Abstract
Background:
Increased health care spending concerns have generated interest in reducing operating room (OR) costs, but the cost awareness of the surgical team selecting intraoperative supplies remains unclear. This work characterizes knowledge of supply cost among surgeons and OR staff in a large academic hospital and seeks to examine the role of experience and training with regards to cost insight.
Methods:
This work is a cross-sectional study of surgeons, trainees, nurses, and surgical technicians (n = 372) across all surgical specialties at a large academic hospital. Participants completed a survey reporting frequency of use and estimated cost for 11 common surgical supplies as well as opinions on access to cost information in the OR. Cost estimation error was expressed as the ratio of estimated-to-actual cost, and groups were compared with one-way analysis of variance and chi-squared testing. Spearman correlation (ρ) was used to describe the relationship between monotonic variables.
Results:
Overestimation error was universal and ranged widely (3.80–49.79). There was no significant difference in estimation accuracy when stratified by role or years of experience. Less expensive items had higher rates of estimation error than more expensive items (P < 0.001), and a moderately strong relationship was found between decreased item cost and increased estimation error (ρ: 0.49). The overwhelming majority (91%) of respondents expressed a desire to learn more about supply pricing.
Conclusions:
Price knowledge of common supplies is globally impaired for entire surgical team but coexists with a strong desire to augment cost awareness. Improved access to cost information has a high potential to inform surgical decision-making and decrease OR waste.
Keywords: Cost awareness, Surgical cost, Cost containment, Intraoperative supply cost, Surgical supply cost
Introduction
In an effort to curtail rising health care costs in the United States, hospital administrators have increasingly turned a scrutinizing eye toward operating rooms (ORs) and the surgeons who work in them. The cost of major surgical procedures is both unregulated and widely variable among institutions,1 and ORs are a component of hospital infrastructure with not only high operating costs but also a high potential for wasted consumables.1 The cost of running an OR has been calculated as roughly $37 per minute or $2220 per hour.2 Surgical waste is also a major issue, with wasted supplies as making up 20% of the total supply cost in the ORs at a single teaching hospital3 and a known association between emergency procedures and a large number of wasted supplies.4
In light of these figures, a number of research efforts have sought to elucidate factors that contribute to OR waste. Differences in surgeon preferences for surgical supplies and implants have been shown to be responsible for a large portion of intraoperative cost variation within the same procedure.5–7 Education of surgeons regarding the cost of supplies has shown to be an effective means of significantly reducing the cost variation, with various studies citing a 10%−21% decrease in cost after the implementation of surgeon education initiatives.5–7
Despite an increasing body of evidence that increased surgeon education with respect to supply costs is an effective means of reducing OR expenditures, all available evidence in the literature is that surgeon awareness of supply costs is severely limited. One study noted that orthopedic surgeons could accurately estimate the cost of the devices they implanted only 21% of the time.8 Other efforts investigating cost awareness with respect to more common and lower cost supplies demonstrated a similarly high level of ignorance among surgeons of all levels of training, with only 14%−25% accuracy cited in these studies.9–11
Although some research attention has been turned toward surgeons and their ability to influence OR waste, OR staff frequently participate in both purchasing committees as well as making intraoperative decisions regarding supply selection. It has been demonstrated that infrastructure-related factors, that is hospital-level purchasing decisions and supply availability, can have a more significant effect on cost variability than individual surgeon practice patterns.12 This work characterizes the knowledge of supply costs among surgeons as well as OR staff in a large academic hospital and seeks to examine the role of experience and training with regard to cost awareness among members of the team.
Methods
This is a cross-sectional study using a survey tool to gather data from the surgeons, trainees, and OR staff members at the Johns Hopkins Hospital. The study and the survey items were reviewed and approved by the Institutional Review Board of the Johns Hopkins Hospital. The survey tool was administered by email to all OR nurses and surgical technicians as well as surgeons and surgical trainees (fellows and residents) in all surgical disciplines. The response was on a voluntary basis. The need for informed consent was waived by the Institutional Review Board.
