BACKGROUND:
Managing patients during the coronavirus disease-2019 (COVID-19) pandemic, and the associated severe acute respiratory syndrome-related coronavirus-2 (SARS-CoV-2) in particular, required the nimble responsiveness for which WOC nurses are known. Problem-solving skills were needed to continue the level of WOC nursing services expected by patients, families, and professional colleagues, while reducing the hours we were physically present at our clinical facility. In order to respond to these demands, our team realized it must create an innovative approach to provide efficient, cost-effective consultations during this global crisis. This Challenges in Practice article summarizes our experience with use of telemedicine technologies to perform remote consultations within the acute care setting.
CASES:
Case 1 was a 52-year-old woman with a history of paraplegia. She had several pressure injuries but had not received topical care for these wounds prior to admission. A consultation for the WOC nurse was requested and performed via telehealth services on a day our team was working off-site. This case illustrates the process our team used to perform a virtual consultation and demonstrates how the use of images placed in the electronic medical record aided in developing an effective plan of care. Case 2 was a 48-year-old man who tested positive for COVID-19. He developed bilateral unstageable pressure injuries on his cheeks after being placed in the prone position for a prolonged period while critically ill. This case describes multiple technologic platforms used for telemedicine consults in a patient with COVID-19 requiring isolation.
CONCLUSIONS:
Remote consultation by WOC nurses was possible in our healthcare system because of previous experience using telemedicine technology and well-established collaborative relationships with providers and bedside nurses. By expanding our use of telemedicine technology, we were able to provide ongoing care to a patient without COVID-19 who had WOC consultation needs, and a patient with strict isolation demands due to COVID-19.
Keywords: Remote wound consultation, Telehealth, Telemedicine, Virtual wound care
INTRODUCTION
We believe that creative solutions to unique problems are the cornerstone upon which WOC nurses have built their practice. The severe acute respiratory syndrome-related coronavirus-2 (SARS-CoV-2) is part of the spectrum of disease caused by the 2019 novel coronavirus, collectively referred to as COVID-19.1 The resulting COVID-19 pandemic required rapid responsiveness and creative problem-solving that we believe forms a cornerstone of our specialty. The pandemic created challenges for the entire healthcare system of the United States, and it challenged the problem-solving skills of our WOC nursing team when faced with a reduction in onsite hours at the 5 hospitals in our healthcare system.
The COVID-19 pandemic began to exert a major impact on the United States in February 2020.2 In response, we developed a task force to determine how each facility in our healthcare system would segregate these highly infectious patients from other patients, caregivers, and facility staff. In the early stages, patients were admitted to intensive care units (ICUs) in each of our healthcare system's facilities. Our healthcare system moved the labor, delivery, and neonatal intensive care units (NICUs) into a new location in mid-February, just 2 weeks before the first patients with COVID-19 were admitted, and work immediately commenced to convert an empty healthcare facility into a site that would exclusively house patients who were positive for the virus. Our first patients with COVID-19 were admitted in March 2020. Within a matter of months, healthcare revenue sources fell sharply as elective procedures were deferred, leading many facilities across the country to scrutinize their budgets; this process led to reassignment of staff duties, reductions in hours worked, and involuntary furloughs in an attempt to reduce the financial impact of the pandemic. Executive leadership encouraged many services, including our WOC team, to create work-from-home guidelines for 2 days a week and to identify creative ways to implement remote consultations. Our WOC nursing team was tasked to create an innovative approach to provide efficient, cost-effective wound care consults during these challenging times.
Fortunately, our healthcare system had experience using a telemedicine platform in the critical care setting prior to the COVID-19 pandemic. We began using virtual ICU technology for real-time telemedicine wound care consultation in 2010.3 Our virtual ICU is a remote care strategy designed to provide constant monitoring and assessment for all critically ill patients in our healthcare system. This technologic platform interfaces with bedside monitors providing the remote clinician the ability to virtually assess remote ICU patients. We created a protocol for implementing a remote wound consultation. The protocol begins with a provider ordering a wound consultation in the patient's electronic medical record (EMR) (EPIC: Verona, Wisconsin). Upon receiving the consultation, the WOC nurse telephones the nurse caring for the patient. The bedside and the WOC nurse agree on a mutually acceptable time for the remote wound consultation to take place. The bedside nurse must be available during the consultation to obtain measurements and answer any objective assessment questions. The in-room camera and audio system (Yorktel: Univago HE platform; Eatontown, New Jersey) allows a remote clinician to visually assess the patients and converse directly with the staff and patient during this process. This 2-way communication enables us to embody our healthcare system's brand promise, “Being right here with you.” Once the assessment is complete, the WOC nurse enters a consultation note. Topical treatment orders are entered into the patient's EMR for the bedside nurse to perform as directed, and the note includes a reference that the provider should reconsult the WOC team for further assistance if necessary.
