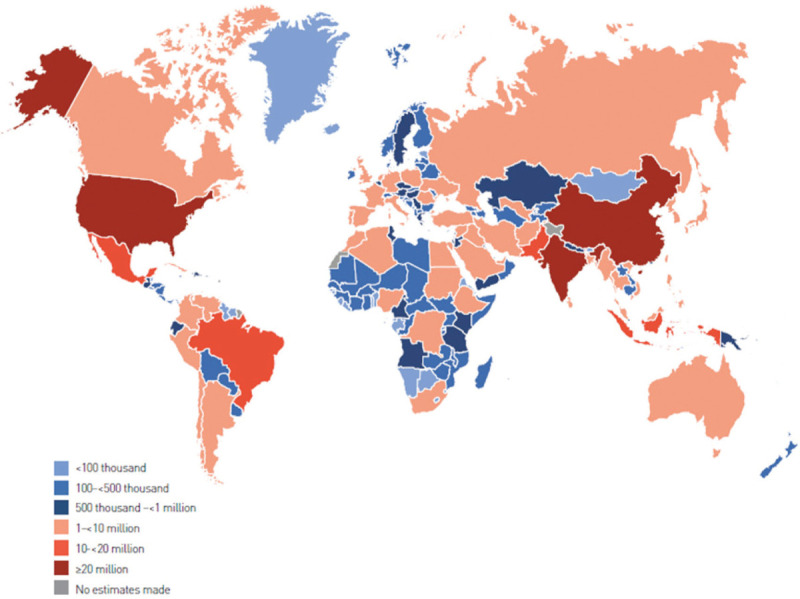
Total estimated number of adults (20- to 79-year-old) with diabetes in 2019. Source. IDF Diabetes Atlas, 9th Edition.
Based on the estimates for 2019 regarding adults between 20 and 79 years old, the projected figure for 2030 is 578.5 million, rising to 700.2 million in 2045 he numbers of patients who will live with diabetes (Table 1).
Table 1.
Number of men and women (20–79 years) with diabetes in 2019, 2030 and 2045
| 2019 | 2030 | 2045 | ||||
|---|---|---|---|---|---|---|
| Number of people with diabetes (millions) | Prevalance (%) | Number of people with diabetes (millions) | Prevalance (%) | Number of people with diabetes (millions) | Prevalance (%) | |
| Men | 240.1 | 9.6 | 296.7 | 10.4 | 357.7 | 11.1 |
| Women | 222.9 | 9.0 | 281.8 | 10.0 | 342.5 | 10.8 |
Source. IDF Diabetes Atlas, 9th Edition.
It is estimated that in 2019, 463 million people will have diabetes and that number is expected to reach 578 million until 2030 and 700 million until 2045. More than 4 million people, between the ages of 20 and 79 died of diabetes related causes in 2019. The number of children and adolescents (in other words until the age of 19) living with diabetes increases annually. Another cause for alarm is the high percentage of undiagnosed diabetes, presently over 50% and being predominantly type 2 diabetes cases. There are situations that people with a set of risk factors, essentially cardiovascular, have more chance to develop cardiovascular disease (heart attack and stroke) and diabetes. This finding is called metabolic syndrome (MS).
The MS does not give symptoms and its only sign is the presence of a prominent abdomen. This syndrome affects more than a third of the adult Portuguese population. Thus, the necessity for urgent diagnosis of people who are undiagnosed with diabetes, and the need to offer adequate and timely treatment to all diabetes sufferers.2
Based on the facts presented, this study aims to gather information about MS and diabetes in order to contribute to the identification of an accurate diagnosis and ensure a better quality of life for patients, focusing on the development of more effective treatment options.
Metabolic syndrome
The first formal definition for MS occurred during a discussion about diabetes among a group of World Health Organization (WHO) consultants in 1998. At the time, the question of resistance to insulin was highlighted as being the main risk, and the need to have a clinical proof of the fore mentioned resistance for the diagnosis.3,4 Consequently, the IDF published a globally recognised and accepted definition of MS in 2006. In the document, MS is defined as a set of cardiovascular and as a new epidemic.5
The Joint Scientific Declaration, published in 2009, characterises the MS as a complexity of risk factors related to the cardiovascular system and diabetes mellitus.3
It may be referred, that among the main comorbidities which are known and associated with the MS may be found among individuals who have abdominal obesity and show resistance to insulin. These 2 conditions are strongly related with the occurrence of metabolic risk factors.
