Abstract
Background and purpose
Spain has been heavily affected by COVID-19. Reallocation of resources for managing the outbreak might have caused a disruption in stroke care. This study analyses the impact on stroke care of reorganising the healthcare system in response to the first COVID-19 outbreak peak in Spain and the strategies adopted by Spanish stroke units to deal with this impact.
Materials and methods
We obtained data from a structured survey sent to the responsible of stroke units across the country. We recorded the number of strokes, stroke code activations, intravenous thrombolysis treatments and mechanical thrombectomies during February and March 2019 and 2020. We also collected information on the impact on workflow metrics and on the availability of specialised neurological care and rehabilitation treatments, the characteristics of stroke care for patients with SARS-CoV-2 infection and the impact on human resources. We compared the activity data between 2019 and 2020 and the information on activity and impact on stroke care between regions classified according to the disease incidence rate.
Results
Fifty-seven (75%) of all stroke units in Spain responded to the survey. There was an overall reduction in admissions for all stroke types during the outbreak’s peak and in the number of stroke code activations and intravenous thrombolysis treatments, results that were independent of the COVID-19 incidence rate. Participants reported a delay in workflow metrics and a reduction of admissions to stroke units, outpatient clinics and rehabilitation therapies. Specific pathways and protocols for managing stroke patients with SARS-CoV-2 infection have been established.
Conclusion
The COVID-19 outbreak has jeopardised all phases of stroke care. As a consequence, some patients with stroke did not receive adequate treatment.
Keywords: stroke
Introduction
SARS-CoV-2 infection, which causes COVID-19, has spread rapidly throughout the world since December 2019 when the first outbreak was detected in Wuhan, China. The outbreak was declared an international public health emergency by the International Health Regulations (2005) Emergency Committee on the 30 January 2020 and was recognised by the WHO as a global pandemic on the 11 March 2020.
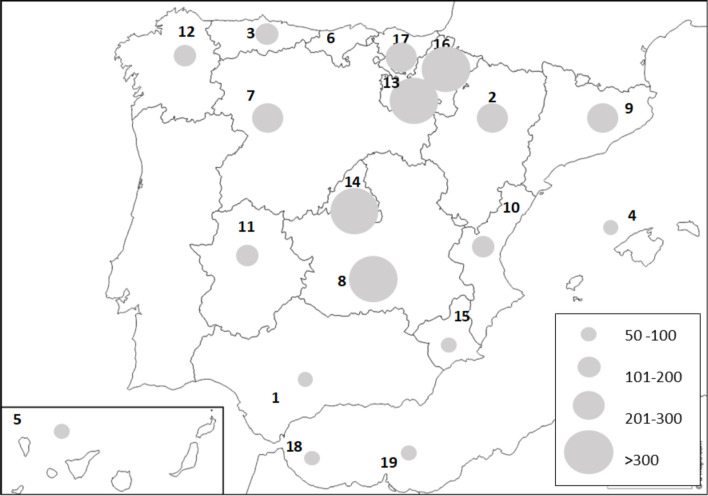
Spain has been one of the countries most heavily affected by COVID-19 in Europe.1 The first case in Spain was confirmed on the 31 January 2020, with number rapidly increasing thereafter, prompting the declaration of a national state of emergency and a population lockdown on the 14 March 2020 in an effort to halt the spread of the disease and prevent the collapse of hospital services. The pandemic’s first peak was reached during the last week of March, when the cumulative rate for the entire country was 217 cases/100 000 inhabitants, ranging from 56 to 612 cases per 100 000 inhabitants in the various autonomous communities (figure 1).2
Figure 1.
Map of the autonomous communities of Spain. Population density and COVID-19 incidence rate. The circles represent the incidence rate at the peak of the pandemic (per 100 000 inhabitants). Population density is shown beside the name of the community (inhabitants/km2). 1: Andalucía (96). 2: Aragón (28). 3: Principality of Asturias (96). 4: Balearic Islands (230). 5: Canary Islands (289). 6: Cantabria (109). 7: Castilla y León (25). 8: Castilla-La Mancha (26). 9: Cataluña (239). 10: Community of Valencia (215). 11: Extremadura (26). 12: Galicia (91). 13: La Rioja (63). 14: Community of Madrid (830). 15: Murcia region (132). 16: Chartered Community of Navarra (63). 17: Basque Country (305). 18: Autonomous City of Ceuta (7207). 19: Autonomous City of Melilla (4239).