The study population was purposely selected as a representative multidisciplinary cross-section of all persons who actively participate in the decision-making process of pulling, opening, and using surgical supplies in the OR; no persons were included who would not be regularly exposed to the survey items as part of the responsibilities associated with their job. We purposely included surgeons and staff in all surgical disciplines, including general, urology, orthopedics, neurosurgery, otolaryngology, plastics, obstetrics and gynecology, and cardiac and vascular surgery. The survey consisted of photos, descriptions, and manufacturer information for 11 general items frequently used in the ORs at our institution (Table 1). For each item, the respondent was asked to estimate the dollar amount of the item in US dollars to the nearest cent as a free-text item and then was asked a multiple-choice item inquiring the frequency with which they encountered this item (on a daily, weekly, monthly, or yearly basis or never). The actual cost of the items was defined as the negotiated cost of the item to the institution to acquire said item; because of the differences in Medicare and private insurance reimbursements, the billed cost to the patient of each item was variable and beyond the scope of this investigation. As part of the survey, respondents also were asked to select their role in the OR and then the number of years they had been in that role—trainees were all asked to select post-graduate year of training. Additional items asked whether or not the respondent had been involved in OR purchasing committees and their attitudes toward the role of supply cost toward OR decision-making and whether they felt their demographic would benefit from more training regarding the cost of OR supplies.
Table 1 –
Items included in survey, manufacturers, and reported costs.
| Item | Manufacturer | Cost |
|---|---|---|
| Dermabond advanced topical skin adhesive (0.7 mL) | Ethicon | $16.67 |
| Blue towel 16″ × 26” (1 pack of 4 towels) | Allcare | $1.22 |
| Large drape sheet 3/4, 60″ × 76” (1 drape) | Kimberly–Clark Corp | $2.40 |
| Gauze sponges 4″ × 4” (pack of 10) | Kendall/Covidien | $1.25 |
| 3–0 Vicryl SH 18″ control release (1 packet of “3–0 pops”) | Ethicon | $8.69 |
| Surgical glove Biogel PI (1 pair of gloves) | Molnlycke healthcare | $1.59 |
| Arm padding—egg crate board (1 unit) | Sunrise medical/BioClinic | $1.32 |
| Skin stapler (1 stapler) | Ethicon endo-surgery | $7.24 |
| 10 cc luer lock (1 syringe) | Becton Dickinson | $0.07 |
| Surgical gown XLG impervious (1 gown) | Care-tech laboratories | $2.58 |
| Perma-hand 2–0 silk tie (1 packet of 12 sutures) | Ethicon | $2.01 |
Data from the survey were analyzed using Stata Version 14.2 (StataCorp LLC, College Station, TX). Continuous variables were analyzed with one-way analysis of variance testing and categorical variables with chi-squared testing. Estimation error was expressed as the ratio of estimated to actual cost, transformed logarithmically where appropriate to facilitate graphic presentation. Spearman correlation (ρ) was calculated to assess the relationship between monotonic variables.
Results
Overall, a total of 777 surveys were administered, with 372 responses for a 47.9% overall response rate; these results are summarized in Table 2. The highest response rates were seen among registered nurses (RNs; 63.7%) and surgical trainees, with attending surgeons and surgical techs responding at lower rates (35.6 and 37%, respectively). Surgeons and RNs had the highest average level of experience (10.1 and 10.7 y, respectively), whereas residents had significantly less (1.8 y; P < 0.001).