Some studies3,5,6 refer that obesity and resistance to insulin are fundamental causes of this syndrome, highlighting that central obesity, which is characterised by the concentration of fat in the abdominal region, is highly associated with MS. Central obesity may also be involved with the development of type 2 diabetes and the risk of cardiovascular diseases. According to the world consensus of MS, the causes are resistance to insulin and central obesity, however, both conditions may be associated with other clinical conditions such as atherosclerosis, overweight and type 2 diabetes.1,5,7
The diagnosis of MS can be made when at least 3 factors of the following 5 are present: abdominal obesity—abdominal circumference that exceeds 102 cm in men and 88 cm in women indicates excess abdominal fat, triglycerides equal to or >150 mg/dl, high density lipoproteins (HDL) cholesterol equal to or <40 mg/dl in men and 50 mg/dl in women, blood pressure equal to or >135/85 mm Hg, and fasting blood glucose equal to or >100 mg/dl.3
MS is considered to be a public health concern due to its growing prevalence. Several scientists have alerted to a greater awareness of people's lifestyles, where the National Health System of every country is concerned. In clinical terms, the focus is on identifying and reducing the risk factors which are associated with the MS, including people's lifestyles.
Epidemiology of the metabolic syndrome
In 2006, the prevalence of the MS was between 20% and 25% worldwide and was already considered as one of the most common chronic diseases, placed fourth in the list of the main causes of death in the whole world.5
A narrative review of the literature available in 20148 showed that the global prevalence of MS varied from 10.0% to 84.0%, being influenced by various socio-economic and demographic factors, among which are age and body mass index. These varied from 5.0% (eutrophic) to 60.0% (obese), as well as 10.0% (20- to 29-year-old) to 45.0% (60- to 69-year-old), respectively.8
In developed European countries the prevalence of MS is high. In this context, an European study analysed 8 cohorts (total: 8200 men and 9363 women) researching the frequency of MS according to the WHO's criteria and compared the data with an alternative proposed definition of MS for non-diabetic individuals. The study concluded that the prevalence of MS varies from 7.0% to 36.0% in men between the ages of 40 and 55, and from 5.0% to 22.0% among women in the same age bracket, although a progressive increase that was directly proportional to the increase in age was noticed for both genders, the percentage was higher among men than women in many cases.9
Further to cardiovascular diseases and type 2 diabetes, the MS is also considered a risk factor for strokes and kidney diseases.10 A study published in the National Health and Nutrition Examination Survey (NHANES) 50, which was carried out in the USA between 1999 and 2010, analysed on a temporary basis the prevalence of MS in adults. Although the analysis showed a decline in the prevalence of MS in the USA, changes in its components were evident among the population, as was the case of abdominal obesity, which was a growing tendency in the whole population since the start of the study.
Another systematic review which was published in 2013 concerning the prevalence of MS in Brazil, covering 10 publications since 2006 to 2012, showed the average prevalence varied from 28.9% to 29.6% due to the criteria for diagnosing MS. The lowest rate was a result of using the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria. When adjustments were made according to age, the average prevalence was 22.0%, rising to 41.3% when it was adjusted by gender.11
Metabolic syndrome and type 2 diabetes
MS has been associated with type 2 diabetes due to its high prevalence worldwide since it is both related to the increase in obesity and a sedentary lifestyle. Several studies suggest that individuals with MS are 5 times more likely to develop type 2 diabetes.3,12,13
Type 2 diabetes is a rising global health problem. Individuals with type 2 diabetes are at higher risk of microvascular complications (including retinopathy, nephropathy and neuropathy) and macrovascular complications (such as cardiovascular diseases and other comorbidities), due to hyperglycaemia and individual components of insulin resistance (IR). Environmental factors also contribute to the multiple physiopathological disturbances responsible for the decrease of glucose homeostasis in type 2 diabetes.14
Diabetes as an important health problem has reached alarming levels. Nowadays, almost half a billion people are living with diabetes worldwide1 (Fig. 2).
Figure 2.

Prediction of increase in diabetes worldwide. Source. IDF Diabetes Atlas, 9th Edition.
