Abstract
The purpose of the current study was to describe the femoral and patellar insertions of the lateral patellofemoral ligament (LPFL) and to determine their location relative to known anatomic and radiographic landmarks. In this descriptive laboratory study, 10 cadaveric knees were dissected, and the patellar and femoral insertions of the LPFL were identified. Each specimen was examined radiographically. The average center of the femoral insertion of the LPFL was calculated in reference to radiographic landmarks.
Introduction
Symptomatic medial instability of the patellofemoral joint is an uncommon clinical entity that can occur after surgical release of the lateral retinaculum of the knee.1–3 Further, diagnosis and treatment of medial subluxation of the patella is difficult, and various surgical treatments have been proposed, such as lateral retinacular repair and isometric lateral patellofemoral ligament (LPFL) reconstruction.4, 5 The knee structures responsible for restraining the medial displacement of the patella include the iliotibial band (ITB), the LPFL, and the lateral patellotibial ligament.6, 7 The lateral stability of the patella, on the other hand, is maintained by the medial patellofemoral ligament (MPFL), medial patellotibial ligament, and medial patellomeniscal ligament, of which the MPFL provides the major restrictive force.8
The gross anatomy of the LPFL and MPFL and their biomechanical participation in the patellofemoral joint are well studied.7–16 For the lateral structures, two distinct fascial layers—superficial and oblique—have been identified within the lateral retinaculum.6 Deep to the retinaculum, two transverse bands exist, one extending from the ITB to the patella (the patellotibial band) and the other from the femur to the patella (the epicondylopatellar band).6 At the lateral aspect of the distal femur, the most superficial layer of the retinaculum is a deep fascial layer, and deep to it exists the obliquely oriented fibers described as arciform fibers.17 Deep to the arciform fibers are the fibers extending directly from the lateral aspect of the quadriceps tendon and the ITB. The deepest two layers are the ITB-patella fibers and the LPFL.7, 14 Merican et al7 described the LPFL as a thickening of the joint capsule and noted that there was also a thickening of the joint capsule extending to the lateral meniscus. In their study investigating the strength of the intermediate structures of the lateral retinaculum, they also identified three distinct structures in the deep lateral retinaculum, namely the ITB-patella, LPFL, and lateral patellomeniscal ligaments.7
Current techniques for LPFL reconstruction include testing before definitive graft placement to identify an isometric point for the graft. To our knowledge, reconstruction of the LPFL based on anatomic insertions at the femur and patella has not been previously described, and radiographic landmarks for the femoral LPFL insertion are currently unknown.4, 5, 18, 19 Such information would be useful to surgeons performing LPFL reconstruction to confirm anatomic placement of the reconstruction soft tissue graft. Therefore, the purpose of the current study was to describe the femoral and patellar insertions of LPFL and to determine their location relative to known anatomic and radiographic landmarks.
Methods
Dissection of the LPFL was performed on 10 embalmed cadaveric knees. The cadavers were randomly selected from the anatomy teaching laboratory at A.T. Still University’s Kirksville College of Osteopathic Medicine (ATSU-KCOM). Standard embalming procedures were used, and all cadavers had undergone double embalming preservation, first with an embalming solution at the funeral home followed by an embalming solution containing 26.25% isopropanol, 11.75% ethylene glycol, 8.5% phenol, 1.25% formaldehyde, 1.25% methanol, and 51% water in the Anatomy Department at ATSU-KCOM. Cadavers were infused with embalming solution through a cannulated right carotid artery and were filled passively for 48 hours. The cadavers were kept at room temperature (approximately 21°C) in the teaching laboratory. The local institutional review board considered the current study exempt.
Dissection procedures were carried out in a consistent manner between specimens. The skin and superficial fascia about the knee were removed. A medial arthrotomy was performed, extending from the quadriceps tendon to the patellar tendon insertion at the tibia. The patellar tendon was released from the tibial tuberosity and reflected superiorly. All attachments to the superior portion of the patella were then removed, leaving only the patellar tendon distally and the lateral retinaculum attached to the patella. The quadriceps muscles were reflected superiorly to the mid-femur, allowing for transection of the femur.
