Abstract
Transgender men remain at risk for gynecologic malignancies, but are an underserved population. Members of the transgender community experience discrimination and have experiences that contribute to health disparities, including in gynecology and oncology. While efforts have been made within the United States to reduce inequalities experienced by members of this community, many needs in the clinical setting remain. Increased education and training among providers and healthcare professionals, and general improvements towards understanding barriers to health screening and health resource uptake may reduce some disparities. Additional research towards screening and cancer surveillance among this community will be necessary to understand any potential additional risks and survival disparities experienced by transgender men. This review focuses on barriers and clinical needs for transgender men in the gynecologic oncology setting, and suggestions for moving forward to improve care for this patient population.
Introduction
Individuals who are transgender or gender non-conforming are becoming more visible in healthcare; however, they have frequently been met with discrimination and have experienced marginalization. Therefore, it is of no surprise that there are health disparities for patients who identify as transgender [1]. Transgender men are individuals who were assigned female at birth, but presently identify as male [2]. These patients experience gynecologic conditions as they are born with female pelvic organs. These conditions include gynecologic malignancies. As such, this review will focus on the needs of transgender men in the gynecologic oncology setting.
Understanding this patient population starts with gaining comprehension of the terminology used to describe these individuals. Breakdown of the important terminology regarding gender, gender identity, and other key definitions, has been well documented by the University of California San Francisco’s Lesbian, Gay, Bisexual and Transgender Resource Center, which serves as an excellent resource [3]. Additionally, it is important to distinguish the difference between gender dysphoria and transgender [2]. Being transgender is an identity and refers to identifying differently from one’s birth assignment, also known as biologic sex, whereas gender dysphoria is a symptom that can be associated with being transgender and occurs when an individual experiences severe psychological distress related to concerns associated with their gender identity.
A key issue previously identified is that, due to many barriers, the size of the transgender community within the United States, or globally, remains unknown [4]. Poor definitions of who in our populations belong to this community, and experienced discrimination and stigma resulting in individuals desiring to not be identified as a gender minority may contribute to this challenge. Until very recently, there has been a lack of acknowledgment and formal rights given to the LGBTQ+ community through legislation within the United States [5]. As there is continued societal growth and acknowledgment of the transgender population and existing hardships, there continues to be a need for improvements in knowledge and care in the clinical setting, providing comfort and respect to members of this community seeking medical services. As previously mentioned, transgender men, just like cisgender women, are at risk for gynecologic malignancies, and as such, it is critical that this specialty continues to work towards addressing the unique needs among this population.
Gender transitioning with pharmacologic/surgical interventions and common practices
Transition therapies are referred to as “gender-affirming” therapies and include medical therapy in the form of hormones as well as surgical procedures that help individuals align their bodies with their internal sense of self. Not all members of the transgender community will undergo pharmacologic or surgical intervention as each individual’s transition is unique [6]. Furthermore, choice to pursue certain surgical interventions also varies as some patients seek chest surgery while others seek both chest surgery and genital surgery. Patients may choose some transition at some point in their lives, but may opt for other therapies later as their goals change over time, with the understanding that some existing therapies are reversible and others are not [2, 7].
One factor that may affect choices around transition is access to care, as not all patients have adequate access. The consequences of insufficient access to therapies may have profound effects, with remarkably high rates of depression and suicidality reported in this population, with some patients resorting to taking street hormones with no medical monitoring [8].
Transgender men who choose to undergo gender affirming hormone therapy primarily transition with exogenous testosterone, which helps patients develop masculine physical features [2, 6, 9–11]. Extent of physical characteristics acquired through therapy are dependent on dosage and duration of use, with some characteristics including increased facial/body hair, vocal changes, changes in genital appearance, and possible interruption of menstruation [9]. Most patients on testosterone experience menstrual suppression, but not all do. For these patients, progesterone options and intrauterine devices may be utilized to help disrupt menstruation [6]. Estrogen-containing options are usually avoided. Among surgical interventions, transgender men may undergo mastectomy (chest reduction, chest masculinizing surgery, and “top” surgery), hysterectomy (with or without bilateral salpingo-oophorectomy), vaginectomy, and reconstructive surgeries to create external genitalia (metoidioplasty or phalloplasty, with or without urethral lengthening).
The extent to which one may undergo hormonal or surgical intervention is highly reliant on not only personal preferences, but also health care barriers [10, 12]. In fact, almost 25% of individuals identifying as transgender in one survey reported not having access to medical care for transition [10]. This includes the failure of most insurance providers to cover hormonal therapy, gender transition surgery, mental health services, as well as inadequate infrastructure for clinicians to code these therapies properly for reimbursement. As such, transgender men may still, and likely many will, have reproductive organs susceptible to gynecologic malignancies. Therefore, it is necessary to perform thorough organ inventories in patients seen for routine care, and to consider individualized health care planning when providing medical services for members of this community.
Discriminatory experiences and cancer-associated risk factors among the transgender community
Members of the LGBTQ+ community at large have historically experienced high levels of discrimination and violence, as well as greater rates of depression, anxiety, and suicide [4]. Until the landmark Supreme Court decision in June 2020, protections in the workplace against discrimination were non-existent, with employers holding the potential to terminate employees based on gender identity or sexual orientation, leading to higher levels of unemployment and poverty, homelessness, as well as poor access to health insurance coverage within this community [4, 5]. The aforementioned factors contribute to increased risks for negative health outcomes in some members of this community.