Epidemiology of diabetes
Type 2 diabetes corresponds to a percentage that ranges from 90.0% to 95.0% of the cases of diabetes which do not require insulin treatment.15
In a great majority of developed countries, diabetes is the main cause related to cardiovascular diseases and other complications. The total number of cases of diabetes in the world has been increasing noticeably, and in 30 years the global prevalence of diabetes has become 12 times greater, a rise which was mostly due to new cases of type 2 diabetes.16
In an update of the IDF World Atlas of Diabetes, the data gathered from 220 countries and territories shows that in 2015 the prevalence of diabetes among adults between the ages of 20 and 79 was approximately 8.8%, which corresponds to about 415 million people. From that total number, only 25.0% are from developed countries, while the remaining results are from emerging and underdeveloped countries. According to the Atlas, the estimate for 2040 is more than 600 million people or 1 in every 10 adults will suffer from diabetes.7
Presently, there are 351.7 million working people between the age of 20 to 64, who have been either diagnosed or not diagnosed with diabetes in 2019. This figure should increase considerably to 417.3 million until 2030 and to 486.1 million until 2045. The greatest rise will occur in regions where the economies are evolving from low earnings to average earnings (Table 2).
Table 2.
Number of adults (20- to 79-year-old) with diabetes by World Bank income ranking in 2019, 2030 and 2045
| 2019 | 2030 | 2045 | ||||
|---|---|---|---|---|---|---|
| World Bank income classification | Prevalence of diabetes (%) | Number of people with diabetes (millions) | Prevalence of diabetes (%) | Number of people with diabetes (millions) | Prevalence of diabetes (%) | Number of people with diabetes (millions) |
| High-income countries | 10.4 (8.6–13.3)∗ | 95.2 (78.7–120.9) | 11.4 (9.4–14.3) | 107.0 (88.3–134.4) | 11.9 (9.8–14.8) | 112.4 (92.2–139.2) |
| Middle-income countries | 9.5 (7.6–12.3) | 353.3 (280.1–455.3) | 10.7 (8.4–13.7) | 449.6 (353.0–576.7) | 11.8 (9.0–15.0) | 551.2 (422.7–705.2) |
| Low-income countries | 4.0 (2.8–6.7) | 14.5 (10.0–24.3) | 4.3 (3.0–7.1) | 21.9 (15.2–36.4) | 4.7 (3.3–7.9) | 36.5 (25.8–60.2) |
95% confidence intervals are reported in brackets.
Source. IDF Diabetes Atlas, 9th Edition.
The age range in which diabetes is more prevalent globally is among 60- to 79-year-old (18.6%), a group where a greater growth, proportional to the cases, is expected. However, quantitatively, there is a greater number of cases in the 40 to 59 age brackets. The majority of the cases of diabetes occurs in low to average income, where a greater increase proportional to the cases is expected. Further to the rise of the economic income, there is an inverse proportional growth, in other words, the lower the income, the greater the prevalence of diabetes.17
The lack of glucose control contributes to the high figures which are associated to the prevalence of the disease, which according to the American Diabetes Association, 33.0% to 49.0% of diabetes is due to sufferers failing to reach the goals for glucose control, blood pressure and cholesterol.15 Other factors worth referring to are: the person having 2 or more diseases, social and financial hardships as well as specific challenges to reach the proposed objectives in the treatment of diabetes.
The global cost for the treatment and prevention of the complications of diabetes has been estimated, in a conservative analysis, to be 673 billion dollars, or according to a more open analysis, the figure rises to 1197 billion dollars. It is forecasted that this figure will have risen from 802 to 1425 billion dollars in 2040.7
Pathophysiology of diabetes
The most recent publications describe the pathophysiology of diabetes as being different between type 1 and type 2. A review about the pathophysiological and pathogenic mechanisms of diabetes made in 2013 showed findings which evidence differences between these 2 types of diabetes. Another narrative review which covers classification, pathophysiology, diagnosis and management of diabetes made in 2015 also supports this information.18,19
