Abstract
The coronavirus disease 2019 (COVID-19) pandemic, resulting from infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused severe and widespread illness in adults, including pregnant women, while rarely infecting neonates. An incomplete understanding of disease pathogenesis and viral spread has resulted in evolving guidelines to reduce transmission from infected mothers to neonates. Fortunately, the risk of neonatal infection via perinatal/postnatal transmission is low when recommended precautions are followed. However, the psychosocial implications of these practices and racial/ethnic disparities highlighted by this pandemic must also be addressed when caring for mothers and their newborns. This review provides a comprehensive overview of neonatal–perinatal perspectives of COVID-19, ranging from the basic science of infection and recommendations for care of pregnant women and neonates to important psychosocial, ethical, and racial/ethnic topics emerging as a result of both the pandemic and the response of the healthcare community to the care of infected individuals.
Subject terms: Medical ethics, Paediatrics, Infection, Viral infection
Introduction
The COVID-19 pandemic has led to significant changes in healthcare delivery and clinical management of pregnant women and their newborns as the availability of healthcare resources, rates of infection, and scientific data continue to evolve. This review provides a summary of the current global literature and professional society recommendations for the management of pregnant women and neonates. Critical gaps in the literature remain, and important areas for future research are identified. The authors performed an extensive literature review of peer-reviewed publications within PubMed and also included published professional society recommendations (last updated on 7/31/20). The topics covered include the virology of SARS-CoV-2 infection, a summary of the current data on the epidemiology, diagnosis, outcomes, and management recommendations of SARS-CoV-2 related to pregnant women and newborns, as well as emerging psychosocial, ethical, and racial/ethnic considerations. This review discusses pertinent topics across numerous disciplines to provide a broad understanding critical to tackling the complex landscape of the COVID-19 pandemic from a neonatal–perinatal perspective.
Basic science of SARS-CoV-2 infection
Origins of SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of the global coronavirus disease 2019 (COVID-19) pandemic, is a member of the Coronaviridae family, initially discovered in the 1960s as the agent responsible for the common cold [1–3]. Since their initial discovery, seven unique coronaviruses have been implicated in clinically relevant infections, with three of the seven (severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus, and SARS-CoV-2) having the capacity to cause severe respiratory illness with significant morbidity and mortality. The Coronaviridae family consists of hundreds of additional viruses that utilize bats as a central reservoir of infection [4, 5]. Zoonotic transmission occurs after the virus undergoes genetic mutations that enable it to infect human cells. In the case of SARS-CoV-2, the receptor-binding domain (RBD) of the coronavirus spike protein located on the viral capsid evolved to enable binding to the human cell-surface protein angiotensin-converting enzyme 2 (ACE2) and initiate viral entry [2, 6]. Phylogenetic analysis of the RBDs of different coronaviruses suggests that SARS-CoV-2 likely originated in bats and that the pangolin was possibly an intermediate host, although further studies are needed to determine the definitive origin [2, 7, 8].
Viral cell entry
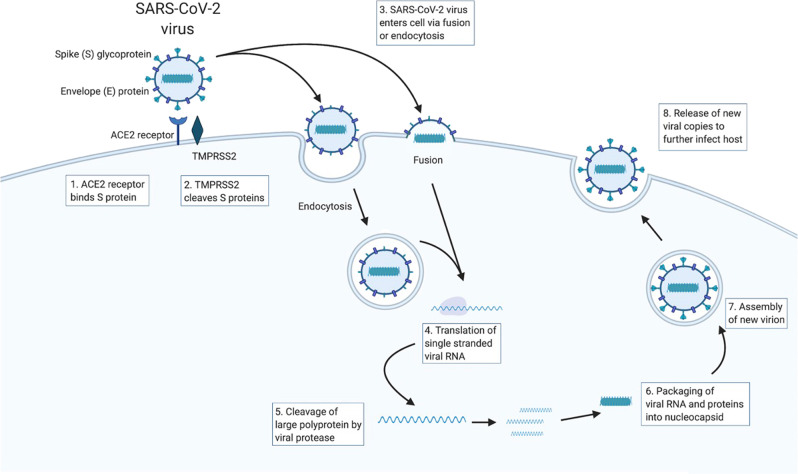
The expression of ACE2 on the epithelial surface of the upper and lower airways permits viral entry into these cells and underlies the ability of SARS-CoV-2 to cause respiratory illness [9–11]. Upon binding to ACE2, the SARS-CoV-2 life cycle requires the proteolytic activity of a host serine protease, Transmembrane protease, serine 2 (TMPRSS2), for viral entry (Fig. 1) [12, 13]. SARS-CoV-2 then gains access to the cytoplasm of the cell either through endocytosis or direct fusion with the host cell membrane [13]. Given that coronaviruses are positive, single-stranded RNA viruses, the viral RNA that enters the cytoplasm can directly be translated by the host protein-synthesis machinery. Translation results in the creation of a large polyprotein that is cleaved by a virally encoded protease to yield individual viral proteins [14]. Subsequent viral replication also requires a virally encoded protein, the RNA-dependent RNA polymerase, to synthesize the RNA intermediaries needed to make more SARS-CoV-2-positive-stranded RNA. Finally, viral proteins and newly synthesized viral RNA are packaged into a complete nucleocapsid that can be released from the cell to propagate infection [15]. The synthesized viral proteins and the host proteins that enable entry into the host cell (ACE2 and TMPRSS2), have been suggested as possible pharmacologic targets.
Fig. 1. SARS-CoV-2 viral entry and replication in host.
The spike (S) glycoproteins of the SARS-CoV-2 virus bind to the ACE2 receptor on the host cell. (2) The TMPRSS2 protein cleaves the S proteins off the viral envelope, (3) allowing for viral entry either by endocytosis or fusion. (4) Single-stranded viral RNA is replicated by host machinery into a large polyprotein. (5) The polyprotein is then cleaved by a viral protease. (6) Viral protein and RNA is then packaged into a nucleocapsid. (7) New virions are assembled and (8) released to further infect the host [12–15].