Patients from the transgender community appear to have higher rates of cancer-related risk factors [1, 13]. Members of this community, as well as other sexual and gender minority groups who have experienced violence or discrimination, have reported higher rates of cigarette/tobacco use and alcohol use including binge drinking [13]. These lifestyle factors are important to consider in transgender men, as cigarette/tobacco use has been associated with cervical neoplasia, vulvar neoplasia, and mucinous epithelial ovarian cancer [14–16].
Studies of transgender individuals have also identified engagement in sexual behaviors which place them at increased risk for cancer-associated human papillomavirus (HPV) strains, including: earlier age at first sexual intercourse, more partner experiences, and lower frequency of condom use during intercourse [13, 17]. Furthermore, a study including 91 transgender men identified that nearly 51% of participants hadn’t undergone a Pap smear for cervical cancer screening and HPV detection within 3 years preceding the survey [18]. Of these individuals, 32% reported never having received a Pap smear. Respondents had greater odds of not receiving screening reportedly due to costs, and fear of discrimination in the clinical setting. Participants of this survey expressed a preference for self-administered HPV testing, unless they had experienced this health screening in the past. Increasing efforts towards interventions such as HPV vaccination and screening among those at higher risk may be beneficial.
Considering the barriers to care experienced by these patients, it is essential to continue discussions on reducing the stigma of sexual and gender identities among the health care field, and the general population at large. These initiatives will aim to increase the comfort of these individuals in the clinical setting, increase the knowledge of specific needs among health care providers, and to reduce the potential violence and discrimination experienced by individuals from the transgender community.
Provider-related barriers for transgender men in the clinical setting
Studies have found that some members of the transgender community who do utilize health care services have been met with poor care from providers either through inadequate services offered, or through discriminatory behavior [4, 12, 19]. In the 2015 U.S. Transgender Survey, 33% of respondents reported negative experiences in the healthcare environment related to their gender identity [19]. Negative experiences included being refused transgender-related care (8%), being harassed verbally (6%), experiencing physical or sexual assault (4%), or having providers unfamiliar with transgender health (24%). Furthermore, transgender men in this survey reported higher frequencies of negative experiences in healthcare than transgender women.
Increasing education in the medical school and residency setting has been noted to enhance the comfort of future practicing clinicians in providing adequate and thorough care to members of this community [20, 21]. Of program directors in one survey, 96% of respondents felt it would be greatly beneficial to add education in this area to residency programs [22]. Implementing such training may improve disparities for patients in this population. There may be larger barriers for current practicing clinicians who have had minimal education regarding, and are reportedly less confident in, providing medical care for the transgender community [23–26]. In a recent survey of nearly 150 oncologists, 70% of these clinicians expressed a desire to receive education to better care for the distinct needs of members of sexual and gender minority groups, where only 20% of respondents felt confident in their knowledge for addressing the needs of the transgender community [25].
Addressing gynecologic oncology needs may produce additional discomfort for transgender men as the care is directly related to reproductive organs that play a role in the stigmatization of their gender identity [6]. Transgender men, as previously mentioned, may have a history of avoiding gynecologic care due to multiple factors [18, 27]. In one study based in Canada, 89 transgender men reported on experiences with gynecologic providers, as well as explanations for avoiding gynecologic care [27]. Among these participants, 70% reported concerns of having to provide education to their clinician regarding transgender health, and 86% reported fear of receiving a gynecologic exam. Normalizing diverse patient backgrounds and providing educational training for clinicians on gender and sexual minority care may alleviate some of these concerns.
One survey of gynecologists reported that 80% of providers had not received any training on caring for patients who are part of the transgender community [26]. When considering provider confidence in caring for transgender male patients, less than 30% of gynecologists felt comfortable with this role. Most of these providers reported being unaware of recommendations for cancer screening in this patient population. As noted by Obedin-Maliver and de Haan, provider education on caring for patients from the transgender community, including education on the use of gender-affirming language, or the use of gender-neutral pronouns, may provide a sense of comfort and acceptance for patients undergoing care for gynecologic conditions [6]. Furthermore, providers should receive education on these topics so they can become familiar with the use of hormones and surgical interventions for gender transition to facilitate better care for transgender patients and recommend or collaborate with providers with higher level of expertise.
Gynecologic oncology provokes emotional distress for many patients. Treatment may include aggressive surgery and intensive medical interventions with high recurrence rates among patients with ovarian cancer and other advanced malignancies. Additionally, there is potential genital physical disfigurement due to necessary surgical or radiation treatment among patients with some gynecologic malignancies, leading to alterations in physical appearance and sexual experiences, and this may add to the stress of seeking and undergoing care in this area among transgender men [28, 29]. Having stated previously that a large portion of transgender men will not have received reproductive surgery as it pertains to gender identity transition, the need for such intervention for gynecologic malignancies offers an opportunity for providers to acknowledge their patients’ different experiences as opposed to cisgender patients in their care. As previously documented by Taylor and Bryson, some patients may be emotionally taking in two separate experiences at once [29]. On the one hand, they are receiving cancer care, but on the other, they may be receiving what could be considered gender-affirming surgeries. Yet for some, cancer-related treatments impair the potential to continue their transition, with little information on the safety of hormone use in cancer patients for gender affirmation, and little information provided by gynecologic oncologists. These very different circumstances may yield conflicting emotional outcomes. The authors also note that the use of “women’s cancer” as a broader, general terminology may result in a sense of not belonging among transgender men seeking care for gynecologic conditions. Integrating education for providers in this specialty on the different psychosocial components of this care, as well as interventions for gender affirmation, could provide a significant impact on both quality of care and psychological outcomes for patients.