Individuals with type 2 diabetes present identifiable circulating insulin levels. An oral glucose tolerance test enables a thorough separation of the different metabolic characteristics.18,19 There are individuals who have normal glucose tolerance; others with impaired or lower glucose tolerance, and they can be stratified as a chemical diabetic group. Those individuals whose hyperglycaemia present values lower than 140 mg/dl have diabetes with mild fasting hyperglycaemia; and over that value, it is classified as diabetes associated with evident fasting hyperglycaemia.18
When a tolerance result is identified, simultaneous damaged glucose and high plasma insulin levels, it is a clear biochemical proof of IR. By progressing from intolerance to diabetes, since insulin levels decrease, the characteristic of the decrease of secretion of that hormone in type 2 diabetes is reinforced, a trait which is commonly evident in the majority of patients with diabetes (type 2).18,19
The pathophysiology of type 2 diabetes involves a variable combination of IR (mainly in the liver and muscles) and a decrease in insulin secretion by pancreatic beta cells. Both can be influenced by genetic and environmental factors. Furthermore, other alterations can be related to the pathophysiology of type 2 diabetes, highlighting the dysregulation of hormonal secretion in entero-hypothalamic and entero-insular axes, reflecting, in this case, the multifactorial nature of the disease.20
The beta cell's incapacity of responding to the increasing demand of peripheral insulin, observed during the progressive evolution of IR in glucose intolerant individuals, is nowadays accepted as a determining phenomenon in the development of diabetes. With this in mind, all the patients with type 2 diabetes have measurable beta cell dysfunction, since the magnitude of the IR after its onset slightly increases with time, however, on the other hand, deterioration of beta cell function is progressive, leading to a progressive loss of therapeutic response from the beta cells.21
During the evolution of IR, it is observed a progressive increase in basal insulin concentrations in the blood, namely in obese individuals. This increase can be maintained in some people, while others lose it. The former will stay normoglycemic and insulin resistant, whilst the latter will definitely lose the capacity of maintaining the glucose homeostasis.22
The ectopic fat deposition has better prognosis as well as a more important role in the development of IR if compared to deposition and evaluation of visceral fat. This happens because muscle and hepatic cells, full of fat, suffer interference in their normal metabolism. The metabolite of triglycerides is capable of influencing insulin signalling, glucose transport, phosphorylation and muscular glycogen synthesis as well as the increase of hepatic gluconeogenesis.23
Insulin is a hormone produced by pancreatic beta cells (Fig. 3), which synthesis is activated when there is an increase of plasma levels of glucose and amino acids, having an effect in several tissues, particularly in muscles, liver and adipose tissue.24
Figure 3.
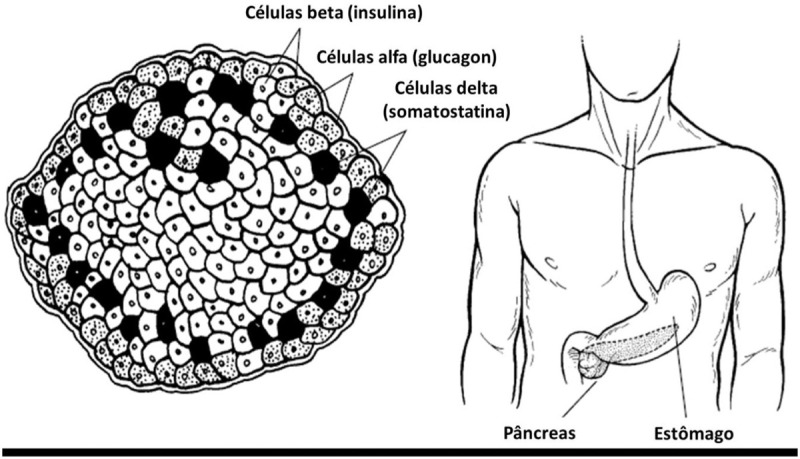
Pancreatic cells. Source. Type 1 Diabetes For Dummies, 2008.
In spite of IR being potentially seen as the main cause, insulin deficiency can also be considered the primary cause, since moderate IR is not enough to effectively induce type 2 diabetes. Furthermore, the majority of the people diagnosed with this disease have both situations. Due to presenting lighter symptomatology, several individuals happen to detect type 2 diabetes when complications are already evident.
Resistance to insulin
In non-diabetic population, the resistance to insulin may be associated with metabolic/cardiovascular alterations, which comprise: systemic arterial hypertension, hypertriglyceridemia, reduction of HDL-c (high density lipoproteins), increase of LDL-c (low density lipoproteins), intolerance to carbohydrates, centripetal obesity, increase of PAI-1, hyperuricemia and atherosclerotic cardiovascular disease. This set of alterations is known as MS. In view of these associations it is important to assess the sensitivity to insulin. The assessment may be divided into direct or indirect methods. The direct methods analyse the effects of a set quantity of insulin injected into an individual. On the other hand, the insulin action may be evaluated through the effect of endogenous insulin, mainly in homeostasis conditions.
