Introduction
Through the course of the last several decades, the rate of obesity has progressively increased and is now one of the leading causes of death worldwide. The World Health Organization reports 1.9 billion adults were overweight in 2016 and 650 million were considered obese.1 According to the Center for Disease Control, the prevalence of obesity in the United States was 30.5% in 1999. This increased to 42.4% by 2017.2 In conjunction with this, chronic illnesses associated with obesity such as diabetes and cardiovascular disease are now among the top causes of death in the United States.3 In 2008, the medical cost for obesity was $147 billion. This was $1,429 higher than the cost for non-obese patients.2
Several factors have been attributed to this epidemic with the western diet considered to be a major contributor to the growing rate of obesity in the United States. Although current lifestyle trends emphasize the importance of eating healthy, we continue to see foods high in fat and sugar as major components of the Western diet which has corresponded to the steady rise in obesity. The management of obesity is therefore an important discussion with many now acknowledging that diet modification would have the greatest impact on this growing epidemic.
What We Should Eat
The recommended daily caloric intake depends on an individual’s age, gender, and level of physical activity.3 Weight gain occurs when more calories are consumed than expended. Healthy weight loss can be achieved with a daily caloric intake of 1,200–1,500 for women and 1,500–1,800 for men.4 The U.S. Departments of Health and Human Services (DHHS) and Agriculture (USDA) have released the Dietary Guidelines for 2015 to 2020.4 This plan encourages a diet rich in nutrients while limiting calories from added sugars, saturated and trans fats, and sodium.5 Added sugars and saturated fats should each contribute less than 10% of the daily caloric intake.5 The American Heart Association recommends that women consume less than 6 teaspoons of sugar daily and men consume less than 9 teaspoons of sugar daily.3 Finally, the recommended daily sodium intake should be less than 2,300 mg.5
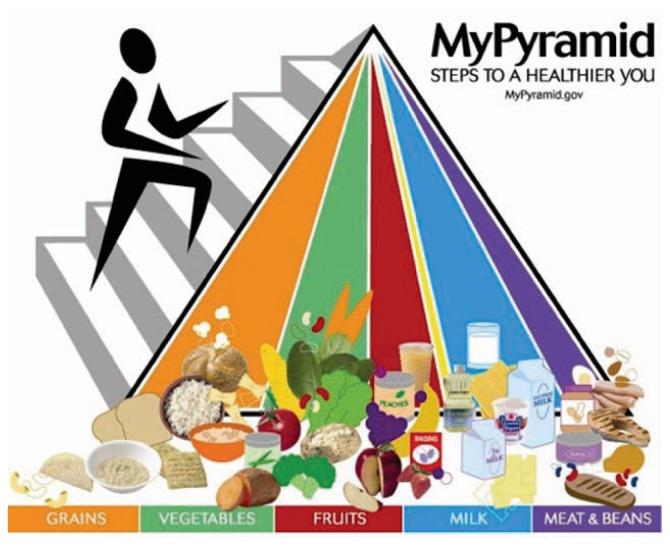
A healthy diet should include foods such as fruits, vegetables, whole grains, and fat-free or low-fat dairy (Figure 1).4 A 2,000 calorie diet should consist of 2.5 cups of vegetables and 2 cups of fruit daily. Protein can be obtained from seafood, lean meat, chicken, legumes, and nuts. Whole grains such as brown rice, quinoa, and oats are also suggested. The USDA dietary guidelines recommend adults consume three cups of non-fat or low-fat dairy per day.4 Eating a healthy diet not only results in weight loss, it can decrease the risk of cardiovascular disease.
Figure 1.
USDA My Pyramid
2005: MyPyramid Food Guidance System; U.S. Department of Agriculture.
ChooseMyPlate https://www.choosemyplate.gov/eathealthy/brief-history-usda-food-guides
The DASH diet is a well-known diet that encourages more fruits and vegetables.6 It avoids foods high in sodium, fats, and sugars. In fact, the Dietary Approaches to Stop Hypertension study found that a diet low in fat and rich in fruits, vegetables, and low-fat dairy resulted in lower systolic and diastolic blood pressures when compared to a standard western diet.6
What is the Western “American” Diet?
