Abstract
Background The social distancing during COVID-19 is likely to cause a feeling of alienation, which may pose a threat to the public's mental health. Our research aims to examine the relationship between negative emotions and Post-Traumatic Stress Disorder (PTSD), considering the mediation effect of alienation and how it is moderated by anxiety and depression.
Methods For this, the current study conducted a cross-sectional survey on 7145 participants during the outbreak of COVID-19, via online questionnaires comprised of a self-designed Negative emotions questionnaire, Symptom Check List 90 (SCL-90), PTSD Checklist-civilian version (PCL-C), and Adolescent Students Alienation Scale (ASAS).
Results A total of 6666 pieces of data from the general population were included in the statistical analysis. The descriptive statistics showed a relatively mild level of mental disorders. Besides, results of Conditional Process Model analysis supported our hypotheses that negative emotions and alienation were both predictors for PTSD symptoms, and their direct and indirect effects were all moderated by the level of anxiety.
Limitations This study was limited by the generality and causality of the conclusion. The moderating effect of depression was left for further study due to the collinearity problem of variables.
Conclusions Social distancing may have an impact on individuals’ mental health by the feeling of alienation, which was moderated by affective disorders. Clinical psychologists should identify individuals’ particular cognition and mental disorders to provide a more accurate and adequate intervention for them.
Keywords: Covid-19, Negative emotions, Alienation, Post-traumatic stress disorders (PTSD), Anxiety, Depression
1. Introduction
Undoubtedly, the outbreak of COVID-19, first reported in Wuhan, Hubei, China (Huang et al., 2020), is an unexpected disaster. Owing to the highly infectious nature of the coronavirus, over nine million confirmed cases have been reported globally (World Health Organization, 2020). Notably, the results of quick surveys after the outbreak of COVID-19 have revealed that people are vulnerable to mental problems associated with the pandemic, such as negative emotions, anxiety and depression symptoms, and post-traumatic stress symptoms (Kang et al., 2020; Vindegaard and Eriksen Benros, 2020). Besides, almost every country around the world has implemented a social distancing policy to reduce the spread of the virus. However, this measure undermines our social activities and relationships. and thus its impact on people's psychological health cannot be ignored (Loades et al., 2020). Due to limited knowledge of the underlying mechanism of its impact, our study attempts to explore the mental problems related to this measure in COVID-19 and what the role it plays.
Negative emotions commonly appear among people in a crisis. When encountering desperate situations, individuals tend to lose the internal balance between the environment and themselves, being referred to as a process of emotional stress. Emotional stress encompasses the experience of negative emotions, including fear, anger, and hopelessness, which are likely to result from stressors that are beyond an individual's control, for example, a novel virus (Dohrenwend, 2000). Research has repeatedly demonstrated the link between emotional stress and the development of mental disorders (Folkman, 2013), among which post-traumatic stress disorder (PTSD) is a prominent one after a crisis. PTSD is defined as persistent disturbances and symptoms after experiencing or witnessing a life-threatening event like a pandemic. The typical symptoms include hyperarousal, re-experiencing of events, and avoiding (American Psychiatric Association, 2013; Xu et al., 2011). Empirical research has found negative emotions to be significantly related to the severity of PTSD symptoms (Dutheil et al., 2020; McLean and Foa, 2017). Theoretically, the cognitive model of PTSD has proposed individuals’ appraisal of trauma leads to negative emotions which further contribute to persistent symptoms of PTSD (Gómez de La Cuesta et al., 2019). For example, negative emotions may mislead one to appraisal the event in an emotional way and reinforce the emotional memory of trauma (Deprince et al., 2010; Ehlers and Clarks, 2000).
To explore the underlying mechanisms of emotionally traumatic-related consequences, the feeling of alienation also worth more attention in a social distancing situation. As John T. Cacioppo, the past president of the Association for Psychological Science (APS) argued, “By nature, we are social creatures”, when individuals are forced to self-isolate, a feeling of alienation is consequently aroused (Cacioppo and Patrick, 2008). Alienation is defined as a loss of connection with oneself and others and theincidental negative feelings, typically exhibited as the feelings of loneliness, uncontrollability, hopelessness, and so forth(DePrince et al., 2011, Dong et al., 2002). It is found that alienation is significantly associated with physical and psychological symptoms, as well as problematic behaviors (i.e. alcohol use and delinquency) among adolescents (Rayce et al., 2009; Walsh et al., 2019). And a meta-analysis on the alienation's correlates indicated that alienation influences one's attitudes and health symptoms (Chiaburu et al., 2014).
In addition, it is revealed that alienation is highly predictive of poor mental health and diverse trauma-related distress (Sprang and Silman, 2013), and alienation appraisal is the most inlfuential predictor of trauma-related distress among the most common categories of appraisals (Mitchell et al., 2020). Furthermore, prior studies have identified alienation appraisal as a critical predictor of the severity of PTSD in children as well as females (Hebenstreit et al., 2015; Srinivas et al., 2015). A meta-analysis also found a large effect size of alienation appraisal on PTSD symptoms in adults (McIlveen et al., 2020), providing another empirical evidence for the relationship between these two variables. Individuals with a high level of alienation from others are more likely to lose the opportunity to reappraisal the trauma experience, impeding the effectiveness of exposure therapy for PTSD. This phenomenon may be a consequence of the lack of the beneficial effects of social support, in that they negatively interpret others’ words or behaviors (Baumeister and Leary, 1995; Cohen, 2004; Ehlers et al., 1998). As such, we consider alienation as a key factor that mediates the relation between negative emotion and PTSD.