In addition to links to monitoring systems, critical care rooms in our healthcare system are hardwired with cameras enabling additional remote links to specialist providers installed on laptops. We also have several rolling carts with cameras enabling remote access to a limited number of patient rooms on medical-surgical inpatient care units. This access uses a similar process via a different software program (Jabber: Cisco; San Jose, California). Despite this history with telemedicine and virtual care technologies, we rapidly realized that the COVID-19 pandemic and sudden surge in acutely and critically ill patients demanded a strategy for visualizing wounds for patients cared for in isolation without direct visual inspection.
As a result, our WOC team created a protocol for telemedicine consultations (Box 1). This protocol enabled providers to enter photographs into the patient's EMR. Secure photography applications had been previously approved for use by the healthcare system and were sporadically used by some providers. The software we used can be easily installed on a mobile phone. Ensuring photographs were placed in the patient's EMR enabled us to provide a consistent approach to performing remote consultations on days we were working off-site, encouraged providers to utilize available technology, and minimized the number of staff members entering isolation rooms.
BOX 1. WOC Nursing Team Process for Use of Telehealth Consultations.
|
Case 1
Ms R was a 52-year-old White woman with a history of paraplegia secondary to a T4 spinal metastasis from a Hurthle cell thyroid carcinoma. Additional comorbid conditions included gastric esophageal reflux disease, diabetes mellitus, and depression. She presented to the emergency department (ED) during the COVID-19 pandemic with multiple complaints including vaginal itching, breast pain, and worsening of her bilateral ischial pressure injuries (PIs). She had not received any topical care for the PIs at home and reported they initially appeared about 3 months prior to admission. She was wheelchair bound, had neurogenic lower urinary tract and bowel dysfunction with dual urinary and fecal incontinence, and stated she had no sensation in the affected areas. Ms R had a fever with a temperature of 102.5°F (39.1°C); her blood pressure was normal as was her white blood cell count indicating she did not meet criteria for a diagnosis of sepsis. Given her febrile state, a viral test for COVID-19 was obtained and found to be negative. Additional blood testing revealed anemia with a hemoglobin level of 9.1 g/dL (91 g/L) and her hematocrit was 28.9% (0.289). Her lactic acid was high normal at 1.9 mmol/L, her serum glucose was elevated at 145 mg/dL (8.0 mmol/L), and her albumin was low at 2.6 g/dL (26 g/L). A computerized tomography (CT) scan of her pelvis revealed no evidence of osteomyelitis; instead, images revealed a collection of gas in the right inferior pubic ramus region—this collection attributed to her PI.
Ms R was admitted to hospital for bilateral ischial-infected PIs and febrile illness. Wound cultures were drawn, and broad-spectrum intravenous antibiotics were administered. A consultation for the WOC nurse was requested while she was undergoing evaluation in the ED; the consultation was performed via telehealth services on a day our team was working remotely. The WOC nurse used a secure, online messaging system (EPIC: Secure Chat; Verona, Wisconsin) to request placement of photographic images into her EMR record. The physician obtaining the photographs used facility-approved photography software (Haiku: Operating System; open source community) to capture the clinically relevant areas of her wounds and adjacent skin. The WOC nurse then reviewed the images and telephoned the bedside nurse to discuss wound characteristic including appearance, measurements, presence of odor or drainage, erythema, warmth, and induration. This consultation resulted in diagnosis of a deep tissue pressure injury (DTPI) on the left lateral heel (Figure 1) and an area of necrotic tissue on the distal plantar surface of the left foot (Figure 2). The WOC nurse also reviewed images placed in the EMR of unstageable PIs to the left and right ischium, (Figures 3 and 4) and initiated a plan of care for topical treatment, pressure redistribution, moisture management, and nutritional support; these interventions were completed by the bedside nurses caring for Ms R. Due to the amount of necrotic tissue, presence of gas noted on the CT, and the extension of the DTPI along the periwound of the left ischial wound, the WOC nurse requested consultation with a general surgeon for sharp wound debridement. The etiology of the left plantar wound was unclear. Ms R had a history of diabetes mellitus and an insensate foot related to her paralysis. In accordance with best practice principles, her care team decided to leave the eschar in place and to monitor the wound. Pressure redistribution heel boots for off-loading were ordered and a mattress replacement with low-air-loss feature was recommended for pressure redistribution and moisture management. In addition, a registered dietician consultation was requested to maximize her nutritional status and supplement her diet as needed to promote wound healing.