Immune response and pathogenesis in neonates, children, and nonpregnant adults
After viral entry into the host cell, it is hypothesized that initial viral recognition and immune activation occurs via Toll-like receptors, Retinoic acid-inducible gene I-like receptors, and inflammasome activation [16, 17]. The host immune response to viral infection has been implicated in causing the pathology and clinical illness seen in SARS-CoV-2 infection, with an overly robust immune response causing more severe illness. A comparison of the inflammatory response between adult survivors and non-survivors of SARS-CoV-2 infection from Wuhan, China, demonstrated significantly higher levels of IL-6, ferritin, and lactate dehydrogenase, as well as significantly lower lymphocyte counts both on admission and throughout hospitalization [18]. Similarly, another study of adults with SARS-CoV-2 from Wuhan, China found higher levels of an array of plasma proinflammatory cytokines (IL-2, IL-7, IL-10, GSCF, IP10, MCP1, MIP1A, and TNFα) in SARS-CoV-2 infected patients who required admission to the intensive care unit (ICU) compared to those who did not need the ICU [19].
The etiology of reduced infection rates and the dampened immune response to infection seen in neonates and older children has been the subject of much debate and currently remains unclear [20–22]. Possible explanations include variations in the expression pattern of ACE2 with aging and the evolution of the immune system and response to infection that occurs with development [23, 24].
Obstetrical considerations in the era of COVID-19
Epidemiology in pregnant women
Pregnancy increases the risk of certain infections, particularly respiratory infections [25, 26].
Rates of infection with SARS-CoV-2 in pregnant women vary geographically and likely reflect the prevalence of the virus in the overall population. For example, data from a single center in New York City show that 20% of 161 pregnant women tested positive for SARS-CoV-2 with an asymptomatic carrier rate of 13% [27]. In contrast, a similar study performed in Connecticut found that 3.9% of pregnant women were positive for SARS-CoV-2 with an asymptomatic carrier rate of 2.9% at time of admission to labor and delivery (in addition to the 1.5% of known infections at time of admission) [28]. Regarding illness severity, data from the Centers for Disease Control (CDC) suggest that pregnant women with COVID-19 are at increased risk for hospitalization and admission to the ICU compared to nonpregnant women of reproductive age [29].
Several studies have demonstrated fetal complications of maternal SARS-CoV-2 infection including medically indicated preterm birth, growth restriction, and miscarriage [26, 30]. Given the hypercoagulability seen in patients with COVID-19, these fetal complications are hypothesized to be due to compromised perfusion in the maternal and/or fetal placental vasculature and possible thrombotic changes [31, 32]. More studies are needed to clarify the impact of SARS-CoV-2 infection on the physiology of pregnancy, the placenta, and resultant fetal complications.
Antenatal management
Based on recommendations from The American College of Obstetricians and Gynecologists (ACOG), prenatal care does not require significant modification based on the presence of SARS-CoV-2 infection alone and should be based on the clinical condition of the pregnant woman [33–35]. In the event that there is a suspected or confirmed SARS-CoV-2 infection in the first trimester, ACOG suggests an additional mid-trimester ultrasound be considered to evaluate fetal anatomy [33]. If infection occurs in the second or third trimester, ACOG guidelines recommend that an additional third-trimester growth assessment can be performed [33]. These recommendations will likely continue to evolve as the impact of SAR-CoV-2 on the developing fetus is better understood.
Use of antenatal corticosteroids in COVID-19
ACOG guidelines currently recommend a course of antenatal steroids for all pregnant women at risk for preterm delivery within 7 days with fetuses <33 6/7 weeks’ gestational age, as well as for late preterm pregnancies 34 0/7 to 36 6/7 weeks’ gestational age with no prior course of steroids administered [36]. Earlier in the pandemic, ACOG recommended against the use of antenatal corticosteroids at or beyond 34 weeks’ gestation, given concerns at the time about the safety of corticosteroids in patients with SARS-CoV-2. These recommendations have since changed in response to new data supporting the possible benefit of treatment with corticosteroids in patients with COVID-19 [33, 37–39]. Specifically, a recent report showed that use of dexamethasone led to a lower 28-day mortality rate in hospitalized patients with COVID-19 who were mechanically ventilated or receiving oxygen [37]. At this time, ACOG guidance recommends that SARS-CoV-2 status should not alter decision-making regarding antenatal corticosteroid administration [33, 36].
Delivery considerations
The experience of labor and delivery has undoubtedly been altered by COVID-19 with numerous measures in place to protect the safety of pregnant women, caregivers, and newborns. ACOG currently recommends prioritization of testing for pregnant women admitted to labor and delivery units with suspected COVID-19 or who develop symptoms of COVID-19 during admission. Additionally, they suggest consideration of universal screening, utilizing rapid polymerase chain reaction (PCR) testing, in high prevalence areas, given concern for asymptomatic infection and transmission [33]. Other general precautions include limiting visitors and isolating persons under investigation (PUIs) or SARS-CoV-2-positive patients in negative pressure rooms, or at least rooms with high-efficiency particulate absorbing units, if negative pressure rooms are unavailable [33, 40].
ACOG recommendations state that SARS-CoV-2 infection alone is not an indication for preterm delivery or cesarean section, and timing of delivery should be informed by disease severity, maternal comorbidities, gestational age, and maternal and fetal status, as the majority of SARS-CoV-2 infections are asymptomatic or mild (defined as symptomatic with stable vital signs) and most individuals make a complete recovery [33, 34, 41]. For pregnant women who require inpatient management, regular monitoring of maternal vitals, and fetal heart rate for assessment of illness severity and fetal distress can assist in determination of delivery timing [41]. In severe illness (respiratory rate ≥30/min, resting SaO2 ≤ 93%, arterial blood oxygen partial pressure (PaO2)/oxygen concentration (FiO2) ≤300 mmHg), or critical illness (respiratory failure requiring mechanical ventilation, shock with organ failure, or refractory hypoxemia necessitating extracorporeal membrane oxygenation), delivery of the premature infant or termination of a nonviable pregnancy may need to be considered to reduce risk of maternal and fetal death [41].
Early delivery may also be warranted in refractory cases of maternal hypoxemia and increased maternal oxygen consumption due to the resultant critical fetal hypoxemia and acidemia. In these cases, the risks of prematurity are balanced against the risk of continued fetal compromise if the pregnancy were to continue [40], similar to the routine management of other conditions during pregnancy that improve after delivery. A review of 51 cases of SARS-CoV-2 infection in pregnant women reported an increase in medically indicated preterm birth and cesarean delivery. In this study, 96% of deliveries occurred by cesarean delivery and the median gestational age was 36.5 weeks’ gestation with delivery indications (available in 34 cases) reported as COVID-19 pneumonia (55.9%), premature rupture of membranes (26.5%), and fetal distress (17.6%). The authors hypothesized that provider and patient anxiety may have influenced this high cesarean delivery rate [42]. More data are needed to determine the impact of COVID-19 on medically indicated preterm birth and delivery.
