Background:
Unicompartmental and total knee arthroplasty (UKA and TKA) have demonstrated excellent mid- and long-term outcomes and have been compared in clinical series for decades; however, to our knowledge, no study has sufficiently matched UKA and TKA cohorts on preoperative osteoarthritis severity. The purpose of this study was to evaluate patient-reported outcomes of radiographically and demographically matched UKA and TKA cohorts.
Methods:
One hundred and thirty-five UKAs and 135 TKAs were matched by patient age, sex, body mass index, and American Society of Anesthesiologists Physical Status (ASA-PS) classification as well as preoperative osteoarthritis severity in medial and lateral tibiofemoral and patellofemoral compartments (Kellgren-Lawrence grading system). Patient-reported outcome measures for pain, function, activity level, and satisfaction were evaluated at minimum 1-year follow-up via components of the modern Knee Society Score, the University of California Los Angeles (UCLA) activity-level score, and a Likert satisfaction scale.
Results:
The patients in the UKA group reported significantly less pain, a higher activity level, and greater satisfaction while performing several functional activities and could walk for a longer amount of time before stopping due to knee discomfort compared with those in the TKA group (p ≤ 0.038). In addition, a greater proportion of patients in the UKA than in the TKA group were “satisfied or very satisfied” with their knee replacement surgery at minimum 1-year follow-up (90% versus 81%; p = 0.043).
Conclusions:
With minimum 1-year follow-up, patients who underwent UKA reported significantly higher function, less pain, and a greater level of patient satisfaction than a radiographically and demographically matched TKA cohort.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
While total knee arthroplasty (TKA) remains an excellent choice for treating isolated compartmental osteoarthritis, unicompartmental knee arthroplasty (UKA) has increased in popularity1. However, controversy still exists regarding the choice between TKA and UKA for patients with end-stage knee osteoarthritis within a single tibiofemoral compartment. Studies comparing TKA and UKA have demonstrated excellent mid- and long-term outcomes and have been compared in clinical series for decades. These studies have largely focused on functional scores and recovery, perioperative complications, and revision rates. The authors of a meta-analysis of available randomized controlled trials found only 3 studies published and concluded that TKA resulted in more postoperative complications but was associated with a lower revision rate compared with UKA at 5 years2. Other studies have suggested that UKA results in better range of motion, more normal knee kinematics, a lower volume of blood loss, and expedited recovery3-13. Survivorship studies show similar results between TKA and UKA14-16, but reviews and national registries continue to demonstrate higher revision rates following UKA13,17-19. The higher revision rate for UKA has been attributed by some to a lower threshold for revision from an inherent bias of having multiple unresurfaced native lateral or patellofemoral compartments, from which the pain is erroneously considered to originate20.
Most existing comparative TKA and UKA studies are potentially confounded by differences in preoperative radiographic disease patterns that represent potential selection bias based on more conservative radiographic indications for UKA. In several studies, cohorts were matched on the basis of age, sex, body mass index (BMI), and preoperative scores of function21-23. Others have minimized cofounding variables by comparing outcomes in patients who have undergone UKA and TKA in contralateral knees24-26. Some studies have attempted to match TKA and UKA cohorts radiographically; however, groups in these studies differed preoperatively by radiographic severity of osteoarthritis27 and outcome metrics obtained preoperatively28. To our knowledge, only 1 modern randomized controlled trial29 has compared medial UKA and TKA treatment arms on the basis of radiographic osteoarthritis severity. The authors found similar Oxford Knee Score values between cohorts, but UKAs were reported to be more effective with less cost at 5-year follow-up. The purpose of the current study was to compare minimum 1-year patient-reported outcome measures (PROMs) in a consecutive series of manual-technique UKAs and a radiographically and demographically matched cohort of TKAs performed by a single high-volume surgeon.
Materials and Methods
Institutional review board approval was received to retrospectively review 158 medial UKAs consecutively performed by 1 surgeon between April 2011 and March 2019. Five UKAs were excluded for the following reasons: resection due to infection prior to 1 year (1 case), conversion of UKA to TKA due to aseptic tibial loosening before 1 year (1 case), bilateral UKA (2 cases), and poor preoperative image quality (1 case). Eighteen additional cases did not have minimum 1-year follow-up outcome data and were removed from the analysis. The remaining 135 medial UKAs were matched to 135 TKAs performed during the same study period. Potential TKA matches used identical exclusion criteria.
