Abstract
Patellar resurfacing during total knee arthroplasty remains a controversial topic.
Some surgeons routinely resurface the patella to avoid the increased rates of postoperative anterior knee pain and reoperation for secondary resurfacing, whilst others selectively resurface based on the presence of preoperative anterior knee pain, damaged articular cartilage, inflammatory arthritis, isolated patellofemoral arthritis, and patellar subluxation and/or maltracking. A third group of surgeons never resurface the patella.
The anatomy and biomechanics of the patellofemoral joint as well as the advances in surgical techniques and prosthetic design must be taken into account when making a decision about whether to resurface the patella. Accurate component implantation if the patella is resurfaced becomes crucial to avoid complications.
In our institution before 2008 we were performing a selective resurfacing of the patella, but in the last decade we have decided to always resurface it, with good outcomes and low complication rate. A reproducible surgical technique may be helpful in reducing the risk of postoperative anterior knee pain and complications related to implants.
In this article we analyse the current trend and controversial topics in dealing with the patella in total knee arthroplasty, and discuss the available literature in order to sustain our choice.
Cite this article: EFORT Open Rev 2020;5:785-792. DOI: 10.1302/2058-5241.5.190075
Keywords: patella, resurfacing, total knee arthroplasty
Introduction
The variability in the decision about whether to resurface the patella in total knee replacement (TKR) is influenced by different factors including geographic location, training of surgeons, implant design and level of constraint. There are currently three possible approaches to the patella during primary total knee arthroplasty: always resurface, never resurface, and selectively resurface. This last option is mainly dictated by pre and intraoperative findings such as preoperative diagnosis, quality of the articular cartilage, patellofemoral congruence and tracking at the time of surgery.
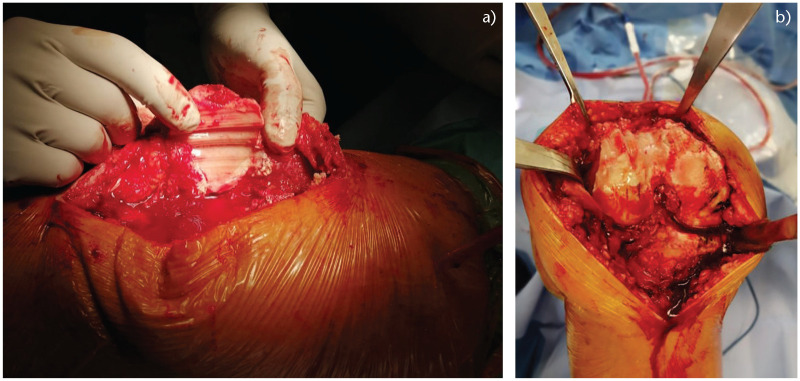
Disagreement is also present in the literature because there are different randomized controlled trials leading to different evidence and conclusions, that will be discussed in this review. In the last decade the improvement in patellar and femoral component design and some advances in the surgical technique may have made patellar resurfacing more attractive. The traditional component is a cemented and all-polyethylene patella, with a dome-shaped design to favour component insertion (Fig. 1).1 The onlay design reduces the risk of patellar fracture and the amount of sacrificed bone.
Fig. 1.
Different types of patellar resurfacing. Dome-shaped is the most common but other geometries are or have been available on the market.
Current trends and controversial topics in dealing with the patella
Geographical trends
If we look at this topic from a geographical point of view as Abdel et al did in their study,2 we will find that in North America, the majority of surgeons (> 90%) routinely resurface the patella. Patellar resurfacing is less common in Asian countries, and is carried out selectively in European nations. Research performed by Vielgut et al3 studied the percentage of patellar resurfacing in total knee arthroplasty (TKA) in 11 arthroplasty registers extracting data from the EFORT website, NORE (Network of Orthopaedic Registries of Europe) and three other international Registries (New Zealand, Canada and Australia). On one hand the Danish knee arthroplasty registry reported a 72% rate of resurfacing the patella, but only 2% of TKAs completed in Norway and 3% in Sweden had a patellar button. Percentage of patellar resurfacing was also high in Canada (70%), Portugal (65%) Australia (45%) New Zealand and England (30%). Three registries did not collect these data (Scotland, Slovakia and Catalunia). These differences between these very close countries may be justified by several factors such as education, training, tradition, experience, and/or clinical evidence, type of implant and constraint.
Furthermore, there might be some medicolegal reasons for resurfacing, such as in the US. On the other hand, when looking at the TKA design used in countries who routinely do not resurface the patella, it is often a Cruciate Retaining (CR) design. In Sweden, for instance, 92.2% of TKA are CR, and the figure is similar in Norway. Furthermore, there are less obvious issues which might influence decision making as well, such as the risk or being sued for malpractice when the patella is not resurfaced.
