ABSTRACT
Platelet-rich plasma has become one of the most widely used facial cosmetics fillers. We evaluated four patients treated by cosmetologists with platelet-rich plasma injections who developed irreversible blindness due to iatrogenic occlusion of the ophthalmic artery; immediately after the injection in the glabellar area in three cases and in the nasolabial fold in one case. Early after the injections the fundi of all patients demonstrated central retinal artery and choroidal occlusions. Later, two patients developed retinal pigment dispersion and one of them a pigmented optic disc. The scars on the skin showed similar characteristics in all patients, which could constitute an important marker in the presumptive diagnosis of platelet-rich plasma injection associated complications.
KEYWORDS: Platelet-rich plasma, optic nerve pigmentation, ophthalmic artery occlusion, blindness
Introduction
Injection of dermal filler is widely used for cosmetic facial rejuvenation. This type of procedure is considered minimally invasive. The types of dermal filler used include autologous fat, hyaluronic acid, polylactic acid, calcium hydroxylapatite, polymethylmethacrylate-collagen,1 and silicone.2 Side effects from these procedures are uncommon. However, these are descriptions of the formation of foreign body granulomas,3 allergic reactions, bruising,4 infections, dermal necrosis,5–7 and migration of filling material.8 More devastating complications include blindness, ischaemic cerebrovascular events, and death, typically due to the embolisation of material into the cranial circulation.7,8
In order to understand the pathophysiology when embolisation causes blindness it is important to remember the anatomy. The central retinal artery (CRA) is a branch of the ophthalmic artery. The ophthalmic artery is connected to the supraorbital, supratrochlear, dorsal nose, and lacrimal arteries that supply the glabellar region, forehead, nose, and lacrimal gland respectively. These arteries are part of the internal carotid artery system. The facial, angular, infraorbital, and temporal superficial arteries that supply the nasolabial and nasojugal folds, the mid-face, and temple respectively, are part of the external carotid artery system. There are anastomoses between the two systems. The mechanism by which dermal fillers induce blindness could be by direct injury to the globe or from accidental high-pressure injection of a fillers into the blood vessel causing retrograde local or distal emboli. Also, the nature of the material filler could be related. Thick, cohesive substances should theoretically be less likely to embolise, unlike oily liquids (fat injections, silicone oil) or particulate solutions (steroid suspensions).4 Also, the particle size and the amount of filler injected per injection site could also affect the risk of embolisation.9,10
Recently, platelet-rich plasma has been developed as a tissue regeneration technique for the treatment of face wrinkles, periorbital dark circles,11 and nasolabial folds.12 Users of this technique claim that there is no risk of infection, transmission of disease, or other side effects.
Herein we describe four patients who had sudden painful loss of vision immediately after platelet-rich plasma injections for facial rejuvenation.
This report follows the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Unidad Oftalmológica de Caracas.
Report of cases
Case 1
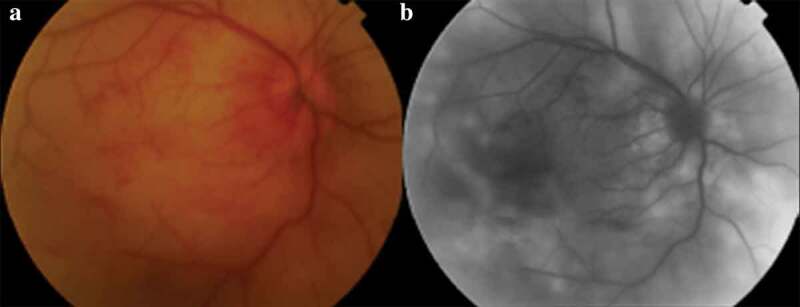
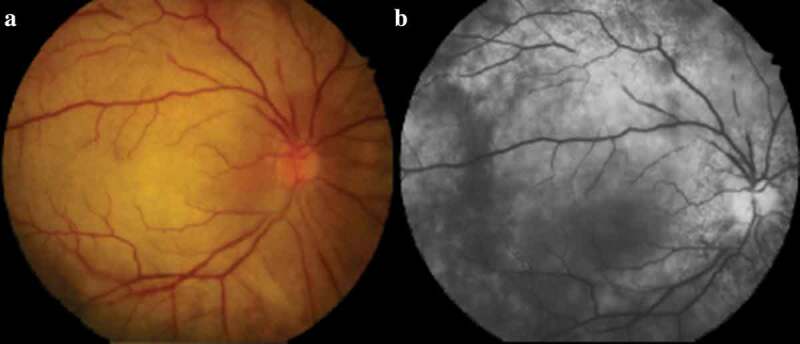
The first case is of a 61-year-old previously healthy woman who received monthly sessions of platelet-rich plasma injections into her hands, face and neck by a cosmetologist. Doing her sixth session, immediately after injection into the left glabellar region, she developed painful sudden loss of vision in the left eye associated with dizziness and vomiting. On assessment the same day her visual acuities were 20/20 with the right eye (OD) and no perception of light (NPL) with the left eye (OS). Fundus examination of the left eye showed generalised retinal whitening, segmental narrowing of the retinal arteries, and white material suggestive of an embolus within the central retinal artery. The retinal veins were attenuated (Figure 1a). Fluorescein angiography (FA) demonstrated patchy choroidal perfusion and blockage of the retinal circulation (Figure 1b).
