Abstract
Objective
There is emerging evidence that COVID-19 disproportionately affects people from racial/ethnic minority and low socioeconomic status (SES) groups. Many physicians across the globe are changing practice patterns in response to the COVID-19 pandemic. We sought to examine the practice changes among rheumatologists and what they perceive the impact to be on their most vulnerable patients.
Methods
We administered an online survey to a convenience sample of rheumatologists worldwide during the initial height of the pandemic (between 8 April and 4 May 2020) via social media and group emails. We surveyed rheumatologists about their opinions regarding patients from low SES and racial/ethnic minority groups in the context of the COVID-19 pandemic. Mainly, what their specific concerns were, including the challenges of medication access; and about specific social factors (health literacy, poverty, food insecurity, access to telehealth video) that may be complicating the management of rheumatologic conditions during this time.
Results
548 rheumatologists responded from 64 countries and shared concerns of food insecurity, low health literacy, poverty and factors that preclude social distancing such as working and dense housing conditions among their patients. Although 82% of rheumatologists had switched to telehealth video, 17% of respondents estimated that about a quarter of their patients did not have access to telehealth video, especially those from below the poverty line. The majority of respondents believed these vulnerable patients, from racial/ethnic minorities and from low SES groups, would do worse, in terms of morbidity and mortality, during the pandemic.
Conclusion
In this sample of rheumatologists from 64 countries, there is a clear shift in practice to telehealth video consultations and widespread concern for socially and economically vulnerable patients with rheumatic disease.
Keywords: Autoimmune Diseases, Epidemiology, Qualitative research
Key messages.
What is already known about this subject?
To date, only one paper has highlighted the widening disparities among vulnerable patients with rheumatic disease during the COVID-19 pandemic.
This review addresses potential reasons for these patients having worse outcomes during this time and the factors that may be driving this disparity, but it does not engage with rheumatologists directly to validate what these reasons are and to seek those that are perhaps less apparent.
What does this study add?
We have sought to understand how rheumatologists are changing their practice and perceive healthcare disparities of patients from racial/ethnic minorities and low SES groups in the context of the COVID-19 pandemic.
We identified several factors that may be driving this disparity, for instance, inability of these patients to access telehealth video and failure to retrieve regular medications.
As the overwhelming majority of rheumatologists who answered the survey have now switched their practices to telehealth, this leaves many vulnerable patients at a great disadvantage.
How might this impact on clinical practice?
Rheumatologists share concerns for low health literacy, poverty, food insecurity and poor access to telehealth video among their vulnerable patients.
Rheumatologists need to be vigilant and proactive about caring for these vulnerable patients during and in the aftermath of the pandemic.
Given the high risk for vulnerable patients with autoimmune disease to contract COVID-19, rheumatologists should educate their patients about hand washing as well as appropriate social distancing practices.
Concrete actions for proactive care for vulnerable patients with autoimmune disease include pushing the prioritisation of vaccination for them once available.
INTRODUCTION
The COVID-19 pandemic caused by the novel virus SARS-CoV-2/2019-nCoV is affecting populations around the globe, resulting in deaths, morbidity and economic despair. As the pandemic evolves, an emerging feature has been that COVID-19 is disproportionately impacting minority and lower socioeconomic status (SES) patient populations worldwide.1–3 Evidence of this trend came to widespread attention after publications reported minority populations had three times the COVID-19 infection rate and almost six times the death rate of non-minority populations,4 5 despite these minorities making up only a small fraction of the total population. Similar reports among low SES populations also have subsequently emerged.6 7
Disease burden for autoimmune diseases is higher among patients from racial/ethnic minority and low SES groups.8–10 Furthermore, patients with autoimmune diseases may have a high number of comorbidities and receive immunosuppressant medications, potentially putting them at greater risk for COVID-19. There has been evidence during the pandemic regarding the potentially higher morbidity and mortality caused by COVID-19 in patients with autoimmune disease.11 The most recent statistics from the Global Rheumatology Alliance reported 2121 patients with rheumatic disease who developed COVID-19 (37.2% white, 13.3% black, 29.1% Latin American), of which 39% were hospitalised and 8% had a mortality.12 To this end, and to accommodate patient care needs during this time, many rheumatologists across the world have changed practices such as using telehealth video, to continue providing medical access to high-risk patients.