Gynecologic oncology risks in transgender men
There has been some effort in attempting to identify the prevalence of these malignancies among transgender men, but the evidence is severely limited [30, 31]. However, a full spectrum of gynecologic malignancies have been documented in transgender men [32–36]. At present, there is no documented increased risk of developing gynecologic malignancies secondary to hormone use among patients transitioning to gender-affirming identities, but this may be due to the limited available data [2, 7].
Testosterone therapy is often successful in inducing amenorrhea and increasing virilization, however there is a lack of long-term data on safety. Concern has been raised in the literature related to exogenous testosterone use and the potential mechanism of aromatization to estrogen, particularly in postmenopausal patients, possibly increasing the risk of hormonally-responsive cancers including type I endometrial cancer [31, 37, 38]. Based on the very limited available data, testosterone does not appear to increase endometrial hyperplasia in transmasculine pre or postmenopausal populations; some patients retain active endometrial tissue but in many cases testosterone induces atrophy similar to what is seen in cisgender female patients [39–41]. To date, only 1 case of endometrial cancer in a transgender male has been documented in the literature [32]. However, in pre-menopausal patients, many continue to have active endometrium while on testosterone therapy. In a multi-institution retrospective review of 94 patients on gender-affirming testosterone therapy who subsequently underwent hysterectomy, 64.9% had proliferative endometrium on pathologic examination, and 1 patient (1.2%) had endometrial hyperplasia without atypia, whereas only 24.5% had atrophic histopathology [40]. Given that additional hormone use with estrogen and/or progesterone is known to affect the endometrium, a subanalysis was conducted excluding patients on additional progesterone and/or estrogen therapy, and this revealed no significant difference in proliferative vs. atrophic endometrium (proliferative in 66.7%, atrophic in 27.2%, hyperplasia without atypia in 1.2%). Furthermore, the duration of testosterone therapy was not associated with endometrial proliferation status or thickness. Patients with a history of bleeding while taking testosterone did not significantly correlate with endometrial histology, duration of testosterone use, pre-operative testosterone levels, or BMI. Considering this data in addition to 4 additional publications on this topic, approximately 50% of patients have persistently active endometrium while on testosterone therapy [40–44]. As symptoms of bleeding, duration of hormone therapy and BMI were not related to persistence of endometrial proliferation or hyperplasia, it is not possible to determine how to most effectively evaluate risk; however, it is still important that providers review symptoms of concern such as irregular or postmenopausal bleeding with patients taking testosterone therapy.
Testosterone has also been hypothesized to contribute to ovarian carcinogenesis through its status as an estrogen precursor or androgen receptor signaling, and several cases of ovarian cancer in transgender men have been reported in the literature with one case documenting abundant androgen receptor expression in the well-differentiated endometrioid ovarian tumor [32–34]. Two cases from the Netherlands reported advanced papillary serous ovarian cancer in transgender male patients under 50 years of age [33]. Both had been treated with testosterone, one for many years. A nested case control study including 1,331 cases and 3,017 matched controls with ovarian cancer subtype data available demonstrated a slight increase in risk of endometrioid and mucinous ovarian cancer subtypes which correlated with higher serum levels of endogenous total and free testosterone, with hazard ratios ranging from 1.2–1.9 [45]. However, data from several other epidemiologic studies is conflicting and data on the effects of exogenous androgen administration on ovarian cancer risk is lacking [46–48]. Some advocate for bilateral salpingo-oophorectomy (BSO) at the time of hysterectomy in transgender men undergoing gender-conforming surgery; however this may not align with the goals of all transmasculine persons and should only be offered as an option [49]. Furthermore, BSO does not completely eliminate the risk for ovarian/primary peritoneal cancer in the cisgender female population, with an estimated risk reduction of 80% in cisgender females at high risk due to a known deleterious BRCA1/2 mutation and would also require lifelong testosterone supplementation or close monitoring for bone health [50–54].
Historically, hirsutism and high levels of androgens were associated with the development of polycystic ovarian syndrome (PCOS) [55]. Subsequent research has demonstrated the process to be more complex, with both genetic and environmental factors playing a role in ovarian hyperandrogenism, insulin resistance and a spectrum of additional clinical manifestations [56]. PCOS has been linked to higher risks of endometrial, ovarian, and other cancer types, particularly in pre-menopausal women in some population-based studies [57–59]. Therefore, plausible concern exists related to hyperandrogenemia among transgender men [60, 61]. Again, evidence is limited by small sample sizes and little available data. However, recent pathologic and morphologic studies of reproductive age of transgender men compared to control cisgender female patients demonstrate increased ovarian cortical thickness, ovarian stromal hyperplasia and luteinization, but no increase in ovarian PCO morphology [62–64]. To date, evidence shows overall conflicting data regarding PCOS and risks of gynecologic malignancies [57, 65, 66]. Currently, no specific guidelines exist in the endocrine or gynecologic societies outlining suggested surveillance for endometrial or ovarian cancers or other hormonally-sensitive malignancies in transgender men on gender-affirming hormone therapy. Generally, routine age-appropriate surveillance is recommended but additional data in this population is warranted to more fully evaluate risk and variations in presentation.