The burden of patients with SARS-CoV-2 infection forced the Spanish healthcare system to reorganise medical care and reallocate resources for managing COVID-19, which might have caused a disruption in stroke care and could have resulted in a negative impact on outcomes.3–5 Stroke is one of the leading causes of death and disability worldwide.6 Due to the highly time-sensitive nature of stroke treatment, major efforts have been employed to construct well-organised healthcare systems to ensure rapid access to acute treatment, which might have been jeopardised by the pandemic. Different strategies to fight this threat according to particular situations and available resources have been published.7–9 Collecting information on the impact of first pandemic peak and the approaches implemented to cope with it could help us meet the challenge of maintaining the adequate care of patients with stroke, given that the pandemic is still far from being controlled.
In this study, we analysed the impact of the COVID-19 pandemic on stroke care and the activity of stroke units (SUs) in Spain, according to the burden this pandemic has placed on the various regions and we describe the organisational strategies implemented by Spanish neurologists during the first pandemic peak.
Methods
Setting
Spain is divided into 17 autonomous communities and 2 autonomous cities (figure 1). Each community has its own regional government with legislative and executive autonomy that includes health policies. Healthcare is essentially provided by Spain’s public health system and hospitals that provide stroke care are managed by the regional government of the autonomous communities. All communities have developed organisational models for stroke care according to their particular characteristics and needs, aiming to provide optimal treatment to each patient and equity in terms of access to the best diagnostic and therapeutic resources, including management in SUs.10 Although the number of available SUs and the population-adjusted rate of SU beds differ by community, most patients with acute stroke are treated in these facilities and, therefore, data from these units during the first pandemic peak could reflect the impact of COVID-19 on stroke care in Spain. The number of inhabitants and population density vary by community, which might account for the differences in the pandemic’s impact among regions. We obtained data on the population per community from the Spanish National Institute of Statistics11 and information on the incidence of COVID-19 from the official sources of the Spanish National Ministry of Health.2
Data source
A committee of experts from the Stroke Group of the Spanish Society of Neurology developed a structured survey that was sent to all neurologists working at SUs in hospitals throughout Spain, along with a letter of invitation to voluntarily participate that explained the study objectives and provided access to the web-based questionnaire. To avoid data duplication, respondents were asked to provide only one survey per hospital. The need to provide only verified data and not estimates was emphasised. The survey was launched on the 13 April 2020 and closed on the 13 August 2020. Throughout the study period, reminders were sent to encourage participation.
The survey recorded five different blocks of questions: (1) the participants’ names and contact details and the number of staff neurologists and residents per neurology department, (2) data on SU activity during February and March 2019 and 2020 (number of transient ischaemic attacks (TIAs), ischaemic strokes (ISs) and intracerebral haemorrhages (ICH) treated, number of stroke code activations and number of intravenous thrombolysis (IVT) treatments and mechanical thrombectomies (MT) performed), (3) information on the impact on acute stroke care during the pandemic (whether the respondents considered that there was an impact or not and whether the impact consisted of longer delays in hospital admission, in attention by a neurologist, in the performance of diagnostic tests or in initiation of IVT or MT or whether the availability of SUs facilities, specialised neurological care, Doppler ultrasound studies, outpatient clinics, or rehabilitation treatments was reduced, and if telemedicine was reinforced), (4) information regarding the characteristics of care for stroke patients with a suspected or confirmed diagnosis of SARS-CoV-2 infection (whether the protocols and care pathways were modified and whether the modifications affected the stroke code pathways, in-hospital pathways, diagnostic protocols, treatment protocols, creation of specific and separated SUs and/or neurology wards) and (5) data on the impact on human resources (number of medical leaves due to contagion or quarantine and the number of neurologists reallocated to reinforce other hospital areas for the care of patients with COVID-19, whether there was a reduction in the number of neurologists dedicated to the SUs or the neurology ward and whether there was an impact on education and research activities). There was the possibility of providing additional information on any of these issues if needed.
Data collection and management and statistical analysis
We collected and managed the study data using REDCap (Research Electronic Data Capture) tools.12 REDCap is a secure, web-based software platform designed to support data capture for research studies and allows audit trails for tracking data manipulation. We exported the data to the STATA V.12.1 statistical package (StataCorp LP, Texas, USA) for analysis.
The data are listed as absolute counts and percentages or as medians and IQR or minimum and maximum as appropriate. We compared the number of TIAs, ISs and ICHs treated at the participating hospitals and the number of stroke code activations, IVTs and MTs performed during February and March 2020 against those in February and March 2019 using the Wilcoxon signed-rank test for non-normally distributed variables or a paired Student’s t-test for those that followed a normal distribution.