While negative emotions and alienation has been identified to be positively associated with PTSD symptoms, moderating factors of this association remain unclear. Depression and anxiety, which have been diagnosed repeatedly, are prevalent disorders among the public (Kessler et al., 2005; Steel et al., 2014) and frequently coexist with PTSD in patients (Brady et al., 2000; Holman et al., 2000; Möller et al., 2016). Armour et al. (2014) found that higher levels of anxiety and depression were observed among patients with PTSD, and it is inferred that depression and anxiety could increase the risk of developing PTSD (Brady et al., 2000). Without sufficient evidence to confirm the inference, a more in-depth examination is warranted.
Individuals with depression or anxiety may have cognitive biases compared to mentally healthy people. For example, feeling uncertain about loss tends to be associated with anxiety, while being sure of loss is linked to depression (Ehlers and Clark, 2000), which potentially influence the effect of negative emotions and alienation. Specifically, people with a high level of depression have been quite likely to suffer from negative emotions, feelings of loneliness, worthlessness, and hopelessness (American Psychiatric Association, 2013; Deprince et al., 2010; Rosenström and Jokela, 2017), which may aggravate the feeling of alienation. Depression is also characterized by social avoidance, rumination, and these outcomes will further make one indulge in negative thinking and undermine social support, enhancing the maintenance of PTSD (Ebert and Dyck, 2004; Fernández-Theoduloz et al., 2019; Berman et al., 2011; Spinhoven et al., 2015; Pugach et al., 2020). Moreover, neuropsychological research leaves controversy over whether depression would make individuals play down the cues of social exclusion to alleviate their grief (Hooley et al., 2009), or more vulnerable (Jobst et al., 2015). It is plausible to posit a similar controversy about the effect of alienation since it often appears after social exclusion (Ren et al., 2018).
As for those anxious individuals, they incline to expect some possible outcomes as negative and endlessly worry about the uncertain future (Craske et al., 2009; Gu et al., 2010). Therefore, in the COVID-19 context, current negative emotion and alienation can pose a more severe and long-lasting impact on them because of people's irrationally worry. On the contrary, the fever model of self-disclosure proposed that individuals with a higher level of anxiety tend to disclose more, which is helpful to release psychological distress (Stiles et al., 1992). So, probably, anxious people could alleviate the burden of negative emotion and feeling of alienation via more self-disclosure. Taken together, the exact moderating effects of depression and anxiety are not yet determined.
In summary, one may deduce that there is an inferior understanding of the impact of negative emotions on PTSD interfering with alienation. Moreover, how affective disorders, namely, anxiety and depression, alter this process is also unclear. Consequently, it is imperative to understand the possible relationships between negative emotions and potential mental illnesses among the general public in the context of the COVID-19 pandemic to advance scientific knowledge and effective psychological assistance.
We hypothesized that while negative emotions predicted more severe PTSD symptoms, alienation played a mediating role in this process. Moreover, anxiety and depression disorders were hypothesized to moderate the direct and indirect effects of negative emotions and alienation on PTSD.
2. Materials and methods
2.1. Participants
Stratified random sampling was employed to select 7145 participants from among the residents of Wanzhou District in Chongqing city, where, in comparison to the other areas in Chongqing, most of the infectious cases had been reported. However, 479 participants’ data were omitted, because they had taken less than five minutes to complete all the questions. Finally, 6666 pieces of data were used in the statistical analysis. The participants comprised 4718 males (70.8%) and 1948 females (29.2%), most between 35- and 50, years of age, and 96.3% have completed high school or higher education. This study was conducted in accordance with the Declaration of Helsinki and the protocol was approved by the review board of the Faculty of Psychology of Southwest University (H20032). Participation in the study was entirely voluntary, with explicit permission of the participants obtained through online consent for the confidential use and processing of data.
2.2. Instruments
2.2.1. Negative emotions questionnaire
The negative emotions questionnaire is a self-reported 7-point Likert scale designed to investigate people's emotional state. In accordance with published reports, six words that describe individuals’ most prevalent emotions were selected: anxious, depressive, sad, helpless, angry, and fearful. The participants were required to rate the extent to which they experienced each of these emotions. The scores of the six items were summed. Higher total scores were indicative of a poor emotional state. Cronbach's α for this questionnaire in the current study was 0.92.
2.2.2. Symptom checklist 90 (SCL-90)
SCL-90 was designed to assess psychological symptoms to evaluate the outcomes of mental health interventions as well as for research purposes. The symptoms are assessed about the previous seven days and are classified into nine dimensions, including anxiety and depression, with scores indicating the severity of symptoms. Cronbach's α values between 0.77 and 0.90 for its dimensions indicated adequate internal reliability (Folkman, 2013). The participants completed two subscales of SCL-90 to measure the level and prevalence rates of anxiety (10 items) and depression (13 items). Cronbach's α values for anxiety and depression were 0.91 and 0.93, respectively.
