Abstract
A 76-year-old man with dyspnea (initial prostate-specific antigen [PSA]: 216 ng/mL) underwent 18F-FDG PET/CT, with uptake in the prostate, lymph nodes, fifth thoracic vertebra (T5), and cricoid cartilage. A biopsy revealed prostate adenocarcinoma (Gleason score 4 + 5, cT4 N1 M1). On initiation of combined androgen blockade therapy, PSA value decreased. However, 4 years later, in a castration-resistant state (PSA 2.14 ng/mL), CT and bone scintigraphy revealed a duodenal tumor and T5 metastasis. 18F–prostate-specific membrane antigen–1007 PET/CT showed uptake in the already known T5 metastasis (SUVmax, 33.55) and even in the duodenal tumor (16.55). The latter was histologically diagnosed as duodenal adenocarcinoma.
Key Words: cricoid cartilage, duodenum adenocarcinoma, FDG, PCa, PSMA-1007
FIGURE 1.
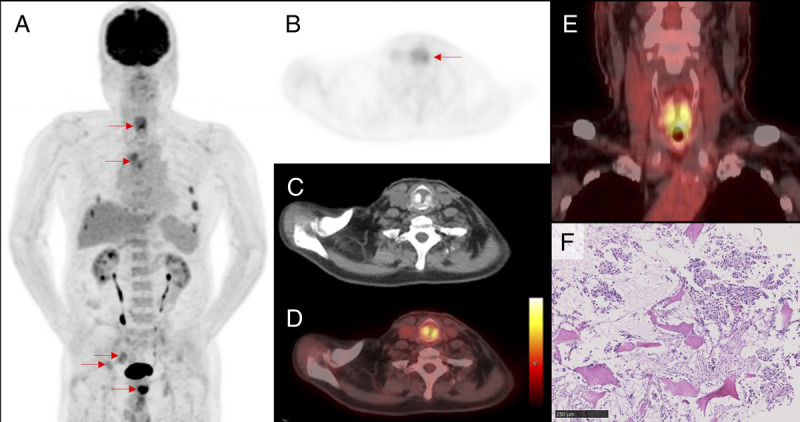
A 76-year-old man presented with dyspnea due to subglottic stenosis around cricoid cartilage (initial prostate-specific antigen [PSA], 216 ng/mL). 18F-FDG PET/CT was performed, revealing uptake in the prostate (SUVmax, 19.23), pelvic lymph nodes (SUVmax, 4.97), thoracic vertebra (T5) (SUVmax, 5.57), coxal bone (SUVmax, 3.75), cricoid cartilage (SUVmax, 6.97), and rib bone fractures. Biopsy revealed prostate adenocarcinoma with metastasis to cricoid cartilage (PSA-positive adenocarcinoma on immunohistochemistry). Maximum intensity projection image (A), the axial PET (B), CT (C), fused PET/CT (D), coronal fused PET/CT (E), and cricoid cartilage hematoxylin-eosin microphotograph (F) are shown. Few cases have been reported with neck metastases from prostate carcinoma. As for laryngeal metastases, only 13 cases have been reported as of 2001 in the literature, and 1 case was reported in 2018.1,2 Recently, 18F-fluorocholine PET and 68Ga–prostate-specific membrane antigen (PSMA) PET/CT detected cricoid or thyroid cartilage metastases from prostate adenocarcinoma.3,4
FIGURE 2.
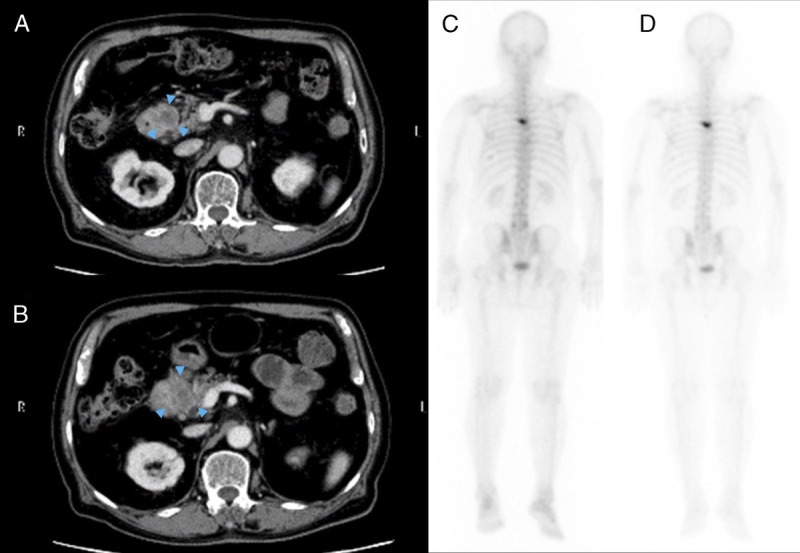
Four years later, the patient was diagnosed as a castrate-resistant state (PSA 2.14 ng/mL); the contrast-enhanced CT (A) revealed a mass at the descending portion of the duodenum. Three months after treatment with enzalutamide, the mass increased in size against PSA decrease (PSA 0.21 ng/mL) (B). (Arrowheads in A and B indicate the duodenal tumor.) T5 metastasis showed no significant change in bone scintigraphy after the enzalutamide treatment (C, D). On the other hand, the continued growth of duodenal tumor caused bile duct obstruction (not shown). Because metastasis of prostate cancer to small intestine is very rare, primary cancer or another kind of tumor was suspected but not diagnosed definitely.5–9 It was necessary to exclude the metastasis of prostate cancer for the treatment policy decision.
FIGURE 3.
