Introduction
Minimizing cognitive side effects of electroconvulsive therapy (ECT) while maintaining clinical efficacy is a key challenge. Given that the electrical charge required to induce a seizure varies by as much as 30-fold among patients (1), and that clinical efficacy and side effects of ECT depend strongly on the dose applied relative to the individual seizure threshold (2), many providers have adopted routine seizure threshold determination at the time of first treatment. As these protocols are not standardized, and likely vary based on the ECT electrode placement and stimulus parameters, information about the typical seizure threshold would help guide clinical practice. This study quantifies the charge required to induce a seizure using right unilateral brief pulse (RUL-BP) ECT in a large retrospective cohort.
Methods
The study population consists of patients aged 18 or older undergoing first lifetime ECT dose titration using RUL-BP (0.5–2 ms pulse width) stimuli at a freestanding academic psychiatric hospital from Jan 2000 to June 2017. Demographic information (age, sex, primary diagnosis), anesthetic, ECT charge, and electrographic seizure duration were extracted from the electronic medical record for this retrospective cohort. All ECT was provided using a Mecta Spectrum 5000Q (Tualatin, OR), and succinylcholine (1 mg/kg) was used as the muscle relaxant. Seizure duration was assessed using two lead bifrontal or fronto-mastoid EEG. The initial step of the dose titration was left to the discretion of the treating psychiatrist, with subsequent steps doubling the applied charge each time by doubling the stimulus duration, or increasing frequency once the maximum 8 second duration was used. Statistical analysis was completed using R (v 3.6, Vienna, Austria). A wavier of informed consent for this retrospective chart review study was provided by the Partners Healthcare Institutional Review Board.
Results
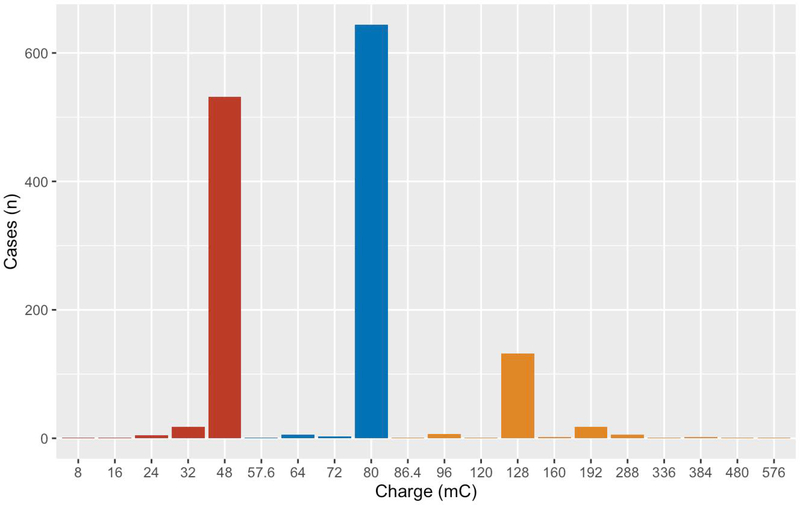
A total of 1,383 patients (588 male; 42.5%) underwent initial RUL-BP dose titration during the study period. Mean age was 49.4±16.9 years, and clinical diagnoses were unipolar depression (1,008; 72.9%), bipolar disorder (211; 15.3%), and other (70; 5.1%). Diagnostic information was missing for 94 patients (6.8%). Anesthetics used were methohexital (1,165; 85.0%), thiopental (128; 9.3%), propofol (73; 5.3%), and etomidate (5; 0.4%). The mean charge to induce a seizure was 75.1±38.4 mC (Figure 1), with a range from 8 mC to 576 mC. In a multivariable linear model of charge dosing, male sex (95% CI 0.34–8.21 mC; p≤0.05), older age (z-score, 95% CI 9.12–13.05 mC; p<0.001), and a diagnosis of bipolar disorder (95% CI 0.43–15.53 mC; p≤0.05) were each associated with higher final doses (Table S1; R2=0.09).
Figure 1:
histogram of charge applied to induce a seizure. Charges are binned into less than 50 mC (red), 50–80 mC (blue), and greater than 80 mC (orange). The charges applied vary by a factor of 72, from a minimum of 8 mC to a maximum of 576 mC.
Discussion
The mean charge needed to induce a seizure in our sample was 75.1±38.4 mC, comparable to the mean of 68.2 mC (95% CI 63.2–73.3 mC) found in a prior meta-analysis of 30 studies (3). There were significant positive effects of male sex, older age, and bipolar diagnosis on dose, but a model incorporating these variables explains only a minority of the variance in dosing, lower than the up to 50% variance explanation from prior models based on much smaller sample sizes (1,4,5). This emphasizes as yet unexplained factors affecting dose, which may include medications (6) and individual biometric properties (4). Notably, effect sizes of the significant variables in our model were all very small in magnitude, in contrast to smaller prior studies finding nearly 60% higher doses in men relative to women (7).
The results from our cohort demonstrate relatively little variation in electrical charge resulting in a seizure in RUL-BP ECT, albeit with a small right tail of patients requiring higher doses. With modern unilateral ECT generally utilizing doses well above seizure threshold for optimal treatment, e.g. 6x seizure threshold, based on our sample this would imply optimal dosing for subsequent treatments of approximately 450 mC. This is above the dose considered “fixed high-dose” in a prior prospective trial (8), and represents more than 75% of the maximal charge output permitted by the FDA for ECT devices in the United States. In our sample, 164 patients (11.9%) had initial treatments with charge >100 mC, and so could not be treated at 6x initial dose given FDA limitations. Moreover, 557 patients (40.3%) were initially treated with doses ≤ 50 mC, and who would be treated at a dose 50% greater than required in a regimen of fixed high-dose treatment. Thus in our cohort, an individualized seizure threshold titration for RUL-BP ECT would be expected to affect treatment dose in more than half of patients treated vs. treating all at a fixed dose. This is in contrast to ultrabrief pulse ECT, for which lower variance in seizure threshold may make titration less valuable (9).
