Abstract
Background:
Surgical treatment of ear carcinomas needs the selection of the appropriate reconstructive techniques, which depends on the location and the dimensions of the defect after excision of the cancer and the quality of blood supply to the peri-lesional skin.
The aim of this study was to evaluate the efficacy and reliability of a new axial island retroauricular flap (middle-retroauricular island flap M-RIF) for coverage of non-helical ear defects with direct donor site closure.
Methods:
All patients, from January 2013 to January 2020, with skin tumors of the non-helix region and undergoing a combined skin-cartilage excision with M-RIF local flap reconstruction under local anesthesia, were enrolled in the study.
Results:
18 patients (14 men and 4 women) underwent auricle skin-cartilage excision and M-RIF flap reconstruction. The mean age was 65 years (range, 60–85); the type of primary lesions were 12 BCC and 6 SCC. One flap wound dehiscence and one donor site infection and partial necrosis of the posterior auricular skin occurred; no other complications were recorded.
Conclusions:
The M-RIF flap is a valid surgical option when dealing with non-helical defects of the anterior pinna. It allows the reconstruction of the defect of the entire anterior surface of the auricle apart from the helix and the lobe and primary donor site closure.
INTRODUCTION
Surgical excision of skin tumors of the face is challenging because it requires both a complete removal of cancer and the best possible cosmetic outcome. The external ear is continuously exposed to UV rays and the recurrence rates on the ear itself, among all facial regions, are critical. Due to poor visual control and its complex 3D aspect, the cancer diagnosis of the auricle happens late, when the cancer has invaded the underlying cartilage.
The external ear is essential for hearing and for the aesthetics of the face but is challenging to reconstruct. Surgical treatment of ear carcinomas carries a high risk of local recurrence and requires careful preoperative planning, often a multidisciplinary approach, and mastering of all reconstructive techniques.
The selection of the appropriate reconstructive techniques depends on the location and the dimensions of the defect after excision of the cancer and the quality of blood supply to the peri-lesional skin. Primary donor closure is preferable but often not possible. The defect can be left to heal by secondary intention. However, the risks of infection, over a prolonged healing time, are high. A skin graft is another possibility, but we rarely use it because generally, the radical excision requires perichondral removal.1
Moreover, in the case of extensive cartilage resection, it does not provide sufficient structural support with additional morbidity of the donor site. Several local flaps from the anterior or posterior aspect of the auricle have been described. When possible, surgeons prefer to use the retroauricular flaps, thanks to their donor region hiding the scar. The donor region, called either the posterior auricular, postauricular or retroauricular, is composed of the skin of the posterior external ear, the retro-auricular groove, and the skin covering the mastoid.2
We used the classification of the retroauricular flaps for the reconstruction of the defects of the external ear according to their vascularity deriving from the posterior auricular artery (PAA).3 This study aims to evaluate the efficacy and reliability of a new axial island retroauricular flap, for coverage of non-helical ear defects with direct donor site closure.
PATIENTS AND METHODS
All patients, from January 2013 to January 2020, with skin tumors of the concha, ante-helix, or triangular fossa and undergoing a combined skin-cartilage excision with local flap reconstruction under local anesthesia, were enrolled in the study. In all cases, patients were previously evaluated by a dermatologist and then referred to the Plastic Surgery Unit. No antibiotics were administered.4 The anterior sutures were removed at 7 days and the posterior ones 14 days after surgery.
Surgical Anatomy
Considering the sagittal plane, the external ear is composed of an anterior and a posterior surface. Its medial part is attached to the head, and the lateral margins are free. The anterior surface is concave and can be divided into several anatomic subunits: helical rim, ante-helix, tragus, antitragus, triangular fossa, concha, ear lobule, and external auditory canal.