All patients had osteoarthritis in the medial compartment and were without a history of trauma, osteotomy, or flexion deformity of >5°. The indications for UKA were based on modified Kozinn and Scott criteria30. The indications included patients with isolated medial osteoarthritis radiographically and clinically, and a lack of notable coronal or sagittal plane deformity. Obesity and lack of anterior cruciate ligament integrity were not strict contraindications to UKA. Patients with asymptomatic chondral lesions on the medial patellar facet or trochlear grove and congruent patellofemoral tracking without joint-space narrowing radiographically were not contraindicated for UKA.
Surgical Technique
All procedures were performed by a single surgeon in a suburban academic center designated for hip and knee arthroplasty. Identical perioperative and pain management protocols were used for all cases. Tranexamic acid was used for all cases and all procedures were performed without robotic assistance.
The UKA procedures were performed using an identical surgical technique, via a mini-midvastus approach and a spacer block technique with conventional instrumentation. Minimal medial release was performed to allow limb alignment to remain in slight residual varus and to avoid overcorrecting into deleterious valgus, as is the optimal standard practice in medial UKA procedures. All UKAs involved the medial compartment, with use of a cemented, fixed-bearing design (ZUK; Smith & Nephew; or Persona Partial Knee; Zimmer Biomet).
TKA procedures utilized a medial parapatellar approach and computer-assisted navigation (Stryker Navigation) for the distal bone cut. The remainder of the bone cuts were made with traditional instrumentation using a measured resection technique. All TKAs involved the use of a cemented or cementless design from 1 of 2 manufacturers (Triathlon; Stryker Orthopaedics; or EMPOWR; DJO Surgical).
Radiographic Evaluation and Matching Criteria
For all UKAs and matched TKAs, the most recent preoperative radiograph was graded (0 to 4) using the Kellgren-Lawrence (KL) grading system for osteoarthritis severity31. Standardized radiographs included weight-bearing anteroposterior, posteroanterior flexion, flexed lateral, and patellofemoral views. A single experienced rater, blinded to clinical and PROM data, graded the preoperative radiographs for osteoarthritis severity. Individual radiographic features of the medial compartment of the tibiofemoral joint (TFJ), the lateral compartment of the TFJ, the medial compartment of the patellofemoral joint (PFJ), and the lateral compartment of the PFJ were scored. Age, sex, BMI, and the American Society of Anesthesiologists Physical Status (ASA-PS) classification were compiled from the electronic medical record for all cases.
Matching criteria for demographic data were age (±7 years), sex, BMI (±7 kg/m2), and ASA-PS classification (±1). Radiographic matching criteria were KL grade (±1 for each compartment).
PROMs
PROMs in this study evaluated pain, satisfaction, function, and activity level via components of the modern Knee Society Score32, a 5-point Likert scale for satisfaction, and the University of California Los Angeles (UCLA) activity-level score. All PROMs were prospectively administered at preoperative and postoperative clinic visits, with the exception of the Likert satisfaction scale, which was administered at postoperative visits only.
Minimum 1-year follow-up for PROM data was operationally defined as ≥10 months from the date of surgery, as patients frequently have 12-month postoperative visits that are not exactly at 12 months following surgery because of personal schedules, life events, travel, etc. After exclusions, the overall data response rate was 88.2% (135 of 153) who had minimum 1-year follow-up PROM data. Previous contemporary TKA outcome studies have demonstrated no differences in PROM values between 12 and 24 months33,34. Therefore, peer-reviewed literature now accepts 1-year follow-up as the essential minimum clinical follow-up duration for PROMs and other functional measures rather than the historical 2-year follow-up that was used specifically for survivorship outcome measures.
Statistical Analysis
All statistical analyses were performed with Minitab 18. Continuous variables were analyzed with a Student 2-sample t test. A Pearson chi-square test was used to test independence among categorical variables, with Fisher exact test p values reported for 2 × 2 contingency tables. A 2-proportion test (Z value) was used to compare 2 specific proportions. A significance level of 0.05 was used for all statistical analyses.
A sample-size estimation for matched case-control cohorts35 was conducted. Using satisfaction data from current literature for UKA36 and TKA37, with power (1 − β) = 0.80, a significance level (α) of 0.05, an estimated proportional difference in UKA and TKA satisfaction (0.92 − 0.80) of 0.12, and an estimated proportional difference of “unsatisfied” patients among the control TKA group (1.0 − 0.80) of 0.20, it was estimated that the sample size for each of the matched cohorts would need to be 55, which was exceeded in both cohorts, rendering the statistical power of this study to be >80%.