Neonatal acquisition, outcomes, diagnosis, and management
Neonatal acquisition
Data indicate low rates of perinatal acquisition among neonates born to mothers positive for SARS-CoV-2. In a review of 27 studies, including data from the United States, China, Italy, Sweden, South Korea, and Honduras, only 4 out of 137 neonates (3%) born to SARS-CoV-2 infected mothers had positive viral PCR testing, and 3 neonates had equivocal testing (5% total prevalence including equivocal tests) [43]. Similar prevalence was reported in a large population-based cohort in the United Kingdom, which found 12/265 (5%) positive neonates born to SARS-CoV-2 infected mothers [44]. In a Spanish cohort, perinatal acquisition occurred in 5/72 (6.9%) of exposed newborns born to SARS-CoV-2-positive mothers, with no difference found between vaginal and Cesarean births [45]. In contrast, data from the National Registry for Surveillance and Epidemiology of Perinatal COVID-19 Infection (NPC-19) found 44/2287 (1.9%) of viral tests to be positive in neonates born to mothers with confirmed SARS-CoV-2 infection [46].
Perinatal transmission of SARS-CoV-2 from mothers to their offspring may occur via the transplacental route, or through environmental exposure to aerosolized droplets of viral particles after birth. Some reports of potential transplacental transmission have shown the presence of anti-SARS-CoV-2 IgG and IgM serum antibodies in neonates born to mothers with SARS-CoV-2 infection; however, all infants in these studies subsequently had negative viral PCR testing [47, 48]. SARS-CoV-2 specific IgM antibodies in neonates may indicate in utero infection given that IgM does not cross the placenta, and positive IgG titers in neonates may reflect maternal or neonatal infection [48, 49]. A recent case report provided virological and pathological evidence of likely transplacental transmission of SARS-CoV-2; the neonate was born to a viremic mother who presented after birth with neurological manifestations and was subsequently found to also have viremia. Histological analysis of the placenta found signs of acute and chronic intervillous inflammation and real-time reverse transcription polymerase chain reaction (RT-PCR) on the placental tissue was positive for SARS-CoV-2 [50]. In other studies, the SARS-CoV-2 virus has been found in the analysis of placental samples, providing evidence of possible transplacental transmission, but contamination at time of delivery could not be excluded [51, 52].
Postnatal contact transmission via environmental contamination is also possible given that live SARS-CoV-2 virus has been isolated from urine and fecal samples [53]. The possibility of transmission via breastmilk is currently under investigation, as initial studies reported negative viral PCR results sent on breastmilk samples from infected mothers [48, 54–56]. Conversely, two recent studies of mother–newborn positive dyads have reported the presence of viral RNA in breastmilk, but it is unclear whether this was the route of transmission versus droplet or contact postnatal transmission [57, 58]. The implementation of infection control precautions in breastfeeding infants may reduce postnatal acquisition. Three New York City hospitals reported a series of 120 neonates born to SARS-CoV-2 infected mothers who all tested negative for the virus at 24 h of life, 5–7 days of life (N = 82 completed follow-up) and 14 days of life (N = 72 completed follow-up). In this cohort, 78% of infants were still breastfeeding at 5–7 days of life, and the study described use of precautions including hand hygiene, maternal use of a surgical mask during breastfeeding and skin-to-skin, and use of a closed isolette when infants were not being held or fed [59]. Risk factors for maternal transmission and neonatal acquisition are not fully elucidated, and it remains unclear if severity of maternal disease, timing of acquisition, gestational age at delivery, or delivery mode contribute to transmission and infection risk.
Neonatal presentations and outcomes
Clinical presentations of neonates infected with SARS-CoV-2 vary greatly, ranging from asymptomatic carriage to critical illness. A systematic review of SARS-CoV-2 infection in children and newborns included a total of 25 neonatal cases [60]. Neonates were most commonly tested due to a history of primary maternal infection (84%). Of the 25 cases, 20% were asymptomatic and a higher proportion of neonates were severely ill compared to children older than 1 month of age (12% vs. 2%). Among symptomatic neonates, the most common clinical presentation was respiratory distress (40%), with fever (32%) and feeding intolerance (24%) also described. Laboratory findings included elevated white blood cell count (20%), creatine phosphokinase (20%), liver enzymes (16%), and C-reactive protein and/or procalcitonin (12%) [60]. One case series included in this review [61] described two neonates who developed disseminated intravascular coagulation and one who suffered multi-organ dysfunction, the latter resulting in neonatal death. Both of these neonates tested negative after birth by nucleic acid amplification test [61].
There have also been reports of presumed postnatal acquisition of SARS-CoV-2 in term or late preterm infants who developed respiratory failure and were found to have ground glass opacities on chest radiography [62–64]. A case report of a 26-week preterm neonate described the new development of streaky infiltrates on chest radiography following acquisition of SARS-CoV-2 infection but had no changes in baseline respiratory support [65]. Additionally, the previously described neonate with confirmed transplacental transmission presented with neurological manifestations, including irritability, inflammatory findings in the cerebrospinal fluid, and white matter injury on brain MRI [50]. Together, these data suggest that neonates with SARS-CoV-2 infection range from asymptomatic to severely ill, with respiratory distress being the most common presentation. While studies are limited, neonates may be at higher risk of experiencing severe illness compared to older children, making them a vulnerable population.
Diagnosis and management
The current gold standard to diagnose SARS-CoV-2 infection is RT-PCR on respiratory specimens. The reliability of this test has been established [66]. However, in asymptomatic or mildly symptomatic patients, as is often the case for newborns and infants, the sensitivity of the assay may be reduced by potential false negatives [61]. Diagnosis via serological testing in neonates is particularly challenging given the transplacental transmission of maternal IgG, and that IgM assays are prone to false-positives and false-negatives, and therefore, while their presence might suggest a fetal response to in utero infection, they are not the gold standard for diagnosis of congenital infections. The presence of IgG and/or IgM antibodies does not clearly define whether infection occurred transplacentally or postnatally, but a rising IgG antibody titer on serial testing may be helpful to identify active infection [49].