The posterior surface is convex with thicker subcutaneous layer that gives more elasticity and laxity to retro auricular tissues. The vascular supply of the retro auricular region comes from numerous vessels arising from the posterior auricular artery that divides in an upper, middle, and lower branch.5
The direction of these branches assures a horizontal vascular path toward the helix, from the medial to the lateral aspect of the posterior external ear. The number of PAA branches varies, ranging from 2 to 4, but the presence of the middle branch is constant.6
Surgical Technique
The middle-retroauricular island flap (M-RIF) was planned and harvested based on the middle branch of the PAA (Fig. 1). By pulling the ear outward, the markings are drawn, as per the otoplasty, in an fusiform shape, based on the middle medial branch of the PPA, with its long axis parallel to the posterior retroauricular groove and a small, superficial, perpendicular incision (Fig. 2), on the cutaneous projection of the vascular pedicle, in direction of the mastoid. The feeding artery can be quickly identified with trans-illumination (Fig. 3).
Fig. 1.
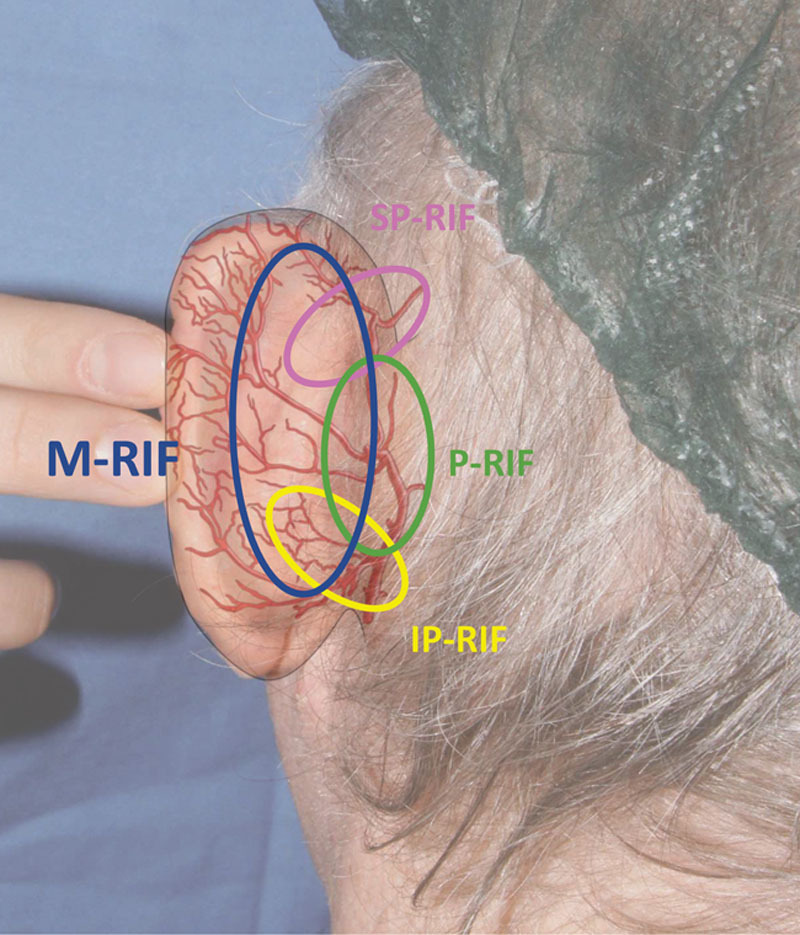
Schematic drawing of different flaps in the retroauricular area based on PAA vascularization (in red). P-RIF, perforator retroauricular island flap; IP-RIF, inferior pedicle retroauricular island flap.
Fig. 2.
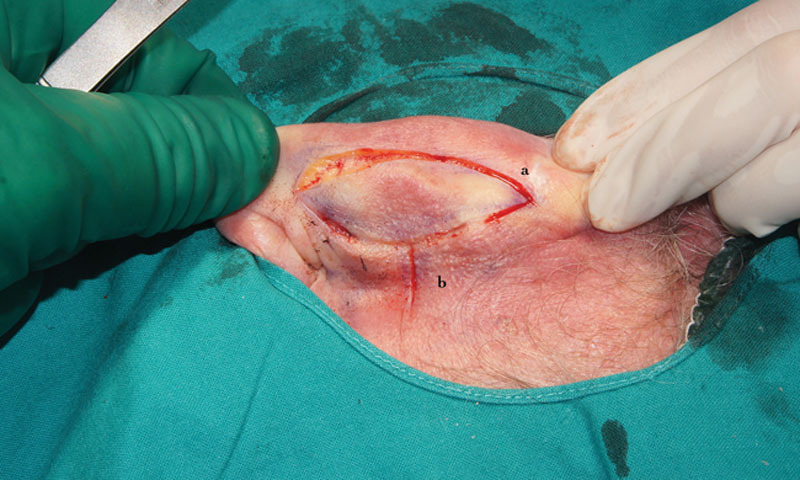
Flap incisions. a, Elliptic (otoplasty) incisions parallel to the retro auricular groove. b, Short perpendicular incision corresponding to the course of the middle branch of the retro auricular artery.