2.2.3. PTSD checklist-civilian version (PCL-C)
PCL-C is a 17-item self-report rating-scale instrument corresponding to the diagnostic criteria for PTSD of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-4), which is designed for civilian-populations use. Higher scores indicate higher PTSD levels, with scores of 30–35 considered probable PTSD among non-clinical populations (National Center for PTSD, 2019; Walker et al., 2002). The PCL-C questions used in our study was modified to be related to the COVID-19 (e.g. “Repeated, disturbing memories, thoughts, or images of the COVID-19?” This scale demonstrated good internal and test-retest reliability in a Chinese sample (Jin et al., 2014). In the current study, Cronbach's α was 0.92.
2.2.4. Adolescent students alienation scale (ASAS)
This scale was originally developed in the Chinese version to examine the feeling of alienation in Chinese people, especially adolescents (Yang, Zhang and Huang, 2002). It comprises 52 items in four dimensions that are rated on a 5-point Likert- scale, ranging from 1 (totally disagree) to 7 (totally agree). The ASAS possesses good validity and reliability as confirmed by studies in China. In the current study, this scale was modified to fit the conditions of adults during COVID-19. Moreover, Cronbach's α was 0.96.
2.3. Procedures
All the data were collected anonymously between February 25 and March 03, 2020, one of the worst periods of the outbreak, via an online survey research platform powered by www.wjx.cn. First, the participants were required to fill in demographic information. Subsequently, they completed the survey in the following order: negative emotions questionnaire; SCL-90 Anxiety and Depression; PCL-C; and ASAS. Data analyses were performed by employing SPSS with PROCESS macro (Hayes and Rockwood, 2020), as there is a significant advantage of PROCESS is that two or more mediators in the moderated- mediation model can be tested simultaneously. We examined the common method bias by using Harman's one-factor test (Podsakoff et al., 2003). No significant common method bias in our dataset was found.
3. Results
3.1. Descriptive statistics, mean differences, and correlations for all variables
The descriptive statistics of key variables are represented in Table 1 . The demographic variables were tested using t-tests and one-way ANOVAs to assess the differences in means between groups. Significant gender and age differences were found only in the negative emotions (tGender = −3.127, p = .002; FAge = 3.317, p = .036) and PTSD scores (tGender = −2.569, p = .010; FAge = 9.556, p < .001). However, the negative emotions, PTSD, anxiety, and depression scores were all significantly different at the various levels of education (FNegEmo = 11.080, p < .001; FPTSD = 5.866, p = .001; FAnx = 14.581, p < .001; FDep = 16.148, p < .001). Given the significant differences, these variables were controlled for subsequent mediation and moderation analysis models.
Table 1.
Descriptive statistics and bivariate correlations.
| M | SD | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|---|
| Negative Emotions | 10.59 | 6.72 | 1.00 | ||||
| Anxiety | 1.31 | 0.47 | 0.71⁎⁎ | 1.00 | |||
| Depression | 1.27 | 0.46 | 0.63⁎⁎ | 0.81⁎⁎ | 1.00 | ||
| PTSD | 22.24 | 7.35 | 0.62⁎⁎ | 0.80⁎⁎ | 0.83⁎⁎ | 1.00 | |
| Alienation | 2.51 | 1.02 | 0.55⁎⁎ | 0.57⁎⁎ | 0.67⁎⁎ | 0.68⁎⁎ | 1.00 |
†Two-tailed test, *p < .05; **p < .01; ***p < .001.
The results of Pearson's correlations are also displayed in Table 1. As expected, all the included variables were positively and significantly correlated with one another.
3.2. Collinearity test
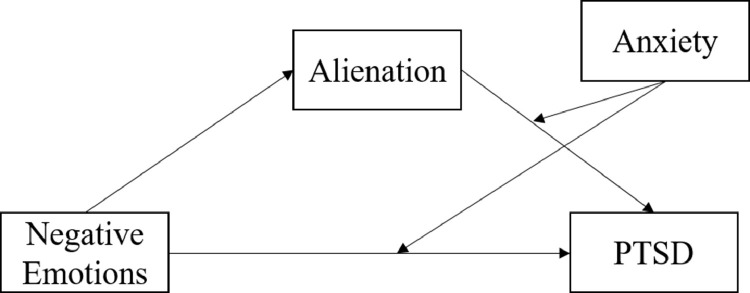
Due to the high correlation between the variables of interest, we conducted a collinearity test. According to the strict criteria, the results showed that there is a risk of collinearity problem, most serious in the variables related to depression. We then used Lasso regression to estimate the model (McNeish, 2015). The results strongly suggested that the interaction terms of negative emotions with depression and the interaction terms of alienation with depression should be excluded from the model, but depression itself was a quite predictive variable (see. Supplementary material). Considering the high correlation of depression with other variables and its significant effect on PTSD, we set it as a control variable in further analyses (Allison, 2010). The new theoretical hypothesis model is depicted in Fig. 1 .
Fig. 1.
Hypothesis Model.
3.3. Mediation analyses
Mediation analyses were performed with gender, age, education, and depression as the control variables. The results are presented in Table 2 . First, negative emotions predicted the severity of PTSD symptoms significantly (Model 1 in Table 2). When the mediating predictor, alienation, was added, the direct effect of negative emotions on PTSD remained significant (Model 3 in Table 2). About the indirect effect, negative emotions significantly predicted alienation, and subsequently, alienation significantly predicted PTSD (Models 2 and 3 in Table 2). Furthermore, the Bootstrapping indicated that alienation significantly mediated the effect of negative emotions on PTSD (ab = 0.038, SE = 0.004, Boot 95% CI = [0.032, 0.047]), and the indirect effect via alienation accounted for 24.36% of the total effect.