Figure 1.
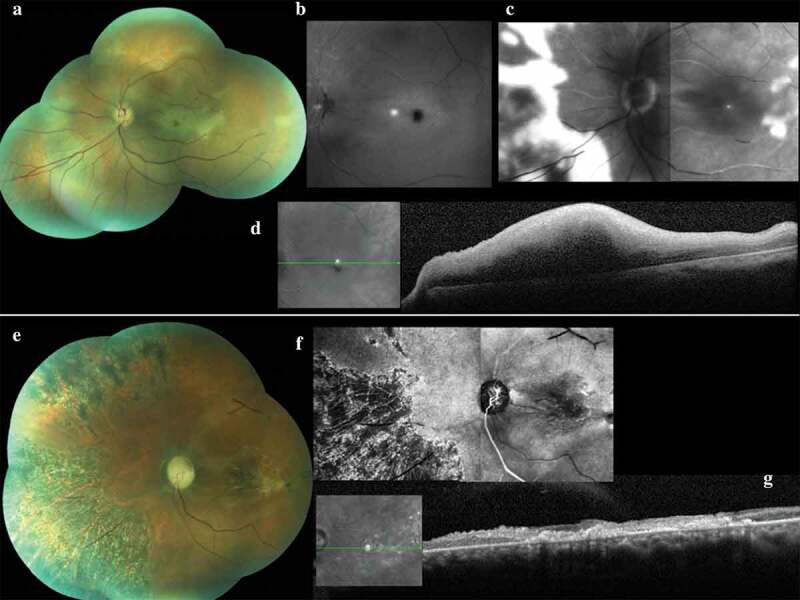
Case 1: Left eye (a) Colour fundus photograph at presentation showing segmental narrowing of the retinal arteries with an embolus within the central retinal artery, a cherry-red spot in the macula and attenuated retinal veins. (b) Fluorescein angiogram at presentation demonstrating blockage of the retinal circulation. (c) Fluorescein angiogram after three days showing limited and sluggish filling of the retinal arteries and late hyperfluorescence in the retinal and perifoveal areas. (d) Optical coherence tomography image of the left eye after three days showing increased macular retinal thickness. After one month: (e) Colour fundus photograph showing a pale optic disc with pigment in the superior temporal region, phantom retinal vessels, pigmentation of the peripheral retinal and macular fibrosis. (f) Fluorescein angiogram demonstrating thinning of the retinal vessels and a hypofluorescent area mixed with mild areas of hyperfluorescence in the intermediate retinal and macular region. (g) Optical coherence tomography image demonstrating atrophy of all the retinal layers and fibrosis of the macular area
Brain magnetic resonance imaging (MRI), magnetic resonance angiography (MRA) of the brain and neck, laboratory tests (for hypercoagulability and vasculitis), and cardiovascular evaluation were unremarkable.
After three days there was limited and sluggish filling of the retinal arteries and late hyperfluorescence in the retinal and foveal area (Figure 1c). Optical coherence tomography (OCT) showed increased macular retinal thickness (Figure 1d). She developed glabellar bruising and hypoaesthesia in the distribution of the first trigeminal branch on the left side (Figure 3a).
Figure 3.