Table 2 –
Response rates for survey by OR role.
| Role | Administered | Completed | Response rate (%) |
|---|---|---|---|
| Surgeon | 261 | 93 | 35.6 |
| Fellow | 43 | 26 | 60.5 |
| Resident | 221 | 114 | 51.6 |
| RN | 171 | 109 | 63.7 |
| Surgical tech | 81 | 30 | 37.0 |
| Total | 777 | 372 | 47.9 |
When examining estimated versus actual costs, there was a large amount of variation in the estimated costs for the various common items, with most respondents overestimating the cost of the survey items. Actual and maximum estimated costs are portrayed in Table 3; of note, the most expensive item, a skin adhesive costing <$20, was estimated by one respondent to cost $750. The range of overestimation by item is also portrayed in Table 3. The estimation error ranged from 3.80 to 49.79 times the actual cost; the lowest and highest rates of overestimation pertained to the highest and lowest cost items, respectively, is represented graphically in Figure 1 as box and whisker plots; the untransformed data are shown in panel A and after logarithmic transformation in panel B. The estimation error was significantly higher for low-cost items (P < 0.001). On comparison, the rate of overestimation was found to be moderately correlated with actual item cost (ρ: 0.49).
Table 3 –
Estimated to actual cost ratios and costs by item.
| Item | Estimated to actual cost ratio | Estimated to actual cost ratio, log | Actual cost ($) | Mean estimated cost ($) | Max estimated cost ($) |