Table 2.
Model characteristics for the mediation analysis.
| Model 1 (PTSD) | Model 2 (Alienation) | Model 3 (PTSD) | ||||
|---|---|---|---|---|---|---|
| Predictor | B | t | B | t | B | t |
| Gender | 0.008 | 2.21* | −0.007 | −0.711 | 0.009 | 1.383 |
| Age | 0.063 | 7.84* | −0.021 | −2.193* | 0.067 | 9.848*** |
| Education | −0.009 | 1.96 | −0.049 | −5.207*** | 0.000 | 0.021*** |
| Depression (C) | 0.736 | 87.679 | 0.544 | 47.885*** | 0.635 | 67.427 |
| Negative Emotions (X) | 0.159 | 19.000*** | 0.210 | 18.496*** | 0.121 | 14.476*** |
| Alienation (M) | 0.185 | 21.093*** | ||||
| R² | 0.716 | 0.479 | 0.733 | |||
| F | 3349.397*** | 1125.89*** | 3051.361*** | |||
†X = independent variable; C = controlling variable; M = mediating variable. X, C, M, Y were all standardized.
‡Two-tailed test, *p < .05; **p < .01; ***p < .001.
3.4. Moderated mediation analyses
Thereafter, we performed moderated mediation analyses by controlling the demographic variables and depression noted previously. The results demonstrated that the effect of negative emotions on PTSD was significantly moderated by anxiety (X*Z: B = −0.038, p < .0001). Particularly, the mediation of alienation was significantly moderated by anxiety (M*Z: B = 0.085, p < .0001) (Table 3 ).
Table 3.
Model characteristics for the conditional process analysis.
| Alienation (M) | PTSD (Y) | |||
|---|---|---|---|---|
| Predictor | B | t | B | t |
| Gender | −0.006 | −0.711 | −0.001 | −0.112 |
| Age | −0.021 | −2.193 | 0.053 | 8.340*** |
| Education | −0.049 | −5.207*** | −0.003 | −0.418 |
| Depression (C) | 0.544 | 47.885*** | 0.369 | 30.684** |
| Negative Emotions (X) | 0.210 | 18.496*** | 0.026 | 2.906*** |
| Alienation (M) | 0.197 | 23.743*** | ||
| Anxiety (Z) | 0.335 | 27.751*** | ||
| Negative Emotions × Anxiety (X × Z) | −0.038 | −8.079*** | ||
| Alienation × Anxiety (M × Z) | 0.085 | 13.568*** | ||
| R² | 0.479 | 0.772 | ||
| F | 1225.890*** | 2498.655*** | ||
†X = independent variable; C = controlling variable; M = mediating variable; Z = moderating variable; Y = dependent variable. X, C, M, Z, Y were all standardized.
‡Two-tailed test, *p < .05; **p < .01; ***p < .001.
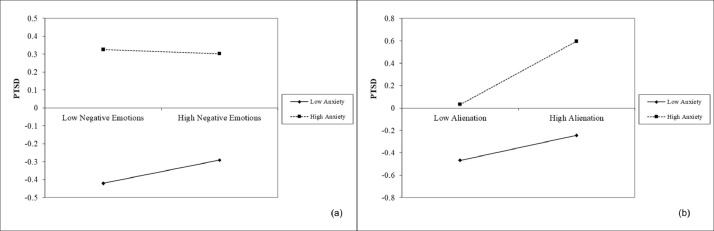
Furthermore, the simple slope plot corresponding to the conditional indirect effect analysis revealed the interactions in a more specific way (Fig. 2 ). Higher levels of anxiety predicted more severe PTSD symptoms. However, while anxiety enhanced the effect of alienation, it weakened the effect of negative emotions. (Table 4 ).
Fig. 2.
Moderating effects: (a) negative emotions (X) × anxiety (Z); (b) alienation (X) × anxiety (Z). X: independent variable; W: moderating variable. X, M, Z, Y were all standardized.
Table 4.
Bootstrapped conditional direct and indirect effects.
| Conditional direct effects | |||||||
|---|---|---|---|---|---|---|---|
| Predictor | Moderator | 95% CI | |||||
| Direct effect | Negative emotions | Effect | SE | LL | UL | ||
| Low | 0.0519 | 0.0105 | 0.0313 | 0.0725 | |||
| High | −0.012 | 0.0088 | −0.0293 | 0.0054 | |||
| Indirect effect | Alienation | ||||||
| Low | 0.0296 | 0.0036 | 0.0232 | 0.0371 | |||
| High | 0.0593 | 0.0066 | 0.0469 | 0.0726 | |||
†X = independent variable; M = mediating variable; Z = moderating variable; Y = dependent variable. X, M, Z, Y were all standardized.
‡The values of moderator: Low: anxiety = −0.664; High: anxiety = 1. (−0.664 is the minimum of anxiety, PROCESS cannot output the effect when anxiety = −1).