Results
No significant differences in patient age, BMI, duration of follow-up (in months), sex, or ASA-PS classification were found between the medial UKA (n = 135) and TKA (n = 135) matched cohorts (p ≥ 0.158) (Table I). The KL grades in the 4 joint locations were also were similar overall between the UKA and TKA groups, but chi-square tests were invalid because of low cell counts (Table II). The lateral PFJ location showed the largest proportional difference between UKA and TKA cohorts; however, the degree of osteoarthritis severity for this location did not influence PROMs (p ≥ 0.355). The lack of statistically significant between-group differences in demographic variables and KL grades confirmed that both UKA and TKA cohorts were nearly equivalent candidates for either a UKA or TKA.
TABLE I.
Demographic Comparison
| TKA | UKA | T Value* | χ2 Value† | P Value | |
| Age‡ (yr) | 64.7 ± 8.9 (41.7-84.0) | 64.9 ± 9.5 (39.7-88.2) | 0.2 | 0.827 | |
| BMI‡ (kg/m2) | 31.5 ± 5.6 (19.4-47.0) | 30.5 ± 5.1 (18.9-44.1) | 1.4 | 0.158 | |
| Duration of follow-up‡ (mo) | 15.7 ± 5.3 (10.6-35.9) | 16.7 ± 10.3 (10.2-80.5) | 1.03 | 0.303 | |
| Sex | 0.7 | 0.464 | |||
| Female | 48.9% | 43.7% | |||
| Male | 51.1% | 56.3% | |||
| ASA-PS classification | 3.3 | 0.352 | |||
| 1 or 2 | 51.1% | 61.9% | |||
| 3 or 4 | 48.9% | 38.1% |
Student 2-sample t test used to compare means.
Chi-square test used to compare proportions.
The values are given as the mean and standard deviation, with the range in parentheses.
TABLE II.
Kellgren-Lawrence Osteoarthritis Severity Comparison*
| Knee Compartment | 0 | 1 | 2 | 3 | 4 |
| Medial TFJ | |||||
| TKA | 0.0% | 0.7% | 30.4% | 47.4% | 21.5% |
| UKA | 0.0% | 0.0% | 28.9% | 54.8% | 16.3% |
| Lateral TFJ | |||||
| TKA | 40.7% | 42.2% | 15.6% | 1.5% | 0.0% |
| UKA | 51.1% | 39.3% | 9.6% | 0.0% | 0.0% |
| Medial PFJ | |||||
| TKA | 48.1% | 33.3% | 17.8% | 0.7% | 0.0% |
| UKA | 57.0% | 31.9% | 9.6% | 1.5% | 0.0% |
| Lateral PFJ | |||||
| TKA | 36.3% | 45.2% | 16.3% | 2.2% | 0.0% |
| UKA | 52.6% | 40.0% | 7.4% | 0.0% | 0.0% |
TFJ = tibiofemoral joint, and PFJ = patellofemoral joint.
Pain and Function
Regarding preoperative pain during the functional activities of walking on an uneven surface, climbing up or down a flight of stairs, and getting up from a low couch or chair without arms, the TKA and UKA cohorts did not differ significantly in the proportion of patients who rated their pain as “slight or no bother” (p ≥ 0.381) (Table III). In addition, the 2 cohorts did not differ with respect to the proportion of patients who, preoperatively, were able to walk >1 hour before stopping due to knee discomfort (p = 0.929) (Table III).
TABLE III.