Using an online survey mechanism, we sought to examine how and whether rheumatologists have changed their practice patterns, and what their perceptions are on how COVID-19 might affect their most vulnerable patients.
METHODS
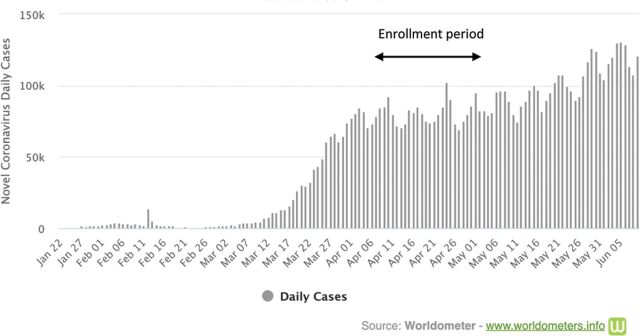
We conducted an online survey of a convenience sample of rheumatologists who practice medicine in diverse settings worldwide. This cross-sectional survey was administered between 8 April and 4 May 2020 during the rising pandemic (figure 1). It was built on an online platform (surveygizmo.com) and was disseminated using social media sites, including LinkedIn, Twitter, Facebook, ResearchGate, WhatsApp, and by email to rheumatology-specific groups. The survey relied on voluntary self-reporting and required that respondents must be rheumatologists (trainees included). We included responses from both adult and paediatric rheumatologists.
Figure 1.
Number of daily cases of COVID-19 worldwide according to date.
The questionnaire, written in English, consisted of basic demographics and questions about how rheumatologists thought their patients from low SES and racial/ethnic minority groups will do in the context of the COVID-19 pandemic; what their specific concerns for these patients were; and patient social factors in their practice, such as low health literacy, poverty, food insecurity, factors that preclude social distancing such as working and dense housing conditions and access to telehealth video. Questions are reported in the Results section; however, other questions in the survey, not included here, have been reported separately. Demographic variables of interest included rheumatologist gender, country of practice, years in rheumatology practice and practice setting. The Institutional Review Board of Hospital for Special Surgery approved the anonymised survey and protocol.
Descriptive statistics such as frequencies and percentages are presented. Bivariate comparisons were performed using Fisher’s exact test and χ2 tests for categorical variables and Wilcoxson-rank sum tests and Student’s t-tests for continuous variables. Statistical significance was determined using an alpha of 0.05 and all analyses were conducted using Stata version 14.
RESULTS
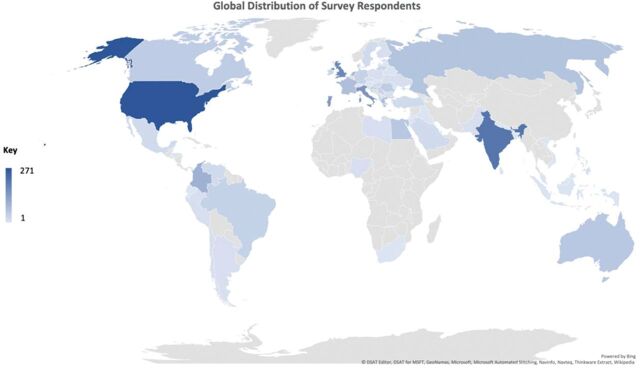
Table 1 summarises the characteristics of the sample. We included 548 rheumatologists who responded to at least 80% of the questionnaire. They were from 64 different countries and responses were comprised of 50% (n=271) from the USA, 30% (n=165) from Europe, 7% (n=37) from India and 14% (n=74) were from the remaining countries grouped as ‘Other’ (figure 2). Of all respondents, 28% practised in a private setting, 58% in academic hospital practices and 12% in publicly supported or government-supported clinics. There was 6% representation from paediatric rheumatologists and 9% treated both adults and children. Overall, 65% of rheumatologists (with the highest proportion from Europe) responded that at least a quarter of their patients relied on government insurance, such as Medicare and Medicaid, in the USA.