§Two-tailed test, *p < .05; **p < .01; ***p < .001.
4. Discussion
Given the current global concern regarding the COVID-19 pandemic, it is exigent to research the prevalence and risk factors of potential mental health problems to address the intervention and governance thereof under emergent conditions. While our study was conducted during a severe period of the COVID-19 spread, it is a little relief that most people did not exhibit severe symptoms of mental disorders. And there are some differences in demographic variables, concurred with other studies on trauma-related mental crises (Liu et al., 2020; Tang et al., 2020; Tian et al., 2020).
The current study revealed a significant mediation of alienation in the development of PTSD symptoms in adults, which concurred with results identified in adolescents (Srinivas et al., 2015). This relation is reasonable in the light of the connotation of alienation and the characteristics of PTSD. It has been alleged that the construction of alienation contains aspects including a sense of meaninglessness, powerlessness, social isolation, and self-alienation (Seeman, 1959), which are all closely related to symptoms associated with PTSD, such as estrangement from others and social withdrawal (Ehlers et al., 1998). In addition, the sense of alienation usually originates from the objective absence of social support, the buffering effect of distress (Woodward et al., 2015), which could erode the psychological resistance of an individual faced with such a crisis. It is also shown that higher levels of anxiety exacerbate the mediating effect of alienation. For individuals with high levels of anxiety, from a physiological and cognitive perspective, their hyperarousal symptoms may be interpreted as an explicitly negative signal that there is something wrong (Mineka and Zinbarg, 2006; Maloney et al., 2014), and they are prone to hold pessimistic expectations about uncertain events (Grupe and Nitschke, 2013). Therefore, they could view the feeling of alienation as more disastrous.
Besides the insight into alienation, a significant effect of negative emotions on PTSD was found in our study. Emotions permit individuals to construct a memory of certain events with value, named emotional memory. Such a form of memory is more vivid and could be more easily retrieved, which however increases the risk of PTSD, especially the flashback symptoms (Dolan, 2002). Accordingly, negative emotions can be regarded as a “prodrome” (a prior manifestation before the onset of disorders) of PTSD (Jacobson and Newman, 2017; Pérez-Edgar and Guyer, 2014). If we could alleviate people's negative emotions in the early stages of a crisis, then there is a chance to prevent them from more severe mental disorders. As for the moderated direct effect of negative emotions, it was weakened to non-significant at a high level of anxiety. One possible explanation is that there exist other factors more readily inducing PTSD than negative emotions, such as alienation based on our result. Another is that anxiety itself has a strong effect on PTSD, which covers the minor effect of negative emotion. These may imply that the original negative emotions are not serious enough to directly cause symptoms of PTSD but through further appraisal or some affective disorders.
With regard to the perspective of practice, firstly, the findings of the present study suggest that it is imperative to assess the feelings of alienation when conducting an intervention with a post-trauma client. Secondly, psychotherapists could adopt an alternative approach to protect individuals from traumatic experiences: reducing their sense of alienation by restructuring their cognition. Besides, it is significant to screen for mental symptoms in the public for the management of mental health during a pandemic. Once mild or moderate manifestations of affective disorders are detected, timely psychological counseling or mental health first aid is necessary to decrease the risk of PTSD. Moreover, attention should be particularly paid to those individuals’ later mental condition, because they are at higher risk of PTSD. The implementation of this notion could be advanced through the use of digital technology, which may be beneficial in maintaining interpersonal and social connections as well as providing information, training, supervision, and support online (Kola, 2020). Exploration of more specific ways of applications is recommended.
The contributions of the current research cannot be considered without reflecting on its several limitations. First, the generalizability of these results may be limited in that the sample comprised non-clinical individuals residing in Wanzhou, Chongqing. Thus, the entire public or groups in which PTSD symptoms are more prevalent were not represented. Thus, future research needs to examine other communities to exclude the potential influence of compound factors. Second, usually mental disorders gradually develop from mild psychological distress, whereas this cross-sectional study could not measure the alterations in alienation and PTSD symptoms over time. Consequently, a causation relationship between variables cannot be determined. Besides, it not sure whether the symptoms are merely induced by the social distancing in COVID-19 or by other events, thus limiting the theoretical and directional conclusions that can be drawn from the research. Third, because the participants were in quarantine, self-report scales were employed to collect the data. Consequently, a single source bias, which is the deviation caused by the common method variance, may have occurred. Even though the test of the common method bias is acceptable, it may still undermine the power of the results. Additionally, albeit the high correlation between variables, particularly depression, anxiety, and PTSD, can be attributed to their high rate of comorbidity and theoretical overlap, it caused a problem of collinearity. Because of this problem, unfortunately, we failed to examine the moderating effect of depression. However, it is not yet sure whether these characteristics of depression can reduce individuals’ sensitivity to newly developed negative emotions and alienation or exaggerate their effects. Examination of this question is intriguing and requires further research using measurements that better distinguish variables. Finally, other influential factors of people's mental health leave to be uncovered by future studies, which will benefit therapeutic practice.