Additionally, as previously discussed, HPV-associated risk factors have historically been elevated within this community [1, 13]. Ensuring adequate surveillance for cervical, vulvar and other HPV-related conditions are important in patients who have retained these structures. HPV vaccination should be discussed and encouraged for transgender patients, just as it is for the general population. It is important to note that testosterone therapy induces atrophy in the tissues of the cervix, which results in frequent insufficient pap results [67]. Therefore, high-risk HPV (hrHPV) testing is important in this population given the unreliable cytology results. The American Cancer Society recently published updated recommendations utilizing primary hrHPV testing for cervical cancer screening, further supporting this practice; as some members of the transgender community may be at higher than average risk for HPV-related lesions, earlier initiation of HPV testing may be warranted, however there is insufficient data to guide initiation of hrHPV testing in this specific setting [68]. Many transgender men feel uncomfortable undergoing HPV screening procedures/exams, as it requires acknowledgement of retained female sexual organs in conflict with their gender identity, and, as mentioned previously, many face discrimination and/or lack of education during their provider visit. Transgender men are much less likely to be up to date with pap screening guidelines and many prefer primary HPV testing via self-sampling, which may improve the uptake of screening [18, 69–71]. One small prospective study comparing provider – collected vs. patient self-sampling of hrHPV swabs demonstrated 71.4% sensitivity and >98% specificity, with a strong preference among participants for self-sampling [72]. Larger studies and meta-analyses have demonstrated good sensitivity and concordance of self-sampling vs. provider sampling for hrHPV and high grade cervical lesions and may be suitable for those uncomfortable with clinical exams [73–75]. However, it should be discussed with patients that clinical exams may detect conditions or pre-malignant/malignant conditions which would not otherwise be detected by cytology or hrHPV testing alone, and clinical exams should still be encouraged.
Breast cancer risk, often considered part of gynecologic cancer care, should be considered and screening continued in those individuals who have not undergone mastectomy [76]. A recent study investigating the risks of breast cancer in transgender individuals utilizing hormone therapy found a decreased risk in transgender men compared with cisgender men and cisgender women, and a significantly increased risk of breast cancer in transgender women (usually ER/PR+) compared to cisgender men, but decreased risk when compared to cisgender women [77]. The study concluded that breast cancer screening guidelines used for cisgender individuals are sufficient for transgender people utilizing hormone therapy and is consistent with professional society guidelines. Transgender men who have undergone mastectomy no longer require mammograms, however there may still be value in regular self-breast exams as breast cancer has still been reported in this setting [78–81].
Taking these findings into consideration, cancer screening recommendations for transgender men are consistent with the general population, however more effort is needed to understand the prevalence, as well as cancer outcomes, in these patients [7, 82]. Cancer surveillance studies among the transgender population will be beneficial to identify specific clinical needs and potential needs for enhanced or earlier screening for gynecologic cancers. There is increased interest and research into quality of life considerations of patients undergoing cancer treatment in general, as patient-centered approaches are considered important aspects of cancer treatment and surveillance. Studies aimed at identifying quality of life outcomes and distress among transgender men with gynecologic cancers may guide education and interventions for providers to enhance a comforting and supportive experience for patients, as well as potential needs for mental health follow-up for patients within this community, as disparities in distress among transgender cancer patients have been previously identified [83].
Conclusions
Several barriers may influence the gynecologic oncology care for transgender men (Figure 1). Such barriers may include psychosocial components, experienced societal or provider-based discrimination, lack of access to adequate and appropriate care, and lack of provider education and comfort. With the recent Supreme Court ruling to protect members of the LGBTQ+ community in the workplace, there may be some alleviation of health disparities for members of the transgender community through improvements with employment and access to health insurance coverage. However, several barriers may remain which will require continued effort put towards researching and implementing interventions for both this community, as well as health care providers such as gynecologic oncologists, to improve long-term health outcomes in a patient population with extensive experiences of discrimination and neglect (Table 1). Further research is important to identify cancer risks and outcomes in this population to improve knowledge and guide recommendations regarding cancer surveillance, treatment, and quality of life outcomes in the transgender community.
Figure 1.