Surgeons’ trends
Always resurface
The reasons why surgeons decide to always resurface the patella are different and supported by several studies: multiple level 1 randomized trials and good-quality meta-analyses have shown a significantly lower rate of secondary resurfacing and reoperation.4–8 Second, although most level 1 randomized trials and subsequent meta-analyses have not shown a statistically significant difference in anterior knee pain, almost all have shown less anterior knee pain in the resurfaced group.4–8 Third, unless preoperative magnetic resonance imaging (MRI) is performed, the quality and thickness of the patella’s articular cartilage at the time of knee arthroplasty are unpredictable as well as how long it would last especially in patients with different age, level of activity, body mass index (BMI) and ethnicities. Finally, a large percentage of patients come with anterior knee pain or radiographic signs of patellofemoral arthritis or present primarily with patellofemoral arthritis, inflammatory arthritis, or diffuse synovial inflammation.
Never resurface
Surgeons who ‘never’ resurface the patella are in opposition and argue that the rate of complications related to patellar resurfacing, such as patellar fractures, poly wear or fracture, component loosening and dissociation, is unacceptable. They also contend that no study in the literature has definitively shown a clear difference between the effect of two different techniques on patellar pain and complications.
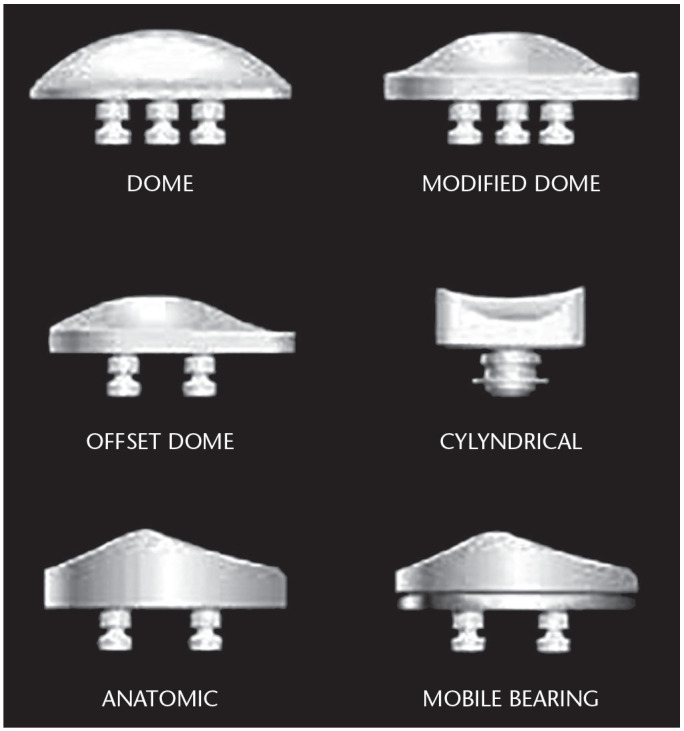
Since no meta-analysis or level 1 study has strongly favoured one philosophy over the other, both groups are able to find arguments in support of their belief. It becomes, however, difficult to justify the decision of not resurfacing in patients with severe arthritis of the patellofemoral joint or referring for anterior knee pain or for inflammatory diseases even if recent publications showed that patients with inflammatory diseases have the same risk of developing anterior knee pain as patients with OA when the patella is not resurfaced (Fig. 2).9
Fig. 2.
An example of severe patellofemoral arthritis.
Selectively resurface
Surgeons who selectively resurface the patella share the philosophy to decide intraoperatively based upon different criteria, mainly the quality of the patellofemoral cartilage. At the moment there are very few published data correlating the intraoperative status of the patellofemoral cartilage and postoperative function. One of the main reasons for not resurfacing the patella, especially in the Asian population, is related to patients’ smaller statures and thin patellar bone, as it may cause patellar fractures. The same group of surgeons, on the other hand, always perform the resurfacing when patients have inflammatory diseases such as rheumatoid arthritis or a severely damaged cartilage.2,3
However, the threshold for resurfacing the patella or not based on the quality of the cartilage, is mainly related to the surgeon’s experience and is not objectively clarified in the literature. In addition, it could be argued that the ability of the surgeon to assess articular cartilage in order to predict the outcome is doubtful, especially intraoperatively.
Implant-related issues
Design, level of constraint and type of implant may influence the choice of whether or not to resurface the patella.