5. Conclusion
Confronted with the global spread of COVID-19, it is essential to attend to the mental health of individuals. Social distancing is likely to result in more feelings of alienation (Pancani et al., 2020), which may play a role in the development of mental problems in the public. To offer an enhanced explanation of the situation and explore feasible treatments, this study examined the relationship between negative emotions and PTSD, wherein the mediation effect of alienation, as well as the moderation effects of anxiety, were particularly considered. The results of statistical analyses indicated that: First, negative emotions and alienation are both predictors for PTSD symptoms; second, their direct and indirect effects are moderated by levels of anxiety. The findings of this study are beneficial for both academic and practical purposes, considering the limitation of such rapid empirical research. Based on our confirmed theoretical model, suggestions for the implementation of health care are proposed, which helps to improve our practice in the future.
6. Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
7. Funding sources
This work was supported by Fundamental Research Funds for the Central Universities (Dong Yang, grant number SWU2009101), Chongqing Planed Social Science Research Program (Dong Yang, grant number 2020TBWT-ZD07), and Chongqing Research and Innovation Fund for Postgraduates (Yue Zhu, grant number CYS20093).
CRediT authorship contribution statement
Yue Zhu: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Visualization, Funding acquisition. Lihua Zhang: Investigation. Xia Zhou: Investigation. Chenxiang Li: Investigation. Dong Yang: Conceptualization, Methodology, Investigation, Resources, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
All other authors declare that they have no conflicts of interest.
Acknowledgments
We are grateful to Sheng Hu for his support all the time. We also give thanks to Yuan Liu who provided suggestions on the statistical analysis method, the reviewer whose comments helped to improve our study, Lijie Zhang and Shuge Yuan who gave advices on revision, and all of our team members.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.12.004.
Appendix. Supplementary materials
References
- Allison P. When can you safely ignore multicollinearity? Stat. Horiz. 2010 http://www.statisticalhorizons.com/multicollinearity [Google Scholar]
- American Psychiatric Association . American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Armour C., Elklit A., Lauterbach D., Elhai J.D. The DSM-5 dissociative-PTSD subtype: can levels of depression, anxiety, hostility, and sleeping difficulties differentiate between dissociative-PTSD and PTSD in rape and sexual assault victims? J. Anxiety Disord. 2014;28:418–426. doi: 10.1016/j.janxdis.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Baumeister R.F., Leary M.R. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995;117:497–529. doi: 10.1037/0033-2909.117.3.497. [DOI] [PubMed] [Google Scholar]
- Berman M.G., Peltier S., Nee D.E., Kross E., Deldin P.J., Jonides J. Depression, rumination and the default network. Soc. Cogn. Affect. Neurosci. 2011;6:548–555. doi: 10.1093/scan/nsq080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady K.T., Killeen T.K., Brewerton T., Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J. Clin. Psychiatry. 2000;61(Suppl 7):22–32. [PubMed] [Google Scholar]
- Cacioppo John T., Patrick William. Loneliness: Human Nature and The Need for Social Connection. W. W. Norton & Company; New York: 2008. [Google Scholar]
- Chiaburu Dan S., Thundiyil Tomas, Jiexin Wang. Alienation and its correlates: A meta-analysis. Eur. Manag. J. 2014;32(1):24–36. doi: 10.1016/j.emj.2013.06.003. [DOI] [Google Scholar]
- Cohen S. Social relationships and health. Am. Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Craske M.G., Rauch S.L., Ursano R., Prenoveau J., Pine D.S., Zinbarg R.E. What is an anxiety disorder? Depress. Anxiety. 2009 doi: 10.1002/da.20633. [DOI] [PubMed] [Google Scholar]
- DePrince A.P., Chu A.T., Pineda A.S. Links between specific posttrauma appraisals and three forms of trauma-related distress. Psychol. Trauma Theory, Res. Pract. Policy. 2011;3:430–441. doi: 10.1037/a0021576. [DOI] [Google Scholar]
- Deprince A.P., Zurbriggen E.L., Chu A.T., Smart L. Development of the trauma appraisal questionnaire. J. Aggress. Maltreat. Trauma. 2010;19:275–299. doi: 10.1080/10926771003705072. [DOI] [Google Scholar]
- Dohrenwend B.P. The role of adversity and stress in psychopathology: some evidence and its implications for theory and research. J. Health Soc. Behav. 2000;41:1–19. doi: 10.2307/2676357. [DOI] [PubMed] [Google Scholar]
- Dolan R.J. Neuroscience and psychology: emotion, cognition, and behavior. Science. 2002;5596(298):1191–1194. doi: 10.1126/science.1076358. [DOI] [PubMed] [Google Scholar]
- Dong Y., Jinfu Z., Xiting H. Adolescent students’ sense of alienation: theoretical construct and scale development. Acta Psychol. Sin. 2002;34:407–413. [Google Scholar]