Given that the pandemic has not affected all regions in Spain equally, we classified the autonomous communities into four groups according to the categorisation of incidence rate recorded in each community (figure 1). We compared the data between the groups to analyse whether there were differences in SU activity or the impact on stroke care depending on the disease burden using the Kruskal-Wallis test or Pearson’s χ2 test, respectively. We also compared the data between those communities with the highest incidence rate (>300 cases/100 000 inhabitants) and the other communities.
Results
Fifty-eight SUs responded to the survey, with one response discarded because no valid data could be retrieved. Ultimately, we analysed data on 57 surveys from 16 autonomous communities, representing 75% of all SUs in Spain. The percentage of SUs that responded to the survey per community was 66%–100% (table 1).
Table 1.
Survey responses by autonomous community
| Autonomous community | Number of responses | % of stroke units responding in the community | % of total responses |
| Andalucía | 9 | 88.9 | 15.8 |
| Aragón | 2 | 100 | 3.5 |
| Principality of Asturias | 2 | 100 | 3.5 |
| Balearic Islands | 1 | 100 | 1.7 |
| Canary Islands | 2 | 100 | 3.5 |
| Cantabria | 1 | 100 | 1.7 |
| Castilla y León | 4 | 80 | 7 |
| Castilla-La Mancha | 2 | 66.7 | 3.5 |
| Cataluña | 8 | 66.7 | 14 |
| Community of Valencia | 4 | 66.7 | 7 |
| Extremadura | 2 | 100 | 3.5 |
| Galicia | 3 | 100 | 5.3 |
| La Rioja * | 0 | 0 | 0 |
| Community of Madrid | 11 | 91.7 | 19.3 |
| Murcia region | 2 | 100 | 3.5 |
| Chartered Community of Navarra | 2 | 100 | 3.5 |
| Basque Country | 3 | 75 | 5.3 |
| Autonomous City of Ceuta † | 0 | 0 | 0 |
| Autonomous City of Melilla † | 0 | 0 | 0 |
*La Rioja has one stroke unit.
†Ceuta and Melilla have no stroke units.
Table 2 shows the number of TIAs, IS and ICH treated in the participating hospitals and the number of stroke code activations, IVTs and MTs performed during February and March 2019 and 2020.
Table 2.
Stroke unit activity in Spanish hospitals during the peak of the pandemic and during the same period in 2019
| Number of responses | February 2019 | February 2020 | P | March 2019 | March 2020 | P | |
| TIA | 49 | 7 (4,12) | 6 (3;10) | 0.12 | 8 (4,12) | 6 (3,8) | 0.019 |
| Ischaemic stroke | 53 | 31 (23,43) | 34 (24;47) | 0.84 | 35 (20,48) | 27 (18,37) | 0.000 |
| Cerebral haemorrhage | 51 | 7 (4,10) | 7 (4;11) | 0.78 | 6 (4,10) | 5 (3,10) | 0.008 |
| Stroke code activation | 41 | 33 (19,51) | 35 (20;59) | 0.9 | 35 (16,53) | 24 (13,43) | 0.000 |
| Intravenous thrombolysis | 56 | 6 (4,8) | 7 (4;11) | 0.67 | 7 (4,11) | 5 (3,9) | 0.000 |
| Thrombectomy | 56 | 6 (3,11) | 8 (2;12) | 0.09 | 7 (2,13) | 6 (2,12) | 0.10 |
Data indicate the number of cases per month presented as: median (IQR).
TIA, transient ischaemic attack.
There was a significant decrease in the number of stroke code activations, all types of strokes treated and IVT performed in the participating hospitals during March 2020, coinciding with the first pandemic peak in Spain. Interestingly, the number of MTs was not reduced. There were no differences in the percentage reduction according to the incidence rate (table 3).
Table 3.
Percentage reduction in stroke unit activity during the peak of the pandemic (March 2020 compared with March 2019) according to the incidence rate
| Total sample | Incidence rate (cases/100 000 inhabitants) | |||||
| 50–100 | 100–200 | 200–300 | >300 | P | ||
| TIA | 19 (0,53) | 17 (−22,56) | 32 (0,62) | 0 (0,50) | 33 (−20,56) | 0.75 |
| Ischaemic stroke | 21 (0,37) | 15 (−6,32) | 21 (6,31) | 15 (0,27) | 37 (23,46) | 0.11 |
| Cerebral haemorrhage | 26 (0,50) | 29 (−33,67) | 21 (0,50) | 7 (0,35) | 29 (16,50) | 0.37 |
| Stroke code activation | 28 (9,42) | 33 (20,42) | 21 (10,32) | 12 (6,42) | 37 (35,54) | 0.26 |
| Intravenous thrombolysis | 25 (0,50) | 42 (−12.5,48) | 50 (0,75) | 22 (0,52) | 36 (0,54) | 0.80 |
| Thrombectomy | 18 (0,43) | 19 (−16,72) | 12 (0,25) | 26 (0,43) | 19 (12.5,43) | 0.78 |
Data are presented as median (IQR).