Group Comparison of Preoperative and Minimum 1-Year PROM Scores
| TKA | UKA | T Value* | χ2 Value† | P Value‡ | |
| Pain with level walking§ | |||||
| Preop. | 5.4 | 5.4 | 0.2 | 0.814 | |
| Min. 1-yr follow-up | 1.4 | 0.7 | 2.9 | 0.004 | |
| Delta | −4.1 | −4.7 | 1.83 | 0.069 | |
| Pain while climbing stairs or inclines§ | |||||
| Preop. | 7.0 | 6.6 | 1.7 | 0.094 | |
| Min. 1-yr follow-up | 2.1 | 1.5 | 2.2 | 0.026 | |
| Delta | −5.2 | −5.1 | 0.0 | 0.965 | |
| UCLA activity level§ | |||||
| Preop. | 4.0 | 4.4 | 1.8 | 0.067 | |
| Min. 1-yr follow-up | 5.6 | 6.0 | 2.1 | 0.038 | |
| Delta | 1.5 | 1.7 | 0.5 | 0.610 | |
| Slight pain or no bother when walking on uneven surface | |||||
| Preop. | 11.1% | 7.8% | 0.8 | 0.381 | |
| Min. 1-yr follow-up | 78.1% | 89.3% | 6.0 | 0.015 | |
| Slight pain or no bother when climbing up or down a flight of stairs | |||||
| Preop. | 4.8% | 7.0% | 0.5 | 0.466 | |
| Min. 1-yr follow-up | 72.1% | 78.9% | 1.7 | 0.197 | |
| Slight pain or no bother getting up from a low couch or chair without arms | |||||
| Preop. | 12.0% | 10.5% | 0.1 | 0.719 | |
| Min. 1-yr follow-up | 69.3% | 87.9% | 13.3 | 0.0003 | |
| >1 hour walking time before stopping due to knee discomfort | |||||
| Preop. | 8.8% | 8.5% | 0.0 | 0.929 | |
| Min. 1-yr follow-up | 45.8% | 72.4% | 19.4 | <0.001 | |
| Satisfied or very satisfied while performing light household activities | |||||
| Preop. | 8.0% | 5.9% | 0.4 | 0.516 | |
| Min. 1-yr follow-up | 81.7% | 94.7% | 10.7 | 0.001 | |
| Satisfied or very satisfied with knee replacement surgery | |||||
| Min. 1-yr follow-up | 81.3% | 90.1% | 4.1 | 0.043 |
Student 2-sample t test used to compare means.
Chi-square test used to compare proportions.
Bold indicates significance.
Mean values are shown. Delta = mean change calculated as min. 1-year minus preoperative value.
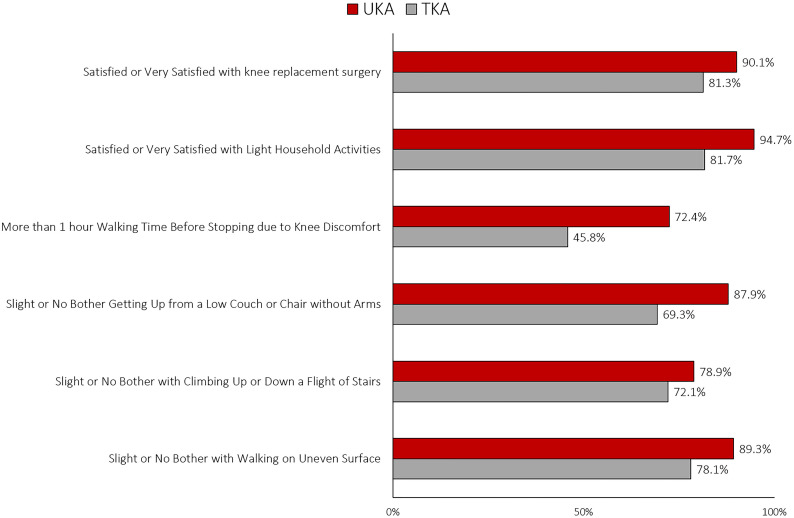
Regarding these same functional measures at minimum 1-year follow-up, a significantly greater proportion of those in the UKA cohort than in the TKA cohort rated their knee pain as “slight or no bother” when walking on an uneven surface and getting up from a low couch or chair without arms (p ≤ 0.015); no difference was found between the groups for pain associated with climbing up or down a flight of stairs (p = 0.197) (Table III) (Fig. 1). Those in the UKA group could also walk for a longer amount of time before stopping due to knee discomfort. Specifically, a significantly greater proportion of patients in the UKA cohort than in the TKA cohort could walk for >1 hour before stopping due to knee discomfort (72% compared with 46%; p < 0.001) (Fig. 1) (Table III).
Fig. 1.
At minimum 1-year follow-up, a greater proportion of patients in the UKA group than in the TKA group reported their knee pain as “slight or no bother” when performing functional activities, could walk for a longer amount of time before stopping due to knee discomfort, and were “satisfied or very satisfied” when performing light household activities and with their knee replacement surgery overall. For all but climbing up or down a flight of stairs, the difference between the groups was significant (p ≤ 0.043).