Table 1.
Characteristics of survey respondents
| Total N=548 (%) |
|
|---|---|
| Age group (years) | |
| 25–34 | 148 (27.0) |
| 35–44 | 220 (40.1) |
| 45–54 | 82 (15.0) |
| 55–64 | 53 (9.7) |
| 65+ | 45 (8.2) |
| Gender | |
| Female | 282 (51.5) |
| Male | 230 (42.0) |
| Do not want to specify | 3 (0.5) |
| Missing | 33 (6.0) |
| Practice type | |
| Academic/government | 387 (70.6) |
| Private practice solo/group/hospital | 153 (27.9) |
| Missing | 8 (1.5) |
| Number of years in rheumatology practice | |
| Currently in training | 80 (14.6) |
| 1–5 | 160 (29.2) |
| 6–10 | 104 (19.0) |
| 11–20 | 101 (18.4) |
| 21+ | 100 (18.2) |
| Missing | 3 (0.5) |
| Adult and/or paediatric practice | |
| Adult | 461 (84.3) |
| Paediatric | 33 (6.0) |
| Both | 50 (9.1) |
| Missing | 3 (0.6) |
Figure 2.
The global distribution of survey respondents. Map colours indicate the number of rheumatologists who answered the survey, with increasing darkness corresponding to higher numbers of respondents.
A sizeable proportion of rheumatologists (19%) estimated that at least a quarter of their patient cohort are from below the poverty line (USA: 23%, Europe: 6%, India: 14%, Other: 37%); others had a few patients living below the poverty line while 10% did not know. Similarly, 11% estimated that more than a quarter of their patients were food insecure while 15% did not know. Of note, estimates of food insecurity were significantly lower from European respondents compared with other countries (USA: 12%, Europe: 2%, India: 8%, Other: 37%). When asked about patient health literacy, 26% of all rheumatologists believed that a quarter of their patients had low health literacy. Estimates of low health literacy were significantly higher from Indian respondents and those from ‘Other’ countries, compared to the USA and Europe (USA: 28%, Europe: 14%, India: 43%, Other: 41%).
Respondents were given several answer choices to the question ‘How have you changed your outpatient practice since the COVID-19 pandemic?’. Only 2% reported making no changes, 34% postponed all visits, 26% postponed follow-up visits, 68% were seeing only urgent patients and 82% changed to seeing patients via telehealth video consultations. Some respondents also provided qualitative answers (table 2). Despite many practices switching from in-person consultations to telehealth video, 17% rheumatologists estimated that more than a quarter of their patients may not have access to telehealth video if they needed to contact their physician. This was frequently reported by the respondents (28%) who had estimated a quarter of their patient cohort as being below the poverty line.
Table 2.