Strengths of this study include a large sample size and consistency of ECT device, personnel, and protocols, which allows for consistent comparisons over the study period. The 1,383 RUL-BP patients reported here are a larger cohort than the aggregate 1,326 unilateral patients reported in a prior meta-analysis of 30 studies (3). Limitations include its retrospective observational nature and lack of consistent titration protocols. In particular, we are unable to assess the number of subthreshold stimuli each patient may have received, and so the doses applied here may overestimate the true seizure thresholds of patients. As treating physicians were free to set the initial charge of the titration, they likewise may have considers factors such as age, gender, or diagnosis in setting dose, and so the associations reported here may be influenced by preconceived notions of seizure threshold differences in these groups. In addition, we are unable to assess concomitant medications which may have affected seizure threshold.
Conclusion
Among 1,383 patients undergoing initial RUL-BP ECT dose titration, the mean charge to induce a seizure was 75.1±38.4 mC. While statistically significant, effects of sex, age, and diagnosis on dose are small, and explain only a minority of the observed sample variance.
Supplementary Material
Acknowledgments
Funding
This work was supported by the National Institute of Mental Health (R25MH094612, JL; R56MH115187 and R01MH120991, THM; 5R01MH112737-03, MEH), and the Brain and Behavior Research Foundation (NARSAD 26489; THM). The sponsors had no role in study design, writing of the report, or data collection, analysis, or interpretation.
Footnotes
Declarations:
Conflicts of Interest
THM receives research funding from the Stanley Center at the Broad Institute, the Brain and Behavior Research Foundation, National Institute of Mental Health, National Human Genome Research Institute Home, and Telefonica Alfa. The remaining authors have no disclosures to report.
Contributor Information
James Luccarelli, Department of Psychiatry, Massachusetts General Hospital, Boston MA; Department of Psychiatry, McLean Hospital, Belmont MA; Harvard Medical School, Boston MA.
Thomas H. McCoy, Jr, Department of Psychiatry, Massachusetts General Hospital, Boston MA; Harvard Medical School, Boston MA.
Stephen J. Seiner, Department of Psychiatry, McLean Hospital, Belmont MA; Harvard Medical School, Boston MA.
Michael E. Henry, Department of Psychiatry, Massachusetts General Hospital, Boston MA; Harvard Medical School, Boston MA.
Bibliography
- 1.Sackeim HA, Decina P, Portnoy S, Neeley P, Malitz S. Studies of dosage, seizure threshold, and seizure duration in ECT. Biol Psychiatry. 1987. March 1;22(3):249–68. [DOI] [PubMed] [Google Scholar]
- 2.Sackeim HA, Prudic J, Devanand DP, Kiersky JE, Fitzsimons L, Moody BJ, et al. Effects of Stimulus Intensity and Electrode Placement on the Efficacy and Cognitive Effects of Electroconvulsive Therapy. N Engl J Med. 1993. March 25;328(12):839–46. [DOI] [PubMed] [Google Scholar]
- 3.van Waarde JA, Verwey B, van der Mast RC. Meta-analysis of initial seizure thresholds in electroconvulsive therapy. Eur Arch Psychiatry Clin Neurosci. 2009. April 21;259(8):467. [DOI] [PubMed] [Google Scholar]
- 4.Colenda CC, McCall WV. A statistical model predicting the seizure threshold for right unilateral ECT in 106 patients. Convuls Ther. 1996. March;12(1):3–12. [PubMed] [Google Scholar]
- 5.Coffey CE, Lucke J, Weiner RD, Krystal AD, Aque M. Seizure threshold in electroconvulsive therapy: I. Initial seizure threshold. Biol Psychiatry. 1995. May 15;37(10):713–20. [DOI] [PubMed] [Google Scholar]
- 6.Chiao S, Isenberg K, North CS. Psychotropic Medication Effects on Seizure Threshold and Seizure Duration During Electroconvulsive Therapy Stimulus Titration. J ECT. 2020. June;36(2):115–122. [DOI] [PubMed] [Google Scholar]
- 7.Sackeim H, Decina P, Prohovnik I, Malitz S. Seizure threshold in electroconvulsive therapy. Effects of sex, age, electrode placement, and number of treatments. Arch Gen Psychiatry. 1987. April;44(4):355–60. [DOI] [PubMed] [Google Scholar]
- 8.McCall WV, Reboussin DM, Weiner RD, Sackeim HA. Titrated Moderately Suprathreshold vs Fixed High-Dose Right Unilateral Electroconvulsive Therapy: Acute Antidepressant and Cognitive Effects. Arch Gen Psychiatry. 2000. May 1;57(5):438–44. [DOI] [PubMed] [Google Scholar]
- 9.Luccarelli J, McCoy THJ, Seiner SJ, Henry ME. Total Charge Required to Induce a Seizure in a Retrospective Cohort of Patients Undergoing Dose Titration of Right Unilateral Ultrabrief Pulse Electroconvulsive Therapy. J ECT [Internet]. 2020. August 18 [cited 2020 Aug 24];Publish Ahead of Print. Available from: https://journals.lww.com/ectjournal/Abstract/9000/Total_Charge_Required_to_Induce_a_Seizure_in_a.99029.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.