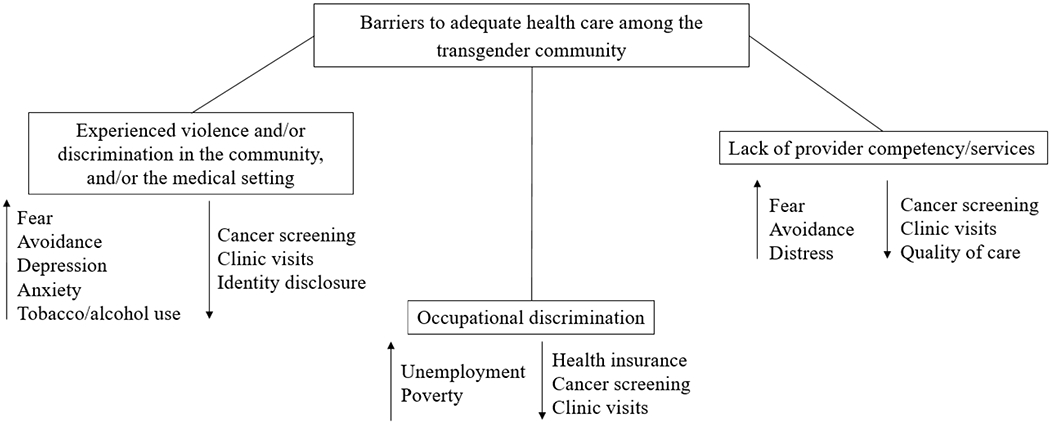
Barriers to adequate health care among the transgender community. Arrows pointing upwards indicate increased characteristics, whereas arrows in the downward direction indicate decreased characteristics.
Table 1.
Recommendations for overcoming provider-related barriers to improve quality of care and health outcomes for members of the transgender community*.
| Barrier | Recommendation |
|---|---|
| Underutilization of cancer preventive services and screening among the transgender community | Enhance community outreach efforts to develop relationships within this community, use of gender neutral pronouns and the invitation for patients to provide their own gender-affirming pronouns to increase clinical comfort, continue to promote cancer screening per general guidelines, increase research efforts towards home-based screening methods for alternative options (i.e. self-sampling for HPV testing) for those avoiding clinical examinations |
| Lack of training and education around gender and sexual minority health | Integrate education surrounding this topic early in the medical education curriculum, implement continuing education on this topic among currently practicing providers (education relating to, but not limited to: terminology and pronoun use, hormonal and surgical therapies before, during, and after cancer care, individualized needs among this population) |
| Disparities in cancer-related distress and patient outcomes | Recognize disparities in distress after a cancer diagnosis and potential unique needs for health resources among this community, and connect patients with providers specializing in these areas |
| Inconclusive evidence on level of risk for cancer incidence, as well as potential survival disparities | Enhance studies on cancer surveillance among this community to identify cancer prevalence, risk and survival disparities to direct future efforts towards mitigating these risks and reducing potential negative outcomes |
This list is not exhaustive but intended to provide insight on enhancing this area of care based on current evidence.
Highlights.
Members of the transgender community have experienced discrimination and rejection in the community and medical setting
Discriminatory experiences may lead to increased cancer-associated risk factors and decreased cancer screening
Transgender men remain at risk for gynecologic malignancies, but face barriers to adequate care
Increased provider education and outreach may improve the care for transgender men in gynecologic oncology
Acknowledgments
Funding: Work on this manuscript (AES) was supported by the National Cancer Institute NIH grant T32CA163184.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: Dr. Ferrando reports annual royalties from UpToDate on the subject of LGBTQ+ health.
References
- 1.Gibson AW, Radix AE, Maingi S, Patel S. Cancer care in lesbian, gay, bisexual, transgender and queer populations. Future Oncology 2017; 13: 1333–1344. [DOI] [PubMed] [Google Scholar]
- 2.Coleman E, Bockting W, Botzer M et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. International Journal of Transgenderism 2012; 13: 165–232. [Google Scholar]
- 3.University of California San Francisco. Terminology: Education & Training. In.
- 4.Winter S, Diamond M, Green J et al. Transgender people: health at the margins of society. The Lancet 2016; 388: 390–400. [DOI] [PubMed] [Google Scholar]
- 5.Liptak A Civil Rights Law Protects Gay and Transgender Workers, Supreme Court Rules. The New York Times 2020; 1. [Google Scholar]
- 6.Obedin-Maliver J, de Haan G. Gynecologic Care for Transgender Adults. Current Obstetrics and Gynecology Reports 2017; 6: 140–148. [Google Scholar]
- 7.Puechl AM, Russell K, Gray BA. Care and Cancer Screening of the Transgender Population. Journal of Women’s Health (15409996) 2019; 28: 761–768. [DOI] [PubMed] [Google Scholar]
- 8.Ray N Lesbian, gay, bisexual and transgender youth: An epidemic of homelessness. In. New York: National Gay and Lesbian Task Force Policy Institute and the National Coalition for the Homeless; 2006. [Google Scholar]
- 9.Unger CA. Hormone therapy for transgender patients. Translational andrology and urology 2016; 5: 877–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White Hughto JM, Rose AJ, Pachankis JE, Reisner SL. Barriers to Gender Transition-Related Healthcare: Identifying Underserved Transgender Adults in Massachusetts. Transgender Health 2017; 2: 107–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2009; 94: 3132–3154. [DOI] [PubMed] [Google Scholar]