Fig. 3.
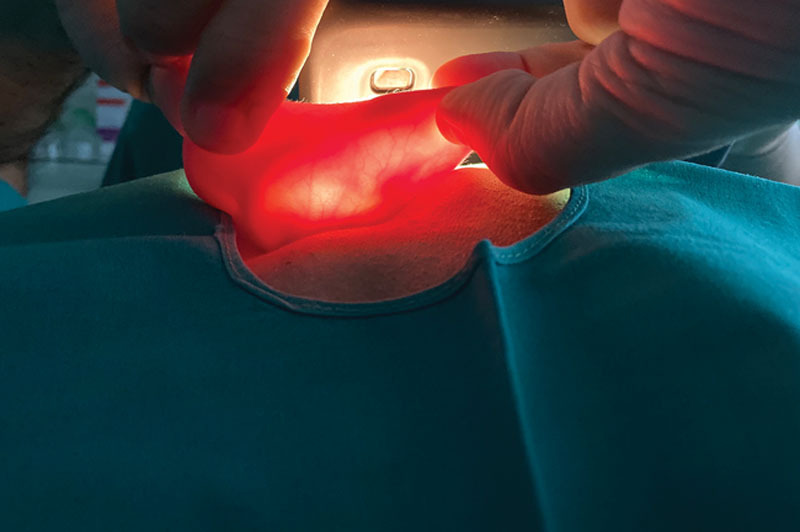
Trans-illumination of the auricle: note the branches of the PAA running perpendicular to the retroauricular groove and the PAA.
First, the skin cancer was excised with 4-mm clear margins around the tumor. All defects in this series were composed of skin and cartilage, and all the specimens sent for a histopathologic analysis.
The first (initial) posterior flap incision is the lateral one; it is profound, reaching the cartilage plane. On the medial side, the incision is shallow, going deep only in the cutaneous plane, paying attention not to injure the vascular pedicle, followed by a careful dissection of the delicate thin tissues (Fig. 4).
Fig. 4.
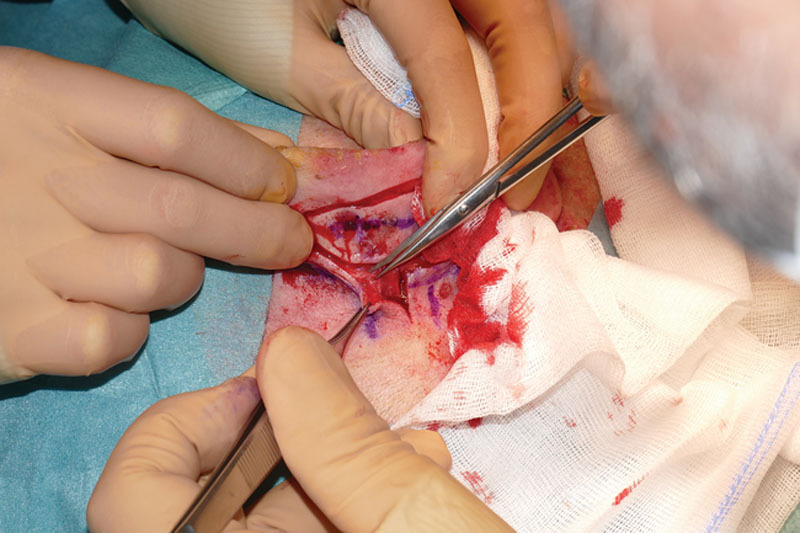
Intra-operative detail: subcutaneous pedicle dissection.