Qualitative questions and responses provided in the survey
| Question | Rheumatologists responses and quotations |
|---|---|
| Are your patients having problems with access to their medications, other than hydroxychloroquine/chloroquine, because of the pandemic? | ‘Travel restrictions’ ‘Transportation issues’ ‘Movement restrictions because of lockdown’ |
| ‘Delay in getting applications approved for biologics by government’ | |
| Do you believe rheumatic patients from racial/ethnic minority groups will do worse in the pandemic? | ‘Certain rheumatic conditions tend to cause worse disease in specific ethnicities and I worry about COVID in those patients and them not reaching out when they should’ |
| ‘Data would suggest so, but this is confounded by socioeconomics best to my knowledge which gets into a different discussion on social determinants of health etc.’ | |
| Do you believe rheumatic patients from lower SES will do worse in the pandemic? | ‘Yes, close living quarters or urban areas can increase risk of transmission’ |
| ‘Lack empowerment to seek care, or distrust of the medical system’ | |
| ‘I worry they will not seek care out when needed’ | |
| ‘Less access to self-protection. i.e. masks’ | |
| ‘Yes, in general they have a more difficult time financially, more single moms, more crowded homes’ | |
| ‘Higher proportion of multiple comorbid conditions in the lower socioeconomic groups’ | |
| ‘Due to loss of medical insurance from loss of employment’ | |
| Do your concerns for your patients vary depending on their social or SES? | ‘Yes, concerned as these patients are less able to effectively socially distance’ |
| ‘Patients who live in large groups, or live in transient housing, or experiencing homelessness.. I worry about this a lot actually’ | |
| ‘Yes, because they are unable to quit their job as they need the money’ | |
| ‘These patients are less concerned because they don’t understand due to lower health literacy’ | |
| ‘Patients who cannot restrict their movement/socially distance because of work requirements: childcare providers, janitors, cashiers’ |
SES, socioeconomic status.
When rheumatologists were asked whether their patients were having problems with access to immunosuppressive medications (other than hydroxychloroquine/chloroquine) as a result of the pandemic, 46% denied this. Of those who did report problems with medication access, 27% said their patients were not going to pick up medications for fear of getting COVID-19; 15% did not have someone to retrieve their medications for them; 36% said that either their pharmacy had shut down or had run out of medications; and 16% believed their patients had encountered financial constraints, perhaps due to loss of employment and/or insurance during the pandemic. A selection of quotes on this topic are summarised in table 2.
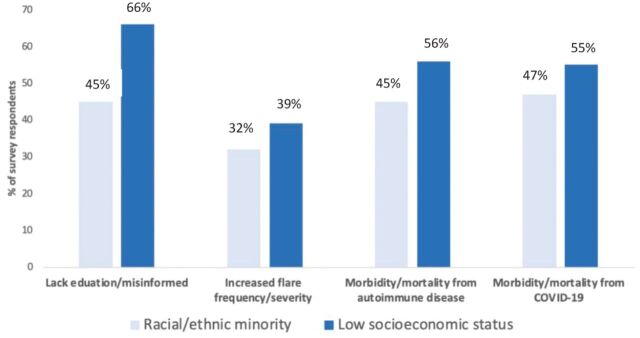
Approximately 28% of rheumatologists responded that more than a quarter of their patients were from a minority racial or ethnic group. When asked ‘Do you believe rheumatic patients who come from a minority racial or ethnic group will do worse in the context of the pandemic?’, 82% of rheumatologists believed that they may do worse. Furthermore, 45% of these respondents considered this due to either lacking education or being misinformed about COVID-19; 32% believed that they may have increased frequency or severity of flares; 45% believed that they may have increased morbidity or mortality from their underlying disease; and 47% believed that they may have increased morbidity or mortality from COVID-19 if infected (figure 3). Select qualitative answers are summarised in table 2.
Figure 3.
Reasons perceived by rheumatologists for worse outcomes in low socioeconomic and racial/ethnic minorities.
Rheumatologists were subsequently asked if they believed their patients wih low SES would do worse if they contracted COVID-19. A higher percentage of rheumatologists (92%), in contrast to the previous question, believed these patients may do worse. Furthermore, more respondents stated that patients may lack education or have misinformation (66%); may have increased frequency or severity of flares (39%); may have increased morbidity or mortality from their underlying disease (56%); and may have increased morbidity or mortality from COVID-19 if they get infected (55%) (figure 3). Additionally, qualitative answers were given, such as ‘Lack empowerment to seek care, or distrust of the medical system’, and others are provided in table 2. Most rheumatologists were concerned for their patients of low SES (91%); specifically, they were concerned about patients living alone (56%); patients living with an elderly person (66%); patients with poor access to technology and the internet (58%); patients who have lost employment during the pandemic (61%); patients with poor access to medical care (55%); and patients with poor access to transportation (55%). Again, qualitative answers, for example, ‘Yes, concerned, as these patients are less able to effectively socially distance’, are reported in table 2.