- 12.Safer JD, Coleman E, Feldman J et al. Barriers to healthcare for transgender individuals. Current opinion in endocrinology, diabetes, and obesity 2016; 23: 168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosario M, Corliss HL, Everett BG et al. Mediation by Peer Violence Victimization of Sexual Orientation Disparities in Cancer-Related Tobacco, Alcohol, and Sexual Risk Behaviors: Pooled Youth Risk Behavior Surveys. American Journal of Public Health 2014; 104: 1113–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou A, Minlikeeva AN, Khan S, Moysich KB. Association between Cigarette Smoking and Histotype-Specific Epithelial Ovarian Cancer: A Review of Epidemiologic Studies. Cancer Epidemiology Biomarkers & Prevention 2019; 28: 1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gunnell AS, Tran TN, Torrång A et al. Synergy between Cigarette Smoking and Human Papillomavirus Type 16 in Cervical Cancer <em>In situ</em> Development. Cancer Epidemiology Biomarkers & Prevention 2006; 15: 2141. [DOI] [PubMed] [Google Scholar]
- 16.Brinton LA, Thistle JE, Liao LM, Trabert B. Epidemiology of vulvar neoplasia in the NIH-AARP Study. Gynecologic Oncology 2017; 145: 298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ceres M, Quinn GP, Loscalzo M, Rice D. Cancer Screening Considerations and Cancer Screening Uptake for Lesbian, Gay, Bisexual, and Transgender Persons. Seminars in Oncology Nursing 2018; 34: 37–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seay J, Ranck A, Weiss R et al. Understanding Transgender Men’s Experiences with and Preferences for Cervical Cancer Screening: A Rapid Assessment Survey. LGBT Health 2017; 4: 304–309. [DOI] [PubMed] [Google Scholar]
- 19.James SE HJ, Rankin S, Keisling M, Mottet L, Anafi M,. The Report of the 2015 U.S Transgender Survey. In. Washington D.C: National Center for Transgender Equality; 2016. [Google Scholar]
- 20.Thomas DD, Safer JD. A SIMPLE INTERVENTION RAISED RESIDENT-PHYSICIAN WILLINGNESS TO ASSIST TRANSGENDER PATIENTS SEEKING HORMONE THERAPY. Endocr Pract 2015; 21: 1134–1142. [DOI] [PubMed] [Google Scholar]
- 21.Safer JD, Pearce EN. A simple curriculum content change increased medical student comfort with transgender medicine. Endocr Pract 2013; 19: 633–637. [DOI] [PubMed] [Google Scholar]
- 22.Grimstad FW, Satterwhite CL, Wieneke CL. Assessing Residency Program Approaches to the Transgender Health CREOG Objective. Transgender Health 2016; 1: 69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Snelgrove JW, Jasudavisius AM, Rowe BW et al. “Completely out-at-sea” with “two-gender medicine”: a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res 2012; 12: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lurie S Identifying Training Needs of Health-Care Providers Related to Treatment and Care of Transgendered Patients: A Qualitative Needs Assessment Conducted in New England. International Journal of Transgenderism 2005; 8: 93–112. [Google Scholar]
- 25.Schabath MB, Blackburn CA, Sutter ME et al. National Survey of Oncologists at National Cancer Institute-Designated Comprehensive Cancer Centers: Attitudes, Knowledge, and Practice Behaviors About LGBTQ Patients With Cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2019; 37: 547–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unger CA. Care of the Transgender Patient: A Survey of Gynecologists’ Current Knowledge and Practice. Journal of Women’s Health 2014; 24: 114–118. [DOI] [PubMed] [Google Scholar]
- 27.Frecker H, Scheim A, Leonardi M, Yudin M. Experiences of Transgender Men in Accessing Care in Gynecology Clinics [24G]. Obstetrics & Gynecology 2018; 131. [Google Scholar]
- 28.Carpenter K AB. Psychological and sexual aspects of gynecologic cancer. Glob. libr. women’s med 2008; 1756–2228. [Google Scholar]
- 29.Taylor ET, Bryson MK. Cancer’s Margins: Trans* and Gender Nonconforming People’s Access to Knowledge, Experiences of Cancer Health, and Decision-Making. LGBT health 2016; 3: 79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Urban RR, Teng NNH, Kapp DS. Gynecologic malignancies in female-to-male transgender patients: the need of original gender surveillance. American Journal of Obstetrics and Gynecology 2011; 204: e9–e12. [DOI] [PubMed] [Google Scholar]
- 31.Mueller A, Gooren L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol 2008; 159: 197–202. [DOI] [PubMed] [Google Scholar]
- 32.Urban RR, Teng NN, Kapp DS. Gynecologic malignancies in female-to-male transgender patients: the need of original gender surveillance. Am J Obstet Gynecol 2011; 204: e9–e12. [DOI] [PubMed] [Google Scholar]
- 33.Hage JJ, Dekker JJ, Karim RB et al. Ovarian cancer in female-to-male transsexuals: report of two cases. Gynecol Oncol 2000; 76: 413–415. [DOI] [PubMed] [Google Scholar]
- 34.Dizon DS, Tejada-Berges T, Koelliker S et al. Ovarian cancer associated with testosterone supplementation in a female-to-male transsexual patient. Gynecol Obstet Invest 2006; 62: 226–228. [DOI] [PubMed] [Google Scholar]
- 35.Schenck TL, Holzbach T, Zantl N et al. Vaginal carcinoma in a female-to-male transsexual. J Sex Med 2010; 7: 2899–2902. [DOI] [PubMed] [Google Scholar]