Case 1: Facial photographs. (a) Glabellar bruising at presentation. (b) After one month showing necrosis and ulceration of the injected area. (c) After four months some improvement. (d) After eight months persistent scarring visible
After one month she developed a pale left optic disc with pigment in the superior temporal region, phantom retinal vessels, pigmentation of the peripheral retinal and macular fibrosis (Figure 1e). FA demonstrated attenuated retinal vessels with hypofluorescent areas mixed with mild hyperfluorescent areas in the macula and mid-peripheral retina (Figure 1f). OCT demonstrated atrophy of all retinal layers and fibrosis of the macular area (Figure 1g).
After four months the pigmentation had increased in the retina and the optic disc remained pale (Figure 2a). After eight months there was retinal detachment in the left eye (Figure 2b,c).
Figure 2.
Case 1: Colour fundus photographs of the left eye (a) after four months demonstrating increased pigmentation of the retina and optic disc. (b, c) After 8 months retinal detachment can be seen
Just after the injection there was bruising at the injection site (Figure 3a). One month after the injection there was skin necrosis and ulceration of the injection area (Figure 3b). After four months this had improved (Figure 3c). After eight months there was persistent scarring in the affected area (Figure 3d).
Case 2
A 63-year-old previously healthy woman developed sudden, painful loss of vision in the right eye after her first injection of platelet-rich plasma in the forehead for wrinkles. In addition, she had dizziness, tinnitus and vomiting acutely. She also noticed the development of iris depigmentation. At her first visit, three weeks after injection, her corrected visual acuities were NLP OD and 20/20 OS. Biomicroscopy showed corneal endothelial pigmentation, iris atrophy, posterior synechiae of the iris and pigment dispersion at the anterior surface of the lens (Figure 4a). The ocular movements were normal. On fundal examination there was a pale right optic disc, central retinal artery occlusion, and retinal haemorrhages along with patchy pigment dispersion and macular fibrosis (Figure 4b). The amalric triangle sign, indicating choroidal ischaemia, was evident in the mid-peripheral retina. FA demonstrated delayed filling of the central retinal artery as well as impaired perfusion of the optic disc and choroid (Figure 4c). OCT showed fibrosis and neurosensory retinal detachment in the macular area with an epiretinal membrane (Figure 4d). A scar was evident in the glabellar area (Figure 4e). Brain MRI and MRA, laboratory tests (for hypercoagulability and vasculitis), and cardiovascular evaluation were unremarkable. The patient did not return for follow-up.
Figure 4.
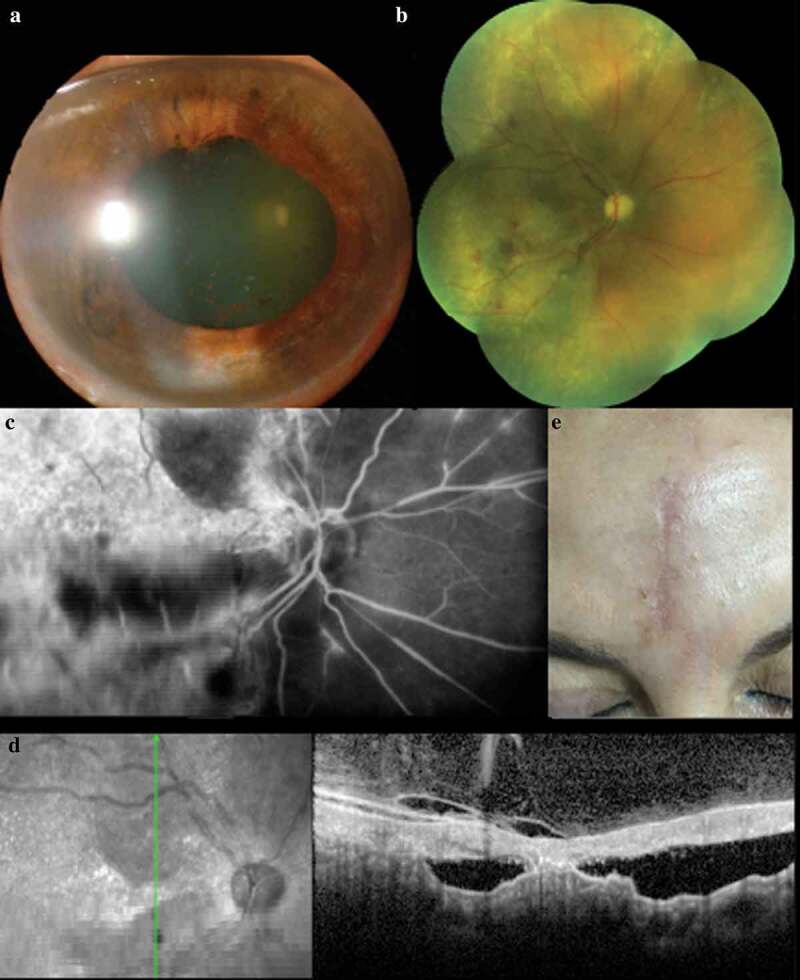