In the US there are a lot of Posterior Stabilized (PS) users, as well in some countries like Denmark, where the patella is routinely resurfaced. PS design has been shown to be more prone to secondary patellar resurfacing as indicated by Maney et al.10 The design of the femoral component might play a role in the decision to resurface, typically with older designs that have a not ‘patellar friendly’ trochlea, with larger flange and thicker anterior design, with a higher transition zone from the trochlea to the intercondylar box. Improvements in the design seem to partly explain the reduction in resurfacing in the Swedish Arthroplasty Register.
Finally, when looking at the TKA design used in countries who routinely do not resurface the patella, it is often a CR design.
Surgical issues
From a surgical point of view, although some improvements have been made in recent years, the instrumentation dedicated to patellar resurfacing remains less accurate compared to the advances made in the instrumentation sets for knee replacements, and a large number of surgeons resurfacing the patella avoid their use, preferring a so-called ‘free hand’ cut.
No real advances in technology such as computer navigation, patient’s specific instruments or robotics have been developed in order to optimize patellar resurfacing, which remains a crude procedure and utilizes poor anatomic landmarks.
Patient-related issues
‘At risk’ categories
Four categories of patients deserve some attention: patients with inflammatory arthritis, obese patients, those who find stair climbing imperative, and females. For different reasons all these categories should be resurfaced. In patients with rheumatoid arthritis the patella tends to become flat and large, and a study performed in Sweden showed better results when the patella was resurfaced.11–13 Concerning obese patients, not resurfacing the patella seems less successful with a higher risk of postoperative pain, and no significant difference in postoperative complications has been found whether the patella was resurfaced or not.14,15
Concerning stair climbing, there are studies showing better performance when the patella was resurfaced and others showing no significant differences.4,6,11,16 In the preoperative phase, the opportunity of asking patients if they are a ‘stair climber or not’ can be used to aid in the decision on whether to offer surgery with or without patellar resurfacing. On the other hand, this is an issue that comes up quite often, mainly in the European countries where there is a high percentage of patients who live in old houses or blocks of flats with no elevators.
Gender can be an important variable to consider: Robertsson et al found that female patients were more satisfied with the result of patellar resurfacing than male patients in the Swedish Knee Arthroplasty Registry.13
Finally, valgus knee is considered a category where patellar resurfacing should be considered.12,13
Anatomical and functional issues
Another point to consider is that, in many cases, patellofemoral arthritis can be the consequence of a more or less dysplastic joint; a factor to consider in this case is the morphology of patella. In the past it was classified as ‘normal’, ‘small’ or ‘absent’, referring to the size of the patella compared to the femoral condyles. Further previous classifications have been proposed to evaluate patellar morphology: the most used are the Wiberg17 classification, modified by Baumgartl18 and Ficat.19 At least seven different patellar morphologies can be described in the literature (Fig. 3). In addition to the anatomical varieties we must add the deformity that derives from osteoarthritic degeneration. If we consider all these anatomical variables in addition to the different possible trochlear variables and designs, in our opinion, it can be difficult to address correct patellar tracking without addressing both the sides involved. In other words, each prosthetic design has only one type of femoral flange (‘more or less patella friendly’) where very different types of patella should adapt. Resurfacing the patella allows to play with the position of the patellar button and better place it over the femoral flange.
Fig. 3.
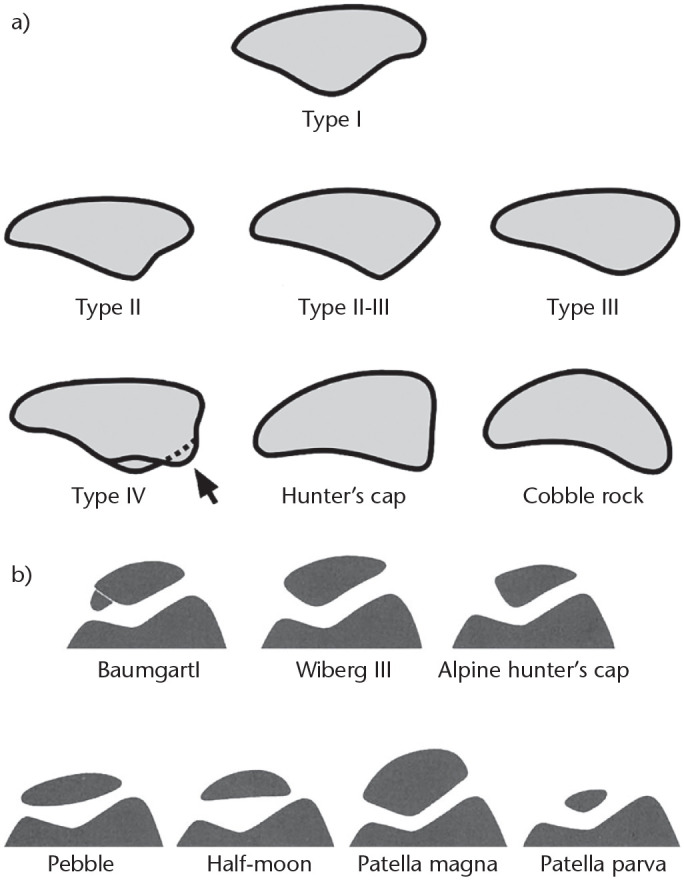
Different types of patellar shape.