Management of SARS-CoV-2 infection in neonates is largely supportive, including respiratory support, oxygen, fluid and electrolyte therapy, and empiric antibiotics if there is suspected bacterial co-infection. Remdesivir, an RNA-dependent inhibitor of RNA polymerase in coronaviruses, is approved for use via an emergency drug authorization by the Food and Drug Administration with no minimum age [67]. Though data for remdesivir are lacking in neonates with COVID-19, remdesivir has safely and effectively been used in Ebola trials in infants under 5 days of age [68]. Additionally, oral absorption is poor, so there is likely limited absorption in neonates from breastmilk of mothers who may be on the agent [69].
During the respiratory management of a suspected or confirmed case of neonatal COVID-19, the risk of aerosol generation and dispersion also depends on the proximity to the patient’s airway and the risk of dispersion of aerosolized droplets through interface leaks or respiratory circuits [70]. Presumably, the lower tidal volumes of neonates and infants compared to adults decrease dispersion [43]. At some institutions, all neonates on respiratory support greater than 2 L/min nasal cannula or those that may require an aerosol-generating procedure are placed on airborne, contact, and eye-shield precautions, however the evidence directing which procedures require these increased precautions is unclear [71].
Recommendations for the management of neonates at risk for COVID-19 infection
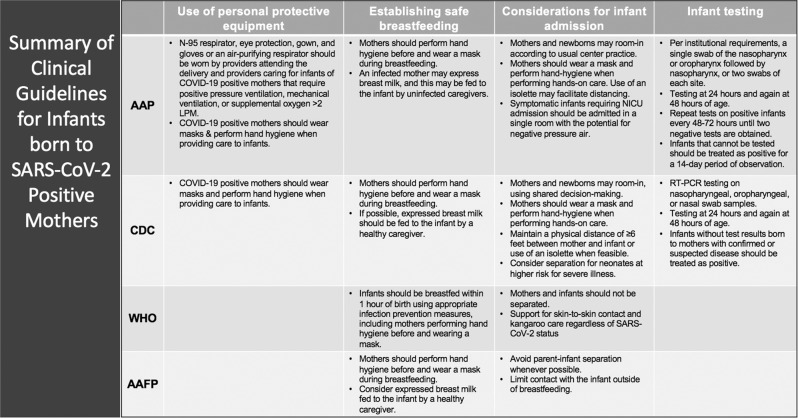
At the time of this review, several organizations, including the CDC, the World Health Organization (WHO), the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN), have provided guidelines for the management of neonates at risk for COVID-19. These guidelines are summarized in Fig. 2. While initial AAP guidelines at the onset of the COVID-19 pandemic recommended temporary separation of the mother and newborn as the risk of perinatal and postnatal transmission were not completely understood, this guidance has since changed. Based on data suggesting that the risk of infection is the same for infants who are temporarily separated from their mothers compared to those that room-in with their mothers, the AAP now recommends that mothers and newborns may room-in according to usual center practice [72]. The CDC continues to recommend temporary separation between SARS-CoV-2-positive or suspected mothers and newborns, defined by maintaining separate rooms, a physical distance of 6 feet or greater between the mother and newborn, or by placing the neonate in a temperature-controlled isolette if the newborn remains in the mother’s room [73]. With regard to rooming-in, both the AAP and CDC recommend barriers between mother and newborn to maintain 6 feet of distance when possible [72, 73]. The WHO does not currently recommend separation of mother and newborn, citing that physiological benefits of breastfeeding and skin-to-skin outweigh the likely limited risk of maternal to newborn transmission, especially in the context of the low virulence within the neonatal population [74]. The AAFP has similarly recommended promotion of breastfeeding and mother–newborn bonding and avoidance of separation of the mother and newborn whenever possible, although does suggest limiting contact between mothers infected with SARS-CoV-2 and their newborns when not directly breastfeeding [75]. Lastly, AWHONN has described the importance of shared decision-making as it relates to care of newborns born to SARS-CoV-2-positive mothers [76].
Fig. 2. Summary of clinical guidelines for care of infants born to SARS-CoV-2-positive mothers, updated as of July 22nd, 2020.
We provide a summary of the clinical guidelines from the American Academy of Pediatrics (AAP), Centers for Disease Control (CDC), World Health Organization (WHO), and American Academy of Family Physicians (AAFP) for care of infants born to SARS-CoV-2-positive mothers, updated as of July 22nd, 2020.
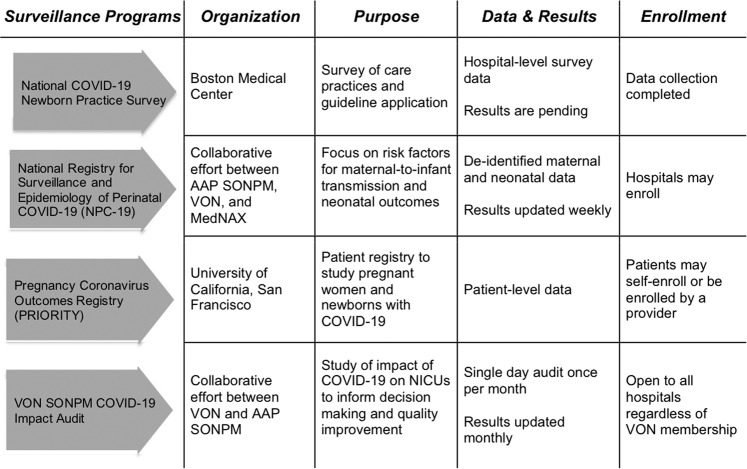
Practice surveillance and national registries
Extensive efforts are underway at hospital, state, and national levels to study the epidemiology and impact of SARS-CoV-2 infection on maternal and infant health and to fill gaps in the literature related to neonatal outcomes. National surveillance programs are summarized in Fig. 3. The National Registry for Surveillance and Epidemiology of Perinatal COVID-19 Infection (NPC-19) is a collaborative effort of the Section on Neonatal–Perinatal Medicine (SONPM) of the AAP, the Vermont Oxford Network (VON) and MedNAX, an organization of private neonatologists [46]. The NPC-19 is collecting data on mother–infant dyads with a goal to identify risk factors for neonatal transmission and outcomes. As of July 25, 2020 data have been collected from 231 centers and include 2067 mother–infant dyads [46, 77]. VON and the SONPM have also launched an audit with the goal of studying the impact of the pandemic on the neonatal community to inform decision-making and improve quality [77]. Additionally, the National COVID-19 Newborn Practice Survey, conducted by Boston Medical Center in May 2020, sought to ascertain the neonatal care practices related to COVID-19 at U.S. birth hospitals. Data collection from this survey has completed, and results are pending. Finally, the PRIORITY Study (Pregnancy Coronavirus Outcomes Registry) is being conducted by the University of California, San Francisco and is currently enrolling pregnant or recently pregnant women with known or suspected SARS-CoV-2 to study the impact of infection on pregnancy and newborns for 1 year following infection [78].