- 36.Driák D, Samudovský M. Could a man be affected with carcinoma of cervix?--The first case of cervical carcinoma in trans-sexual person (FtM)--case report. Acta Medica (Hradec Kralove) 2005; 48: 53–55. [PubMed] [Google Scholar]
- 37.Gooren LJ. Clinical practice. Care of transsexual persons. N Engl J Med 2011; 364: 1251–1257. [DOI] [PubMed] [Google Scholar]
- 38.Clendenen TV, Hertzmark K, Koenig KL et al. Premenopausal Circulating Androgens and Risk of Endometrial Cancer: results of a Prospective Study. Horm Cancer 2016; 7: 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zang H, Sahlin L, Masironi B et al. Effects of testosterone treatment on endometrial proliferation in postmenopausal women. J Clin Endocrinol Metab 2007; 92: 2169–2175. [DOI] [PubMed] [Google Scholar]
- 40.Grimstad FW, Fowler KG, New EP et al. Uterine pathology in transmasculine persons on testosterone: a retrospective multicenter case series. Am J Obstet Gynecol 2019; 220: 257.e251–257.e257. [DOI] [PubMed] [Google Scholar]
- 41.Perrone AM, Cerpolini S, Maria Salfi NC et al. Effect of long-term testosterone administration on the endometrium of female-to-male (FtM) transsexuals. J Sex Med 2009; 6: 3193–3200. [DOI] [PubMed] [Google Scholar]
- 42.Grynberg M, Fanchin R, Dubost G et al. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod Biomed Online 2010; 20: 553–558. [DOI] [PubMed] [Google Scholar]
- 43.Loverro G, Resta L, Dellino M et al. Uterine and ovarian changes during testosterone administration in young female-to-male transsexuals. Taiwan J Obstet Gynecol 2016; 55: 686–691. [DOI] [PubMed] [Google Scholar]
- 44.Khalifa MA, Toyama A, Klein ME, Santiago V. Histologic Features of Hysterectomy Specimens From Female-Male Transgender Individuals. Int J Gynecol Pathol 2019; 38: 520–527. [DOI] [PubMed] [Google Scholar]
- 45.Ose J, Poole EM, Schock H et al. Androgens Are Differentially Associated with Ovarian Cancer Subtypes in the Ovarian Cancer Cohort Consortium. Cancer Res 2017; 77: 3951–3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tworoger SS, Lee IM, Buring JE, Hankinson SE. Plasma androgen concentrations and risk of incident ovarian cancer. Am J Epidemiol 2008; 167: 211–218. [DOI] [PubMed] [Google Scholar]
- 47.Rinaldi S, Dossus L, Lukanova A et al. Endogenous androgens and risk of epithelial ovarian cancer: results from the European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Epidemiol Biomarkers Prev 2007; 16: 23–29. [DOI] [PubMed] [Google Scholar]
- 48.Ose J, Fortner RT, Rinaldi S et al. Endogenous androgens and risk of epithelial invasive ovarian cancer by tumor characteristics in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 2015; 136: 399–410. [DOI] [PubMed] [Google Scholar]
- 49.Grimstad F, Boskey E. Empowering Transmasculine Youth by Enhancing Reproductive Health Counseling in the Primary Care Setting. J Adolesc Health 2020; 66: 653–655. [DOI] [PubMed] [Google Scholar]
- 50.Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst 2009; 101: 80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hembree WC, Cohen-Kettenis PT, Gooren L et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2017; 102: 3869–3903. [DOI] [PubMed] [Google Scholar]
- 52.Moravek MB. Gender-Affirming Hormone Therapy for Transgender Men. Clin Obstet Gynecol 2018; 61: 687–704. [DOI] [PubMed] [Google Scholar]
- 53.Lips P, van Kesteren PJ, Asscheman H, Gooren LJ. The effect of androgen treatment on bone metabolism in female-to-male transsexuals. J Bone Miner Res 1996; 11: 1769–1773. [DOI] [PubMed] [Google Scholar]
- 54.Van Caenegem E, Wierckx K, Taes Y et al. Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. J Clin Endocrinol Metab 2012; 97: 2503–2511. [DOI] [PubMed] [Google Scholar]
- 55.Futterweit W, Deligdisch L. Histopathological Effects of Exogenously Administered Testosterone in 19 Female to Male Transsexuals. The Journal of Clinical Endocrinology & Metabolism 1986; 62: 16–21. [DOI] [PubMed] [Google Scholar]
- 56.Rosenfield RL, Ehrmann DA. The Pathogenesis of Polycystic Ovary Syndrome (PCOS): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism Revisited. Endocr Rev 2016; 37: 467–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harris HR, Terry KL. Polycystic ovary syndrome and risk of endometrial, ovarian, and breast cancer: a systematic review. Fertility Research and Practice 2016; 2: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yin W, Falconer H, Yin L et al. Association Between Polycystic Ovary Syndrome and Cancer Risk. JAMA Oncol 2019; 5: 106–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update 2014; 20: 748–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Balen AH, Schachter ME, Montgomery D et al. Polycystic ovaries are a common finding in untreated female to male transsexuals. Clin Endocrinol (Oxf) 1993; 38: 325–329. [DOI] [PubMed] [Google Scholar]