|---|---|---|---|---|---|
| Dermabond | 3.80 | 0.87 | 16.67 | 63.30 | 750 |
| Towels | 17.85 | 2.49 | 1.22 | 21.78 | 200 |
| Drape | 18.02 | 2.40 | 2.40 | 43.25 | 250 |
| Sponges | 12.96 | 2.06 | 1.25 | 16.20 | 165 |
| Vicryl sutures | 4.20 | 0.90 | 8.69 | 36.53 | 400 |
| Gloves | 6.76 | 1.43 | 1.59 | 10.74 | 150 |
| Padding | 8.56 | 1.48 | 1.32 | 11.29 | 200 |
| Stapler | 5.93 | 1.36 | 7.24 | 42.94 | 400 |
| Syringe | 49.79 | 3.19 | 0.07 | 3.49 | 50 |
| Gown | 9.47 | 1.71 | 2.58 | 24.43 | 300 |
| Silk sutures | 9.17 | 1.44 | 2.01 | 18.43 | 350 |
Fig. 1 –
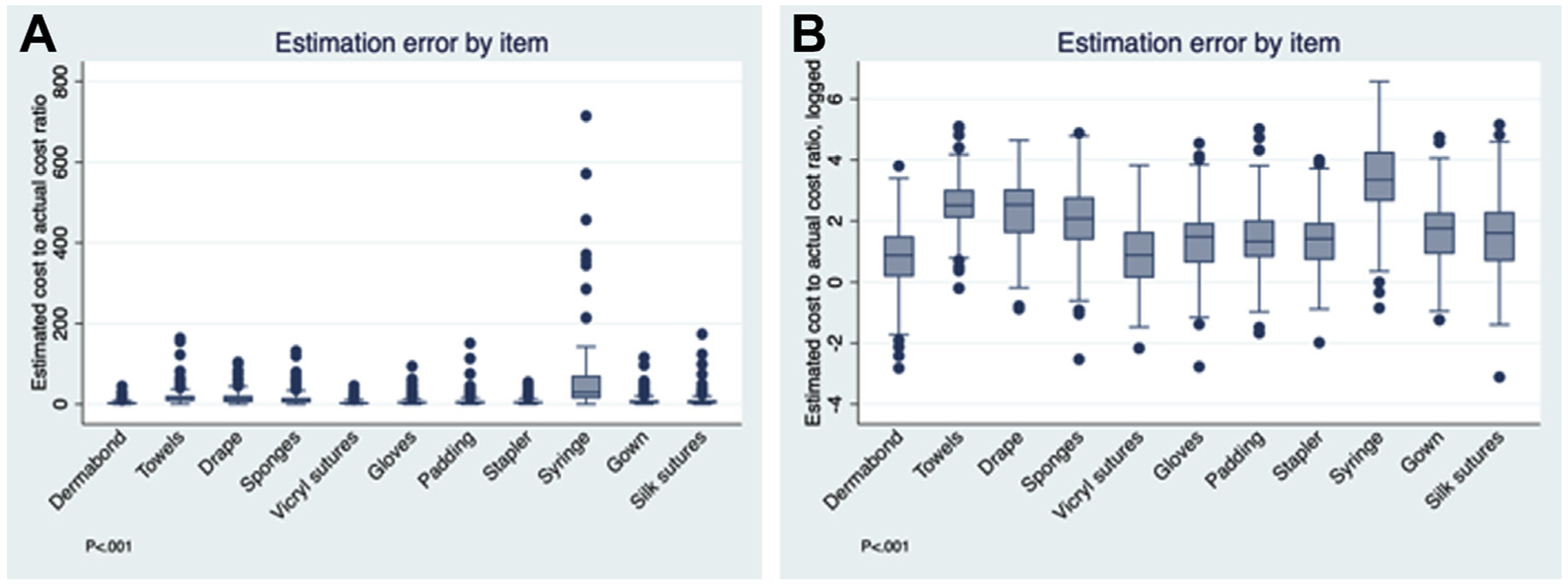
(A) Box and whisker plot of estimated cost to actual cost by item; (B) logarithmic transformation of estimated cost to actual cost by item.
Responses were further subdivided by item, role, and frequency of use. These results are portrayed in Figure 2 as bar graphs. There were no statistically significant differences in estimation error within items by frequency of use (panel A, P = 0.06) and no significant differences in estimation error when subdivided by role in the OR (panel B, P = 0.06) or years of work experience (panel C, P = 0.77).
Fig. 2 –
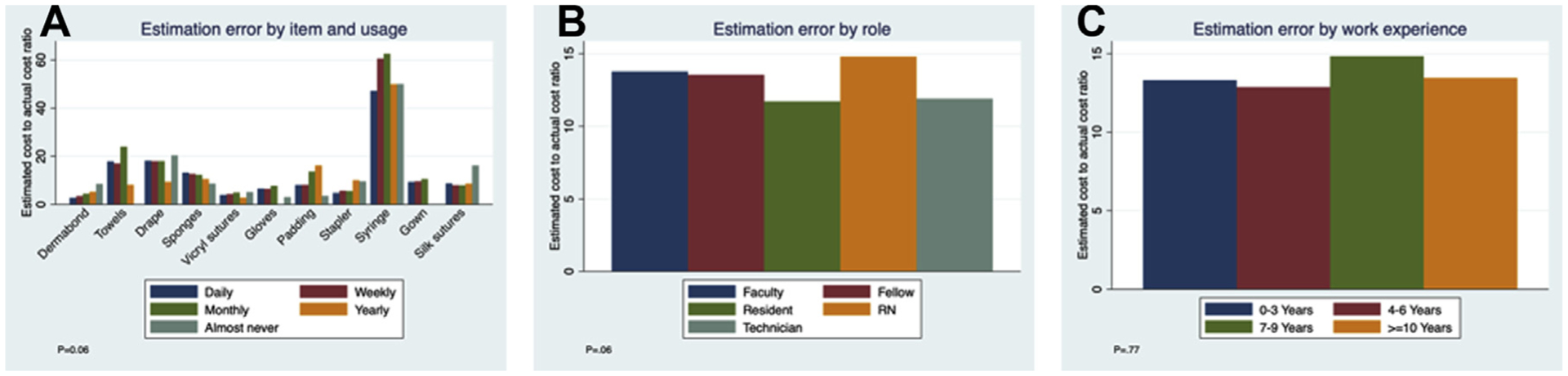
(A) Bar graph of estimated to actual cost ratio of item and frequency of use; (B) estimated to actual cost ratio by role; (C) by years of work experience.