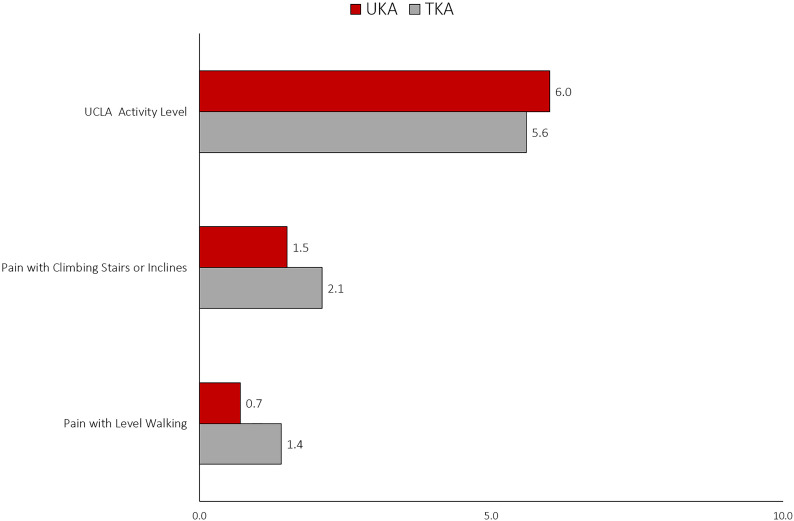
Mean scores preoperatively for pain with level walking and pain while climbing stairs or inclines did not differ significantly between the TKA and UKA groups (p ≥ 0.094) (Table III). At minimum 1-year follow-up, the UKA cohort showed significantly lower scores for pain with level walking and pain while climbing stairs or inclines (p ≤ 0.026) (Fig. 2). While pain scores for both groups improved from preoperative scores, there were no significant differences in the change from preoperative to minimum 1-year (“delta”) between the TKA and UKA cohorts (p ≥ 0.069) (Table III).
Fig. 2.
Mean scores for activity level and pain with level walking and pain climbing stairs or inclines at minimum 1-year follow-up were significantly better for the UKA group compared with the TKA group; however, differences did not reach the MCID of 2 for these numerical rating scales.
Activity Level
Mean UCLA activity-level scores preoperatively did not differ significantly between the UKA and TKA groups (4.4 compared with 4.0, respectively; p = 0.067) (Table III). At minimum 1-year follow-up, the UKA cohort had a significantly higher mean activity level (6.0 compared with 5.6; p = 0.038) (Fig. 2); however, the change from preoperative (delta) did not differ significantly between the UKA and TKA cohorts (p = 0.610) (Table III).
Satisfaction
Preoperatively, the UKA and TKA groups did not differ significantly with respect to satisfaction while performing light household activities (p = 0.516) (Table III). However, at minimum 1-year follow-up, a significantly greater proportion of those in the UKA group were “satisfied or very satisfied” with their knee while performing light household activities (95% compared with 82%; p = 0.001) (Fig. 1). Furthermore, Likert scale satisfaction scores revealed a significantly greater proportion of those in the UKA group were “satisfied or very satisfied” with their knee replacement surgery at minimum 1-year follow-up (90% compared with 81%; p = 0.043) (Fig. 1) (Table III).
Discussion
Arthroplasty surgeons rely on scientific evidence to make sound decisions about the merits of various surgical procedures. It remains somewhat controversial whether isolated medial compartment osteoarthritis is best treated with UKA or TKA, and to our knowledge, only 1 modern randomized controlled trial comparing UKA and TKA suggests that UKA should be the first choice for late-stage isolated medial compartment osteoarthritis29. While that randomized controlled trial provides the most robust and scientifically sound data to date, the follow-up period of 5 years for a joint replacement population could be argued to be less than ideal because other medical issues and general age-related decline unrelated to the joint replacement could influence PROM surveys as these patients age further. Although it is important that postoperative evaluation takes place at early, mid-, and long-term follow-up, patients may have optimized function and pain scores closer to a year after surgery, which may be the optimal time point at which to compare PROM outcomes between these cohorts. Other studies have attempted to compare PROMs at earlier time points by matching TKA and UKA cohorts radiographically; however, inherent bias remains in these studies as the TKA and UKA groups differed preoperatively by radiographic osteoarthritis severity27 and outcome metrics obtained preoperatively28.
Admittedly, while a well-designed randomized controlled trial remains the scientific gold standard for comparing surgical treatment modalities in most scenarios, retrospective studies with appropriately matched cohorts that minimize and account for statistical confounding variables can provide valuable information. The UKA and TKA cohorts in the current study showed no significant differences in terms of demographics and severity of osteoarthritis confirmed on preoperative radiographs with the KL grading system (p ≥ 0.158) (Tables I and II). Our UKA cohort reported a higher satisfaction level in the performance of light household activities (“satisfied or very satisfied,” 95%) and greater overall Likert satisfaction (90%) with their knee replacement, consistent with the findings of a previous, similar study22, which used the same satisfaction survey. The authors found a significant difference in the proportion of patients in the UKA cohort compared with the TKA cohort who reported “satisfied or very satisfied” with their knee replacement (86% compared with 71%). We also found that a significantly greater proportion of patients in the UKA group than in the TKA group were “satisfied or very satisfied” (90% compared with 81%; p = 0.043).