The indirect methods consist of: fasting insulinemia, homeostasis model assessment (HOMA), HOMA-Adiponectinemia (HOMA-AD), QUICKI (Quantitative Insulin Sensitivity Check Inbox, Oral Glucose Tolerance Test (OGTT), and Frequent Sample IV Glucose Tolerance Test (FSIVGTT).
In the absence of the above-mentioned methods, there are complementary means to assess IR, namely: ATIC (Average thickness of internal carotid), hormones, enzymes, inflammatory markers, coagulation factors, anthropometric indicators and body composition. The last 2 assess the individual's phenotype and may be clustered according to the type of obesity being assessed: central or generalized.25
Complications of diabetes
Generically, diabetes can result in several complications associated with organs and tissues such as the heart, blood vessels, eyes, kidneys and nerves (eg, retinal lesion or physical disability due to lower limb amputation).26
One of the many complications associated with diabetes is hypoglycaemia. When blood glucose levels are under 70 mg/dl, it is considered severe hypoglycaemia and if they are under 40 mg/dl, a hypoglycemic crisis is considered diabetic ketoacidosis, being more common in type 1 diabetes, but which can be fatal.27
Diabetic retinopathy, which is common in type 1 and 2 diabetes, is a microvascular complication which frequently leads to blindness in adults and it can be related to the duration of diabetes, hypertension, hyperglycaemia and nephropathy.28
Another common complication is kidney failure and the association with diabetes makes it easier for its clinical evolution towards dialysis. Diabetic Kidney Disease (DKD) is the main triggering factor of end-stage kidney disease. In type 2 diabetes, the DKD marker is albumin-to-creatinine ratio, which represents an excellent cardiovascular risk factor in a 3 to 1 ratio.16,28
Diabetes also presumes the development of several diseases such as non-alcoholic fatty liver disease, periodontal disease, hearing loss, erectile dysfunction, depression, difficulty in conceiving or during pregnancy.26
Every patient with diabetes presents a few metabolic risks which need intervention whether in their lifestyle or medication administration. Hyperglycaemia which has diabetic glucose levels is one of the 5 criteria associated with MS diagnosis both by National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) and IDF. The majority of people with type 2 diabetes fit in the criteria associated with MS.3,16
Conclusion
The majority of the studies included in this review reveal that MS is a cluster of disturbances which, once associated with other pathologies, causes severe alterations in the human body that affects namely patients with type 2 diabetes.
Some studies also refer that people with a recent diagnosis of diabetes can be “seen” with this syndrome since it can affect both the newly diagnosed diabetics and those who have been diagnosed for longer. Therefore, it depends on the type of comorbidities that each person has. Closely related to this is the duration of diabetes, a factor which can ease the emergence of MS, whether at a quicker or a slower rate, due to the several comorbidities associated with, including cardiac and vascular problems.
It can be taken into consideration that the environment which surrounds the individual (eg, place of residence or geographic area) can be favourable to this kind of pathology. In addition to the environment, other characteristics can be taken into account such as labour and working conditions, hygiene, social conditions, amongst others.
Supporting this line of thought, it can be concluded that socioeconomic status, provided by the environment and the lifestyle of our population, namely European, is a risk factor for cardiovascular diseases and other comorbidities, mainly MS.
In some systematic reviews, different methods were used, in terms of evaluation of MS. One of them classified these methods in terms of relevance in a hierarchical manner: first NCEP ATP III (2001), followed by a modified version of 2005 (AHA/NHLBI), then WHO (1998), and, at last, a modified version of WHO (1999). In the research made, the described diagnosis criteria used both for type 2 diabetes and MS possibly contribute to the high heterogeneity between these pathologies.
Comparing individual components of MS in individuals from a type 2 diabetes sample, obesity is more common in women than men as well as hypertension, uncontrolled hyperglycaemia, high levels of triglycerides and LDL-c and low levels of HDL-c. The same authors say that such alterations increase with age in this particular population, becoming a potential factor for cardiovascular risk factors.
Globally, it is observed the importance of a holistic and non-fragmented vision, not only when it comes to diabetes but also to the cluster of comorbidities to which it may be associated with, including MS.
It is suggested the development of more studies about this topic, similar to the ones made in oriental and developing countries, in order to evaluate and compare health conditions, disease and epidemics. It would also be interesting to evaluate the possible cultural influence of each continent and its population on the prevalence of the disease.
Conflicts of interest
The authors declare no competing interests.