TIA, transient ischaemic attack.
When comparing regions with the highest incidence rate with the other regions, the differences were also not significant. The dispersion in the results suggests heterogeneity in the pandemic’s impact on SU activity throughout Spain.
All but one of the participants considered that the COVID-19 outbreak had a negative impact on the care of patients with stroke, mainly in terms of delays in receiving treatment. Seventy-seven per cent of participants reported longer times to arrival at the hospital, 14% reported longer delays in receiving care by neurologists and 54% in performing diagnostic tests, 37% reported longer door-to-needle times (if IVT) and 33% reported longer door-to-femoral puncture times (if MT). Longer delays in attention were more frequently reported by centres in the autonomous communities with a higher incidence of the disease, although the difference was only significant for reported delays in performing diagnostic tests (table 4).
Table 4.
Reported impact on stroke care during the pandemic according to the incidence rate
| Total sample | Incidence rate (cases/100,000 inhabitants) | |||||
| 50–100 | 100–200 | 200–300 | >300 | P | ||
| Longer delay to hospital arrival | 44 (77) | 10 (77) | 9 (75) | 12 (71) | 13 (86) | 0.74 |
| Longer delay to neurologist | 8 (14) | 2 (15) | 1 (8) | 1 (6) | 4 (27) | 0.35 |
| Longer delay to diagnostic tests | 31 (54) | 6 (46) | 5 (42) | 7 (41) | 13 (88) | 0.035 |
| Longer door-to-needle time | 21 (37) | 5 (38) | 4 (33) | 4 (23.5) | 8 (53) | 0.37 |
| Longer door-to-puncture time | 19 (33) | 4 (31) | 4 (33) | 6 (35) | 5 (33) | 0.99 |
Data are presented as number (%) of affirmative responses in each group.
Three participants (5.3%) stated that specific treatments for patients with stroke such as reperfusion therapies were interrupted in their hospitals, 18 (32%) reported that patients were not admitted to the SU, and one hospital indicated that their patients with stroke were no longer managed by neurologists. In 47 SUs (82%), rehabilitation treatments were interrupted. Doppler ultrasound vascular studies were cancelled in 20 (35%) centres. Outpatient clinics reduced their activity in most cases, in-person consultations were cancelled in 39 (68%) of the participating hospitals, and teleconsultation was implemented in all but three hospitals (95%).
Regarding the management of patients with stroke with a suspected or confirmed diagnosis of SARS-CoV-2 infection, most centres progressively adapted their treatment protocols as the number of cases increased, with the aim of maintaining adequate treatment for stroke and COVID-19, while ensuring the protection of attending staff and preventing the spread of the infection. Twenty-nine (51%) centres that usually work within a collaborative network for providing reperfusion therapies reorganised their stroke code pathways and resources to provide on-site treatment, avoiding interhospital transfers. In the emergency room, 35 centres (61%) organised separate hotspots and triage pathways for these patients’ diagnosis and management, 43 (75%) centres designed specific protocols for staff protection, 36 (63%) included specific tests for COVID-19 within their urgent diagnostic protocols such as performing chest CT together with neuroimaging, additional blood tests and PCR for SARS-CoV-2 in nasal and oropharyngeal swabs and 26 centres (46%) modified their management protocols, including more restrictive criteria for reperfusion therapies. There were organisational changes for hospital admissions, separating COVID-free from COVID-positive areas in all centres. Seven (12%) centres created a specific SU for patients with COVID-19, 10 (18%) created a COVID-19 neurology ward and 30 (53%) of the respondents stated that their patients with stroke and COVID-19 were admitted to internal medicine wards and not to the neurology wards or SU.
The outbreak also affected the human resources of the neurology departments and their activities, with a reduced number of dedicated neurologists due to medical leave as a consequence of contagions and quarantines as well as reallocations to reinforce other hospital areas for the care of patients with COVID-19. Table 5 shows the number of medical staff in the participating hospitals and the number of contagions, quarantines and reallocations during the study period.
Table 5.