Figure 1.
Left heel deep pressure tissue injury.
Figure 2.
Left foot eschar.
Figure 3.
Unstageable pressure injury of right ischium.
Figure 4.
Unstageable pressure injury of left ischium.
The following day, when the team was on location, the WOC nurse simultaneously assessed the ischial wounds with the general surgery team. The surgeon performed bedside sharp debridement to the bilateral ischium unstageable PI (Figure 5) and ordered topical application of an enzymatic debridement ointment in conjunction with pulsatile lavage daily. The WOC nurse reassessed the wounds during a follow-up consult the following week to determine whether there were any other recommendations necessary for wound care; no change in the treatment plan was indicated. When our team signed off the case, the patient's wounds were being managed by the general surgery team and the physical therapy department who were providing daily pulsatile lavage to assist with removal of nonviable tissue.
Figure 5.
Bilateral unstageable pressure injuries following surgical debridement.
Case 1 illustrates the value of having a process for a provider to enter photographs into the patient's EMR. Ms R was admitted on a day our team was performing remote consultations; her unstageable PIs had developed odor, drainage, and an increased amount of nonviable tissue. The WOC nurse contacted the primary physician and requested that photographs be entered the EMR, using the steps we created to enable this procedure. Once the images were uploaded into the patient's progress notes, our team could assess the wound appearance and order the appropriate topical treatment for the healthcare team to perform. We were also able to arrange a joint visit with a surgeon the following day to develop a collaborative plan—thus providing rapid formulation and execution of sharp wound debridement needed to remove nonviable tissue from the wound bed.
Case 2
Mr G was a 48-year-old Spanish-speaking male and migrant farm worker who arrived in the United States in April 2020 for work. He lived with 6 other farm workers, practiced social distancing and wore a mask, and drove separately when commuting to work or home. Despite these preventive actions, he developed fever, cough, and malaise 8 days after arriving in the United States. Two days later he developed respiratory distress and altered mental status. Emergency medical services were summoned by his coworkers when Mr G exhibited difficulty breathing. When paramedics arrived, his initial oxygen saturation was 50% on room air. Mr G was placed on a nonrebreather mask and transported to our ED. During transport he experienced periods of apnea requiring bag-valve-mask ventilation. He was diaphoretic, tachycardic, tachypneic, and clearly in respiratory distress. Within the first hour of his arrival, Mr G underwent emergency insertion of a triple-lumen central catheter for parenteral fluids and medications, was intubated, and placed on ventilator support. Adequately oxygenating Mr G proved difficult; he ultimately required increased levels of positive end expiratory pressure, inverse ratio pressure-controlled ventilation settings, nitric oxide, and prone positioning. Just under 6 hours after arrival to the ED, Mr G was diagnosed with COVID-19 by nasopharyngeal swab and placed in a medically induced coma using a neuromuscular blockade with paralytics and sedation.
Twenty-two hours after arrival, Mr G was placed on continuous renal replacement therapy (CRRT) dialysis for continued anuria and a rising serum creatinine. Blood clotting and blockage of his central catheter lines developed within 36 hours of his hospital admission. Mr G required ongoing adjustments of continuous intravenous anticoagulation and frequent changes of clotted lines. The patient experienced CRRT line occlusions that occurred when his head was repositioned from side to side while in the prone position. Position-related line occlusions and oxygenation instability prohibited head repositioning while in the prone position for over 48 hours. One week after admission, Mr G was able to tolerate a supine position for 8 hours per day.