On the anterior surface of the ear, the dissection of the profound aspect of the pedicle can be performed bluntly until we cut the cartilage branch at a point cephalic to the ponticulus of the auricula. A through-and-through defect is created, and with the ear pushed back, the island flap becomes visible. When the flap is attached only by its pedicle, the skin island is pulled through the full-thickness defect with hooks or forceps and positioned on the anterior surface of the auricle (Fig. 5). The flap can be transferred in two ways: “revolving door” or “twisted.” The revolving door movement, also called “flip-flop,” is a transposition flap that turns by 180 degrees on its long axis with the medial posterior margin becoming the anterolateral one (Fig. 6). By twisting the flap on its minor axis, the superior side of the retroarticular flap becomes, on the anterior surface, the inferior part of the defect.
Fig. 5.
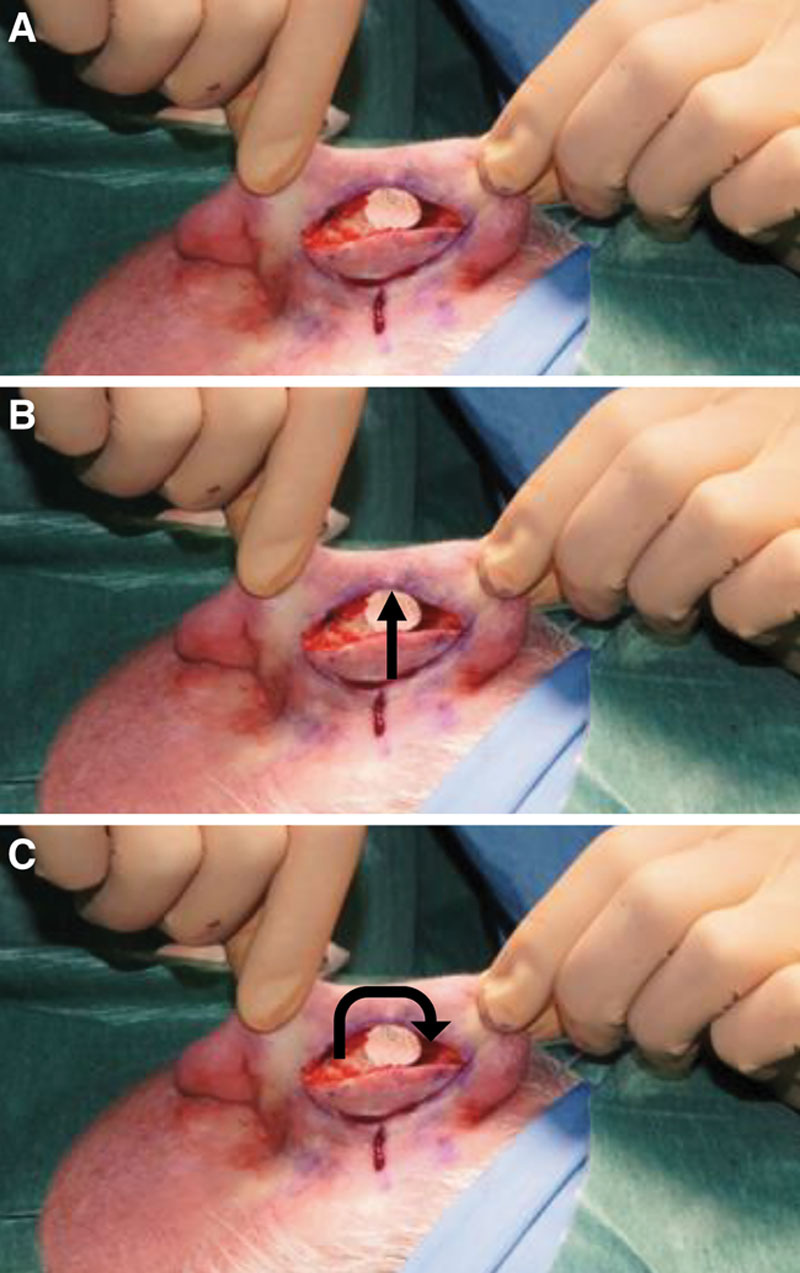
M-RIF flap transposition. A, Intra-operative detail: M-RIF flap before transposition into the full thickness defect after en-bloc cancer excision. The type of movement that can be performed is indicated by arrows: a rotation on the long axis with a “flip flop” movement (B) while the twisted movement (C) can be performed rotating the flap on its minor axis.