Case 2: Right eye (a) Biomicrosopy photograph showing iris depigmentation, posterior synechiae and pigment dispersion at the anterior surface of the lens. (b) Colour fundus photograph revealing a pale optic disc, central retinal artery occlusion, retinal haemorrhages, patchy pigment dispersion and macular fibrosis. (c) Fluorescein angiogram demonstrating delayed filling of the central retinal artery, impaired perfusion of the optic disc and choroid, and hyperfluorescence areas in the retina. (d) Optical coherence tomography image showing fibrosis, neurosensory retinal detachment in the macular area and an epiretinal membrane. (e) Facial photograph showing a scar in the glabellar area
Case 3
A 52-year-old previously healthy woman developed painful loss of vision in the right eye and vomiting immediately after platelet-rich plasma injection in the right nasolabial fold and glabellar area. She had had many previous injections by her cosmetologist. At the first visit, after 24 hours, the visual acuities were NLP OD and 20/20 OS. There was an incomplete oculomotor nerve palsy (mild ptosis, restricted adduction and vertical gaze) affecting her right eye. Biomicroscopy showed flare in the anterior chamber and corneal folds. The intraocular pressure of her right eye was 3 mmHg. She had a central retinal artery occlusion without a cherry-red spot but had multiple retinal haemorrhages (Figure 5a). FA showed delayed filling of the central retinal artery and vein with areas of patchy choroidal non-perfusion (Figure 5b). She had bruising at the injection sites.
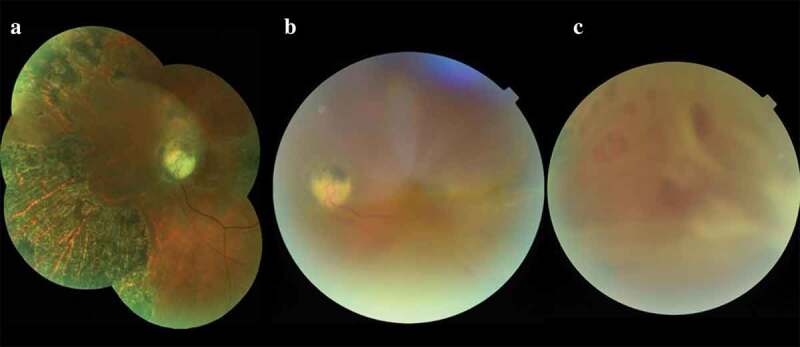
Figure 5.
Case 3: Right eye (a) Colour fundus photograph showing central retinal artery occlusion without a cherry-red spot. (b) Fluorescein angiogram showing delayed filling of the central retinal artery and vein with areas of patchy choroidal non-perfusion
Brain MRI/MRA, laboratory tests (for hypercoagulability and vasculitis), and cardiovascular evaluation were unremarkable.
She did not attend for follow-up but she sent a skin photograph after one month showing necrosis of the forehead, right periorbital region, right cheek, and right nasal area.
Case 4
A 50-year-old previously healthy woman developed eye pain with transient blue vision followed by loss of vision in the right eye immediately after her first platelet-rich plasma and platelet gel injection into the forehead, glabellar area, and right external canthus of the eye. In addition, she complained of headache, nausea, urinary urgency, and right ptosis. At the first visit, three weeks after the injection, the visual acuities were NLP OD and 20/15 OS. She had a complete right oculomotor nerve palsy. Fundal examination revealed a pale retina with a central retinal artery occlusion (Figure 6a). FA demonstrated delayed filling of the central retinal artery with areas of patchy choroidal non-perfusion (Figure 6b). She did not return for follow-up.