Fig. 3. National surveillance programs of newborns exposed to SARS-CoV-2 in the United States, as of July 31, 2020.
We provide a summary of national surveillance programs collecting data on newborns exposed to SARS-CoV-2 in the United States, as of July 2020.
Psychosocial, ethical, and racial/ethnic considerations in the care of newborns and families during the COVID-19 pandemic
One of the major ethical concerns that has emerged from the COVID-19 pandemic is the separation of mothers with suspected or confirmed SARS-CoV-2 from their newborns after delivery. Professional society guidance on this issue has been conflicting, as described previously. Reports in the media of hospitals unilaterally separating mothers from their newborns without discussions of risks and benefits with families have exacerbated parental fear and concerns.
The medical and psychosocial implications of separation after birth are undoubtedly significant. Separation has been hypothesized to interfere with the establishment of breastfeeding and lead to decreased bonding between a mother and her newborn, which may have long-term consequences [79]. Separation without adequate parental involvement in decision-making may result in a loss of trust in the healthcare system. The combination of these concerns has led some women to change their birthing plan due to their fear of separation from their newborn at birth, inability to have a primary support person during delivery, and fear of being infected with SARS-CoV-2 in the hospital [80]. Current data are lacking and further research is needed on the impact of these changes, but there is the potential for an increase in home births and increased demand for midwives and other personnel to attend home deliveries, which may not be able to be met by the current out-of-hospital-birthing system.
Many of the neonatal/perinatal ethical concerns discussed above relate to balancing parental decision-making rights while mitigating risks to newborns, maintaining public trust in the healthcare system, and issues of equity and bias. Parents are generally given decision-making rights for their children, thus, in the absence of serious harm for the newborn, parents are allowed to consent or decline separation after appropriate counseling [81]. Transparency from hospitals about the guidelines they follow, and how they will implement policies aligned with those guidelines is key to maintaining public trust during the pandemic [82].
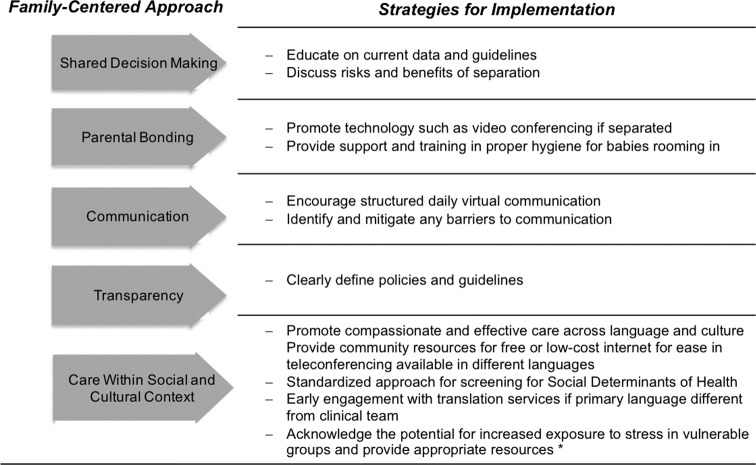
The long-term implications of COVID-19 in the neonatal and maternal populations are unknown, and stress and adversity experienced by families during the pandemic may have implications on health and well-being [83, 84]. Therefore, providers must continue to seek a balance for their patient’s safety and wellbeing. Figure 4 details existing recommendations for providing family-centered care, in order to ease parental distress in the face of possible family separation and other issues created by COVID-19 [82, 85].
Fig. 4.
Strategies for providing family-centered care for mothers and newborns during a pandemic [82, 85].
Finally, consideration of the ethical implications of neonatal care during the COVID-19 pandemic must include a discussion of disparities. Despite being a racial/ethnic minority of the general U.S. population, the non-White population has been disproportionately impacted by infection, severe disease manifestations, and death [86–90]. Data collected from the CDC suggest this is true specifically for Hispanic and non-Hispanic Black pregnant women [29]. Multiple mechanisms are responsible for these disparities, including the disproportionate burden of chronic medical conditions among Black and non-White Hispanic/Latinx adults in America, disparities in living conditions, residential segregation, inequitable access to food and healthcare systems, and environmental particulate pollution [86, 91]. Furthermore, the disproportionate representation of Black and non-White Hispanic and Latinx adults in “essential” jobs places communities of color in America at a disproportionate risk of infection [91]. There is a need to understand how bias in the healthcare system, long known to a be driver of disparities, impacts neonatal and perinatal outcomes during the pandemic [92, 93]. Vulnerable groups, including individuals in prisons, individuals with disabilities, individuals experiencing homelessness, immigrants, refugees, and asylum seekers are also disproportionately affected by the pandemic and need attention and ethical considerations [94–97]. Further research and longitudinal studies will be useful in addressing current gaps in understanding the long-term implications of COVID-19 on all populations, across the life course.