Fig. 6.
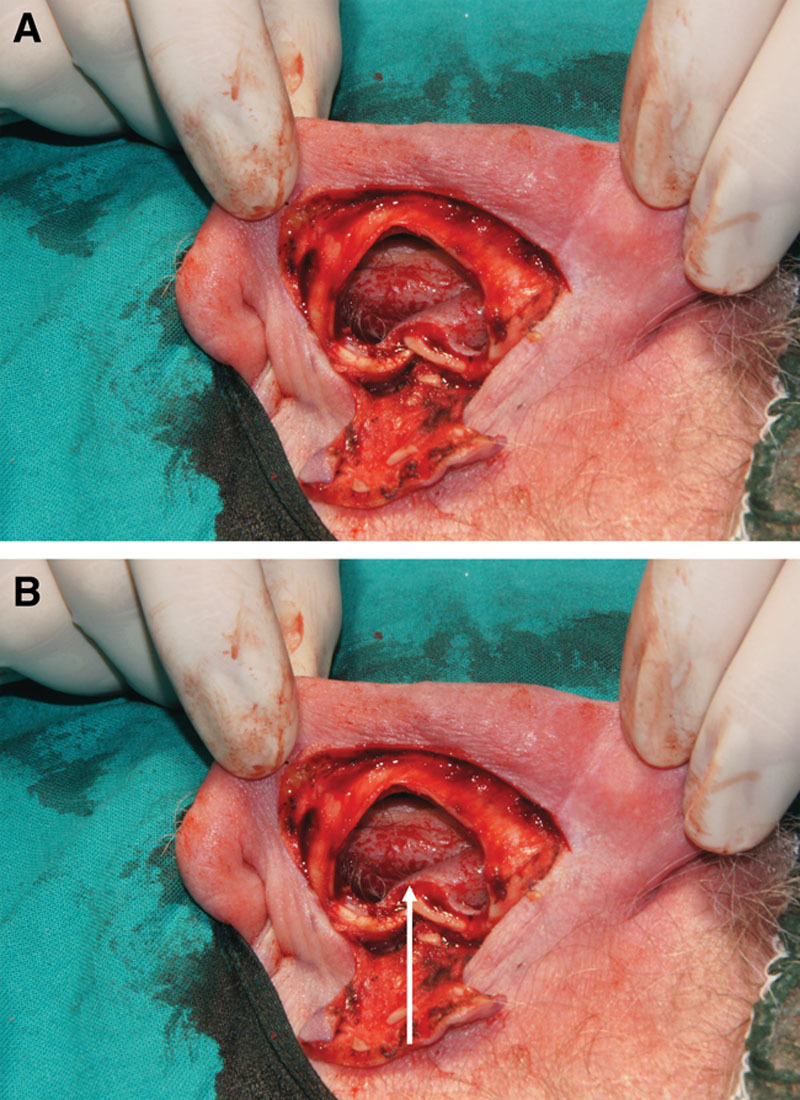
M-RIF flap before transposition. Note: the distal posterior flap margin becomes the medial anterior one (arrow).
The flap can be tailored to the exact dimensions of the defects and secured with interrupted sutures. Sufficient undermining of anterior defect enhances the cosmetic result by minimizing the trap door phenomenon. The preoperative otoplasty-like drawings allow for a direct donor site closure (Fig. 7).
Fig. 7.

Direct closure of the donor site.
RESULTS
From January 2014 to January 2020, 18 patients (14 men and 4 women) underwent auricle skin-cartilage excision and M-RIF flap reconstruction. The mean age was 65 years (range, 60–85); the type of primary lesions were 12 BCC and 6 SCC.
In all patients, we confirmed the radicality of the excision by histology. In 13 cases, the revolving door type movement of the flap was performed while in 5 the twisted type movement. We recorded 1 flap wound dehiscence and 1 donor site infection and partial necrosis of the posterior auricular skin; both were treated conservatively. No other complications were found (hematoma, flap necrosis, or infections) at the recipient site and only one donor wound infection was noted, which required a longer time to heal.