On day 8, our team was consulted for bilateral blackened facial wounds beneath the endotracheal tube stabilization device. We diagnosed unstageable medical device–related pressure injuries (MDRPIs).4 No photographs of the affected areas were available; our team conducted a telehealth visit with assistance from the bedside nurse, using our remote ICU camera system. This process usually allows our WOC team to visually assess the patients and communicate verbally with the bedside nurse and the patient. However, the camera, which had been installed in the new facility that housed patients with COVID-19, would not rotate enough to allow visualization of Mr G's wounds. As an alternative, we asked his bedside nurse to describe the skin damage via the telemedicine portal; she provided measurements of the wounds, a description of their appearance and locations. Silicone foam dressings (Allevyn: Smith and Nephew, Andover, Massachusetts) were placed over the areas and under the endotracheal tube stabilizer to protect the underlying skin and promote healing. A telehealth visit the following week (conducted using the same technologic platform) indicated no change in the appearance of the wounds. The silicone foam dressing was changed to a hydrocolloid (Replicare: Smith and Nephew, Andover, Massachusetts) to promote autolytic debridement of the cheek wounds. Mr G underwent a tracheostomy 3 weeks after admission and no longer had a medical device over the affected areas. During subsequent weekly assessments, the WOC team repeatedly provided care to Mr G via telemedicine with the assistance of verbal descriptions and measurements of the wound provided by his bedside nurses. After 3 weeks, the eschar began to soften and lift at the edges, and Mr G no longer required continuous venovenous hemodialysis. He was transferred to a different hospital location in our healthcare system to begin hemodialysis. At this point we used the secure, online messaging system developed by the manufacturer of our EMR (EPIC: Secure Chat) to request photographic images be placed into the patient's EMR. A provider again used our facility-approved photography software to photograph the areas of concern for Mr G's EMR. Because of strict isolation demands, a mobile phone was placed into a plastic bag to prevent spread of the coronavirus and obtain these essential photographs. Although of comparatively poor quality, the WOC team was nevertheless able to assess the unstageable PI locations (Figure 6). Mupirocin ointment was ordered twice daily to promote moist healing and assist with softening the remaining eschar; the areas were left open to air. After 5 weeks of COVID-19 isolation precautions, Mr G tested negative for the coronavirus. At this point, his left cheek wound had loose yellow slough, some of which was easily removed with cleansing. The wound was now more definitely diagnosed as a full-thickness Stage 3 PI, measuring 0.5 cm × 0.5 cm × 0.3 cm, with 50% red and 50% yellow tissue in the wound bed. The right cheek also had loose slough, which removed easily when cleansed, revealing a Stage 3 PI, 0.8 cm × 0.8 cm × 0.1 cm, with 100% pink tissue in the wound bed (Figure 7). Topical treatment with the mupirocin ointment was continued. After 7 weeks, Mr G's wound had remodeled to skin level (Figures 8 and 9). We predict he will have scars to his both cheeks when the wounds have healed, and remodeling is complete related to the depth of tissue involvement.
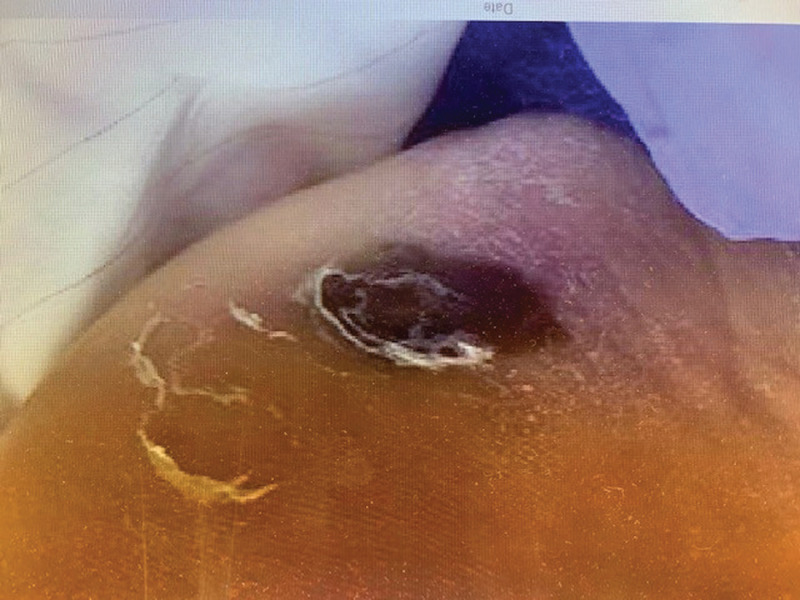
Figure 6.
Unstageable pressure injuries of bilateral cheeks—photograph taken with a mobile phone protected in a plastic bag.
Figure 7.
Bilateral unstageable pressure injuries to cheeks.
Figure 8.
Right cheek healing pressure injury.
Figure 9.
Left cheek healing pressure injury.
This case illustrates the challenges faced when providing wound care to a patient on strict isolation because of COVID-19. We experienced barriers when obtaining photographs of wounds for patients in strict isolation due to COVID-19. For example, this patient was admitted to our newly created COVID-19 hospital, where there were remote cameras available, which were not functioning to their full capacity, rendering it difficult to obtain clear images of the MDRPIs caused by prolonged prone positioning. In order to overcome this obstacle, we relied upon the bedside nurses' descriptions of the wound appearance and related characteristics. A photograph was eventually obtained using a mobile phone placed in a plastic bag and brought into the patient's room. This arrangement produced images with reduced clarity; nevertheless, they were of sufficient quality to enable diagnosis of unstageable PIs that were successfully managed with topical therapy.5
DISCUSSION
Prior to the COVID-19 pandemic, our healthcare system comprised 5 acute care facilities with approximately 1200 inpatient beds. A sixth site, a freestanding women's health hospital with a NICU was closed in mid-February, just 2 weeks prior to the arrival of our first patients with COVID-19 in March 2020. The patient population from that site was transitioned into a newly built facility adjacent to our main hospital location.