The typical Western (American) diet is low in fruits and vegetables, and high in fat and sodium. Moreover, this diet consists of large portions, high calories, and excess sugar.3 This excess sugar accounts for more than 13% of the daily caloric intake with beverages constituting 47% of these added sugars.4 Other sources include cookies, cakes, and candy.
Although fruits and vegetables contain natural sugars, they provide nutrients such as vitamins, minerals, and antioxidants while added sugars only contribute calories.3 The western diet is also noted to be high in saturated and trans fats. These fats not only contribute more calories; they increase low-density lipoproteins leading to atherosclerosis.
There has recently been increasing interest in the effect of dietary patterns on the immune system. One study compared mice that were fed a western diet to mice that were fed a standard fiber-rich diet.7 The western diet consisted of foods high in fats and sugars and low in fiber. These mice were found to have higher levels of inflammation and sepsis resulting in worse outcomes.7
The True Cost of Obesity and the Western Diet
Individuals who are obese or overweight are at a higher risk of developing chronic illnesses such as type 2 diabetes, cardiovascular disease, hypertension, hyperlipidemia, sleep apnea, or cancer. In fact, half of all Americans have a preventable chronic illness.3 According to the American Heart Association, 81 million American adults have cardiovascular disease which includes coronary artery disease or cerebrovascular disease. One-third of American adults have hypertension and more than 85% of patients with type 2 diabetes are considered overweight.3
Type 2 diabetes mellitus, once a disease primarily seen in adults, now presents in younger generations as a result of increasing childhood and adolescent obesity. According to the CDC, 13.7 million children and adolescents are considered obese in the United States.8
Multiple studies have also shown that obesity during midlife increases the risk of developing dementia. With fifty million people affected by dementia worldwide, there has been great interest in identifying preventable risk factors.9 A recent study evaluated the effect of diet modification and weight loss in elderly obese patients with mild cognitive impairment. These patients reduced their caloric intake and consumed more fruits, vegetables, fibers, and whole grains. The findings proved that weight reduction through diet modification improves cognition with these individuals showing improvements in verbal memory, verbal fluency, executive function and global cognition.9
Reproductive studies have reported that the increase in obesity rate has had a significant effect on fertility as well. More than 20% of reproductive-age women in the United States are considered obese.10 Pathophysiology of the infertility processes have shown that obesity affects the hypothalamic-pituitary-ovarian axis by suppressing gonadotropin release. This leads to anovulation and infertility.10
Polycystic Ovarian Syndrome, another common endocrine condition which increases a woman’s risk for infertility, is also associated with obesity. Studies have shown that modifying diets to include healthy and nutritious foods results in improved fertility.10
Interestingly, there have been reviews describing the benefit of healthy eating patterns on male fertility as well.11 Studies from several countries have shown that diets consisting of fruits, vegetables, seafood, chicken, and whole grains are associated with better semen quality while consumption of high amounts of trans and saturated fats were linked to poor semen quality.11
The Current Crisis: COVID-19 and Obesity
With the current COVID-19 pandemic, there are multiple studies showing associations between illness severity and obesity. A study done in New York City found patients with a BMI of 30–34 were 1.8 times more likely to be admitted to an intensive care unit.12 Those with a BMI greater than 35 were 3.6 times more likely to be admitted to an ICU. A corresponding report from France found that the use of mechanical ventilation was seven-fold higher for patients with a BMI greater than 35 compared to patients with a BMI of less than 25.12
Hypotheses to explain these findings include a link between obesity and hypoventilation syndrome and obstructive sleep apnea. Prior studies have also shown higher levels of inflammatory markers in obese patients. Moreover, COVID-19 has been associated with venous thrombosis. There is now grave concern for obese patients affected by this virus given the increased risk of thrombosis already seen in these patients.12
The new healthcare crisis with the COVID-19 pandemic has changed the way of living for many Americans. Most people are now working from home, and unfortunately many others are now unemployed. This has also appeared to have a significant effect on dietary patterns as well. Healthcare providers are now observing that patients are consuming more than they did prior to the lockdown. This, combined with limited physical activity due to stay-at-home orders is resulting in weight gain. With many individuals now unemployed, the issue of food insecurity has also been brought to the forefront. With limited access to healthy foods already a challenge for a large proportion of the United States’ population, the current economic and health crisis is expected to unfortunately increase the prevalence of obesity.