Impact on human resources
| Total number per neurology department | Number of reallocated | % reallocated | Number of contagions | Number in quarantine | % of medical leaves | |
| Staff neurologists | 17 (7; 35) | 4 (0; 14) | 22 (0; 73) | 2 (0; 12) | 1.5 (0; 7) | 18 (0; 57) |
| Resident neurologists | 6 (0; 16) | 4 (0; 16) | 51 (0; 100) | 1 (0; 6) | 1 (0; 3) | 23 (0; 75) |
Data are presented as mean (range).
Due to the reduced number of available neurologists, 89% of the participating centres reported changes in their usual activities, which included a reduction in the number of neurologists dedicated to the SU or the neurology ward in 49% of cases, in the number of on-call neurologists in 18% and in discontinuation of the neurology on-call service in one case (2%). Most of the participants discontinued their research and teaching activities (72% and 82%, respectively).
Discussion
This study provides data on the impact of the COVID-19 pandemic on stroke care in Spain and on how Spanish SUs reorganised their management procedures in a health system overwhelmed by the rapid surge of patients with COVID-19. Although partial data from specific regions and centres have been previously published,3–5 8 13 there was a need for information from a national perspective similar to that provided by other European countries.9
This study confirms the overall reduction in admissions of all types of strokes during the first peak of the outbreak in Spain and the significant reduction in the number of stroke code activations and IVTs performed, while the number of MTs did not significatively decrease. However, the magnitude of the decrease varied considerably among the participating centres, with a number of them reporting no decrease, and it did not appear to be related to the incidence of COVID-19 in the regions. This finding probably reflects the differences in these centres’ characteristics in terms of size, catchment area and volume of patients treated in normal conditions and the differences among the regions in the organisational systems for providing care. A decrease in stroke admissions as a consequence of the pandemic has been also reported in other countries9 14 and in certain areas of Spain.3–5 13 This decrease has been attributed to several reasons15: fear of contagion that might prevent individuals from seeking medical care, especially for milder or transient strokes, non-recognition of symptoms by isolated or older patients, misdiagnosis in the context of the concomitant symptoms of SAR-CoV-2 infection and overload of emergency medical and ambulance services. Our survey did not include questions about the possible explanations for the decrease in stroke admissions, but the findings suggest that numerous causes could have contributed at the light of the significant variability observed in the reported data. Moreover, admissions for all types of stroke were similarly reduced, and the decrease in stroke code activations did not correlate with the incidence rate in the communities. Whatever the reasons for the decrease in activity and given there is no reason to suspect that fewer strokes occurred during the pandemic, our results suggest that a number of patients did not reach hospitals and therefore did not receive appropriate treatment during this period.
Most of the participants reported increased delays in arrival to the hospital, and half of the participants indicated delays in the performance of diagnostic tests, which possibly reflects the overload of the emergency services, given that delays were more frequently reported among those centres in the communities that experienced higher COVID-19 incidence rates. This, together with the decrease in stroke admissions and delayed arrival at the hospital beyond the window of opportunity for recanalisation therapies, might have accounted for the reduced number of IVTs and MT shown. These results are consistent with those of previous studies that reported a decrease in the absolute number of reperfusion therapies performed during the outbreak.3–5 16 17 However, most of these studies showed that the percentage of eligible patients who was treated remained stable,4 5 17 and two studies reported no significant time delays in door-to-IVT or door-to-MT.3 16 In our survey, delays in receiving care from a neurologist and in starting IVT or MT were less frequently reported than delays in other workflow metrics, and the number of MTs was not reduced. Together with the abovementioned reports, these results might reflect the significant efforts undertaken by neurologists to preserve in-hospital stroke care despite the adverse conditions.
The survey results show that various organisational strategies have been implemented in Spanish hospitals to ensure stroke care and to protect patients and staff from contagion. The observed variability is probably due to the differences in the available resources and in healthcare system organisations between regions and to the need to rapidly adopt decisions in the absence of substantiated recommendations or specific roadmaps. Resources of SUs and neurology departments were reallocated to cope with the massive arrival of patients with COVID-19, which has had a negative impact on stroke care. A third of centres in our survey stated that patients with stroke could not be admitted to their SU, and the outpatient clinics and rehabilitation therapies were cancelled in most centres. The situation was even poorer for patients with SARS-CoV-2 infection and stroke. Few centres could organise COVID-19 SUs or neurology wards, and most patients had no access to SUs or specialised neurological care. Telemedicine was reinforced in almost all participating centres, a good option for patient follow-up but it needs adequate planning and technical equipment,14 which, in this stressful situation, was far from optimal. It is highly likely that the disruption in all steps of stroke care during the pandemic has affected the recovery and adherence to secondary prevention measures of patients who experienced a stroke in Spain.