All consultant service providers, including 5 advanced practice nurses who manage WOC nursing services across our healthcare system, were charged to minimize the number of personnel who would enter the isolation room of patients with COVID-19, reduce personal protective equipment use, and reduce risk of nonessential exposure. Our previous experience with telemedicine using both in-room and cart-mounted camera systems proved beneficial in developing a strategy for remote consultations during the pandemic. Bedside nurses with enhanced skills in wound assessment and treatment also proved invaluable for this new care delivery model.
When our new facility reopened with a mission to provide care to patients with COVID-19, we found that the previously installed remote camera system in the critical care rooms was not functioning properly and did not allow us to obtain photographs of patients' wounds. We held a virtual team meeting to maintain social distancing and discuss possible solutions. The hospital system had recently purchased iPads (Apple, Inc, Cupertino, California) to enable patients to communicate with family members who were unable to visit, due to restricted visitation policies aimed at minimizing the risk of spreading infection across the community. We were able to FaceTime (Apple, Inc) with bedside nurses in the patient rooms and use this technologic platform to conduct wound assessments in real time, while the bedside nurse measured the wound and answered any additional queries. We also used remote technology, which was already available (Haiku, Univago, Jabber), to review images before entering a consultation note and initiating topical treatment orders remotely. Our team discussed concerns related to possible security or Health Insurance Portability and Accountability Act (HIPAA) violations if consultations were performed using these devices. In order to facilitate compliance with social distancing in healthcare while allowing providers to care for patients, the Centers for Medicare & Medicaid Services released a ruling on March 17, 2020, which allowed for a variety of virtual methods for communication with patients. This provided flexibility for use of telemedicine to care for patients and waived the prior HIPAA-compliant rules for use of devices.6
There were several times photographs were not available in the EMR despite our team's requests for images to be entered into the progress notes. Barriers to photography occurred for several reasons; the provider was not familiar with the process and did not feel comfortable taking the photographs, or they felt it was too difficult to bring a device into the isolation room to take a photograph. The WOC team recognized the stress staff members were under when caring for patients with COVID-19 in isolation; also there were changes in staffing patterns and reassignment of nursing roles and locations. Consultations were not performed near shift change or during times of increased staff responsibilities and often required rescheduling as the patient or nurses' priorities dictated. We were flexible and problem-solved in new and innovative ways; these are valuable skills that all WOC nurses are accustomed to having in their toolkit when performing patient consults (key points: Box 2).
BOX 2. Keys Points for Successful Use of Telemedicine Technology When Performing Remote Wound Consultations.
|
CONCLUSIONS
Remote consultation by WOC nurses was possible in our multisite enterprise because of previous experience using telemedicine technology and well-established collegial and collaborative relationships with providers and bedside nurses. Limitations during the COVID-19 pandemic included increased stress levels for providers who may have lacked familiarity with digital photography and bedside nurses who may have been working in unfamiliar settings due to reassignment. Lack of access to digital devices was a barrier that required creative solutions. Flexibility, dedication to timely consultation, and relentless pursuit of positive patient outcomes were key traits exhibited by the WOC nursing team members.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Katella K. Our New COVID-19 Vocabulary—What Does It All Mean? https://www.yalemedicine.org/stories/covid-19-glossary/ Accessed July 1, 2020.
- 2.Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States, Feb 24-April 21, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18):551–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clegg A, Brown T, Engels D, Griffin P, Simonds D. Telemedicine in a rural community hospital for remote wound care consultations. J Wound Ostomy Continence Nurs. 2011;38(3):301–304. [DOI] [PubMed] [Google Scholar]
- 4.Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services. Medicare Telemedicine Healthcare Provider Fact Sheet. Baltimore, MD: Centers for Medicare & Medicaid Services. [Google Scholar]
- 6.WOCN Board of Directors Task Force. Recommendations for wound assessment and photodocumentation in isolation. J Wound Ostomy Continence Nurs. 2020;47(4):319–320. [DOI] [PMC free article] [PubMed] [Google Scholar]