Overall, there was an agreement with the statement, “Should personnel receive more training about supply prices?” with 335 positive responses (91%; Fig. 3). This was similarly reflected in the responses of agreement with the statement, “Price should factor into decision-making in the operating room,” with 346 positive responses (93%). There were no significant differences in the responses to the survey questions inquiring about the respondent’s desire for additional cost awareness training when broken down by years of experience (panel A, P = 0.75) or by surgical role (panel B, P = 0.31).
Fig. 3 –
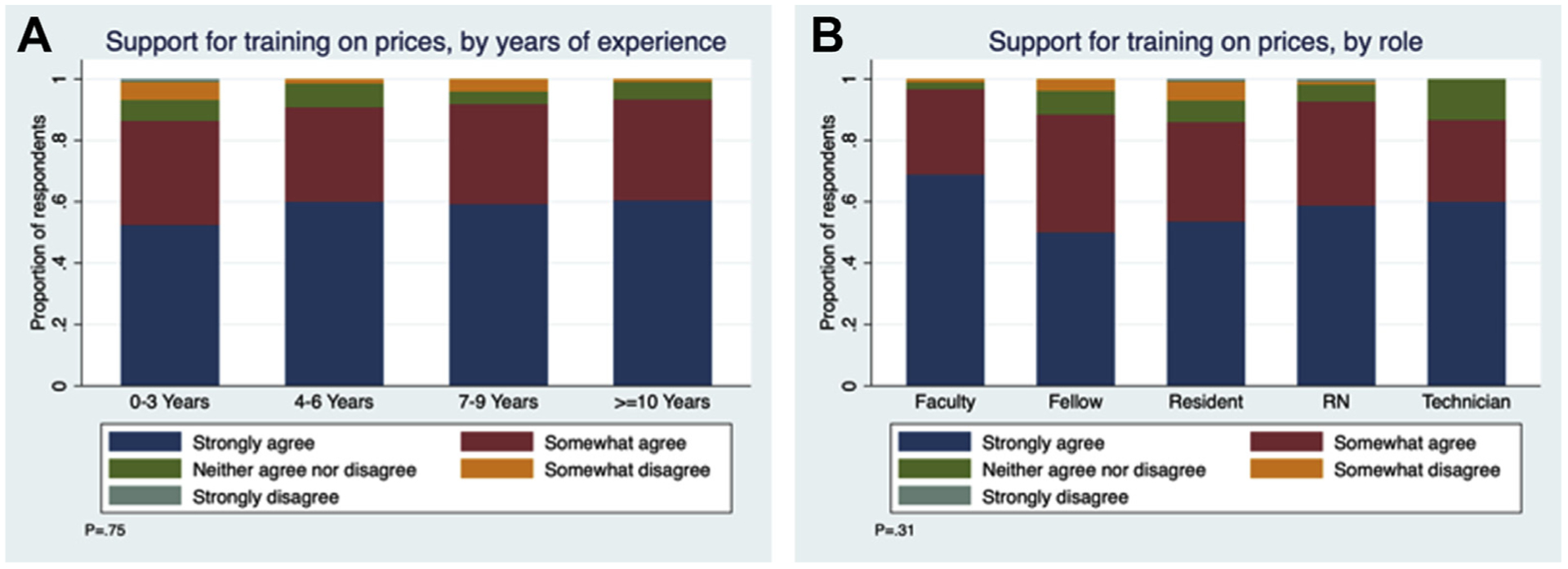
(A) Stacked bar graph of support for training on prices by years of experience; (B) by role.