Figure 6.
Case 4: Right eye (a) Colour fundus photograph showing segmental narrowing of the retinal arteries and a pale retina with central retinal artery occlusion. (b) Fluorescein angiogram demonstrating delayed filling of the central retinal artery with areas of patchy choroidal non-perfusion
Discussion
Platelet rich plasma has been employed in dermatology, gastroenterology, orthopaedics, general, dental, maxillofacial, and ocular surgery.13 In facial plastic surgery it has been used to eliminate wrinkles, dark periorbital circles,11 and nasolabial folds.12
Lyophilised autologous fibrin activated with bovine thrombin allows the plasma to function as an osteoconductive graft inducing release of growth factors as well as fibrin, fibronectin, and vibronectin into a wound area.11,14 In ophthalmology it is employed for ocular surface problems and as an adjuvant therapy in high myopic macular holes.15,16
Users of platelet-rich subdermal injections into the face claim that there is no risk of infection, transmission of diseases, or other side effects.11,17 However, we have reported here four patients who lost their vision immediately after facial injection of platelet-rich plasma.
We could not obtain information about the platelet-rich plasma preparation, composition, technique, and dosage employed in our patients, but most of the platelet-rich plasma preparation protocols are similar to each other. They involve the withdrawal of autologous blood in the presence of an anticoagulant, its centrifugation with plasma separation, leukocyte inclusion or exclusion, and the activation of platelets, most frequently with calcium chloride. Lysophosphatidic acid is produced by platelets following stimulation by prothrombotic agents in the bloodstream and that could be also important in the development of arterial occlusion.18
Embolisation into the ophthalmic circulation has been reported after filler injection in the nasolabial folds, glabellar lines, and periorbital region wrinkles.7,19 As has been discussed above, extensive anastomoses between the external and internal carotid artery territory around the eye creates the risk that material inadvertently injected at high pressure into any facial artery could embolise into the ophthalmic artery, presumably by retrograde flow via the supratrochlear or supraorbital arteries (as happened in cases 1, 2, and 4) or nasal dorsal artery (as presumably occurred in the third case). This results in infarction of the retina as well as the choroid.7,19
If the iris is affected it suggests occlusion of the long ciliary arteries. Obstruction of the blood supply to the extraocular muscles and nerves causes ophthalmoplegia and ptosis. Acute anterior segment ischaemia and lack of blood flow to the sensory nerves of the face and orbit could explain the ocular pain that occurred in some cases. Although occlusion of the central or branch retinal arteries is not usually reversible, ophthalmoplegia and corneal oedema can recover as occurred in one of the cases (case 2). Some authors like Wook Park Sun et al. hypothesised that ocular pain and attenuated choroidal vascularity on OCT could be good indicators of iatrogenic artery occlusion with poor visual prognosis.7
Late pigmentation of the retina and optic nerve, as we observed in cases 1 and 2, could be due to reactive proliferation of the juxtapapillary pigment epithelium which migrate into the atrophic tissues of the retina and the optic disc.20 One might also speculate that there could be a reaction with the calcium chloride employed in the activation of the platelet-rich plasma.
Skin necrosis following injection of dermal filler is a severe and early complication as we observed in the first three cases, probably due to interruption of vascular supply to the area by direct injury, compression of vasculature or obstruction of the vessels by the dermal filler.21 The glabella is one of the most susceptible areas to tissue necrosis due its vascular anatomy (small vessels branching from supratrochlear and suprarobital arteries with limited collateral circulation).21 The scars on the skin showed similar characteristics in all patients, which could constitute an important marker in the presumptive diagnosis of platelet-rich plasma injection associated complications.
Kalyam et al.22 reported a patient who developed irreversible blindness following periocular autologous platelet-rich plasma skin rejuvenation treatment, with clinical manifestations similar to our patients. The authors inferred that the syringe was not drawn back upon before injection to assess for intravascular needle placement and this may have led to inadvertent intra-arterial injection.22
The Aesthetic Interventional Induced Visual Loss (AIIVL) Consensus Group included consultant plastic and aesthetic surgeons from the UK and China, Consultant Ophthalmic Surgeons from the UK and United States, and the American Society of Plastic Surgeons. This group proposed guidelines to prevent and treat vision loss due to facial filler injections (summarised in Table 1), however the efficacy of these treatments remains unproven.10,23,24
Table 1.