The impact of the outbreak on human resources is also remarkable and has contributed to jeopardise stroke care. Not only were numerous neurologists reassigned to the care of patients with COVID-19 but many of them also become infected and/or had to quarantine. There was also major variability between centres, which probably reflects the varying exposure risk. Healthcare practitioners are at high risk18 and therefore measures need to be assured to protect them.
Finally, another important issue addressed in this study is the effect of the pandemic on education and research activities that were discontinued in most of the centres. These activities need to be preserved because are crucial for maintaining high standards of quality in the healthcare system.
Given that stroke is the second leading cause of death and one of the main causes of disability, it is important to preserve the quality of stroke services even in these adverse conditions. At the beginning of this unprecedented situation, hospitals had to improvise solutions, which is not the case at present. There are lessons to learn from the experience published worldwide and from the suggested guidelines to protect professionals and patients.19–21 The pandemic is currently far from being controlled, and efforts should be made to balance the allocation of resources to guarantee the adequate management of COVID-19 and other prevalent and disabling diseases such as stroke. Institutions should not lose sight of this goal, or they will risk losing the trust of their health workers and the population.
Our study has a number of limitations. First, we did not collect information on the characteristics of the participating SUs. We therefore could not adjust the results accordingly. Second, this study was not based on systematically recorded data, thereby it has a risk of bias in the reporting. There was also a lack of data on the outcomes.
In conclusion, the rapid surge of the COVID-19 outbreak has greatly stressed the healthcare system in Spain, which has led to disruption of all phases of stroke care. As a consequence, some patients with stroke have not received adequate treatment, due to not reaching the hospitals in time or because they could not be managed by stroke physicians in specialised facilities, which might have negatively impacted the patients’ outcomes. Lessons should be learnt from this experience to prevent this situation from reoccurring.
Acknowledgments
Editorial assistance was provided by Morote Traducciones.
Footnotes
Collaborators: Stroke Group - Spanish Society of Neurology: Andalucía: María Dolores Fernández Pérez (Hospital Virgen De Las Nieves. Granada), Esther Gallardo Corral (Hospital Neurotraumatologico de Jaén), Patricia Martínez Sánchez (Hospital Universitario Torrecárdenas. Almería), Francisco Moniche (Hospital Universitario Virgen del Rocio. Sevilla), Juan Manuel Oropesa (Hospital Juan Ramón Jiménez. Huelva), Soledad Pérez Sánchez (Hospital Universitario Virgen Macarena. Sevilla), Raul Espinosa Rosso (Hospital Universitario Puerta del Mar. Cádiz), Jose Antonio Tamayo Toledo (Hospital Regional Universitario Malaga), Roberto Valverde Moyano (Hospital Universitario Reina Sofía. Córdoba). Aragón: Carlos Tejero Juste (Hospital Clínico Universitario Lozano Blesa. Zaragoza), Herbert Tejada Meza (Hospital Universitario Miguel Servet. Zaragoza). Principality of Asturias: Elena López-Cancio Martínez (Hospital Universitario Central Asturias. Oviedo), Ignacio Casado Menéndez (Hospital Universitario De Cabueñes. Gijón). Balearic Islands: M Carmen Jimenez Martinez (Hospital Universitario Son Espases. Mallorca). Canary Islands: Antonio Medina Rodriguez (Hospital universitario Nuestra Señora de Candelaria. Santa Cruz de Tenerife), Juan Carlos López Lopez Fernandez (Hospital Universitario de Gran Canarias Doctor Negrín. Las Palmas de Gran canaria). Cantabria: Enrique Jesús Palacio Portilla (Hospital Universitario Marqués de Valdecilla. Santander). Castilla y León: Juan Francisco Arenillas Lara (Hospital Clínico Universitario de Valladolid), Javier Tejada García (Complejo Asistencial Universitario de León), Yolanda Bravo Anguiano (Hospital Universitario de Burgos), Marta Ferrero Ros (Complejo Asistencial de Segovia). Castilla-La Mancha: Jose C. Segundo Rodriguez (Hospital Virgen de la Salud. Toledo), ÓscarAyo Martín (Complejo Hospitalario Universitario de Albacete). Cataluña: Pere Cardona (Hospital Universitari Bellvitge. L'Hospitalet de Llobregat. Barcelona), Jaume Roquer González (Hospital del