Conclusion
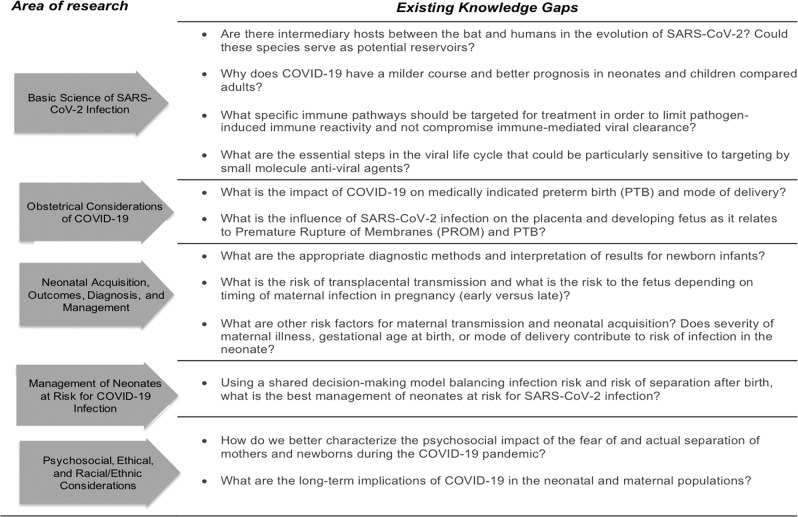
In this comprehensive review, we have presented an up-to-date summary of the literature on the management of the COVID-19 pandemic, with a focus on the care of pregnant women and newborns. Current data suggest the risk of neonatal transmission is low and that neonatal disease most commonly ranges from asymptomatic to mildly symptomatic. This has informed existing recommendations from professional societies for the management of these populations. These recommendations represent different perspectives and prioritization, taking into consideration factors including the current understanding of disease transmission and pathology, local infection rates, and existing resources. The COVID-19 pandemic has created an unprecedented challenge for the global healthcare system. Research efforts have mobilized rapidly, but many questions and knowledge gaps remain in our understanding of basic disease pathophysiology, epidemiology, and clinical manifestations of illness in pregnant women and neonates (Fig. 5). There remains a critical need for the adaptation of the healthcare system, as information is changing rapidly and the knowledge informing best practices in the care of pregnant women and newborns continues to evolve.
Fig. 5. Existing knowledge gaps related to neonatal–perinatal perspectives of COVID-19.
Current knowledge gaps in the literature related to neonatal–perinatal perspectives of COVID-19.
Acknowledgements
LCF, ARD, RMR, and AS’s work was supported by the National Institute of Child Health and Human Development of the National Institutes of Health under award number T32HD098061. KSB and YSF’s work was supported by AHRQ grant number T32HS000063 as part of the Harvard-wide Pediatric Health Services Research Fellowship Program. JCL’s work was supported by the National Library of Medicine of the National Institute of Health under grant number T15LM007092. PED’s work was supported by the National Heart Lung and Blood Institute, Program in Blood Coagulation and Vascular Biology, of the National Institutes of Health under award number T32HL007917-21.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–9. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tyrrell DA, Bynoe ML. Cultivation of viruses from a high proportion of patients with colds. Lancet. 1966;1:76–7. doi: 10.1016/s0140-6736(66)92364-6. [DOI] [PubMed] [Google Scholar]
- 4.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–92. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong ACP, Li X, Lau SKP, Woo PCY. Global epidemiology of Bat coronaviruses. Viruses. 2019;11:174. doi: 10.3390/v11020174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–9. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li X, Giorgi EE, Marichann MH, Foley B, Xiao C, Kong XP, et al. Emergence of SARS-CoV-2 through recombination and strong purifying selection. bioRxiv. Preprint ahead of print March 2020; 10.1101/2020.03.20.000885. [DOI] [PMC free article] [PubMed]
- 8.Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450–2. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9:45. doi: 10.1186/s40249-020-00662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM, Miao VN, Tzouanas CN, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181:1016–35 e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sungnak W, Huang N, Becavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681–7. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffmann M, Kleine-Weber H, Schroeder S, Kruger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–80. e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L, Lin D, Sun X, Curth U, Drosten C, Sauerhering L, et al. Crystal structure of SARS-CoV-2 main protease provides a basis for design of improved alpha-ketoamide inhibitors. Science. 2020;368:409–12. doi: 10.1126/science.abb3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–8. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park A, Iwasaki A. Type I and Type III interferons—induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020;27:870–8. doi: 10.1016/j.chom.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yap JKY, Moriyama M, Iwasaki A. Inflammasomes and pyroptosis as therapeutic targets for COVID-19. J Immunol. 2020;205:307–12.. doi: 10.4049/jimmunol.2000513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhochak N, Singhal T, Kabra SK, Lodha R. Pathophysiology of COVID-19: Why Children Fare Better than Adults? Indian J Pediatr. 2020;87:537–46.. doi: 10.1007/s12098-020-03322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carsetti R, Quintarelli C, Quinti I, Piano Mortari E, Zumla A, Ippolito G, et al. The immune system of children: the key to understanding SARS-CoV-2 susceptibility? Lancet Child Adolesc Health. 2020;4:414–6. doi: 10.1016/S2352-4642(20)30135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Molloy EJ, Bearer CF. COVID-19 in children and altered inflammatory responses. Pediatr Res. 2020;88:340–41. doi: 10.1038/s41390-020-0881-y. [DOI] [PubMed] [Google Scholar]
- 23.Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA. 2020;323:2427–29. doi: 10.1001/jama.2020.8707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song R, Preston G, Yosypiv IV. Ontogeny of angiotensin-converting enzyme 2. Pediatr Res. 2012;71:13–9. doi: 10.1038/pr.2011.7. [DOI] [PubMed] [Google Scholar]
- 25.Mor G, Cardenas I. The immune system in pregnancy: a unique complexity. Am J Reprod Immunol. 2010;63:425–33. doi: 10.1111/j.1600-0897.2010.00836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dashraath P, Wong JLJ, Lim MXK, Lim LM, Li S, Biswas A, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222:521–31. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vintzileos WS, Muscat J, Hoffmann E, John NS, Vertichio R, Vintzileos AM, et al. Screening all pregnant women admitted to labor and delivery for the virus responsible for coronavirus disease 2019. Am J Obstet Gynecol. 2020;223:284–6. doi: 10.1016/j.ajog.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campbell KH, Tornatore JM, Lawrence KE, Illuzzi JL, Sussman LS, Lipkind HS, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in Southern Connecticut. JAMA. 2020;323:2520–2. doi: 10.1001/jama.2020.8904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:769–75. doi: 10.15585/mmwr.mm6925a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sentilhes L, De Marcillac F, Jouffrieau C, Kuhn P, Thuet V, Hansmann Y, et al. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol. 2020;223:914.e1–914.e15. doi: 10.1016/j.ajog.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shanes ED, Mithal LB, Otero S, Azad HA, Miller ES, Goldstein JA Placental pathology in COVID-19. medRxiv. 2020; preprint ahead of print 12 May 2020; 10.1101/2020.05.08.20093229. [DOI] [PMC free article] [PubMed]
- 32.Baergen RN, Heller DS, Goldstein JA. Placental pathology in COVID-19. Am J Clin Pathol. 2020;154:279. doi: 10.1093/ajcp/aqaa101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.COVID-19 FAQs for Obstetrician-Gynecologists, Obstetrics: The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical-information/physician-faqs/covid-19-faqs-for-ob-gyns-obstetrics.