Consensus guidance for the prevention and treatment of aesthetic interventional induced visual loss. Adapted from Humzah et al.24
| Preventive actions |
|---|
| General advice: |
| Understand facial vascular anatomy |
| Consent patients regarding the risk of vision loss |
| Recognise warning signs of occlusion |
| Avoid high-risk facial areas when possible |
| Injection techniques: |
| Apply minimal pressure |
| Slow administration |
| Low volume |
| Mix filler with injectable vasoconstrictors |
| Aspirate prior to injecting |
| Apply occlusive pressure in the area of the supraorbital notch when performing injections in high risk areas |
| Optimal equipment: |
| Small syringe volumes |
| Larger cannula ≥25 G to reduce risk of entering vessels |
|
Treatment strategies |
| Lower intraocular pressure: |
| Ocular massage |
| Anterior chamber paracentesis |
| Timolol drops |
| Ocular massage |
| Intravenous acetazolamide or mannitol |
| Minimise retinal damage: |
| Hyperbaric oxygen |
| Topical and systemic steroids |
| Aspirin |
| Carbon dioxide rebreathing |
| Alternative treatments: |
| Hyalorinidase |
| Urokinase |
| Sublingual glyceryl trinitrate |
The complications of injection of platelet-rich plasma into the face can be devastating. As recommended by all authors who have described such complications we emphasise the importance that these procedures are performed by skilled cosmetologists who are aware of the potential complications and that patients are counselled as to the risks beforehand.
Declaration of interest statement
The authors declare no conflict of interest.
References
- 1.Cohen S, Dover J, Monheit G, et al. Five-year safety and satisfaction study of PMMA-collagen in the correction of nasolabial folds. Dermatol Surg. 2015. December;41(Suppl 1):S302–13. doi: 10.1097/DSS.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 2.Joseph JH. The case for synthetic injectables. Facial Plast Surg Clin North Am. 2015. November;23(4):433–445. doi: 10.1016/j.fsc.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Daines SM, Williams EF. Complications associated with injectable soft-tissue fillers: a 5-year retrospective review. JAMA Facial Plast Surg. 2013. May;15(3):226–231. doi: 10.1001/jamafacial.2013.798. [DOI] [PubMed] [Google Scholar]
- 4.Golberg RA, Fiaschetti D. Filling the periorbital hollow with hyaluronic acd gel: initial experience with 244 injections. Opthalmic Plast Reconstr Surg. 2006. Sep–Oct;22(5):335–341. doi: 10.1097/01.iop.0000235820.00633.61. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch RJ, Stier M. Complications of soft tissue augmentation. J Drugs Dermatol. 2008. September;7(9):841–845. [PubMed] [Google Scholar]
- 6.Kassir R, Kolluru A, Kassir M. Extensive necrosis after injection of hyaluronic acid filler: case report and review of the literature. J Cosmet Dermatol. 2011. September;10(3):224–231. doi: 10.1111/jcd.2011.10.issue-3. [DOI] [PubMed] [Google Scholar]
- 7.Park SW, Woo SJ, Park KH, Huh JW, Jung C, Kwon OK. Iatrogenic retinal artery occlusion caused by cosmetic facial filler injections. Am J Ophthalmol. 2012;154:653–662. doi: 10.1016/j.ajo.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 8.Carruthers JD, Fagien S, Rohrich RJ, Weinkle S, Carruthers A. Blindness caused by cosmetic filler injection: a review of cause and therapy. Plast Reconstr Surg. 2014. December;134(6):1197–1201. doi: 10.1097/PRS.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 9.Kim YK, Jung C, Wood SJ, Park KH. Cerebral angiographic findings of cosmetic facial filler related ophthalmic and retinal artery occlusion. J Korean Med Sci. 2015. December;30(12):1846–1855. doi: 10.3346/jkms.2015.30.12.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paap MK, Milman T, Ugradar S, Goldberg R, Silkiss RZ. Examining the role of retrobulbar hyaluronidase in reversing filler- induced blindness: a systematic review. Ophthalmic Plast Reconstr Surg. 2019. December 24. In Press. [DOI] [PubMed] [Google Scholar]