Recent studies published by Saffarini et al20,21 and Kuo22 show that even the so-called patellar friendly implants are not able to restore normal morphology of the anterior femur. Using a patellar implant may therefore help to better match the two components.
Anterior knee pain after TKA
This is another controversial topic. At the moment, research into a ‘perfect’ design for patellar friendly components continues, and the science of patellar resurfacing has yet to be finalized. The selective resurfacing of the patella, for those who advocate this choice, needs to involve looking at different parameters intraoperatively, including size and thickness of patella bone, native patellar tracking, quality of articular cartilage, and presence of inflammatory synovial tissues. This large number of parameters and the difficulty of objectively judging all of them often pushes the surgeon to resurface the patella in the majority of cases.
The ability of the surgeon to assess articular cartilage in order to predict the outcome is doubtful, especially intraoperatively.23,24 The main reasons for not resurfacing the patella are the presence of viable cartilage with no exposed bone, adequate patellofemoral congruence, young age, a normally shaped patella of appropriate thickness, and no history of inflammatory diseases of any kind.14–25 Among the indications for not resurfacing the patella, the most important is a very thin and severely eroded patella where thickness of the patella even after conservative resection would be less than 10–12 mm.
Parvizi et al4 also published a comprehensive meta-analysis that included 14 prospective, randomized studies comparing un-resurfaced and resurfaced patellae in total knee arthroplasty. There was a lower relative risk of anterior knee pain in the resurfaced group compared with the un-resurfaced group (P = 0.01). They also described their results for secondary resurfacing. They found that both components of the Knee Society Score (KSS) significantly improved after the secondary procedure.
Literature evidence and review
Since 2005, various randomized controlled trials and meta-analyses have been published comparing outcomes between patients with resurfaced and un-resurfaced patellae. These studies showed a reduction in the revision rates in patients who underwent patellar resurfacing without showing a reduction in the anterior knee pain.5–7,26,27
Among the supporters of patellar resurfacing, Parvizi et al4 and Nizard et al5 were among the first to report a reduction of anterior knee pain and a lower revision rate in patients who underwent a TKA with patellar resurfacing. These data anticipate the studies of other authors, such as Adravanti et al26 who reported a wide case-series of 861 patients, clinically and radiographically evaluated at mid-term follow-up. Patients were evaluated using the knee pain scale (KPS).27 The KPS has four subscales, including frequency and intensity of pain experienced during both ambulation/climbing and transfer activities. The best possible score is 12, while the worst possible score is 66.
The authors reported that 801 patients showed a KPS < 36. Among the remaining 60 patients, 33 had a KPS > 36. Twenty-seven patients underwent further surgical procedures and among them 22 underwent revision surgery of the target knee. However, in only 0.6% of the cases of reintervention, patellofemoral complications were found to be the cause, confirming a very low rate of complications related to patellar resurfacing.
Concerning postoperative outcomes, two studies found a significantly increased KSS score in the resurfacing group compared to the non-resurfacing group.6,28 Vukadin et al evaluated the effects of patellar resurfacing in 60 patients with valgus deformity of the knee. In 30 patients treated with resurfacing they found, although not statistically relevant, a higher clinical and functional improvement in the examined clinical scores compared to the patients who did not undergo patellar resurfacing. Valgus knee deformity, rheumatic disease, patellofemoral arthritis and maltracking are contemporary indications supporting patellar resurfacing.29 James F. Fraser30 published in 2017 a systematic review of the literature from 2004 to 2014 using registry data from Australia, Denmark, England, New Zealand, Norway and Sweden. The reported data showed low resurfacing rates in the northern Europe, with Norway at 4% and Sweden having the most significant reduction of the procedure (from 15% to 2%). The USA reported higher rates (80%), and Australia had a major increase from 49% to 55% in the study period. Fraser and Spangehl showed that the resurfacing was associated with a lower revision rate, as described earlier, without influencing anterior knee pain.30
Chen et al6 showed opposite conclusions in a literature metanalysis. They did not find statistically significant differences in anterior knee pain, and they also associated patellar resurfacing with a higher rate of intraoperative fractures (fixation with a single central peg has been suggested to increase the risk of fracture), as well as with the other classical risks related to prosthetic implant, such as loosening.8 The incidence of loosening has ranged across studies from 0.4% to 4%31 and has decreased since the introduction of dome-shaped patellar implants. In the 2014 Swedish Knee Arthroplasty Registry Annual Report, patella resurfacing was actually found to increase the risk of revisions from 2003 to 2012 with a relative risk of 1.2 (CI 1⁄4 1.1–1.4) when compared with un-resurfaced patellae in primary TKA.32 In their randomized controlled trial, Burnett et al33 analysed 64 patients who underwent total knee replacement, comparing the clinical results obtained in patients in whom patellar resurfacing was performed and those in whom the procedure had not been performed. As also suggested in the previous literature,6,34,35 no clinical difference was found in the two groups either for range of motion or for scores (Knee Society Clinical Rating Score), or in the rate of revision and anterior knee pain. This study, in our opinion, is important because it refers to results with a long-term follow-up (10 years) without showing significant complications or disadvantages related to the procedure.