The lateral retinaculum is composed of a dense connective tissue sheath that forms the lateral portion of the joint capsule.7 Associated with the lateral retinaculum are multiple distinct bundles of connective tissue forming three ligaments: the patellar portion of the ITB, the LPFL, and the lateral patellotibial ligament.7 The patellar portion of the ITB is the most superficial of the ligaments and is composed of thickened bands of deep fascia that contain laterally oriented fibers that insert onto the lateral aspect of the patella.7 The ITB attachment to the lateral aspect of the patella was released followed by a complete removal of the iliotibial tract. Removal of the entire iliotibial tract allowed for better visualization of the lateral retinaculum and isolation of the LPFL.
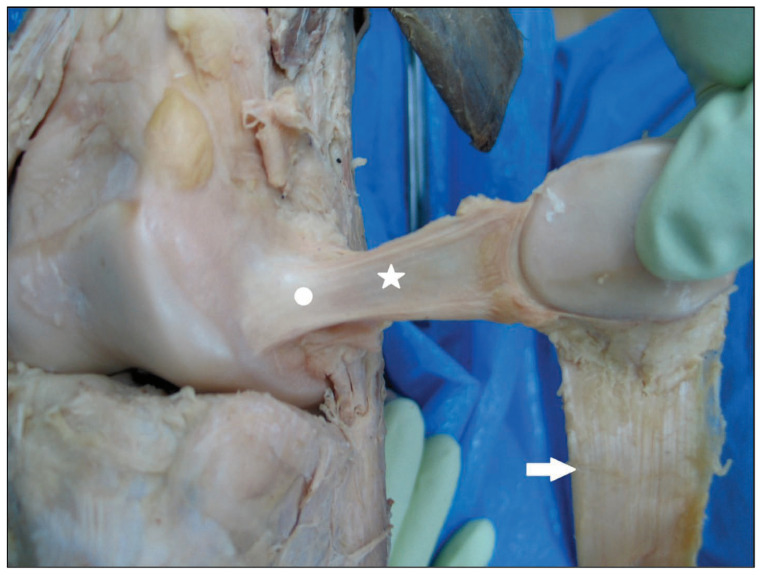
The LPFL, which is immediately deep to the patellar portion of the ITB, originates on the lateral epicondyle of the femur and inserts on the lateral patella.7 Gross inspection of the ligament confirmed that it appeared to be a thickened band of fibers within the lateral retinaculum and joint capsule. The portions of lateral retinaculum attached to the LPFL were released both superiorly and inferiorly from the patella and femur, which allowed isolation of the LPFL and made it the only soft tissue attachment from the femur to the patella (Figure 1).
Figure 1.
Anatomic dissection of the lateral patellofemoral ligament (LPFL). The LPFL (white star) was consistently identified with insertions at the lateral border of the patella and near the lateral femoral epicondyle (white dot). Also pictured is the patellar tendon (arrow) after release from the tibial tuberosity.
Disarticulation of the femorotibial joint was performed to allow for inspection and proper imaging. The anterior and posterior cruciate ligaments, the medial and lateral collateral ligaments, and the meniscotibial ligaments were transected. The muscles of the posterior compartment of the thigh were detached from their distal attachments and reflected superiorly to mid-femur. The proximal attachment of the gastrocnemius was released from the posterior femur and reflected distally. The popliteal nerves and vessels were transected and reflected superiorly and inferiorly. The femur was transected about 20 cm proximal to the distal femoral condyles, and the patellofemoral portion—the patella, distal femur, and LPFL—was removed from the specimen.
To image each specimen, the patella was everted to extend the LPFL (Figure 1). The patella was fixed in a clamp device, which allowed photographs to be taken at the same distance for each specimen. A metric ruler was incorporated into the image to allow image analysis and to verify measurements. The image obtained with the camera showed the attachment of the LPFL to the patella. In eight specimens, the LPFL was detached from the lateral femoral insertion, marked using a felt tip pen, and photographed using digital photography.