DISCUSSION
In this worldwide survey of rheumatologists conducted during the COVID-19 pandemic, respondents notably shared concerns of food insecurity, low health literacy, worsening poverty and factors that preclude social distancing such as working and dense housing conditions among their patients. Ninety-eight per cent of rheumatologists have made practice changes, with 82% now using telehealth. Despite this significant change in healthcare delivery, 17% of respondents reported that at least a quarter of their patients may not have access to telehealth video, particularly those below the poverty line. Rheumatologists shared concern particularly for their patients from racial/ethnic minority and low SES groups, and these concerns seem to be greater for patients of low SES.
This survey confirms that in response to the pandemic, a vast majority of rheumatologists are implementing practice changes, for instance, delayed non-urgent and new patient visits, routine injections are postponed and many urgent consults are conducted via telehealth video. Similar changes have been reported in other subspeciality and medical practices globally.13–15 This not only reflects efforts from rheumatologists to increase, or at least sustain, medical access for their patients during this time but also the actions of health systems which rapidly implemented a regulatory framework to authorise, integrate and reimburse telehealth video services.16 To access telehealth video, patients must have access to either telephone or internet access with a device, as well as knowledge on how to manoeuvre the online healthcare system. While many patients are able to benefit from this rapid shift in medical practice, it is important to note that our data indicate that patients who are below the poverty line may not have access to telehealth video and subsequently their rheumatologists. This lack of access might be associated with worse outcomes as perceived by rheumatologists, especially for patients with autoimmune diseases who are differentially represented in vulnerable communities. Inequalities in access to digital technology already existed, yet the COVID-19 crisis has exacerbated this disparity dramatically.17 18 The inability to access technology and subsequently vital healthcare represents a major risk factor of vulnerability during this pandemic.
There is growing and undeniable evidence that COVID-19 affects patients from racial and ethnic minority and low SES groups.1–3 Certain autoimmune diseases, such as lupus, are more prevalent in these vulnerable populations and have worse outcomes, regardless of a global pandemic.19–21 Concerns of health illiteracy, increasing food insecurity and worsening poverty have become prominent, globally, during the COVID-19 pandemic.22 23 The evidence from our survey reveals that rheumatologists share similar concerns for their patients. Patients with autoimmune disease are at higher risk not only for infection with COVID-19 but also of the morbidity that ensues, and therefore health literacy (understanding the risks and preventative measures) is especially crucial.11 Rheumatologists must partner with other patient care providers, policymakers, community leaders and others to help address the problem of low health literacy.
A majority of rheumatologists in our survey believe that patients from minority racial or ethnic groups as well as low SES groups will do worse during the COVID-19 pandemic. Interestingly, rheumatologists universally seem to be more concerned about their patients of low SES than those from racial and ethnic minorities. The greater concern for patients of low SES might be due to the global nature of the study and the widespread economic impact COVID-19 is causing. Additionally, racial and ethnic minorities refer to different populations in different countries, making it difficult for some respondents to identify and categorise these in the context of the survey questions. Furthermore, the economic disruption caused during this pandemic has been immense. Rates of unemployment have increased globally,24 differentially affecting those already in lower socioeconomic classes and low-income countries. In addition, vulnerable populations are more likely to have low-paying jobs that do not accommodate work from home options, social distancing, provide health insurance or paid medical leave.25 It is important to be aware of these factors affecting vulnerable populations to develop informed policies to target resources and ensure equity.