In a review, Putman et al36 suggested that complications on the patella after a TKA are associated with different factors, related to the patient (valgus knee, obesity, lateral retinacular release, and a thin patella) and to the surgery. Among these are an asymmetric bone cut with a greater than 2-mm difference in medial vs. lateral, lateral release (and consequent patellar blood supply compromised with risk of fracture on necrotic base), and femoral and/or tibial rotational malalignment.37 The authors stress the fact that particular attention should be paid to femoral internal rotation, which, when present, can produce patellar maltracking with subsequent patellar instability38 and stiffness as assessed by Berger et al39 who performed a combined analysis of component rotation, both on the femur and on the tibia: combined internal rotation of 1° to 4° correlated with patellar tilting and maltracking, combined internal rotation of 3° to 8° with patellar subluxation, and combined internal rotation in of 7° to 17° with patellar dislocation.
Another point of discussion is the infection rate that seems not to be influenced by the resurfacing of the patella,40 as shown by a previous systematic review. These findings demonstrate that the longer surgical time taken for the resurfacing does not increase the risk of infection.
Concerning surgical technique and choice of implant, patellar thickness may be critical in influencing outcomes and range of motion as shown in studies by Lee et al and Ritter et al.40,41 When a patellar resurfacing is performed, restoring the native patellar thickness is a crucial point to achieve optimal range of motion (ROM) and the patient’s clinical satisfaction as shown by Devers et al42 (quality of life, SF-36 and Western Ontario and McMaster University. To restore native patellar thickness can be key to improve subjective outcomes as shown by Alcerro et al.43 Moreover, Roessler et al44 showed that patella tilt, patella height and thickness, as well as the delta angle, were significant predictors of a need for secondary patellar resurfacing after primary TKA.
Ghosh et al underlined in their study that anterior overstuffing may lead to decreased flexion, patellofemoral maltracking, subluxation, increased patellofemoral compression and shear forces contributing to increased component wear, and possibly pain compromising outcomes.45 Less discussed in the literature but as important as overstuffing is understuffing of the third compartment, which may lead to patellar instability, reduction of the quadriceps lever arm and extension-lag.43 It can be a complication of either resurfacing or non-resurfacing of the patella.
In support of resurfacing, a cost-effectiveness analysis was conducted by Weeks et al46 in 2018: the authors use a decision analytic model representing a hypothetical TKA cohort, with or without patellar resurfacing, using data from the 2014 Australian Registry. Their results suggest that TKA with resurfacing is cost-effective compared to not resurfacing. Not resurfacing the patella resulted in higher costs and lower quality-adjusted life year at 14 years; the authors suggest that this point is connected with the higher revision rates for un-resurfaced TKA.
A very recent meta-analysis published by Migliorini et al47 showed overall better outcomes with patellar resurfacing, detecting a lower rate of postoperative anterior knee pain and reoperation. Moreover, the resurfacing group showed greater value of the Hospital for Special Surgery Score (HSS), KSS and related subscales. In favour of the retaining group, a slightly better ROM was evidenced.
A meta-analysis published by Teel et al48 only partially agrees, and stresses the risk of reoperation, showing that the only clear relationship is that knees that do not receive patellar resurfacing are more likely to receive reoperation, most often for secondary resurfacing. However, the disease burden of differing complication profiles associated with resurfacing and non-resurfacing groups remains unclear.
Finally, concerning secondary replacement of the patella and its potential benefits and risks, a meta-analysis published by Van Jonbergen et al49 showed significant improvement in knee scores in all nine considered studies that reported functional outcomes, although no clinically significant improvement in knee scores was observed. Moreover, reported complications include infections and impaired wound healing, patellar instability, and patellar fracture. They concluded that because the available evidence is of generally low quality, the results of this systematic review only support a weak recommendation for secondary patellar resurfacing if patient satisfaction and clinically important improvement of functional outcomes are the desired endpoints.