- Dutheil F., Mondillon L., Navel V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol. Med. 2020;33(0):1–2. doi: 10.1017/S0033291720001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert A., Dyck M.J. The experience of mental death: the core feature of complex posttraumatic stress disorder. Clin. Psychol. Rev. 2004;24:617–635. doi: 10.1016/j.cpr.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Clark D.M. A cognitive model of posttraumatic stress disorder. Behav. Res. Ther. 2000;38:319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Clark D.M., Dunmore E., Jaycox L., Meadows E., Foa E.B. Predicting response to exposure treatment in PTSD: the role of mental defeat and alienation. J. Trauma. Stress. 1998;11:457–471. doi: 10.1023/A:1024448511504. [DOI] [PubMed] [Google Scholar]
- Fernández-Theoduloz G., Paz V., Nicolaisen-Sobesky E., Pérez A., Buunk A.P., Cabana Á., Gradin V.B. Social avoidance in depression: a study using a social decision-making task. J. Abnorm. Psychol. 2019 doi: 10.1037/abn0000415. [DOI] [PubMed] [Google Scholar]
- Folkman S. Springer; New York, New York, NY: 2013. Stress: Appraisal and Coping, in: Encyclopedia of Behavioral Medicine; pp. 1913–1915. [DOI] [Google Scholar]
- Gómez de La Cuesta G., Schweizer S., Diehle J., Young J., Meiser-Stedman R. The relationship between maladaptive appraisals and posttraumatic stress disorder: a meta-analysis. Eur. J. Psychotraumatol. 2019;10 doi: 10.1080/20008198.2019.1620084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grupe D.W., Nitschke J.B. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat. Rev. Neurosci. 2013;14:488–501. doi: 10.1038/nrn3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu R., Ge Y., Jiang Y., Luo Y.J. Anxiety and outcome evaluation: the good, the bad and the ambiguous. Biol. Psychol. 2010;85:200–206. doi: 10.1016/j.biopsycho.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F., Rockwood N.J. Conditional process analysis: concepts, computation, and advances in the modeling of the contingencies of mechanisms. Am. Behav. Sci. 2020;64:19–54. doi: 10.1177/0002764219859633. [DOI] [Google Scholar]
- Hebenstreit C.L., Maguen S., Koo K.H., DePrince A.P. Latent profiles of PTSD symptoms in women exposed to intimate partner violence. J. Affect. Disord. 2015;180:122–128. doi: 10.1016/j.jad.2015.03.047. [DOI] [PubMed] [Google Scholar]
- Holman E.A., Silver R.C., Waitzkin H. Traumatic life events in primary care patients: a study in an ethnically diverse sample. Arch. Fam. Med. 2000;9:802–810. doi: 10.1001/archfami.9.9.802. [DOI] [PubMed] [Google Scholar]
- Hooley J.M., Gruber S.A., Parker H.A., Guillaumot J., Rogowska J., Yurgelun-Todd D.A. Cortico-limbic response to personally challenging emotional stimuli after complete recovery from depression. Psychiatry Res. - Neuroimage. 2009;171:106–119. doi: 10.1016/j.pscychresns.2008.04.001. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N.C., Newman M.G. Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychol. Bull. 2017;143:1155–1200. doi: 10.1037/bul0000111. [DOI] [PubMed] [Google Scholar]
- Jin Y., Xu J., Liu H., Liu D. Posttraumatic stress disorder and posttraumatic growth among adult survivors of Wenchuan earthquake after 1 Year: prevalence and correlates. Arch. Psychiatry. Nurse. 2014;28:67–73. doi: 10.1016/j.apnu.2013.10.010. [DOI] [PubMed] [Google Scholar]
- Jobst A., Sabass L., Palagyi A., Bauriedl-Schmidt C., Mauer M.C., Sarubin N., Buchheim A., Renneberg B., Falkai P., Zill P., Padberg F. Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression. J. Psychiatr. Res. 2015;60:170–177. doi: 10.1016/j.jpsychires.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., Chen J., Guan L., Wang G., Ma H., Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Chiu W.T., Demler O., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry. 2005;62:617. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kola L. Comment global mental health and Covid-19. Lancet Psychiatry. 2020;0366:19–20. doi: 10.1016/S2215-0366(20)30235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Luo W.-T., Li Y., Li C.-N., Hong Z.-S., Chen H.-L., Xiao F., Xia J.-Y. Psychological status and behavior changes of the public during the Covid-19 epidemic in China. Infect. Dis. Poverty. 2020;9:58. doi: 10.1186/s40249-020-00678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid Systematic Review: the Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020 doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney E.A., Sattizahn J.R., Beilock S.L. Anxiety and cognition. Wiley Interdiscip. Rev. Cogn. Sci. 2014;5:403–411. doi: 10.1002/wcs.1299. [DOI] [PubMed] [Google Scholar]
- Mineka S., Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: it's not what you thought it was. Am. Psychol. 2006;61:10–26. doi: 10.1037/0003-066X.61.1.10. [DOI] [PubMed] [Google Scholar]
- McIlveen R., Curran D., Mitchell R., DePrince A., O'Donnell K., Hanna D. A meta‐analytic review of the association between alienation appraisals and posttraumatic stress disorder symptoms in trauma‐exposed adults. J. Trauma. Stress. 2020;33(5):720–730. doi: 10.1002/jts.22530. [DOI] [PubMed] [Google Scholar]
- McLean C.P., Foa E.B. Emotions and emotion regulation in posttraumatic stress disorder. Curr. Opin. Psychol. 2017;14:72–77. doi: 10.1016/j.copsyc.2016.10.006. [DOI] [PubMed] [Google Scholar]