Discussion
In general, the data presented here reaffirm the lack of knowledge by surgeons and surgical trainees with respect to supply costs and a high level of desire to augment that knowledge. Beyond that, we also demonstrate that this phenomenon extends to nursing and surgical technicians as well and is irrespective of years of experience in a surgical setting. Previous data have estimated that 75%−90% of surgeons cannot accurately estimate cost9,10,13; however, these outcomes are determined by a variable definition of what constitutes accuracy. Therefore, in the present work, we opted to report data in the form of logarithmically transformed estimation error, which ranged from 0.86 to 3.19, or an untransformed overestimation of 3.80–49.79 times the actual cost. This high level of error persisted regardless of the number of years the individual had worked in the OR, how frequently the individual used that item, and the individual’s role in the OR (surgeon, trainee, nurse, and surgical tech). Similarly, even for those individuals involved in purchasing committees, this activity did not seem to reduce estimation error for this set of common supplies.
Overall, this indicates that the health care system, in general, does a poor job of educating trainees and staff about cost, and that this has been the case for years. The pervasive ignorance of price that is repeatedly demonstrated among surgeons and OR staff is largely a product of the economic structure of modern health care.13 As employees of hospitals rather than independent proprietors, surgeons act as intermediaries in the delivery of health care. This role as neither true consumer nor true seller largely insulates surgeons and OR staff from changes in supply and implant price. Therefore, this group does not respond organically to changes in price in a way that would be predicted for sellers and consumers in a more straightforward economy.14–16 In a number of ways, this is by design: surgeons and their allies in providing health care should be shielded from cost in a way that allows them to make intraoperative decisions that are patient driven, not cost driven.15 That said, complete naiveté with respect to cost is problematic and can beget needless waste.
Clearly, the level of desire among surgeons and OR staff to receive this cost information is high, with 66%−90% of respondents to the present and other similar surveys, indicating that they want to know more about supply cost and use it to inform decision-making.9,10,13 The use of individualized surgeon scorecards and peer education from surgeons identified as having low procedural costs has resulted in a 10%−21% decrease in per procedure costs.5,7 Even more simply, one study focused on orthopedic trauma used a simple color designation to rate the cost of implants, which was posted on the wall in the OR. This simple, almost passive intervention served to increase affordable implant use by 56% (P < 0.0001), translating into a cost savings of $216,495 yearly.17 A similar effort announced the costs of consumables aloud to cardiologists performing percutaneous coronary interventions, saving an average of $234.77 per procedure (6%, P = 0.01) with no impact on outcomes.18 Posting or announcing such information within the operative suite has the dual strength of empowering all members of the team, including nurses and technicians, to engage in the decision-making process. All the above positive experiences highlight a repeating theme—that education alone can effectively reduce costs without the need for positive or negative incentives for achieved reductions.6
When discussing how to increase the overall value of OR procedures, often much of the discussion is focused on cost reduction; however, increasing quality also serves to increase the value of individual procedures. It is important to remember that overly spartan use of supplies can increase operative times, which can potentially affect outcomes.19–21 One study examining elective laparoscopic cholecystectomy at a single institution noted that the lowest cost surgeon with respect to consumable supplies had the longest operative times.22 Cost awareness should not simply be a means of discouraging the use of expensive items but also encouraging the use of low-cost items that may save valuable OR minutes and minimize the duration of anesthesia. Thus far, initiatives to reduce intraprocedural costs have not correlated with impaired outcomes,7,18,23,24 but it is important to keep the potential for harm in mind when aggressive cost reduction is attempted.
The items included in this survey are relatively low-cost items, with the most expensive item, a skin adhesive, costing <$20. This fact dictated the selection of the outcome of estimation error as a ratio rather than as an absolute cost difference. Absolute cost is a valuable endpoint and one that should be taken into consideration particularly with respect to higher cost items where even a small degree of estimation error on an expensive implant will carry considerable weight in the overall cost of the operation. With respect to low-cost items, it is the frequency of their use rather than their absolute cost, which makes cost estimation errors significant; thus, ratio of estimation error was selected to highlight the repercussions of cost ignorance at the low end of the cost spectrum. The relative widespread ignorance with respect to the costs of frequently used items almost certainly signifies a corresponding lack of knowledge with respect to more expensive items. Although there was a moderate relationship detected between decreased item cost and increased magnitude of estimation error (ρ: 0.49), this cannot and should not be extrapolated to assume that more expensive items will inherently be estimated with greater accuracy.