Tips for patellar resurfacing
To optimize patellar resurfacing, the surgical technique should be the most possibly reproducible and follow some key points. First of all, the removal of synovial tissue and peripatellar osteophytes is necessary for an adequate exposure. The level of resection is indicated by the chondro-osseous junction as well as the insertion of the tendons which can be outlined using electrocautery (it is not a denervation).The resection can be carried out free-hand or with dedicated instruments keeping the sawblade parallel to the anterior surface of the patella. It is important to measure the patella before resection to restore the previous thickness (mean thickness is 26 mm for males and 23 mm for females); around 15 mm of native bone is necessary to reduce the risk of fracture and adequate restoration of patellar thickness is critical to maximize efficiency. It is important to avoid an asymmetric cut. The medial facet is typically thicker than the lateral side. A lateral facetectomy is often necessary and recommended after a recommended 2.5 mm medialization of the patellar button. Superior placement of the patellar component is also recommended in order to minimize patellar clunk and catching in the intercondylar region.
Conclusions
Patellar resurfacing in total knee replacement is still a controversial topic within the orthopaedic community. We support resurfacing of this joint. In our opinion, resurfacing the patella is a reproducible and safe procedure, and may reduce the risk of anterior knee pain, additional surgery to replace the patella in a second step (most of the time unsuccessful) in the hope of avoiding stiffness and anterior pain, and revision. The technique must be accurate both for the patellar implant as well for the femoral component, in terms of rotational alignment. Resurfacing the patella can also aid in the optimization of the patella femoral tracking, while positioning the plastic button accordingly (proximal and medial positioning, while optimizing the thickness of the construct). Finally, the matching of two purposely designed surfaces (patella and flange) avoids the risk of forcing different anatomically shaped patellae into a metal surface of one single design (Fig. 4 and Fig. 5).
Fig. 4.

Preoperative X-rays of a patient with three-compartmental knee arthritis on the right side and severe patellofemoral degeneration.
Fig. 5.
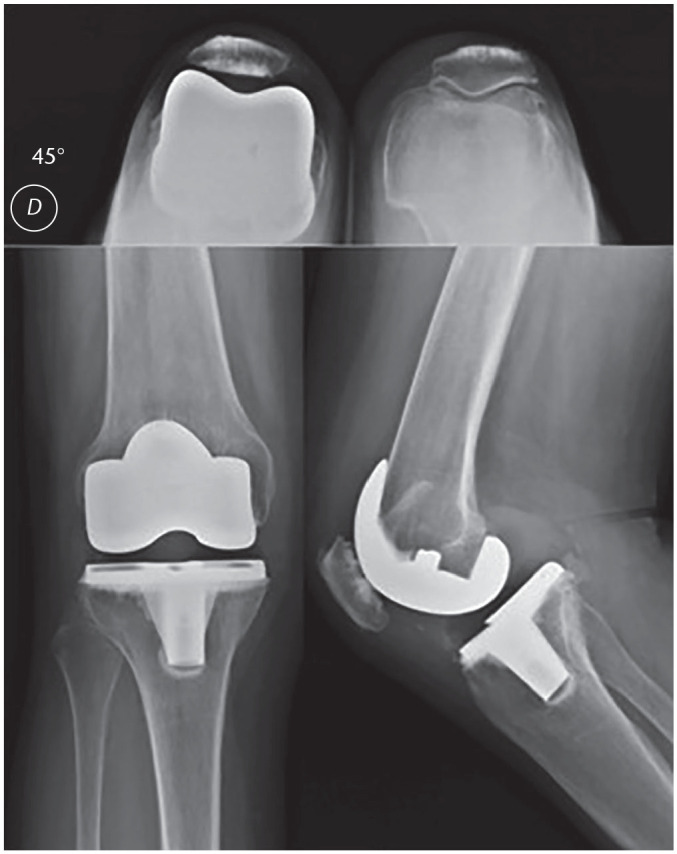
Postoperative X-rays of the patient shown in Fig. 4, demonstrating good alignment of the femoral and tibial components, good restoration of patellar height and patellar tracking.