The eight intact patellofemoral specimens were used for radiographic imaging of the femoral insertion of the LPFL. The visual center of the LPFL femoral attachment was approximated and marked with a radiopaque metal pin. Using live fluoroscopy, each specimen was rotated to obtain a “perfect lateral” knee radiograph, in which the posterior condyles were precisely overlapped on the image. Radiographs were obtained and stored to a digital picture archiving and communication system (PACS). The radiopaque markers were identified, and measurements from the center of the LPFL to the corticomedullary line anteriorly, inferiorly, and posteriorly were obtained using the metal pin as a reference. Using PACS imaging software, the average radiographic center of the femoral attachment of the LPFL was calculated. The average center of the femoral insertion of the LPFL was calculated in reference to specific radiographic landmarks, namely, Blumensaat’s line and the posterior surface of the femoral cortex.
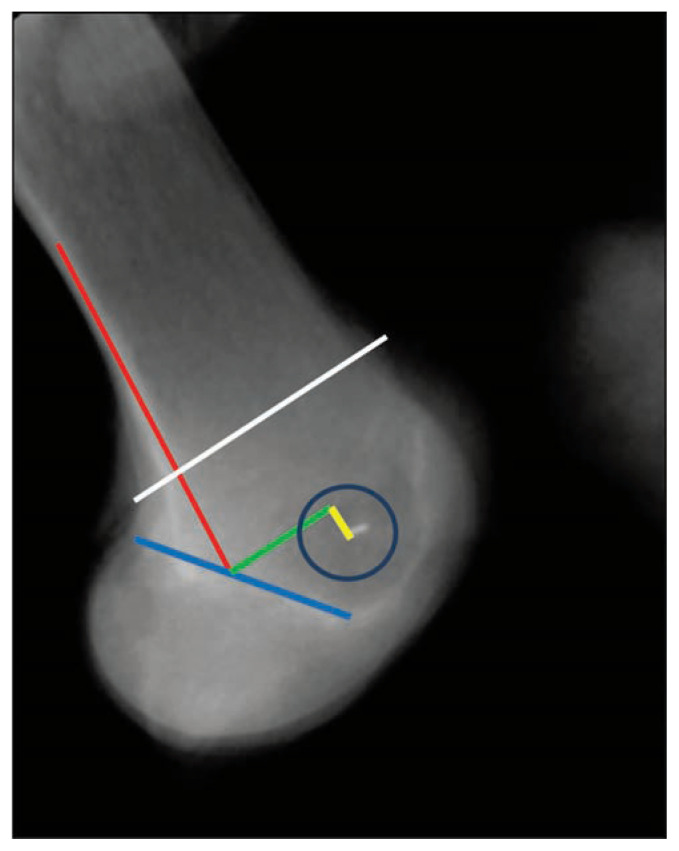
To account for size variation, regression analysis was used to determine whether the insertion of the LPFL could be identified by the anterior-posterior distance of the distal femoral shaft at the junction of the posterior femoral condyle and the femoral shaft (Figure 2, white line). Specifically, the anterior distance from the junction of the posterior femoral cortical extension line and Blumensaat’s line to the LPFL insertion point (green line) and the distal distance to the LPFL insertion point (yellow line) were calculated using the following equations:
Figure 2.
Lateral radiograph of the distal femur and landmarks for identification of the insertion of the lateral patellofemoral ligament (LPFL). The insertion of the posterior femoral cortical extension line (red line) and Blumensaat’s line (blue line) serve as the starting point for identification of the LPFL insertion (blue circle). Using regression analysis, the anteroposterior distance of the distal femoral shaft at the junction of the posterior femoral condyles perpendicular to the axis of the femur (white line) was correlated with the anterior distance (green line) and the distal distance to the LPFL insertion point (yellow line).
The coefficient of determination (R2) was used to determine the predictability of the regression model.
Results
The patellar insertion of the LPFL was found to consistently encompass the entire lateral margin of the patella. The average radiographic center (Figure 2) of the femoral insertion of the LPFL (blue circle) on a lateral radiograph was 13.9 mm (95% CI, 9.9–17.8 mm) anterior (green line) and 5.3 mm (95% CI, 2.5–8.0 mm) distal (yellow line) to the intersection of a line extending from Blumensaat’s line (blue line) and the posterior femoral cortex (red line).
The regression analysis for size variation found coefficients of determination of 0.71 for the green line and 0.74 for the yellow line.
Discussion
The purpose of the current study was to describe the femoral and patellar insertions of LPFL and to determine their location relative to known anatomic and radiographic landmarks. We identified a relatively consistent radiographic femoral insertion of the LPFL, which was correlated with the anteroposterior diameter of the distal femur on the lateral view of the knee.