Mar. Barcelona), Manuel Jesus Gómez-Choco Cuesta (Hospital Moises Broggi. Sant Joan Despí. Barcelona), Joan Marti Fabregas (Hospital de la Santa Creu i Sant Pau. Barcelona), Joaquín Serena Leal (Hospital Universitari Dr Josep Trueta. Girona), Francisco Purroy (Hospital Universitari Arnau de Vilanova. Lleida), Sergi Amaro Delgado (Hospital Clinic. Barcelona), Jorge Pagola (Hospital Vall D'hebron. Barcelona). Community of Valencia: Nicolas Lopez Hernandez (Hospital General Universitario Alicante), Alejandro Ponz De Tienda (Hospital Clínico Universitaro de Valencia), Cristina Soriano Soriano (Hospital General Universitario de Castellón. Castellón de La Plana), José Tembl Ferrairó (Hospital Universitario La Fe. Valencia). Extremadura: Ignacio Casado Naranjo (Hospital Universitario de Cáceres), Jose M. Ramirez Moreno (Hospital Universitario de Badajoz). Galicia: Mar Castellanos Rodrigo (Complejo Hospitalario Universitario A Coruña), Jose Luis Maciñeiras Montero (Hospital Alvaro Cunqueiro. Vigo), Emilio Rodríguez Castro (Hospital Clínico de Santiago de Compostela). Community of Madrid: María Alonso De Leciñana (Hospital Universitario La Paz. Madrid), Joaquin Carneado Ruiz (Hospital Universitario Puerta de Hierro. Madrid), Patricia Calleja Castaño (Hospital Universitario Doce de Octubre. Madrid), Jose Antonio Egido Herrero (Hospital Clinico Universitario San Carlos. Madrid), Andres Garcia Pastor (Hospital General Universitario Gregorio Marañón. Madrid), Alicia De Felipe Mimbrera (Hospital Universitario Ramón y Cajal. Madrid), Araceli García Tejada (Fundación Jiménez Díaz. Madrid), Marta Guillán Rodríguez (Hospital Universitario Rey Juan Carlos. Móstoles), Laura Izquierdo Esteban (H. Universitario Príncipe de Asturias. Alcalá de Henares), Beatriz Oyanguren Rodeño (H. Universitario de Torrejón. Madrid), Álvaro Ximénez-Carrillo Rico (Hospital Universitario La princesa. Madrid). Murcia region: Ana Morales Ortiz (Hospital Clinico Universitario Virgen de la Arrixaca. Murcia), Cristina Sánchez-Vizcaíno (Hospital Universitario Santa Lucia. Cartagena). Chartered Community of Navarra: María Herrera Isasi (Complejo Hospitalario de Navarra. Pamplona), Pablo Irimia Sieira (Clínica Universidad de Navarra. Pamplona). Basque Country: M. Mar Freijo Guerrero (Hospital Cruces. Barakaldo), Maite Martínez Zabaleta (Hospital Universitario Donostia), Juan Manuel García Sánchez (Hospital Universitario de Basurto-OSI Bilbao).
Contributors: MAdL: study concept and design. Data analysis. Drafting the manuscript. MC: study concept and design. Critical review of the manuscript. ÓA: study concept and design. Critical review of the manuscript. AM: study concept and design. Critical review of the manuscript.
Funding: SL funded by the Foundation for Biomedical Research of the University Hospital La Paz, IdiPAZ.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Stroke Group - Spanish Society of Neurology:
María Dolores Fernández Pérez, Esther Gallardo Corral, Patricia Martínez Sánchez, Francisco Moniche, Juan Manuel Oropesa, Soledad Pérez Sánchez, Raul Espinosa Rosso, Jose Antonio Tamayo Toledo, Roberto Valverde Moyano, Carlos Tejero Juste, Herbert Tejada Meza, Elena López-Cancio Martínez, Ignacio Casado Menéndez, M Carmen Jimenez Martinez, Antonio Medina Rodriguez, Juan Carlos López Fernandez, Enrique Jesús Palacio Portilla, Juan Francisco Arenillas Lara, Javier Tejada García, Yolanda Bravo Anguiano, Marta Ferrero Ros, Jose C Segundo Rodriguez, Pere Cardona, Jaume Roquer González, Manuel Jesus Gómez-Choco Cuesta, Joan Marti Fabregas, Joaquín Serena Leal, Francisco Purroy, Sergi Amaro Delgado, Jorge Pagola, Nicolas Lopez Hernandez, Alejandro Ponz De Tienda, Cristina Soriano Soriano, José Tembl Ferrairó, Ignacio Casado Naranjo, Jose M Ramirez Moreno, Jose Luis Maciñeiras Montero, Emilio Rodríguez Castro, Joaquin Carneado Ruiz, Patricia Calleja Castaño, Jose Antonio Egido Herrero, Andres Garcia Pastor, Alicia De Felipe Mimbrera, Araceli García Tejada, Marta Guillán Rodríguez, Laura Izquierdo Esteban, Beatriz Oyanguren Rodeño, Álvaro Ximénez-Carrillo Rico, Cristina Sánchez-Vizcaíno, María Herrera Isasi, Pablo Irimia Sieira, Mar Freijo Guerrero, Maite Martínez Zabaleta, and Juan Manuel García Sánchez
Data availability statement
Data are available upon reasonable request. Data are available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
References
- 1. World Health Organization . WHO Covid-19. WHO coronavirus disease (COVID-19) Dashboard, 2020. Available: https://covid19.who.int/ [Accessed 29 Aug 2020].