Footnotes
ICMJE Conflict of interest statement: FB reports consultancy for Zimmer Biomet and Limacorporate, grants/grants pending from Limacorporate, payment for lectures including service on speakers’ bureaus from Zimmer Biomet and Limacorporate, royalties from Zimmer Biomet and Limacorporate, and payment for development of educational presentations from Zimmer Biomet, Limacorporate and Fidia, all outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Norman Scott W. Patella resurfacing – always. Insall & Scott. Surgery of the knee. Sixth edition New York: Elsevier, 20171637–1646. [Google Scholar]
- 2. Abdel MP, Parratte S, Budhiparama NC. The patella in total knee arthroplasty: to resurface or not is the question. Curr Rev Musculoskelet Med 2014;7:117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vielgut I, Kastner N, Pichler K, et al. Application and surgical technique of total knee arthroplasties: a systematic comparative analysis using worldwide registers. Int Orthop 2013;37:1465–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res 2005;438:191–196. [DOI] [PubMed] [Google Scholar]
- 5. Nizard RS, Biau D, Porcher R, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res 2005;432:196–203. [DOI] [PubMed] [Google Scholar]
- 6. Chen K, Li G, Fu D, Yuan C, Zhang Q, Cai Z. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop 2013;37:1075–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am 2011;93:1301–1309. [DOI] [PubMed] [Google Scholar]
- 8. Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am 2012;94:2270–2278. [DOI] [PubMed] [Google Scholar]
- 9. Pehlivanoglu T, Balci HI, Demirel M, Cakmak MF, Yazicioglu O, Kil icoglu OI. Prevalence of anterior knee pain after patellar retention total knee arthroplasty: comparison of patients with rheumatoid arthritis versus primary osteoarthritis. Acta Orthop Traumatol Turc 2019;53:420–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maney AJ, Frampton CM, Young SW. Age and prosthetic design as risk factors for secondary patella resurfacing. J Arthroplasty 2020;35:1563–1568. [DOI] [PubMed] [Google Scholar]
- 11. Picetti GD, III, McGann WA, Welch RB. The patellofemoral joint after total knee arthroplasty without patellar resurfacing. J Bone Joint Surg Am 1990;72:1379–1382. [PubMed] [Google Scholar]
- 12. Scott WN, Kim H. Resurfacing the patella offers lower complication and revision rates. Orthopedics 2001;24:24. [DOI] [PubMed] [Google Scholar]
- 13. Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 2000;71:262–267. [DOI] [PubMed] [Google Scholar]
- 14. Kawakubo M, Matsumoto H, Otani T, Fujikawa K. Radiographic changes in the patella after total knee arthroplasty without resurfacing the patella: comparison of osteoarthrosis and rheumatoid arthritis. Bull Hosp Jt Dis 1997;56:237–244. [PubMed] [Google Scholar]
- 15. Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am 2002;84:187–193. [DOI] [PubMed] [Google Scholar]
- 16. Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br 1996;78:226–228. [PubMed] [Google Scholar]
- 17. Wiberg G. Rontgenographic and anatomic studies on the femoropatellar joint: with special reference to chondromalacia patellae. Acta Orthop Scand 1941;12:319–410. [Google Scholar]
- 18. Baumgartl F. Das Kniegelenk. Berlin: Springer Verlag, 1964. [Google Scholar]
- 19. Ficat P. Pathologie fémoro-patellaire. Paris: Masson, 1970. [Google Scholar]
- 20. Saffarini M, Demey G, Nover L, Dejour D. Evolution of trochlear compartment geometry in total knee arthroplasty. Ann Transl Med 2016;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Müller JH, Li K, Reina N, Telmon N, Saffarini M, Cavaignac E. Sexual and ethnic polymorphism result in considerable mismatch between native trochlear geometry and off-the-shelf TKA prostheses. Knee Surg Sports Traumatol Arthrosc 2020. doi: 10.1007/s00167-020-05871-3 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22. Kuo AW, Chen DB, Wood J, MacDessi SJ. Modern total knee arthroplasty designs do not reliably replicate anterior femoral morphology. Knee Surg Sports Traumatol Arthrosc 2019. doi: 10.1007/s00167-019-05610-3 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23. Kim BS, Reitman RD, Schai PA, Scott RD. Selective patellar nonresurfacing in total knee arthroplasty: 10 year results. Clin Orthop Relat Res 1999;367:81–88. [PubMed] [Google Scholar]
- 24. Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am 2003;85:212–217. [DOI] [PubMed] [Google Scholar]
- 25. Soudry M, Mestriner LA, Binazzi R, Insall JN. Total knee arthroplasty without patellar resurfacing. Clin Orthop Relat Res 1986;205:166–170. [PubMed] [Google Scholar]
- 26. Adravanti P, Tecame A, De girolamo L, Ampollini A, Papalia R. Patella resurfacing in total knee arthroplasty: a series of 1280 patients at midterm follow-up. J Arthroplasty 2018;33:696–699. [DOI] [PubMed] [Google Scholar]
- 27. Rejeski WJ, Ettinger WH, Jr, Shumaker S, et al. The evaluation of pain in patients with knee osteoarthritis: the knee pain scale. J Rheumatol 1995;22:1124–1129. [PubMed] [Google Scholar]
- 28. Sandiford NA, Alao U, Salamut W, Weitzel S, Skinner JA. Patella resurfacing during total knee arthroplasty: have we got the issue covered? Clin Orthop Surg 2014;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vukadin OB, Blagojević ZB, Baščarević ZL, Slavković NS, Stevanović V, Vukomanović BD. The importance of patellar resurfacing in total knee arthroplasty for symptomatic valgus degenerative deformity. Acta Chir Orthop Traumatol Cech 2017;84:30–34. [PubMed] [Google Scholar]
- 30. Fraser JF, Spangehl MJ. International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014. J Arthroplasty 2017;32:83–86. [DOI] [PubMed] [Google Scholar]
- 31. Healy WL, Wasilewski SA, Takei R, Oberlander M. Patellofemoral complications following total knee arthroplasty: correlation with implant design and patient risk factors. J Arthroplasty 1995;10:197–201. [DOI] [PubMed] [Google Scholar]
- 32. The Swedish Knee Arthroplasty Register: Annual reports 2003–2014.