As a final point, intraoperative decisions that govern supply cost are merely one part of the potentially modifiable factors that contribute to the overall cost of a surgical hospital stay. At least one study examining the institutional factors that contribute to surgical supply cost states that the purchasing decisions made by the hospital have a far greater potential to impact procedural supply costs than do individual surgeons.12 The fact that purchasing committee involvement did not correlate with cost knowledge in this study raises questions about the associated benefit to staff knowledge gleaned by serving on such committees, but nonetheless, there is an ongoing need for clinical staff to be engaged in purchasing decisions on an institutional level. Finally, it must be noted that cost savings measures extend beyond the OR. At least one study of surgical cost education initiatives noted that even significant decreases in intraoperative costs did not impact the overall cost of admission.13 Turning cost-savings focus to areas outside the surgical suite, such as toward standardized postoperative pathways for particular procedures, may have a higher potential impact on significantly reducing health care expenditures.
The strengths of this work include its inclusion of multiple surgical disciplines at all levels of training as well as its inclusion of ancillary OR staff within the survey respondents, as prior investigations into OR cost awareness have focused solely on surgeons and surgical trainees, often within a single surgical specialty. Limitations include the survey-based nature of the study, which was returned on a voluntary basis, potentially introducing self-selection bias into the results. Similarly, the heterogeneity of the educational backgrounds and ages of the respondents may have inherently introduced bias into their responses. The general nature of this survey is both a strength and a weakness in that it incorporates the most frequently used items in our ORs; however, its general audience rendered us unable to include more expensive items germane to specific specialties (i.e., robotic components, staplers, orthopedic implants, vascular grafts, meshes, etc.) whose per-use impact on overall operating costs is much higher.
Conclusion
As a whole, these survey results demonstrate a lack of knowledge regarding the cost of common OR supplies, that is, pervasive among surgeons, surgical trainees, and OR staff members. In spite of that, there coexists a general desire among survey respondents to augment their knowledge and apply it to intraoperative decision-making. Providing surgeons with feedback regarding their own cost data in a way that maintains their ability to make patient-centered decisions regarding supply selection is paramount in reducing surgical waste and increasing procedural value. Similarly, initiatives to reduce surgical costs should extend beyond the OR, as standardized postoperative care pathways can have a greater impact on the overall cost of postoperative hospital stays.
Supplementary Material
Acknowledgment
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Footnotes
Disclosure
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jss.2020.02.007.
REFERENCES
- 1.Gani F, Makary MA, Pawlik TM. The price of surgery: markup of operative procedures in the United States. J Surg Res. 2017;208:192–197. [DOI] [PubMed] [Google Scholar]
- 2.Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153:e176233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chasseigne V, Leguilinel-Blache G, Nguyen TL, et al. Assessing the costs of disposable and reusable supplies wasted during surgeries. Int J Surg. 2018;53:18–23. [DOI] [PubMed] [Google Scholar]
- 4.Rigante L, Moudrous W, de Vries J, et al. Operating room waste: disposable supply utilization in neurointerventional procedures. Acta Neurochir (Wien). 2017;159:2337–2340. [DOI] [PubMed] [Google Scholar]
- 5.Zygourakis CC, Valencia V, Moriates C, et al. Association between surgeon scorecard use and operating room costs. JAMA Surg. 2017;152:284–291. [DOI] [PubMed] [Google Scholar]