In addition, in the current study, a significantly greater proportion of patients in the UKA group compared with the TKA group reported their knee pain as “slight or no bother” for the functional activities of walking on an uneven surface and getting up from a low couch or chair without arms, and could walk for a longer amount of time before stopping due to knee discomfort (p ≤ 0.015). Our observations corroborate findings from other institutions using different functional and activity components of PROM surveys7,38. Moreover, the UKA cohort had a significantly higher mean UCLA activity-level score and significantly lower mean scores for pain with level walking and pain with climbing stairs or inclines at minimum 1-year follow-up (p ≤ 0.038); however, the minimal clinically important difference (MCID) of 2 was not reached for these numerical rating scales of pain and activity level39.
As noted, our findings are largely consistent with previous findings of improved functional and activity scores for UKA compared with TKA7,38,40. However, none of those previous comparative studies accounted for the severity of osteoarthritis when comparing UKA and TKA, enhancing the reliability of our observations. Manzotti et al.28 were the first, to our knowledge, to match patients undergoing manual-technique UKA and robotic-assisted TKA by age, sex, preoperative range of motion, and preoperative osteoarthritis severity using the Ahlbäck classification41. However, although none of the preoperative findings differed significantly, there were several trends toward significant differences in the duration of latest follow-up, preoperative flexion, preoperative hip-knee-ankle angle, and preoperative Knee Society total and functional component scores (p ≤ 0.067), which could have influenced the postoperative findings28. Recently, van der List et al.27 conducted a study of UKA compared with TKA in which they attempted to match patients by osteoarthritis severity; however, those who underwent manual-technique TKA with computer-navigation assistance presented with significantly worse osteoarthritis in the medial and patellofemoral compartments compared with patients in the robotic-assisted UKA group. Despite the potential confounding preoperative variables, both studies found significantly higher postoperative function scores for UKA compared with TKA27,28, similar to the current study.
The data presented in our study should be considered in the context of a historical study by Newman et al., who performed a randomized controlled trial of UKA versus TKA involving 102 patients14,42. The authors randomized the patients to either UKA or TKA after arthrotomy and, at 5-year follow-up, reported significantly greater range of motion as well as improved function and earlier discharge for the patients who received a UKA42. The authors further reported the maintenance of optimal outcomes and no greater failure rate for the UKA group at the 15-year follow-up, despite the death of 43 patients (45 knees, 44%) prior to follow-up14. It is important to consider that these 2 cohorts involve historical implants not currently in use and a single outcome measure, the Bristol Knee Score, that is potentially more blunt and less discerning with regard to differentiating between UKA and TKA patients compared with the modern PROMs used in the current study.
While this study demonstrates superior early outcomes for patients who underwent UKA compared with TKA, these early advantages should be weighed against the ample registry data that demonstrate significantly greater failure rates and decreased survivorship for UKA compared with TKA18,43. From the Finnish Arthroplasty Registry, the data of 4,713 patients who underwent UKA and 83,511 who underwent TKA were compared. The 10 and 15-year survivorship for UKA was 80.6% and 69.6% compared with 93.3% and 88.7% for TKA at the respective follow-up intervals43. Using data from the National Joint Registry for England and Wales, 25,334 UKAs were propensity-matched to 75,996 TKAs. The UKA group had worse implant survivorship for revision and revision/reoperation, with a subhazard ratio of 2.12 and 1.38 at 8 years, respectively. However, length of stay as well as mortality, complications, and readmission rates were greater for TKA at all time points18.
This study has limitations. First, the analysis was performed in a retrospective manner; however, PROMs were prospectively administered for both UKAs and TKAs by clinical staff not directly involved in the study. Second, data reflect the experience of a high-volume surgeon with extensive experience in knee arthroplasty procedures and therefore may not be applicable to low-volume settings. Third, only 1 experienced rater graded preoperative radiographs for osteoarthritis severity. Fourth, the outcomes reported in this manuscript are minimum 1-year, and longer-term PROM outcomes could change with respect to contralateral or patellofemoral compartment deterioration. Further, the clinical relevance of many significant findings found in this study remains unknown and warrant further study for MCIDs of these measures.
Despite the limitations, the current study is one of the first studies to compare modern PROMs in UKA and TKA cohorts appropriately matched on demographics and preoperative osteoarthritis severity, making them equivalent candidates for either TKA or UKA, and indicates that patients suitable for either procedure will likely experience better early outcomes with UKA.