On the first follow-up visit, one day after surgery, 3 of the 5 twisted flaps presented a mild venous stasis that resolved spontaneously.7 The objective and subjective outcomes were considered satisfactory by both the patients and the surgeons. At the follow-up visits, we paid particular attention to the contour and shape of the auricle and the skin texture, which we judged pleasing (Fig. 8).
Fig. 8.
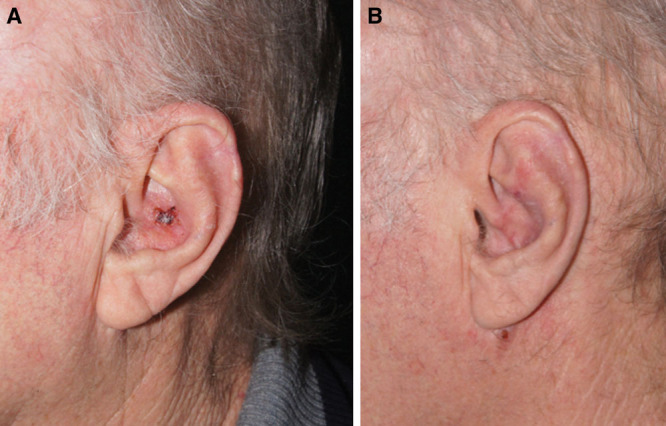
Pre and postoperative views at 4 months.
DISCUSSION
The external ear is a common location of several skin lesions, benign, pre-neoplastic, and neoplastic. The most frequent skin cancers are basal cell and squamous cell carcinoma. Basal cell carcinoma accounts for 90% of all malignant skin lesions of the head-neck district. Because of the higher exposure to ultraviolet rays, the commonly affected anatomical subunits include the helix and the preauricular region.8 Like all basal cell carcinomas, also those located on the auricle can occur in different clinical forms.9 The most frequent is the nodular-ulcerative type, which frequently invades the cartilage.
The second most frequent tumor is squamous cell carcinoma, which involves the ear in 24% of the head and neck patients. Also, in the case of squamous cell carcinoma, the most affected subunits are the helix and the ante-helix, which is the most exposed part of the external ear to actinic damage.
The high local recurrence rate requires a rather aggressive and extensive surgical removal of these tumors. An estimated 7%–14% of head and neck melanomas are found on the external ear, particularly on helix and ante-helix. The most affected are men, probably for short haircuts, with an average age of 65 years. The left ear is most frequently affected, perhaps relative to the greater exposure of this side of the body while driving.
Concha and antehelix reconstruction are challenging. Every distortion of morphology and contour of the auricle is connected to aesthetic appearance and can lead to psychological discomfort for the patient. When possible, we prefer the direct repair for soft tissue closure after tumor excision on the auricle. Taking into consideration the oncologic radicality, anatomic location, and size of the defect, we can opt also for other reconstructive options. Healing by secondary intention takes time and carries a high risk of exposed cartilage infection.
Skin grafts are widely used even though they suffer from centripetal contraction, difficult graft take also related to dressing changes, and the lack of structural support. They often involve an additional donor site.10 Skin grafting is a straightforward procedure but leaves a contour deficit because of a depression in the treated area.11 When auricular cartilage is exposed, skin grafts are indicated for coverage only in the presence of intact perichondrium or a well-vascularized recipient bed. Composite skin-cartilage grafts from the contralateral retroauricular region is another reconstructive option.
Compared with skin grafts, the local flaps present superior outcomes in terms of the morphological aspect of the external ear and a quick and easy solution with a rapid learning curve.12 Preauricular flaps are not the first choice because they can alter the local morphology, they transfer hairy skin in the non-hairy area, and they might need secondary procedures. Secondary procedures are a drawback seen also with post auricular flaps that are folded and pulled through to the anterior surface of the ear.13
The retroauricular region represents the gold standard local flap donor site because of low residual morbidity, the possibility of effectively hiding scars, donor closure by direct suturing, and because of its rich vascularization.14
Masson firstly described the island flap from behind the ear, which was popularized later by Jackson.15 The versatile revolving door island flap from the retro auricular region was surgically refined and described as P-IF (perforator island flap).16–18 The superior pedicle retro auricular island flap (SP-RIF) is vascularized through the anastomosis between the upper branch of the posterior postauricular artery (PPA) and the posterior branch of the superficial temporal artery.19
The majority of flaps from the retro auricular region, based on the PAA (eg, I-RIF), are pedicled on their vertical axis and are moved to the anterior pinna by transposition or folding, with or without de-epithelialization of the proximal part of their pedicle.20 The only flap based on the horizontal branch of the PPA, which is de-epithelialized, and uses the revolving door movement is the post auricular helix-based adipo-dermal pedicle turnover (PHAT) flap,21 which depends on the retrograde vascular network of the helix.4
The middle PAA branch retroauricular island flap (M-RIF), described in the present patient series, to date, is the first horizontally oriented constant pedicle island flap, which uses only the retroauricular skin (otoplasty-like skin incisions); it is parallel to the retro auricular groove, and allows reconstruction of the non-helical anterior surface of the ear.