- 34.Stephens AJ, Barton JR, Bentum NA, Blackwell SC, Sibai BM. General guidelines in the management of an obstetrical patient on the labor and delivery unit during the COVID-19 pandemic. Am J Perinatol. 2020;37:829–36.. doi: 10.1055/s-0040-1710308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222:415–26. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Antenatal corticosteroid therapy for fetal maturation Committee Opinion No. 713. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2017;130:e102–9. doi: 10.1097/AOG.0000000000002237. [DOI] [PubMed] [Google Scholar]
- 37.Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19—Preliminary Report. N Engl J Med. 2020; epub ahead of print July 2020. 10.1056/NEJMoa2021436
- 38.COVID-19 Treatment Guidelines. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines.: National Institutes of Health; 2020. https://www.covid19treatmentguidelines.nih.gov/ [PubMed]
- 39.Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–87. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller E, Leffert L, Landau R. Society for maternal-fetal medicine and society for obstetric and anesthesia and perinatology labor and delivery COVID-19 considerations. Society for maternal fetal medicine society for obstetric anesthesia and perinatology. 2020;9:67–83. [Google Scholar]
- 41.Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. 2020;99:439–42. doi: 10.1111/aogs.13836. [DOI] [PubMed] [Google Scholar]
- 42.Della Gatta AN, Rizzo R, Pilu G, Simonazzi G. Coronavirus disease 2019 during pregnancy: a systematic review of reported cases. Am J Obstet Gynecol. 2020;223:36–41. doi: 10.1016/j.ajog.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shalish W, Lakshminrusimha S, Manzoni P, Keszler M, Sant’Anna GM. COVID-19 and neonatal respiratory care: current evidence and practical approach. Am J Perinatol. 2020;37:780–91. doi: 10.1055/s-0040-1710522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. doi: 10.1136/bmj.m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martinez-Perez O, Vouga M, Cruz Melguizo S, Forcen Acebal L, Panchaud A, Munoz-Chapuli M, et al. Association between mode of delivery among pregnant women with COVID-19 and maternal and neonatal outcomes in Spain. JAMA. 2020;324:296–9. doi: 10.1001/jama.2020.10125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.SONPM National Registry for Surveillance and Epidemiology of Perinatal COVID-19 Infection: Section on Neonatal-Pernatal Medicine. American Academy of Pediatrics. 2020. https://my.visme.co/view/ojq9qq8e-npc-19-registry.
- 47.Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323:1848–9. doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dong L, Tian J, He S, Zhu C, Wang J, Liu C, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846–8. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kimberlin DW, Stagno S. Can SARS-CoV-2 Infection Be Acquired In Utero?: More Definitive Evidence Is Needed. JAMA. 2020;323:1788–9. doi: 10.1001/jama.2020.4868. [DOI] [PubMed] [Google Scholar]
- 50.Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Do Cao J, et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020;11:3572. doi: 10.1038/s41467-020-17436-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Penfield CA, Brubaker SG, Limaye MA, Lighter J, Ratner AJ, Thomas KM, et al. Detection of SARS-COV-2 in placental and fetal membrane samples. Am J Obstet Gynecol MFM. 2020; e-pub ahead of print May 2020. 10.1016/j.ajogmf.2020.100133. [DOI] [PMC free article] [PubMed]
- 52.Patane L, Morotti D, Giunta MR, Sigismondi C, Piccoli MG, Frigerio L, et al. Vertical transmission of COVID-19: SARS-CoV-2 RNA on the fetal side of the placenta in pregnancies with COVID-19 positive mothers and neonates at birth. Am J Obstet Gynecol MFM. 2020; e-pub ahead of print May 2020. 10.1016/j.ajogmf.2020.100145. [DOI] [PMC free article] [PubMed]
- 53.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–4. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang S, Guo L, Chen L, Liu W, Cao Y, Zhang J, et al. A case report of neonatal 2019 coronavirus disease in China. Clin Infect Dis. 2020;71:853–7. doi: 10.1093/cid/ciaa225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–15. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, et al. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis. 2020; e-pub ahead of print March 2020; 10.1093/cid/ciaa226.
- 57.Gross R, Conzelmann C, Muller JA, Stenger S, Steinhart K, Kirchhoff F, et al. Detection of SARS-CoV-2 in human breastmilk. Lancet. 2020;395:1757–8. doi: 10.1016/S0140-6736(20)31181-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tam PCK, Ly KM, Kernich ML, Spurrier N, Lawrence D, Gordon DL, et al. Detectable severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in human breast milk of a mildly symptomatic patient with coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2020; e-pub ahead of print May 2020; 10.1093/cid/ciaa673. [DOI] [PMC free article] [PubMed]
- 59.Salvatore CM, Han JY, Acker KP, Tiwari P, Jin J, Brandler M, et al. Neonatal management and outcomes during the COVID-19 pandemic: an observation cohort study. Lancet Child Adolesc Health. 2020;4:721–7. doi: 10.1016/S2352-4642(20)30235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liguoro I, Pilotto C, Bonanni M, Ferrari ME, Pusiol A, Nocerino A, et al. SARS-COV-2 infection in children and newborns: a systematic review. Eur J Pediatr. 2020;179:1029–46.. doi: 10.1007/s00431-020-03684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020;9:51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sinelli MT, Paterlini G, Citterio M, Di Marco A, Fedeli T, Ventura ML Early neonatal SARS-CoV-2 infection manifesting with hypoxemia requiring respiratory support. Pediatrics. 2020; e-pub ahead of print May 2020. 10.1542/peds.2020-1121. [DOI] [PubMed]
- 63.Coronado Munoz A, Nawaratne U, McMann D, Ellsworth M, Meliones J, Boukas K. Late-onset neonatal sepsis in a patient with Covid-19. N Engl J Med. 2020;382:e49. doi: 10.1056/NEJMc2010614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Precit MR, Yee R, Anand V, Mongkolrattanothai K, Pandey U. Dien, et al. A case report of neonatal acute respiratory failure due to SARS-CoV-2. J Pediatric Infect Dis Soc. 2020;9:390–2. doi: 10.1093/jpids/piaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Piersigilli F, Carkeek K, Hocq C, van Grambezen B, Hubinont C, Chatzis O, et al. COVID-19 in a 26-week preterm neonate. Lancet Child Adolesc Health. 2020;4:476–8. doi: 10.1016/S2352-4642(20)30140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:1–8. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Coronavirus (COVID-19) Update: FDA Issues Emergency Use Authorization for Potential COVID-19 Treatment: U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment.