Footnotes
Investigation performed at the IU Health Hip & Knee Center, Fishers, Indiana
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The project described was supported by the Indiana University Health–Indiana School of Medicine Strategic Research Initiative. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A205).
References
- 1.Borus T, Thornhill T. Unicompartmental knee arthroplasty. J Am Acad Orthop Surg. 2008. January;16(1):9-18. [DOI] [PubMed] [Google Scholar]
- 2.Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J. Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol. 2015. July;25(5):799-806. Epub 2015 Feb 13. [DOI] [PubMed] [Google Scholar]
- 3.Yang KY, Wang MC, Yeo SJ, Lo NN. Minimally invasive unicondylar versus total condylar knee arthroplasty—early results of a matched-pair comparison. Singapore Med J. 2003. November;44(11):559-62. [PubMed] [Google Scholar]
- 4.Akizuki S, Mueller JK, Horiuchi H, Matsunaga D, Shibakawa A, Komistek RD. In vivo determination of kinematics for subjects having a Zimmer Unicompartmental High Flex Knee System. J Arthroplasty. 2009. September;24(6):963-71. Epub 2008 Aug 12. [DOI] [PubMed] [Google Scholar]
- 5.Griffin T, Rowden N, Morgan D, Atkinson R, Woodruff P, Maddern G. Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: a systematic study. ANZ J Surg. 2007. April;77(4):214-21. [DOI] [PubMed] [Google Scholar]
- 6.Hollinghurst D, Stoney J, Ward T, Gill HS, Newman JH, Murray DW, Beard DJ. No deterioration of kinematics and cruciate function 10 years after medial unicompartmental arthroplasty. Knee. 2006. December;13(6):440-4. Epub 2006 Sep 14. [DOI] [PubMed] [Google Scholar]
- 7.Hopper GP, Leach WJ. Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc. 2008. October;16(10):973-9. Epub 2008 Aug 12. [DOI] [PubMed] [Google Scholar]
- 8.Isaac SM, Barker KL, Danial IN, Beard DJ, Dodd CA, Murray DW. Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee. 2007. June;14(3):212-7. Epub 2007 Mar 6. [DOI] [PubMed] [Google Scholar]
- 9.Jahromi I, Walton NP, Dobson PJ, Lewis PL, Campbell DG. Patient-perceived outcome measures following unicompartmental knee arthroplasty with mini-incision. Int Orthop. 2004. October;28(5):286-9. Epub 2004 Jun 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeer PJ, Cossey AJ, Keene GC. Haemoglobin levels following unicompartmental knee arthroplasty: influence of transfusion practice and surgical approach. Knee. 2005. October;12(5):358-61. [DOI] [PubMed] [Google Scholar]
- 11.Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW; Oxford Hip and Knee Group. Rapid recovery after Oxford unicompartmental arthroplasty through a short incision. J Arthroplasty. 2001. December;16(8):970-6. [DOI] [PubMed] [Google Scholar]
- 12.Walton NP, Jahromi I, Lewis PL, Dobson PJ, Angel KR, Campbell DG. Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg. 2006. April;19(2):112-6. [DOI] [PubMed] [Google Scholar]
- 13.Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD. Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018. June;26(6):1811-22. Epub 2017 Nov 28. [DOI] [PubMed] [Google Scholar]
- 14.Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009. January;91(1):52-7. [DOI] [PubMed] [Google Scholar]
- 15.Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011. February;93(2):198-204. [DOI] [PubMed] [Google Scholar]
- 16.White SH, Roberts S, Kuiper JH. The cemented twin-peg Oxford partial knee replacement survivorship: a cohort study. Knee. 2015. September;22(4):333-7. Epub 2015 May 21. [DOI] [PubMed] [Google Scholar]
- 17.Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008. August;79(4):499-507. [DOI] [PubMed] [Google Scholar]
- 18.Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014. October 18;384(9952):1437-45. [DOI] [PubMed] [Google Scholar]
- 19.Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012. January;470(1):84-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murray DW, Liddle AD, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint J. 2015. October;97-B(10)(Suppl A):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amin AK, Patton JT, Cook RE, Gaston M, Brenkel IJ. Unicompartmental or total knee arthroplasty?: Results from a matched study. Clin Orthop Relat Res. 2006. October;451:101-6. [DOI] [PubMed] [Google Scholar]