- 61.Mueller A, Gooren LJ, Naton-Schötz S et al. Prevalence of polycystic ovary syndrome and hyperandrogenemia in female-to-male transsexuals. J Clin Endocrinol Metab 2008; 93: 1408–1411. [DOI] [PubMed] [Google Scholar]
- 62.Caanen MR, Schouten NE, Kuijper EAM et al. Effects of long-term exogenous testosterone administration on ovarian morphology, determined by transvaginal (3D) ultrasound in female-to-male transsexuals. Hum Reprod 2017; 32: 1457–1464. [DOI] [PubMed] [Google Scholar]
- 63.Ikeda K, Baba T, Noguchi H et al. Excessive androgen exposure in female-to-male transsexual persons of reproductive age induces hyperplasia of the ovarian cortex and stroma but not polycystic ovary morphology. Hum Reprod 2013; 28: 453–461. [DOI] [PubMed] [Google Scholar]
- 64.Grimstad FW, Fowler KG, New EP et al. Ovarian Histopathology in Transmasculine Persons on Testosterone: A Multicenter Case Series. J Sex Med 2020; 17: 1807–1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Harris HR, Babic A, Webb PM et al. Polycystic Ovary Syndrome, Oligomenorrhea, and Risk of Ovarian Cancer Histotypes: Evidence from the Ovarian Cancer Association Consortium. Cancer Epidemiology Biomarkers & Prevention 2018; 27: 174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dumesic DA, Lobo RA. Cancer risk and PCOS. Steroids 2013; 78: 782–785. [DOI] [PubMed] [Google Scholar]
- 67.Peitzmeier SM, Reisner SL, Harigopal P, Potter J. Female-to-male patients have high prevalence of unsatisfactory Paps compared to non-transgender females: implications for cervical cancer screening. J Gen Intern Med 2014; 29: 778–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fontham ETH, Wolf AMD, Church TR et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin 2020. [DOI] [PubMed] [Google Scholar]
- 69.Peitzmeier SM, Khullar K, Reisner SL, Potter J. Pap test use is lower among female-to-male patients than non-transgender women. Am J Prev Med 2014; 47: 808–812. [DOI] [PubMed] [Google Scholar]
- 70.Gatos KC. A Literature Review of Cervical Cancer Screening in Transgender Men. Nurs Womens Health 2018; 22: 52–62. [DOI] [PubMed] [Google Scholar]
- 71.McDowell M, Pardee DJ, Peitzmeier S et al. Cervical Cancer Screening Preferences Among Trans-Masculine Individuals: Patient-Collected Human Papillomavirus Vaginal Swabs Versus Provider-Administered Pap Tests. LGBT Health 2017; 4: 252–259. [DOI] [PubMed] [Google Scholar]
- 72.Reisner SL, Deutsch MB, Peitzmeier SM et al. Test performance and acceptability of self-versus provider-collected swabs for high-risk HPV DNA testing in female-to-male trans masculine patients. PLoS One 2018; 13: e0190172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Snijders PJ, Verhoef VM, Arbyn M et al. High-risk HPV testing on self-sampled versus clinician-collected specimens: a review on the clinical accuracy and impact on population attendance in cervical cancer screening. Int J Cancer 2013; 132: 2223–2236. [DOI] [PubMed] [Google Scholar]
- 74.Arbyn M, Verdoodt F, Snijders PJ et al. Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta-analysis. Lancet Oncol 2014; 15: 172–183. [DOI] [PubMed] [Google Scholar]
- 75.Zhao FH, Lewkowitz AK, Chen F et al. Pooled analysis of a self-sampling HPV DNA Test as a cervical cancer primary screening method. J Natl Cancer Inst 2012; 104: 178–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Committee Opinion no. 512: health care for transgender individuals. Obstet Gynecol 2011; 118: 1454–1458. [DOI] [PubMed] [Google Scholar]
- 77.de Blok CJM, Wiepjes CM, Nota NM et al. Breast cancer risk in transgender people receiving hormone treatment: nationwide cohort study in the Netherlands. Bmj 2019; 365: l1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gooren LJ, van Trotsenburg MA, Giltay EJ, van Diest PJ. Breast cancer development in transsexual subjects receiving cross-sex hormone treatment. J Sex Med 2013; 10: 3129–3134. [DOI] [PubMed] [Google Scholar]
- 79.Ganly I, Taylor EW. Breast cancer in a trans-sexual man receiving hormone replacement therapy. Br J Surg 1995; 82: 341. [DOI] [PubMed] [Google Scholar]
- 80.Burcombe RJ, Makris A, Pittam M, Finer N. Breast cancer after bilateral subcutaneous mastectomy in a female-to-male trans-sexual. Breast 2003; 12: 290–293. [DOI] [PubMed] [Google Scholar]
- 81.Nikolic DV, Djordjevic ML, Granic M et al. Importance of revealing a rare case of breast cancer in a female to male transsexual after bilateral mastectomy. World J Surg Oncol 2012; 10: 280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Patel JM, Dolitsky S, Bachman GA, Buckley de Meritens A. Gynecologic cancer screening in the transgender male population and its current challenges. Maturitas 2019; 129: 40–44. [DOI] [PubMed] [Google Scholar]
- 83.Kamen C, Mustian KM, Dozier A et al. Disparities in psychological distress impacting lesbian, gay, bisexual and transgender cancer survivors. Psychooncology 2015; 24: 1384–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]