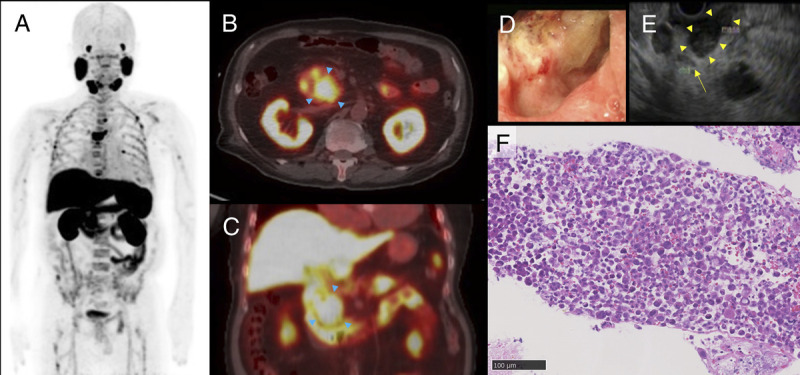
Six weeks later, to evaluate the state of metastatic castration-resistant prostate carcinoma and the duodenal tumor (PSA 0.02 ng/mL), he underwent 18F-PSMA-1007 PET/CT followed by endoscopic ultrasound (EUS)–guided fine-needle aspiration. Maximum intensity projection image (A), the axial and coronal fused PET/CT images (B, C), the endoscopic image (D), and the EUS image (E) are shown. 18F-PSMA-1007 PET/CT revealed abnormal uptake in the T5 bone metastasis (SUVmax, 33.55) and the duodenal tumor (SUVmax, 16.55), as well as physiological uptake in the hepatobiliary and intestinal tract. According to the EUS findings (E), the common bile duct (arrow) was located away from the duodenal tumor (arrowheads), indicating that the latter did not originate from the bile duct or pancreas. Histological examination revealed duodenal adenocarcinoma (F: hematoxylin-eosin stain microphotograph) negative for PSA on immunohistochemistry (not shown). As previously reported, some tumors other than prostate cancer can be positive on PSMA PET, such as brain metastases from breast cancer, glioblastoma recurrence, thyroid adenoma, and other benign lesions.10–13 When we find high uptake of 18F-PSMA-1007 in an isolated rapidly growing tumor, we should pay attention to the possibility of mimicking metastasis from prostate cancer.
Footnotes
Conflicts of interest and sources of funding: none declared.
Contributor Information
Fumihiko Soeda, Email: soeda@tracer.med.osaka-u.ac.jp.
Hiroki Kato, Email: kato@tracer.med.osaka-u.ac.jp.
Motohide Uemura, Email: uemura@uro.med.osaka-u.ac.jp.
Norio Nonomura, Email: nono@uro.med.osaka-u.ac.jp.
REFERENCES
- 1.Prescher A Schick B Stütz A, et al. . Laryngeal prostatic cancer metastases: an underestimated route of metastases? Laryngoscope. 2002;112(8 Pt 1):1467–1473. [DOI] [PubMed] [Google Scholar]
- 2.Olvera M Delgado M Vázquez M, et al. . Unusual presentation of prostate cancer metastatic to the cricoid cartilage and oral cavity. Case Rep Med. 2018;2018:5207204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng SJ Sinha AK Loi HY, et al. . Asymptomatic metastasis to cricoid from prostate carcinoma: an incidental finding detected on 18F-choline PET/CT. Jpn J Radiol. 2015;33:298–301. [DOI] [PubMed] [Google Scholar]
- 4.Tupalli A Damle NA Thankarajan AS, et al. . An unusual case of simultaneous cricoid and thyroid cartilage metastases from prostatic adenocarcinoma on 68Ga-PSMA PET/CT. Nucl Med Mol Imaging. 2020;54:61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malhi-Chowla N Wolfsen HC Menke D, et al. . Prostate cancer metastasizing to the small bowel. J Clin Gastroenterol. 2001;32:439–440. [DOI] [PubMed] [Google Scholar]
- 6.Lee SW Lee TY Yeh HZ, et al. . An unusual case of metastatic small intestinal tumor due to prostate cancer. J Chin Med Assoc. 2009;72:271–274. [DOI] [PubMed] [Google Scholar]
- 7.Fidan S, Kocak G, Fidan E. An unusual metastasis of prostate cancer to duodenum. J Coll Physicians Surg Pak. 2016;26:133–134. [PubMed] [Google Scholar]
- 8.Minardi AJ Jr Zibari GB Aultman DF, et al. . Small-bowel tumors. J Am Coll Surg. 1998;186:664–668. [DOI] [PubMed] [Google Scholar]
- 9.DiSario JA Burt RW Vargas H, et al. . Small bowel cancer: epidemiological and clinical characteristics from a population-based registry. Am J Gastroenterol. 1994;89:699–701. [PubMed] [Google Scholar]
- 10.Tang K Wang Z Lin J, et al. . Hürthle cell thyroid adenoma showing avid uptake on 18F-PSMA-1007 PET/CT. Clin Nucl Med. 2020;45:223–224. [DOI] [PubMed] [Google Scholar]
- 11.Marafi F Sasikumar A Alfeeli M, et al. . 18F-PSMA 1007 uptake in brain metastases from breast cancer. Clin Nucl Med. 2020;45:e77–e79. [DOI] [PubMed] [Google Scholar]
- 12.Marafi F Sasikumar A Fathallah W, et al. . 18F-PSMA 1007 brain PET/CT imaging in glioma recurrence. Clin Nucl Med. 2020;45:e61–e62. [DOI] [PubMed] [Google Scholar]
- 13.Panagiotidis E Paschali A Giannoula E, et al. . Rib fractures mimicking bone metastases in 18F-PSMA-1007 PET/CT for prostate cancer. Clin Nucl Med. 2019;44:e46–e48. [DOI] [PubMed] [Google Scholar]