Lateral patellar dislocation is a common injury that occurs at a rate of 5.8 to 77 per 100,000 individuals and has a similar incidence as that of anterior cruciate ligament ruptures in young athletes.20 The mechanism of patellar dislocation most commonly involves a valgus moment of the knee joint with external tibial rotation under eccentric contraction of the quadriceps.20 This injury can occur in athletes during a planting and pivoting movement. Often, the patella will spontaneously reduce with forceful extension of the knee. Redislocation is frequent at a rate of 14%–55%, and 50% of patients experience symptomatic pain.20 Patient complaints are medial peripatellar knee pain caused by damage of the medial structures, specifically the MPFL, that stabilize the patella leading to pain or instability. Without associated injuries, conservative treatment of the patella region is recommended for first-time dislocations.20
The MPFL is the primary restraint to lateral translation of the patella and accounts for 53%–67% of the medial restraining force, especially in the first 30° of knee flexion prior to patellar engagement in the femoral trochlea.20, 21 Incidentally, the MPFL is injured in 94% of lateral patellar dislocations and most commonly at the femoral attachment.22 The anatomy of the MPFL is well described as 55 mm long and ranging from 3–30 mm in width. The location of the femoral attachment has been noted to be 9.5 ± 1.8 mm proximal and 5.0 ± 1.7 mm posterior of the center of the medial epicondyle.18–22
Surgical reconstruction of the MPFL is often prescribed for patients who have poor outcomes from conservative treatment. Studies investigating MPFL reconstruction suggest excellent outcomes and low recurrence rates. For instance, a meta-analysis of eight studies that involved 186 MPFL reconstructions (mean patient age=24 years) showed a low recurrence rate, and the authors noted that MPFL reconstruction provided “favorable clinical and radiographic outcomes.”23 Buckens et al24 reviewed 14 studies (level of evidence III and IV) and also found low recurrence rates and favorable outcomes. Based on the available data, however, the authors noted that the current research was heterogenous and without long-term outcomes data.24 Despite these limitations, they suggested MPFL reconstruction was superior to extensor mechanism realignment procedures and older stabilization techniques.24 Others have also recommended MPFL reconstruction, noting that osseous realignment should be rethought and that MPFL reconstruction is probably a more patient friendly option.20, 24
Medial instability of the patella is a much less common clinical finding. This diagnosis is difficult and relies on a careful history and thorough physical examination. Patients often describe a history of arthroscopic or open release of the lateral retinaculum of the knee. Knee function is markedly impaired, and patients may have had previous surgical procedures to correct instability of the extensor mechanism with subsequent scar tissue formation, synovitis, and possibly muscle atrophy.4 Diagnostic criteria include the ability to passively subluxate or dislocate the patella medially while reproducing the patient’s symptoms.2
Treatment of medial patellar instability is difficult and includes operative and nonoperative options. Repair and reconstruction of the lateral stabilizing ligaments have been previously described, but an anatomic reconstruction of the LPFL has not been presented in the literature. Hughston et al2 described various surgical techniques for the treatment of medial patellar subluxation. For instance, they suggested direct lateral retinacular repair with and without vastus lateralis repair could be performed if retinacular tissue was sufficient.2 When insufficient lateral retinacular tissue was present, one of three procedures were suggested to reconstruct the patellotibial ligament.2 The first method involved the detachment of a 3–4 cm strip of iliotibial band, leaving the distal insertion intact at Gerdy’s tubercle.2 The second method involved detachment of the lateral one-fourth of the patellar tendon from the tibial tubercle and subsequent reattachment to the lateral tibial tubercle.2 The third method was a combined technique involving an anastomosis of a strip of ITB and lateral patellar tendon.2 Another surgical technique was described by Tietge et al25 and used a 4–5 cm × 1 cm partial-thickness quadriceps tendon graft. For this technique, an isometric point is identified using a commercially available isometer at the lateral femoral epicondyle.25
Recently, a surgical reconstruction of the lateral patellofemoral ligament with a gracilis tendon allograft has been suggested.26, 27 One of the pitfalls of the procedure was a failure to accurately identify the site of the femoral attachment of the lateral patellofemoral ligament.27 Correct identification of this site using radiographic landmarks described in the current study could aid in avoiding this pitfall.