- 2. Ministerio de Sanidad . Health alert and emergency co-ordination centre (CCAES). Coronavirus infection in Spain. Available: https://www.mscbs.gob.es/en/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm [Accessed 29 Aug 2020].
- 3. Rudilosso S, Laredo C, Vera V, et al. Acute stroke care is at risk in the era of COVID-19. Stroke 2020;51:1991–5. 10.1161/STROKEAHA.120.030329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Montaner J, Barragán-Prieto A, Pérez-Sánchez S, et al. Break in the stroke chain of survival due to COVID-19. Stroke 2020;51:2307–14. 10.1161/STROKEAHA.120.030106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tejada Meza H, Lambea Gil Álvaro, Saldaña AS, et al. Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in north-west Spain. Int J Stroke 2020;15:755–62. 10.1177/1747493020938301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. GBD 2016 Stroke Collaborators . Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2019;18:439–58. 10.1016/S1474-4422(19)30034-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baracchini C, Pieroni A, Viaro F, et al. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol Sci 2020;41:1003–5. 10.1007/s10072-020-04375-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fuentes B, Alonso de Leciñana M, Calleja-Castaño P, et al. Impact of the COVID-19 pandemic on the organisation of stroke care. Madrid stroke care plan. Neurologia 2020;35:363–71. 10.1016/j.nrl.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bersano A, Kraemer M, Touzé E, et al. Stroke care during the COVID‐19 pandemic: experience from three large European countries. Eur J Neurol 2020;27:1794–800. 10.1111/ene.14375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alonso de Leciñana M, Morales A, Martínez-Zabaleta M, et al. Characteristics of stroke units and stroke teams in Spain in 2018. Pre2Ictus project. Neurologia 2020:S0213-4853(20)30222-X. 10.1016/j.nrl.2020.06.012 [DOI] [PubMed] [Google Scholar]
- 11. Instituto Nacional de Estadística . Population by autonomous community and autonomous City and sex. Available: https://www.ine.es/jaxiT3/Datos.htm?t=2853#!tabs-tabla [Accessed 29 Aug 2020].
- 12. Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tejada Meza H, Lambea Gil Á, Sancho Saldaña A, et al. Ischaemic stroke in the time of coronavirus disease 2019. Eur J Neurol 2020;27:1788–92. 10.1111/ene.14327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Markus HS, Brainin M. COVID-19 and stroke-A global world stroke organization perspective. Int J Stroke 2020;15:361–4. 10.1177/1747493020923472 [DOI] [PubMed] [Google Scholar]
- 15. Aguiar de Sousa D, Sandset EC, Elkind MSV. The curious case of the missing strokes during the COVID-19 pandemic. Stroke 2020;51:1921–3. 10.1161/STROKEAHA.120.030792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pop R, Quenardelle V, Hasiu A, et al. Impact of the COVID‐19 outbreak on acute stroke pathways – insights from the Alsace region in France. Eur J Neurol 2020;27:1783–7. 10.1111/ene.14316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhao J, Li H, Kung D, et al. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 2020;51:1996–2001. 10.1161/STROKEAHA.120.030225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moscola J, Sembajwe G, Jarrett M, et al. Prevalence of SARS-CoV-2 antibodies in health care personnel in the new York City area. JAMA 2020;324:893–5. 10.1001/jama.2020.14765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rodríguez-Pardo J, Fuentes B, Alonso de Leciñana M, et al. Acute stroke care during the COVID-19 pandemic. ictus Madrid program recommendations. Neurologia 2020;35:258–63. 10.1016/j.nrleng.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Khosravani H, Rajendram P, Notario L, et al. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke 2020;51:1891–5. 10.1161/STROKEAHA.120.029838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhao J, Rudd A, Liu R. Challenges and potential solutions of stroke care during the coronavirus disease 2019 (COVID-19) outbreak. Stroke 2020;51:1356–7. 10.1161/STROKEAHA.120.029701 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. Data are available from the corresponding author upon reasonable request.