- 6.Gitelis M, Vigneswaran Y, Ujiki MB, et al. “Educating surgeons on intraoperative disposable supply costs during laparoscopic cholecystectomy: a regional health system’s experience. Am J Surg. 2015;209:488–492. [DOI] [PubMed] [Google Scholar]
- 7.Vigneswaran Y, Linn JG, Gitellis M, et al. Educating surgeons may allow for reduced intraoperative costs for inguinal herniorrhapy. J Am Coll Surg. 2015;220:1107–1112. [DOI] [PubMed] [Google Scholar]
- 8.Okike K, O’Toole RV, Pollack AN, et al. Survey finds few orthopedic surgeons know the costs of the devices they implant. Health Aff (Millwood). 2014;33:103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryan JM, Rogers AC, Robb WB. A study evaluating cost awareness amongst surgeons in a health service under financial strain. Int J Surg. 2018;56:184–187. [DOI] [PubMed] [Google Scholar]
- 10.Jackson CR, Eavey RD, Francis DO. Surgeon awareness of operating room supply costs. Ann Otol Rhinol Laryngol. 2016;125:369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt B, Meng MV, Hampson LA. Operating room supply cost awareness: a cross-sectional analysis. Urol Pract. 2019;6:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Childers CP, Hofer IS, Cheng DS, et al. Evaluating surgeons on intraoperative disposable supply costs: details matter. J Gastrointest Surg. 2018;23:2054–2062. [DOI] [PubMed] [Google Scholar]
- 13.Al Zamil MA, Arafa MA. Awareness of surgeons in Saudi Arabia about the surgical costs and investigations: multicenter study. J Surg Educ. 2017;74:187–190. [DOI] [PubMed] [Google Scholar]
- 14.Glennie RA, Barry SP, Alant J, et al. Will cost transparency in the operating theatre cause surgeons to change their practice? J Clin Neurosci. 2019;60:1–6. [DOI] [PubMed] [Google Scholar]
- 15.Kernick DL. Introduction to health economics for the medical practitioner. Postgrad Med J. 2003;79:147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Green M The economics of healthcare.” prepared by industry supports education; 2007 London, UK: Ltd for the Office of Health Economics; 2007. Available at: https://www.ohe.org/sites/default/files/TheEconomicsofHeathCare2007.pdf. Accessed October 1, 2019. [Google Scholar]
- 17.Okike K, Pollak R, O’Toole RV, Pollak AN. Red-yellow-green: effect of an initiative to guide surgeon choice of orthopaedic implants. J Bone Joint Surg Am. 2017;99:e33. [DOI] [PubMed] [Google Scholar]
- 18.Asher E, Mansour J, Wheeler A, et al. Cost awareness decreases total percutaneous coronary intervention procedural cost: the SHOPPING (Show How Options in Price for Procedures Can Be Influenced Greatly) trial. Catheter Cardiovasc Interv. 2017;89:1207–1212. [DOI] [PubMed] [Google Scholar]
- 19.Daley BJ, Cecil W, Clarke PC, et al. How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee Surgical Quality Collaborative. J Am Coll Surg. 2015;220:550–558. [DOI] [PubMed] [Google Scholar]
- 20.Cheng H, Chen BP, Soleas IM, et al. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt). 2017;18:722–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Catanzarite T, Saha S, Pilecki MA, et al. Longer operative time during benign laparoscopic and robotic hysterectomy is associated with increased 30-day perioperative complications. J Minim Invasive Gynecol. 2015;22:1049–1058. [DOI] [PubMed] [Google Scholar]
- 22.Adkins HH, Hardacker TJ, Ceppa EP. Examining variation in cost based on surgeon choices for elective laparoscopic cholecystectomy. Surg Endosc. 2016;30:2679–2684. [DOI] [PubMed] [Google Scholar]
- 23.Brauer DG, Ohman KA, Jaques DP, et al. Surgeon variation in intraoperative supply cost for pancreaticoduodenectomy: is intraoperative supply cost associated with outcomes? J Am Coll Surg. 2018;226:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robinson JR, Carter NH, Gibson C, et al. Improving the value of care for appendectomy through an individual surgeon-specific approach. J Pediatr Surg. 2018;53:1181–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