With better understanding of the anatomical structure of the lateral aspect of the knee, reconstructive surgery is becoming a more valid choice of treatment for medial patellar subluxation. Although LPFL reconstruction has been previously described, correlations to anatomical descriptions of the ligament have not been well documented.25 The known lateral patellar stabilizing structures are the ITB, the LPFL, and the lateral patellomeniscal ligament; and distinct superficial and oblique fascial layers have been identified in the lateral retinaculum.6 Two transverse bands of tissue exist deep to the retinaculum, one extending from the ITB to the patella and the other from the femur to the patella, which are known as the patellotibial and epicondylopatellar bands, respectively.6
The current study had sampling bias as a limitation. All knee specimens were obtained from cadavers at a gross anatomy laboratory, and all cadavers were donated through the body donation program.
Conclusion
In the current study, we identified a relatively consistent radiographic femoral insertion of the LPFL at on a lateral radiograph at 13.9 mm (95% CI, 9.9–17.8 mm) anterior and 5.3 mm (95% CI, 2.5–8.0 mm) distal to the intersection of a line extending from Blumensaat’s line and the posterior femoral cortex (red line). To our knowledge, radiographic landmarks had not been established for the LPFL insertion before our study. Such landmarks have been proposed for the MPFL; Redfern et al28 suggested the radiographic insertion was 0.5 mm anterior to the distal posterior cortex and 3 mm proximal to the apex where it meets Blumensaat’s line. Our results suggested the consistent radiographic femoral insertion of the LPFL was size-referenced to the anteroposterior diameter of the distal femur on the lateral view of the knee. These newly identified radiographic landmarks for the attachment of the LPFL may have important clinical implications and may be used to assist surgeons in reconstructing the LPFL when indicated.
Footnotes
Kevin Marberry, MD, (above), is in the Department of Surgery at Kirksville College of Osteopathic Medicine, A.T. Still University, Kirksville, Missouri. Karl Boehm, DO, is at Christus Spohn Memorial Hospital, Corpus Christy, Texas. Fredrick Korpi, DO, is at Spectrum Orthopedics, Columbus, Ohio. Jane Johnson, MA, is at the A.T. Still Research Institute, and Peter Kondrashov, PhD, is in the Anatomy Department, Kirksville College of Osteopathic Medicine, A.T. Still University, Kirksville, Missouri.
Disclosure
None reported.
References
- 1.Betz RR, Magill JT, 3rd, Lonergan RP. The percutaneous lateral retinacular release. Am J Sports Med. 1987;15(5):477–482. doi: 10.1177/036354658701500508. [DOI] [PubMed] [Google Scholar]
- 2.Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16(4):383–388. doi: 10.1177/036354658801600413. [DOI] [PubMed] [Google Scholar]
- 3.Saper MG, Shneider DA. Medial patellar subluxation: diagnosis and treatment. Am J Orthop (Belle Mead NJ) 2015;44(11):499–504. [PubMed] [Google Scholar]
- 4.Hughston JC, Flandry F, Brinker MR, Terry GC, Mills JC., 3rd Surgical correction of medial subluxation of the patella. Am J Sports Med. 1996;24(4):486–491. doi: 10.1177/036354659602400413. [DOI] [PubMed] [Google Scholar]
- 5.Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med. 1994;22(5):680–686. doi: 10.1177/036354659402200517. [DOI] [PubMed] [Google Scholar]
- 6.Fulkerson JP, Gossling HR. Anatomy of the knee joint lateral retinaculum. Clin Orthop Relat Res. 1980;(153):183–188. [PubMed] [Google Scholar]