- 22.Kim MS, Koh IJ, Choi YJ, Lee JY, In Y. Differences in patient-reported outcomes between unicompartmental and total knee arthroplasties: a propensity score-matched analysis. J Arthroplasty. 2017. May;32(5):1453-9. Epub 2016 Nov 27. [DOI] [PubMed] [Google Scholar]
- 23.Lim JW, Cousins GR, Clift BA, Ridley D, Johnston LR. Oxford unicompartmental knee arthroplasty versus age and gender matched total knee arthroplasty - functional outcome and survivorship analysis. J Arthroplasty. 2014. September;29(9):1779-83. Epub 2014 Apr 5. [DOI] [PubMed] [Google Scholar]
- 24.Cameron HU, Jung YB. A comparison of unicompartmental knee replacement with total knee replacement. Orthop Rev. 1988. October;17(10):983-8. [PubMed] [Google Scholar]
- 25.Dalury DF, Fisher DA, Adams MJ, Gonzales RA. Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics. 2009. April;32(4):orthosupersite.com/view.asp?rID=38057. [PubMed] [Google Scholar]
- 26.Laurencin CT, Zelicof SB, Scott RD, Ewald FC. Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res. 1991. December;273:151-6. [PubMed] [Google Scholar]
- 27.van der List JP, Chawla H, Villa JC, Pearle AD. The role of patient characteristics on the choice of unicompartmental versus total knee arthroplasty in patients with medial osteoarthritis. J Arthroplasty. 2017. March;32(3):761-6. Epub 2016 Aug 24. [DOI] [PubMed] [Google Scholar]
- 28.Manzotti A, Confalonieri N, Pullen C. Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop. 2007. June;31(3):315-9. Epub 2006 Aug 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A, Kent S, Hudson J, Carr A, Leal J, Campbell H, Fitzpatrick R, Arden N, Murray D, Campbell MK; TOPKAT Study Group. The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet. 2019. August 31;394(10200):746-56. Epub 2019 Jul 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989. January;71(1):145-50. [PubMed] [Google Scholar]
- 31.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957. December;16(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scuderi GR, Sikorskii A, Bourne RB, Lonner JH, Benjamin JB, Noble PC. The Knee Society Short Form reduces respondent burden in the assessment of patient-reported outcomes. Clin Orthop Relat Res. 2016. January;474(1):134-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramkumar PN, Navarro SM, Haeberle HS, Ng M, Piuzzi NS, Spindler KP. No difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2018. July;33(7):2322-9. Epub 2018 Feb 21. [DOI] [PubMed] [Google Scholar]
- 34.Samuelsson K, Magnussen RA, Alentorn-Geli E, Krupic F, Spindler KP, Johansson C, Forssblad M, Karlsson J. Equivalent knee injury and osteoarthritis outcome scores 12 and 24 months after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register. Am J Sports Med. 2017. July;45(9):2085-91. [DOI] [PubMed] [Google Scholar]
- 35.Rosner B. Fundamentals of biostatistics. 7th ed. Brooks/Cole, Cengage Learning; 2011. [Google Scholar]
- 36.Lee M, Huang Y, Chong HC, Ning Y, Lo NN, Yeo SJ. Predicting satisfaction for unicompartmental knee arthroplasty patients in an Asian population. J Arthroplasty. 2016. August;31(8):1706-10. Epub 2016 Feb 8. [DOI] [PubMed] [Google Scholar]
- 37.Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: a systematic review. HSS J. 2018; July;14(2):192-201. Epub 2018 Jun 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burn E, Sanchez-Santos MT, Pandit HG, Hamilton TW, Liddle AD, Murray DW, Pinedo-Villanueva R. Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: a propensity score-matched cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2018. May;26(5):1455-64. Epub 2016 Dec 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004. August;8(4):283-91. [DOI] [PubMed] [Google Scholar]
- 40.Ahn JH, Kang DM, Choi KJ. Bilateral simultaneous unicompartmental knee arthroplasty versus unilateral total knee arthroplasty: a comparison of the amount of blood loss and transfusion, perioperative complications, hospital stay, and functional recovery. Orthop Traumatol Surg Res. 2017. November;103(7):1041-5. Epub 2017 Aug 5. [DOI] [PubMed] [Google Scholar]
- 41.Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277:277: 7-72. [PubMed] [Google Scholar]
- 42.Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998. September;80(5):862-5. [DOI] [PubMed] [Google Scholar]
- 43.Niinimäki T, Eskelinen A, Mäkelä K, Ohtonen P, Puhto AP, Remes V. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res. 2014. May;472(5):1496-501. Epub 2013 Nov 19. [DOI] [PMC free article] [PubMed] [Google Scholar]