Conclusion
The western diet has been a significant contributor to the growing rate of obesity over the last several decades. Individuals who are overweight or obese have a higher chance of developing comorbidities such as diabetes, cardiovascular disease, and cancer. Although obesity is a significant risk factor, it is preventable and can be improved with changes in diet. We now see a link between obesity and COVID-19 illness severity which again emphasizes the importance of such interventions during the time of the pandemic. There are various types of diets that all promise weight loss. However, by avoiding certain foods that are popular in the American diet and including healthier options such as those recommended by the USDA, we can significantly reduce the rate of obesity and its long-term complications.
Footnotes
Varundeep Rakhra, DO, is an Endocrinology Fellow at the University of Missouri-Kansas City Endocrinology Fellowship program. Suguni Loku Galappaththy, MD, MSMA member since 2020, and Sheetal Bulchandani, MD, MSMA member since 2020, are Internal Medicine Residents at the University of Missouri-Kansas City. Peminda Cabandugama, MD, (left), is an Assistant Professor of Medicine and Faculty Member of the Endocrinology Fellowship Program at University of the Missouri-Kansas City, Kansas City, Missouri.
Disclosure
None reported.
References
- 1.World Health Organization. Obesity and Overweight. Apr, 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 2.Centers for Disease Control and Prevention. Overweight & Obesity. Jun, 2020. https://www.cdc.gov/obesity/data/adult.html.
- 3.Wartella EA, Lichtenstein AH, Boon CS, editors. Institute of Medicine (US) Committee on Examination of Front-of-Package Nutrition Rating Systems and Symbols. Front-of-Package Nutrition Rating Systems and Symbols: Phase I Report. Washington (DC): National Academies Press (US); 2010. p. 4. Overview of Health and Diet in America. [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services. US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th edition. Dec, 2015. [Google Scholar]
- 5.DeSalvo KB, Olson R, Casavale KO. Dietary Guidelines for Americans. Journal of American Medical Association. 2016;315(5):457–458. doi: 10.1001/jama.2015.18396. [DOI] [PubMed] [Google Scholar]
- 6.Appel LJ, Moore TJ, Obarzanek E, et al. A Clinical Trial of the Effects of Dietary Patterns on Blood Pressure. New England Journal of Medicine. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 7.Napier BA, Andres-Terre M, Massis LM, et al. Western Diet Regulates Immune Status and the Response to LPS-Driven Sepsis Independent of Diet Associated Microbiome. PNAS. 2019;116(9):3688–3694. doi: 10.1073/pnas.1814273116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Childhood Obesity Facts. Jun, 2019. https://www.cdc.gov/obesity/data/childhood.html.
- 9.Horie NH, Serrao VT, Simon SS, et al. Cognitive Effects of Intentional Weight Loss in Elderly Obese Individuals with Mild Cognitive Impairment. Journal of Clinical Endocrinology Metabolism. 2016;101(3):1104–1112. doi: 10.1210/jc.2015-2315. [DOI] [PubMed] [Google Scholar]
- 10.Broughton DE, Moley KH. Obesity and female infertility: Potential Mediators of Obesity’s Impact. Fertility and Sterility. 2017;107(4):840–847. doi: 10.1016/j.fertnstert.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Gaskins AJ, Chavarro JE. Diet and Fertility: A Review. American Journal of Obstetrics and Gynecology. 2018;218(4):379–389. doi: 10.1016/j.ajog.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sattar N, McInnes IB, McMurray JJV, et al. Obesity Is a Risk factor for Severe COVID-19 infection. Circulation. 2020;142:4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]