- 7.Merican AM, Sanghavi S, Iranpour F, Amis AA. The structural properties of the lateral retinaculum and capsular complex of the knee. J Biomech. 2009;42(14):2323–2329. doi: 10.1016/j.jbiomech.2009.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hinckel BB, Gobbi RG, Demange MK, et al. Medial patellofemoral ligament, medial patellotibial ligament, and medial patellomeniscal ligament: anatomic, histologic, radiographic, and biomechanical study. Arthroscopy. 2017;33(10):1862–1873. doi: 10.1016/j.arthro.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Baldwin JL. The anatomy of the medial patellofemoral ligament. Am J Sports Med. 2009;37(12):2355–2361. doi: 10.1177/0363546509339909. [DOI] [PubMed] [Google Scholar]
- 10.Capkin S, Zeybek G, Ergur I, Kosay C, Kiray A. An anatomic study of the lateral patellofemoral ligament. Acta Orthop Traumatol Turc. 2017;51(1):73–76. doi: 10.1016/j.aott.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeFroda SF, Shah KN, Lemme N, Koruprolu S, Ware KJ, Owens BD. Biomechanical properties of the lateral patellofemoral ligament: a cadaveric analysis. Orthopedics. 2018;41(6):e797–e801. doi: 10.3928/01477447-20180912-04. [DOI] [PubMed] [Google Scholar]
- 12.Merican AM, Amis AA. Anatomy of the lateral retinaculum of the knee. J Bone Joint Surg Br. 2008;90(4):527–534. doi: 10.1302/0301-620X.90B4.20085. [DOI] [PubMed] [Google Scholar]
- 13.Merican AM, Iranpour F, Amis AA. Iliotibial band tension reduces patellar lateral stability. J Orthop Res. 2009;27(3):335–339. doi: 10.1002/jor.20756. [DOI] [PubMed] [Google Scholar]
- 14.Merican AM, Kondo E, Amis AA. The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech. 2009;42(3):291–296. doi: 10.1016/j.jbiomech.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Shah KN, DeFroda SF, Ware JK, Koruprolu SC, Owens BD. Lateral patellofemoral ligament: an anatomic study. Orthop J Sports Med. 2017;5(12) doi: 10.1177/2325967117741439. 2325967117741439-2325967117741439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanaka MJ, Chahla J, Farr J, 2nd, et al. Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2537–2550. doi: 10.1007/s00167-018-5266-y. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan EB. Surgical approach to the lateral (peroneal) side of the knee joint. Surg Gynecol Obstet. 1957;104(3):346–356. [PubMed] [Google Scholar]
- 18.Richman NM, Scheller AD., Jr Medial subluxation of the patella without previous lateral retinacular release. Orthopedics. 1998;21(7):810–813. doi: 10.3928/0147-7447-19980701-12. [DOI] [PubMed] [Google Scholar]
- 19.Shannon BD, Keene JS. Results of arthroscopic medial retinacular release for treatment of medial subluxation of the patella. Am J Sports Med. 2007;35(7):1180–1187. doi: 10.1177/0363546507299445. [DOI] [PubMed] [Google Scholar]
- 20.Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007;35(3):484–492. doi: 10.1177/0363546507299237. [DOI] [PubMed] [Google Scholar]
- 21.Huber C, Zhang Q, Taylor WR, Amis AA, Smith C, Hosseini Nasab SH. Properties and function of the medial patellofemoral ligament: a systematic review. Am J Sports Med. 2020;48(3):754–766. doi: 10.1177/0363546519841304. [DOI] [PubMed] [Google Scholar]
- 22.Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 23.Smith TO, Walker J, Russell N. Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2007;15(11):1301–1314. doi: 10.1007/s00167-007-0390-0. [DOI] [PubMed] [Google Scholar]
- 24.Buckens CF, Saris DB. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med. 2010;38(1):181–188. doi: 10.1177/0363546509353132. [DOI] [PubMed] [Google Scholar]
- 25.Teitge RA, Torga Spak R. Lateral patellofemoral ligament reconstruction. Arthroscopy. 2004;20(9):998–1002. doi: 10.1016/j.arthro.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 26.Borbas P, Koch PP, Fucentese SF. Lateral patellofemoral ligament reconstruction using a free gracilis autograft. Orthopedics. 2014;37(7):e665–668. doi: 10.3928/01477447-20140626-66. [DOI] [PubMed] [Google Scholar]
- 27.Saper M. Lateral patellofemoral ligament reconstruction with a gracilis allograft. Arthrosc Tech. 2018;7(4):e405–e410. doi: 10.1016/j.eats.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38(2):293–297. doi: 10.1177/0363546509347602. [DOI] [PubMed] [Google Scholar]