- 33. Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res 2007;464:65–72. [DOI] [PubMed] [Google Scholar]
- 34. Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am 2005;87:1438–1445. [DOI] [PubMed] [Google Scholar]
- 35. Fu Y, Wang G, Fu Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2011;19:1460–1466. [DOI] [PubMed] [Google Scholar]
- 36. Putman S, Boureau F, Girard J, Migaud H, Pasquier G. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res 2019;105:S43–S51. [DOI] [PubMed] [Google Scholar]
- 37. Huten D, Basselot F, Gicquel H, Common H. Rotation fémorale dans les prothèses de genou. In: Lustig S, Parratte S, eds. Prothèses totales de genou. Paris: Elsevier, 2016:123–139. [Google Scholar]
- 38. Grassi A, Compagnoni R, Ferrua P, et al. Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc 2018;26:3206–3218. [DOI] [PubMed] [Google Scholar]
- 39. Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 1998;356:144–153. [DOI] [PubMed] [Google Scholar]
- 40. Lee QJ, Yeung ST, Wong YC, Wai YL. Effect of patellar thickness on early results of total knee replacement with patellar resurfacing. Knee Surg Sports Traumatol Arthrosc 2014;22:3093–3099. [DOI] [PubMed] [Google Scholar]
- 41. Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty: clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 2003;85:1278–1285. [DOI] [PubMed] [Google Scholar]
- 42. Devers BN, Conditt MA, Jamieson ML, Driscoll MD, Noble PC, Parsley BS. Does greater knee flexion increase patient function and satisfaction after total knee arthroplasty? J Arthroplasty 2011;26:178–186. [DOI] [PubMed] [Google Scholar]
- 43. Alcerro JC, Rossi MD, Lavernia CJ. Primary total knee arthroplasty: how does residual patellar thickness affect patient-oriented outcomes? J Arthroplasty 2017;32:3621–3625. [DOI] [PubMed] [Google Scholar]
- 44. Roessler PP, Moussa R, Jacobs C, et al. Predictors for secondary patellar resurfacing after primary total knee arthroplasty using a ‘patella-friendly’ total knee arthroplasty system. Int Orthop 2019;43:611–617. [DOI] [PubMed] [Google Scholar]
- 45. Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA. The effect of over-stuffing the patellofemoral joint on the extensor retinaculum of the knee. Knee Surg Sports Traumatol Arthrosc 2009;17:1211–1216. [DOI] [PubMed] [Google Scholar]
- 46. Weeks CA, Marsh JD, MacDonald SJ, Graves S, Vasarhelyi EM. Patellar resurfacing in total knee arthroplasty: a cost-effectiveness analysis. J Arthroplasty 2018;33:3412–3415. [DOI] [PubMed] [Google Scholar]
- 47. Migliorini F, Eschweiler J, Niewiera M, El Mansy Y, Tingart M, Rath B. Better outcomes with patellar resurfacing during primary total knee arthroplasty: a meta-analysis study. Arch Orthop Trauma Surg 2019;139:1445–1454. [DOI] [PubMed] [Google Scholar]
- 48. Teel AJ, Esposito JG, Lanting BA, Howard JL, Schemitsch EH. Patellar resurfacing in primary total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty 2019;34:3124–3132. [DOI] [PubMed] [Google Scholar]
- 49. Van Jonbergen HPW, Boeddha AV, van Raaij JJAM. Patient satisfaction and functional outcomes following secondary patellar resurfacing. Orthopedics 2016;39:e850–e856. [DOI] [PubMed] [Google Scholar]