- 11.Mehryan P, Zartab H, Rajabi A, Pazhoohi N, Firooz A. Assessment of efficacy of platelet-rich plasma (PRP) on infraorbital dark circles and crow’s feet wrinkles. J Cosmet Dermatol. 2014. March;13(1):72–78. doi: 10.1111/jocd.2014.13.issue-1. [DOI] [PubMed] [Google Scholar]
- 12.Sclafani AP. Platelet-rich fibrin matrix for improvement of deep nasolabial folds. J Cosmet Dermatol. 2010. March;9(1):66–71. doi: 10.1111/jcd.2010.9.issue-1. [DOI] [PubMed] [Google Scholar]
- 13.Ramos-Torrecillas J, De Luna-Bertos E, García-Martínez O, Ruiz C. Clinical utility of growth factors and platelet-rich plasma in tissue regeneration: a review. Wounds. 2014. July;26(7):207–213. [PubMed] [Google Scholar]
- 14.Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014. May 8;4(1):3–9. doi: 10.32098/mltj.01.2014.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anitua E, Muruzabal F, Tayebba A, et al. Autologous serum and plasma rich in growth factors in ophthalmology: preclinical and clinical studies. Acta Ophthalmol. 2015. December;93(8):e605–14. doi: 10.1111/aos.12710. [DOI] [PubMed] [Google Scholar]
- 16.Figueroa MS, Govetto A, Arriba-Palomero PD. Short-term results of platelet-rich plasma as adjuvant to 23-G vitrectomy in the treatment of high myopic macular holes. Eur J Ophthalmol. 2016. August 4;26(5):491–496. doi: 10.5301/ejo.5000729. [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Gonzalez JM, Cano-Sanchez JGonzalo-Lafuente JC, Campo-Trapero J, Esparza-Gomez G, Seoane J. Do ambulatory-use Platelet-Rich Plasma (PRP) concentrates present risks? Med Oral. 2002. Nov-Dec;7(5):375–390. [PubMed] [Google Scholar]
- 18.Bosetti M, Boffano P, Marchetti A, Leigheb M, Colli M, Brucoli M. The number of platelets in patient’s blood influences the mechanical and morphological properties of PRP-clot and lysophosphatidic acid quantity in PRP. Int J Mol Sci. 2019. December 24;21(1):E139:1–13. doi: 10.3390/ijms21010139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carle MV, Roe R, Novack R, Boyer DS. Cosmetic facial fillers and severe vision loss. JAMA Opthalmol. 2014. May;132(5):637–639. doi: 10.1001/jamaophthalmol.2014.498. [DOI] [PubMed] [Google Scholar]
- 20.Daicker BC, Kreuzer G. Acquired black disc and melanotic retina after resection of an orbital meningioma. Klin Monbl Augenheilkd. 1981. November;179(5):322–329. doi: 10.1055/s-2008-1057321. [DOI] [PubMed] [Google Scholar]
- 21.Kang BK, Kang IJ, Jeong KH, Shin MK. Treatment of glabella skin necrosis injection of hyaluronic acid usind platelet rich plasma. J Cosmet Laser Ther. 2016;18(2):111–112. doi: 10.3109/14764172.2015.1052512. [DOI] [PubMed] [Google Scholar]
- 22.Kalyam K, Kavoussi SC, Ehrlich M, et al. Irreversible blindness following periocular autologous platelet-rich plasma skin rejuvenation treatment. Ophthal Plast Reconstr Surg. 2017. May/June;33(3S Suppl 1):S12–S16. doi: 10.1097/IOP.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 23.Lee W, Koh IS, Oh W, Yang EJ. Ocular complications of soft tissue filler injections: a review of literature. J Cosmet Dermatol. 2019. November 11. doi: 10.1111/jocd.13213. [DOI] [PubMed] [Google Scholar]
- 24.Humzah MD, Ataullah S, Chiang C, Malthora R, Golberg R. The treatment of hyaluronic acid aesthetic interventional induced visual loss (AIIVL): a consensus on practical guidance. J Cosmet Dermatol. 2019. February;18(1):71–76. doi: 10.1111/jocd.12672. [DOI] [PMC free article] [PubMed] [Google Scholar]