- McNeish D.M. Using lasso for predictor selection and to assuage overfitting: a method long overlooked in behavioral sciences. Multivariate Behav. Res. 2015;50(5):471–484. doi: 10.1080/00273171.2015.1036965. [DOI] [PubMed] [Google Scholar]
- Mitchell R., Hanna D., Brennan K., Curran D., McDermott B., Ryan M., Craig K., McCullough E., Wallace P., Dyer K.F.W. Alienation appraisals mediate the relationships between childhood trauma and multiple markers of posttraumatic stress. J. Child Adolesc. Trauma. 2020;13:11–19. doi: 10.1007/s40653-018-0220-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möller H.-J.J., Bandelow B., Volz H.-P.P., Barnikol U.B., Seifritz E., Kasper S. The relevance of ‘mixed anxiety and depression’ as a diagnostic category in clinical practice. Eur. Arch. Psychiatry Clin. Neurosci. 2016;266:725–736. doi: 10.1007/s00406-016-0684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for PTSD . 2019. Using the PTSD Checklist (PCL)http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp [Google Scholar]
- Pancani, L., Marinucci, M., Aureli, N., & Riva, P. (2020). Forced social isolation and mental health: a study on 1006 Italians under COVID-19 lockdown. 10.31234/osf.io/uacfj. [DOI] [PMC free article] [PubMed]
- Pérez-Edgar K.E., Guyer A.E. Behavioral Inhibition: temperament or Prodrome? Curr. Behav. Neurosci. Rep. 2014;1:182–190. doi: 10.1007/s40473-014-0019-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff P.M., MacKenzie S.B., Lee J.Y., Podsakoff N.P. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 2003;88:879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Pugach C.P., Campbell A.A., Wisco B.E. Emotion regulation in posttraumatic stress disorder (PTSD): rumination accounts for the association between emotion regulation difficulties and PTSD severity. J. Clin. Psychol. 2020;76:508–525. doi: 10.1002/jclp.22879. [DOI] [PubMed] [Google Scholar]
- Rayce S.L.B., Holstein B.E., Kreiner S. Aspects of alienation and symptom load among adolescents. Eur. J. Public Health. 2009;19:79–84. doi: 10.1093/eurpub/ckn105. [DOI] [PubMed] [Google Scholar]
- Ren D., Wesselmann E.D., Williams K.D. Hurt people hurt people: ostracism and aggression. Curr. Opin. Psychol. 2018;19(17):34–38. doi: 10.1016/j.copsyc.2017.03.026. [DOI] [PubMed] [Google Scholar]
- Rosenström T., Jokela M. Reconsidering the definition of major depression based on collaborative psychiatric epidemiology surveys. J. Affect. Disord. 2017;207:38–46. doi: 10.1016/j.jad.2016.09.014. [DOI] [PubMed] [Google Scholar]
- Seeman M. On the meaning of alienation. Am. Sociol. Rev. 1959;24:783. doi: 10.2307/2088565. [DOI] [Google Scholar]
- Spinhoven P., Penninx B.W., Krempeniou A., van Hemert A.M., Elzinga B. Trait rumination predicts onset of Post-Traumatic Stress Disorder through trauma-related cognitive appraisals: a 4-year longitudinal study. Behav. Res. Ther. 2015;71:101–109. doi: 10.1016/j.brat.2015.06.004. [DOI] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Srinivas T., DePrince A.P., Chu A.T. Links between posttrauma appraisals and trauma-related distress in adolescent females from the child welfare system. Child Abuse Negl. 2015;47:14–23. doi: 10.1016/j.chiabu.2015.05.011. [DOI] [PubMed] [Google Scholar]
- Steel Z., Marnane C., Iranpour C., Chey T., Jackson J.W., Patel V., Silove D. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int. J. Epidemiol. 2014;43:476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles W.B., Shuster P.L., Harrigan J.A. Disclosure and anxiety: a test of the fever model. J. Pers. Soc. Psychol. 1992;63:980–988. doi: 10.1037/0022-3514.63.6.980. [DOI] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Eriksen Benros M. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain. Behav. Immun. 2020:1–12. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker E.A., Newman E., Dobie D.J., Ciechanowski P., Katon W. Validation of the PTSD checklist in an HMO sample of women. Gen. Hosp. Psychiatry. 2002;24:375–380. doi: 10.1016/S0163-8343(02)00203-7. [DOI] [PubMed] [Google Scholar]
- Walsh S.D., Kolobov T., Simanovskaya O. What is it about perceived discrimination that can lead immigrant adolescents to alcohol use and delinquency? The mediating role of feelings of alienation. Subst. Use Misuse. 2019;54:65–77. doi: 10.1080/10826084.2018.1495738. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2020. WHO Coronavirus Disease (COVID-19) Dashboard.https://covid19.who.int/ (accessed 24 June 2020) [Google Scholar]
- Woodward M.J., Eddinger J., Henschel A.V., Dodson T.S., Tran H.N., Beck J.G. Social support, posttraumatic cognitions, and PTSD: the influence of family, friends, and a close other in an interpersonal and non-interpersonal trauma group. J. Anxiety Disord. 2015;35:60–67. doi: 10.1016/j.janxdis.2015.09.002. [DOI] [PubMed] [Google Scholar]
- Xu J., Zheng Y., Wang M., Zhao J., Zhan Q., Fu M., Wang Q., Xiao J., Cheng Y. Predictors of symptoms of posttraumatic stress in Chinese university students during the 2009 H1N1 influenza pandemic. Med. Sci. Monitor. 2011;17(7) doi: 10.12659/MSM.881836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on request.