- 68.Mulangu S, Dodd LE, Davey RT, Jr., Tshiani Mbaya O, Proschan M, Mukadi D, et al. A randomized, controlled trial of Ebola Virus disease therapeutics. N Engl J Med. 2019;381:2293–303. doi: 10.1056/NEJMoa1910993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Remdesivir. In: Drugs and Lactation Database (LactMed). Bethesda (MD): National Library of Medicine (US). http://www.ncbi.nlm.nih.gov/books/NBK556881. Accessed 8 June 2020.
- 70.Chan MTV, Chow BK, Lo T, Ko FW, Ng SS, Gin T, et al. Exhaled air dispersion during bag-mask ventilation and sputum suctioning - Implications for infection control. Sci Rep. 2018;8:198. doi: 10.1038/s41598-017-18614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Verma S, Lumba R, Lighter JL, Bailey SM, Wachtel EV, Kunjumon B, et al. Neonatal intensive care unit preparedness for the Novel Coronavirus Disease-2019 pandemic: A New York City hospital perspective. Curr Probl Pediatr Adolesc Health Care. 2020;50:100795. doi: 10.1016/j.cppeds.2020.100795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.American Academcy of Pediatrics. FAQs: Management of Infants Born to Mothers with Suspected or Confirmed COVID-19. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/faqs-management-of-infants-born-to-covid-19-mothers/.
- 73.Centers for Disease Control and Prevention. Evaluation and Management Considerations for Neonates At Risk for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/caring-for-newborns.html.
- 74.Clinical managment of COVID-19: Interim guidance. World Health Organization. May 27, 2020. Report No.: WHO/2019-nCoV/clinical/2020.5.
- 75.AAFP Statement on Breastfeeding and COVID-19. The American Academy of Family Physicians. 2020. https://www.aafp.org/about/policies/all/breastfeeding-covid19.html
- 76.AWHONN COVID-19 Practice Guidance: Association of Women’s Health, Obstetric and Neonatal Nurses; [Available from: https://awhonn.org/novel-coronavirus-covid-19/covid19-practice-guidance/.
- 77.VON SONPM COVID-19 Impact Audit: Vermont Oxford Network. https://public.vtoxford.org/covid-19/.
- 78.PRIORITY: Pregnancy Coronavirus Outcomes Registry: University of California San Francisco. https://priority.ucsf.edu/.
- 79.Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016;11:CD003519. doi: 10.1002/14651858.CD003519.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Davis-Floyd R, Gutschow K, Schwartz DA. Pregnancy, birth and the COVID-19 Pandemic in the United States. Med Anthropol. 2020;39:413–27. doi: 10.1080/01459740.2020.1761804. [DOI] [PubMed] [Google Scholar]
- 81.Diekema DS. Parental refusals of medical treatment: the harm principle as threshold for state intervention. Theor Med Bioeth. 2004;25:243–64. doi: 10.1007/s11017-004-3146-6. [DOI] [PubMed] [Google Scholar]
- 82.Should New Mothers With Covid-19 Be Separated From Their Newborns?: The Hastings Center; 2020. https://www.thehastingscenter.org/why-new-mothers-with-covid-19-should-not-be-separated-from-their-newborns/.
- 83.Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of C, Family H, Committee on Early Childhood A, Dependent C. et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 84.Barrero-Castillero A, Morton SU, Nelson CA, 3rd, Smith VC. Psychosocial stress and adversity: effects from the perinatal period to adulthood. Neoreviews. 2019;20:e686–e96. doi: 10.1542/neo.20-12-e686. [DOI] [PubMed] [Google Scholar]
- 85.Hart JL, Turnbull AE, Oppenheim IM, Courtright KR. Family-centered care during the COVID-19 Era. J Pain Symptom Manage. 2020;60:e93–e97. doi: 10.1016/j.jpainsymman.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323:1891–2. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 87.Biggs HM, Harris JB, Breakwell L, Dahlgren FS, Abedi GR, Szablewski CM, et al. Estimated community seroprevalence of SARS-CoV-2 Antibodies—Two Georgia Counties, April 28-May 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:965–70. doi: 10.15585/mmwr.mm6929e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59:137–9. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N Engl J Med. 2020;382:2534–43. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Azar KMJ, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities in outcomes among COVID-19 patients in a large health care system In California. Health Aff. 2020;39:1253–62. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 91.Centers for Disease Control and Prevention. Health Equity Considerations and Racial and Ethnic Minority Groups. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fracial-ethnic-minorities.html.
- 92.Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: a Systematic Review. Am J Public Health. 2015;105:e60–76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96:826–33. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Okonkwo NE, Aguwa UT, Jang M, Barre IA, Page KR, Sullivan PS, et al. COVID-19 and the US response: accelerating health inequities. BMJ Evid Based Med. 2020, e-pub ahead of print June 2020. 10.1136/bmjebm-2020-111426. [DOI] [PMC free article] [PubMed]
- 95.Hawks L, Woolhandler S, McCormick D. COVID-19 in Prisons and Jails in the United States. JAMA Intern Med. 2020;180:1041–2. doi: 10.1001/jamainternmed.2020.1856. [DOI] [PubMed] [Google Scholar]
- 96.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5:e186–e7. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Page KR, Venkataramani M, Beyrer C, Polk S. Undocumented U.S. Immigrants and Covid-19. N Engl J Med. 2020;382:e62. doi: 10.1056/NEJMp2005953. [DOI] [PubMed] [Google Scholar]