The M-RIF flap, beside the well-known advantages of the previously described retroauricular flaps (the excellent texture, color match with the anterior recipient surface of the auricle and preservation of the auricle contour), can cover all defects of any size on the anterior surface of ante-helix, concha, or triangular fossa, and can be performed with local anesthetic. The other advantage of M-RIF flap is the primary donor closure avoiding the auricular pinning (frequently seen with the revolving door flap) with better cosmetic appearance (Fig. 9).
Fig. 9.

At 3 months postoperative follow up. Note: no pinning.
In our series, the majority of the M-RIF flaps were used taking advantage of the revolving door movement because, with the twisted ones, we saw more venous stasis and more need for more complex skeletonizing of the pedicle. The twisted movement remains indicated in the few cases where the anterior skin lesion is near to the helical rim, and therefore the projection of the distal incision of the flap is placed more proximal. Indeed, to avoid the deformity of the helical margin contour when we plan a revolving door movement, an additional sharp dissection of the medial cutaneous portion of the skin flap is necessary (Fig. 10); moreover, the undermining of the skin around the defect is advisable to prevent the trap door phenomenon of the flap.
Fig. 10.
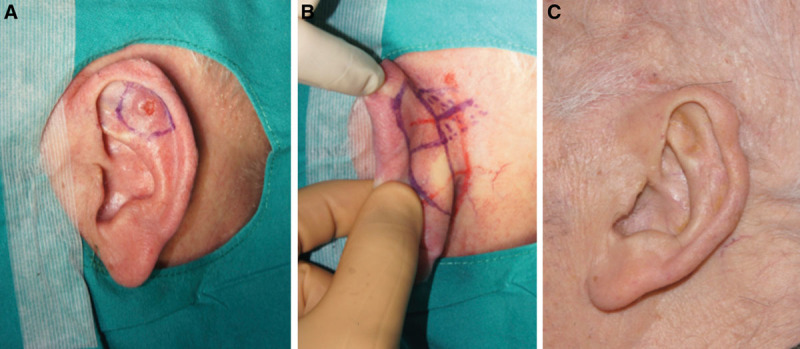
Clinical case. A, B, Preoperative markings; C, Result at 6 months postoperative.
CONCLUSIONS
The median middle PAA branch retro auricular island flap is a valid surgical option when dealing with non-helical defects of the anterior pinna. It allows the reconstruction of the defect of the entire anterior surface of the auricle apart from the helix and the lobe and primary donor site closure.