References
- [1].International Diabetes Federation IDF Diabetes Atlas. 9th edBrussels: International Diabetes Federation; 2019. [Google Scholar]
- [2].Alberti K, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. [DOI] [PubMed] [Google Scholar]
- [3].Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. [DOI] [PubMed] [Google Scholar]
- [4].Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. [DOI] [PubMed] [Google Scholar]
- [5].Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–480. [DOI] [PubMed] [Google Scholar]
- [6].Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. [DOI] [PubMed] [Google Scholar]
- [7].International Diabetes Federation IDF Diabetes Atlas. 7th edBrussels: International Diabetes Federation; 2015. [Google Scholar]
- [8].Kaur J. A comprehensive review on metabolic syndrome. Cardiol Res Pract. 2014;2014:943162. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [9].Balkau B, Charles M-A, Drivsholm T, et al. Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabetes Metab. 2002;28:364–376. [PubMed] [Google Scholar]
- [10].Beltrán-Sánchez H, Harhay MO, Harhay MM, McElligott S. Prevalence and trends of metabolic syndrome in the adult US population, 1999–2010. J Am Coll Cardiol. 2013;62:697–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].de Carvalho Vidigal F, Bressan J, Babio N, Salas-Salvadó J. Prevalence of metabolic syndrome in Brazilian adults: a systematic review. BMC Public Health. 2013;13:1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Huang PL. A comprehensive definition for metabolic syndrome. Disease Models Mech. 2009;2:231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Garvey WT, Ryan DH, Henry R, et al. Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care. 2014;37:912–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Ministério da Saúde. Retrato da Saúde, Portugal; 2018. https://www.sns.gov.pt/wp-content/uploads/2018/04/RETRATO-DA-SAUDE_2018_compressed.pdf. [Google Scholar]
- [15].American Diabetes Association Classification and diagnosis of diabetes. Diabetes Care. 2015;38 (Suppl 1):S8–S16. [DOI] [PubMed] [Google Scholar]
- [16].Leon BM, Maddox TM. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6:1246–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–149. [DOI] [PubMed] [Google Scholar]
- [18].Baynes HW. Classification, pathophysiology, diagnosis and management of diabetes mellitus. J Diabetes Metab. 2015;6:1–9. [Google Scholar]
- [19].Ozougwu J, Obimba K, Belonwu C, Unakalamba C. The pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. J Physiol Pathophysiol. 2013;4:46–57. [Google Scholar]
- [20].DeFronzo RA. Pathogenesis of type 2 diabetes mellitus. Med Clin. 2004;88:787–835. [DOI] [PubMed] [Google Scholar]
- [21].Cnop M, Welsh N, Jonas JC, Jorns A, Lenzen S, Eizirik DL. Mechanisms of pancreatic beta-cell death in type 1 and type 2 diabetes: many differences, few similarities. Diabetes. 2005;54 (Suppl 2):S97–S107. [DOI] [PubMed] [Google Scholar]
- [22].Prentki M, Nolan CJ. Islet beta cell failure in type 2 diabetes. J Clin Invest. 2006;116:1802–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Sjöström C, Lissner L, Sjöström L. Relationships between changes in body composition and changes in cardiovascular risk factors: the SOS Intervention Study. Swedish Obese Subjects. Obes Res. 1997;5:519–530. [DOI] [PubMed] [Google Scholar]
- [24].De Luca C, Olefsky JM. Inflammation and insulin resistance. FEBS Lett. 2008;582:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25]. Geloneze B, Vasques, AC, Tambascia MA. Resistência à Insulina: como diagnosticar na Prática Clínica. In: Amelio F. de Godoy-Matos. (Org.). Endocardiometabologia na prática clínica. 2 ed. São Paulo: Guanabara Koogan Ltda, 2011;(1):47–63. [Google Scholar]
- [26]. National Center for Health Statistics (US). Health, United States, 2014: With Special Feature on Adults Aged 55–64. Hyattsville, MD: National Center for Health Statistics (US); 2015 May. Report No.: 2015–1232. [PubMed] [Google Scholar]
- [27].American Diabetes Association Diabetes care in the hospital, nursing home, and skilled nursing facility. Diabetes Care. 2015;38 (Suppl 1):S80–S85. [DOI] [PubMed] [Google Scholar]
- [28].American Diabetes Association Microvascular complications and foot care. Diabetes Care. 2015;38 (Suppl 1):S58–S66. [DOI] [PubMed] [Google Scholar]