There important limitations to consider. First, we conducted an online survey, which was advertised through social media and email campaigns, and it is impossible to estimate how many rheumatologists had seen the survey and had the opportunity to participate; as a result, response rates cannot be measured. Second, this was a convenience sample; therefore, selection bias might be present because we have larger representation from certain countries and academic practices. Third, 65% of respondents were currently in training or within the first 10 years of rheumatology practice. This age group of physicians may be more likely to respond to a survey sent via social media and the internet, therefore perhaps reflecting a respondent bias. Lastly, nations vary with regards to minority groups and those below the poverty line; therefore, making generalisations might be difficult. However, a great strength of this study is the large number of respondents and representation from 64 diverse countries-including both low- and high-income countries.
In summary, in this global survey of rheumatologists during the initial peak of the COVID-19 pandemic, there was a shared concern for patients with rheumatic disease who suffer from food insecurity, low health literacy and worsening poverty. While 82% of rheumatologists were using telehealth video, access to it seemed to be a challenge among patients living below the poverty line. Vulnerable patients with autoimmune disease from racial/ethnic minority and low SES groups are perceived to have poor outcomes during the pandemic by their rheumatologists. Thus, it is important to understand the systemic factors affecting vulnerable patients, particularly in minority and low SES groups, to engage on an individual and on a community level to minimise inequities through advocacy and healthcare policies. Lastly, rheumatologists need to be vigilant and proactive about caring for these vulnerable patients during, and in the aftermath of the pandemic. This proactive care, for instance, might include prioritisation of the vaccination for these high-risk patients when one becomes available.
Acknowledgments
The authors greatly appreciate the assistance of the following colleagues in helping with survey edits and distribution (alphabetically listed): Medha Barbhaiya, Mary Crow, Paul DeMarco, Avinash Jain, Catherine MacLean, Lisa Mandl, Bhowmik Meghnathi, Sapan Pandya, Diyu Pearce-Fisher, Linda Russell, Jonathan Samuels, Haley Tornberg and Grace Wright. The authors would like to acknowledge the following groups: Department of Rheumatology, Hospital for Special Surgery, USSONAR (Ultrasound School of North American Rheumatologists), Indian Rheumatology Association, Association of Women in Rheumatology and Wisconsin Rheumatology Association. The authors would also like to acknowledge the participation of all the rheumatologists who graciously responded to the survey and to those who have been battling COVID-19 with courage and fortitude.
Footnotes
Contributors: BM, CM, SI, SMG, ARB: concept, data collection, data analysis and interpretation, writing, supervision. DJ-K, MF, CM, VA, AG: data collection, data analysis and interpretation, writing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: SI receives grant funds from the National Institute of Arthritis and Musculoskeletal and Skin Diseases; SMG grants and personal fees from Novartis—consulting/research support, Pfizer—consulting/research support, BMC Musculoskeletal Disorders—editorial board and Horizon—research support; DJ-K owns stocks in the following companies: Cytodyn, Walgreens, AstraZeneca. All other authors have declared that no competing interests exist.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplemental information.