Footnotes
Published online 11 November 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
References
- 1.Stucker FJ, Jr, Shaw GY. The perichondrial cutaneous graft. A 12-year clinical experience. Arch Otolaryngol Head Neck Surg. 1992;118:287–292. [DOI] [PubMed] [Google Scholar]
- 2.Schonauer F, Vuppalapati G, Marlino S, et al. Versatility of the posterior auricular flap in partial ear reconstruction. Plast Reconstr Surg. 2010;126:1213–1221. [DOI] [PubMed] [Google Scholar]
- 3.Cordova A, D’Arpa S, Pirrello R, et al. Retroauricular skin: a flaps bank for ear reconstruction. J Plast Reconstr Aesthet Surg. 2008;61 Suppl 1:S44–S51. [DOI] [PubMed] [Google Scholar]
- 4.Mascarello M, Papa G, Arnez ZM, et al. Acute necrotizing pancreatitis related to tigecycline. J Antimicrob Chemother. 2012;67:1296–1297. [DOI] [PubMed] [Google Scholar]
- 5.Park C, Shin KS, Kang HS, et al. A new arterial flap from the postauricular surface: its anatomic basis and clinical application. Plast Reconstr Surg. 1988;82:498–505. [DOI] [PubMed] [Google Scholar]
- 6.Hénoux M, Espitalier F, Hamel A, et al. Vascular supply of the auricle: anatomical study and applications to external ear reconstruction. Dermatol Surg. 2017;43:87–97. [DOI] [PubMed] [Google Scholar]
- 7.Arnež ZM, Ramella V, Papa G, et al. Is the LICOX PtO2 system reliable for monitoring of free flaps? Comparison between two cohorts of patients. Microsurgery. 2019;39:423–427. [DOI] [PubMed] [Google Scholar]
- 8.Valdatta L, Perletti G, Maggiulli F, et al. FRAIL scale as a predictor of complications and mortality in older patients undergoing reconstructive surgery for non-melanoma skin cancer. Oncol Lett. 2019;17:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dioguardi D, Portincasa A, Giudice G, et al. Clinica, epidemiologia ed orientamento terapeutico nei tumori cutanei maligni del padiglione auricolare: dieci anni di esperienza. G Chir Plast. 19927:127–133. [Google Scholar]
- 10.Cuomo R, Grimaldi L, Brandi C, et al. Skin graft donor site: a procedure for a faster healing. Acta Biomed. 2017;88:310–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitkov M, Martinez JC. Reconstruction of a full-thickness superior auricular defect. Dermatol Surg. 2018;44:1579–1582. [DOI] [PubMed] [Google Scholar]
- 12.Dessy LA, Figus A, Fioramonti P, et al. Reconstruction of anterior auricular conchal defect after malignancy excision: revolving-door flap versus full-thickness skin graft. J Plast Reconstr Aesthet Surg. 2010;63:746–752. [DOI] [PubMed] [Google Scholar]
- 13.Roche AM, Griffin M, Shelton R, et al. The folded postauricular flap: a novel approach to reconstruction of large full thickness defects of the conchal bowl. Am J Otolaryngol. 2017;38:706–709. [DOI] [PubMed] [Google Scholar]
- 14.Masson JK. A simple island flap for reconstruction of concha-helix defects. Br J Plast Surg. 1972;25:399–403. [DOI] [PubMed] [Google Scholar]
- 15.Jackson IT, Milligan L, Agrawal K. The versatile revolving door flap in the reconstruction of ear defects. Eur J Plast Surg. 1994;17:131–133. [Google Scholar]
- 16.Krespi YP, Ries WR, Shugar JM, et al. Auricular reconstruction with postauricular myocutaneous flap. Otolaryngol Head Neck Surg. 1983;91:193e6. [DOI] [PubMed] [Google Scholar]
- 17.Talmi YP, Horowitz Z, Bedrin L, et al. Auricular reconstruction with a postauricular myocutaneous island flap: flip-flop flap. Plast Reconstr Surg. 1996;98:1191–1199. [DOI] [PubMed] [Google Scholar]
- 18.McInerney NM, Piggott RP, Regan PJ. The trap door flap: a reliable, reproducible method of anterior pinna reconstruction. J Plast Reconstr Aesthet Surg. 2013;66:1360–1364. [DOI] [PubMed] [Google Scholar]
- 19.Cordova A, D’Arpa S, Moschella F. An innervated retroauricular skin flap for total earlobule reconstruction. Br J Plast Surg. 2003;56:818–821. [DOI] [PubMed] [Google Scholar]
- 20.Chen C, Chen ZJ. Reconstruction of the concha of the ear using a postauricular island flap. Plast Reconstr Surg. 1990;86:569–572. [DOI] [PubMed] [Google Scholar]
- 21.Beustes-Stefanelli M, O’Toole G, Schertenleib P. The postauricular helix-based adipodermal-pedicle turnover (PHAT) flap: an original single-stage technique for antihelix and scapha reconstruction. Ann Plast Surg. 2016;76:57–66. [DOI] [PubMed] [Google Scholar]