REFERENCES
- 1.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA 2020;323:2192 10.1001/jama.2020.7197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med 2020;8:547–8. S2213-600(20)30228-9 10.1016/S2213-2600(20)30228-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID-19 report - intensive care national audit and research center. Available https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports (accessed 2 Jun 2020)
- 4.Dyer O. COVID-19: black people and other minorities are hardest hit in US. BMJ 2020;369:m1483 10.1136/bmj.m1483 [DOI] [PubMed] [Google Scholar]
- 5.Moore N. In Chicago, COVID-19 is hitting the black community hard. National Public Radio 6 April 2020. Available https://www.npr.org/sections/coronavirus-live-updates/2020/04/06/828303894/in-Chicago-COVID-19-is-hitting-the-black-community-hard
- 6.Mapped: how coronavirus death toll has hit the poorest areas hardest. Available https://www.telegraph.co.uk/news/2020/05/01/coronavirus-death-toll-double-poorest-areas-ons-statistics-reveal/ (accessed 4 Jun 2020)
- 7.COVID-19 will hit the poor hardest. Here’s what we can do about it. Available https://blogs.worldbank.org/voices/COVID-19-will-hit-poor-hardest-heres-what-we-can-do-about-it (accessed 4 Jun 2020)
- 8.Greenberg JD, Spruill TM, Shan Y, et al. Racial and ethnic disparities in disease activity in patients with rheumatoid arthritis. Am J Med 2013;126(12):1089–98. 10.1016/j.amjmed.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Putrik P, Ramiro S, Keszei AP, et al. Lower education and living in countries with lower wealth are associated with higher disease activity in rheumatoid arthritis: results from the multinational COMORA study. Ann Rheum Dis 2016;75(3):540 10.1136/annrheumdis-2014-206737 [DOI] [PubMed] [Google Scholar]
- 10.Yelin E, Trupin L, Yazdany J. A prospective study of the impact of current poverty, history of poverty, and exiting poverty on accumulation of disease damage in systemic lupus erythematosus. Arthritis Rheumatol 2017;69:1612–22. 10.1002/art.40134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gianfrancesco M, Hyrich KL, Al-Adely S, et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 global rheumatology alliance physician-reported registry. Ann Rheum Dis 2020 10.1136/annrheumdis-2020-217871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Data from the COVID-19 global rheumatology alliance global registry. Available https://rheum-COVID.org/updates/combined-data.html (accessed 14 Sep 2020)
- 13.Blue R, Yang AI, Zhou C, et al. Telemedicine in the era of COVID-19: a neurosurgical perspective. World Neurosurg 2020. 10.1016/j.wneu.2020.05.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barney A, Buckelew S, Mesheriakova V, et al. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health 2020;67:164–71. 10.1016/j.jadohealth.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med 2020;382:1679–81. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 16.Contreras CM, Metzger GA, Beane JD, et al. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg 2020;1–6. 10.1007/s11605-020-04623-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beaunoyer E, Dupéré S, Guitton MJ. COVID-19 and digital inequalities: reciprocal impacts and mitigation strategies. Comput Hum Behav 2020;111:106424. 10.1016/j.chb.2020.106424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray KN, Mehrotra A, Yabes JG, et al. Telemedicine and outpatient subspecialty visits among pediatric Medicaid beneficiaries. Acad Pediatr 2020;20:642–51. S1876-2859(20)30164-9 10.1016/j.acap.2020.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molokhia M, McKeigue P. Risk for rheumatic disease in relation to ethnicity and admixture. Arthritis Res 2000;2:115–25. 10.1186/ar76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MGG P-L, Greisinger A, Richardson M, et al. Determinants of treatment adherence in ethnically diverse, economically disadvantaged patients with rheumatic disease. J Rheumatol 2005;32:913–9. https://www.jrheum.org/content/32/5/913.long [PubMed] [Google Scholar]
- 21.Demas KL, Costenbader KH. Disparities in lupus care and outcomes. Curr Opin Rheumatol 2009;21:102–9. 10.1097/BOR.0b013e328323daad [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loopstra R. Vulnerability to food insecurity since the COVID-19 lockdown. The Food Foundation, 2020. [Google Scholar]
- 23.Niles MT, Bertmann F, Belarmino EH, et al. The early food insecurity impacts of COVID-19. medRxiv 2020. 10.1101/2020.05.09.20096412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coronavirus hits jobs, millions face unemployment and poverty. Available https://www.trtworld.com/magazine/coronavirus-hits-jobs-millions-face-unemployment-and-poverty-35294 (accessed 4 Jun 2020)
- 25.COVID-19 is hitting black and poor communities the hardest, underscoring fault lines in access and care for those on margins. Available https://theconversation.com/COVID-19-is-hitting-black-and-poor-communities-the-hardest-underscoring-fault-lines-in-access-and-care-for-those-on-margins-135615 (accessed 2 Jun 2020)