Abstract
Little is known about regional differences in volume, treatment, and outcomes of STEMI patients undergoing PCI during the pandemic. The objectives of this study were to compare COVID-19 pandemic and prepandemic periods with respect to regional volumes, outcomes, and treatment of patients undergoing percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI) between January 1, 2019 and March 14, 2020 (pre-COVID period) and between March 15, 2020 and April 4, 2020 (COVID period) in 51 New York State hospitals certified to perform PCI. The hospitals were classified as being in either high-density or low-density COVID-19 counties on the basis of deaths/10,000 population. There was a decrease of 43% in procedures/week in high-density COVID-19 counties (p <0.0001) and only 4% in low-density counties (p = 0.64). There was no difference in the change in risk-adjusted in-hospital mortality rates in either type of county, but STEMI PCI patients in high-density counties had longer times from symptom onset to hospital arrival and lower cardiac arrest rates in the pandemic period. In conclusion, the decrease in STEMI PCIs during the pandemic was mainly limited to counties with a high density of COVID-19 deaths. The decrease appears to be primarily related to patients not presenting to hospitals in high-density COVID regions, rather than PCI being avoided in STEMI patients or a reduction in the incidence of STEMI. Also, high-density COVID-19 counties experienced delayed admissions and less severely ill STEMI PCI patients during the pandemic. This information can serve to focus efforts on convincing STEMI patients to seek life-saving hospital care during the pandemic.
One of the collateral impacts of COVID-19 has been the large decrease in patients hospitalized for life-threatening events. ST-elevation myocardial infarction (STEMI) is a life-threatening condition that requires immediate transport to the hospital for stabilization and restoration of blood flow. Primary percutaneous coronary intervention (PCI) is the recommended treatment modality for patients with STEMI.1 Previous studies have demonstrated that catheterization laboratory activations for STEMI as well as hospitalizations for STEMI and related conditions have decreased during the COVID-19 pandemic.2, 3, 4, 5, 6, 7, 8, 9, 10, 11 However, they did not thoroughly investigate differences in patient characteristics, processes of care, and outcomes between the pandemic and prepandemic periods that could enhance further understanding of the impact of the pandemic on STEMI patients. A couple of recent studies did examine some of these issues, but for all acute cardiovascular conditions, and they were was focused on health systems rather than a specific geographic region of the United States.10 , 11 Furthermore, earlier studies did not examine the differential impact of the pandemic as a function of its magnitude.
Methods
This study is exempted from IRB approval since it is retrospective and all personal identifiers were encrypted. Data were obtained from New York State's Percutaneous Coronary Interventions Reporting System (PCIRS), a mandatory PCI registry that has been used since 1992 to report hospital and cardiologist-level outcomes to hospitals and the public. The registry contains detailed information about each patient who underwent PCI, including demographics; preprocedural risk factors; periprocedural outcomes; and dates of admission, discharge, and procedure. As of January 3, 2020, there is also a variable that denotes the presence of COVID-19 during the PCI admission.
This study examined data from STEMI patients undergoing PCI in 51 of the 65 hospitals in New York State certified to perform PCI who volunteered to submit data in an expedited time frame. The remaining 14 hospitals were not included because they did not send voluntary data. The participating hospitals were identified as being in either high-density or low-density COVID-19 counties on the basis of deaths/10,000 population because there was a clear demarcation in both mortality and in cases per capita among counties. High-density (HD) COVID-19 counties had ≥10.2 deaths per 10,000 population (and also had ≥37.2 cases per 10,000 population) and lower-density (LD) COVID-19 counties had ≤4.3 deaths per 10,000 population (and also had ≤16.9 cases per 10,000 population) as of March 30, 2020.12 There was no other subdivision of counties for which such a large gap existed. The 10 HD counties were the boroughs of New York City, the 2 counties in Long Island, and regions just north of New York City (Westchester, Rockland, and Orange Counties), see Supplementary Appendix, Figure.
The study included 7,047 STEMI patients who underwent primary or rescue PCI. STEMI was defined as having ECG evidence and cardiac biomarkers (see the Online Appendix for a complete definition). The January 1, 2019 to March 14, 2020 prepandemic period included 6,584 patients admitted during January 1, 2019 to March 14, 2020, and the pandemic period included 463 patients admitted during March 15, 2020 to April 25, 2020 who were discharged by April 30, 20. The demarcation time March 15, 2020 was chosen because it was when social distancing was recommended by the federal government, and because it was clear from inspecting the data that this was the time when arrival patterns changed.
A linear regression analysis was used to examine the mean number of PCIs performed per week in the 6 weeks before the pandemic period to ascertain that there was no underlying secular trend before the pandemic. Then, the mean number of PCIs performed per week in that 10-week period and in the 6-week pandemic study period was compared for all hospitals, and for hospitals in HD and LD counties. We also compared the mean number of PCIs per week performed in the 2020 pandemic study period with the mean number in the period exactly 1 year before (March 15, 2019 to April 25, 2019) to ensure that differences in PCIs performed between the prepandemic and pandemic periods were not related to seasonal variations.
Differences in patient risk factors and processes of care (transfers, use of thrombolytics, onset to door time, door to balloon time) between procedures performed during the prepandemic period and pandemic study period were examined for hospitals in HD and LD counties. Two-sample t tests or Wilcoxon Rank Sum tests were used to test for differences in continuous variables and Chi-square tests were used to test for differences in categorical variables.
Backward logistic regression models were used to test for a difference in in-hospital mortality for the 2 time periods for HD and LD counties. The independent control variables included all patient risk factors available in the registry, including demographics (age, sex, race, and ethnicity), hemodynamic state, ejection fraction, type of angina, and numerous co-morbidities (see Table 1 ). The time period (prepandemic, pandemic) was the binary study variable.
Table 1.
Patient characteristics, processes of care, and outcomes for STEMI patients undergoing PCI in COVID-19 and pre-COVID-19 periods in New York State
| Hospitals in high COVID density Counties |
Hospitals in low COVID density Counties |
||||||
|---|---|---|---|---|---|---|---|
| Before COVID | During COVID | P-value for difference in prevalence | Before COVID | During COVID | P-value for difference in prevalence | ||
| Jan 1, 2019 - Mar 14, 2020 | Mar 15, 2020 - Apr 30, 2020 | Jan 1, 2019 - Mar 14, 2020 | Mar 15, 2020 - Apr 30, 2020 | ||||
| Characteristic | (N = 3,411, 94.80%) | (N = 187, 5.20%) | (N = 3,173, 92.00%) | (N = 276, 8.00%) | |||
| Observed in-hospital mortality rate | 4.98% | 5.35% | 0.82 | 5.26% | 3.62% | 0.24 | |
| Length of stay (day) | mean±sd | 6.23 ± 11.92 | 3.72 ± 2.29 | 4.99 ± 8.20 | 3.94 ± 3.29 | ||
| (For admissions before April 16, 20) | median (q1-q3) | 4 (3-6) | 3 (3-4) | <0.0001 | 4 (3-5) | 3 (3-4) | <0.0001 |
| COVID | Confirmed | 9.63% | 0.36% | ||||
| Suspected | 4.81% | 2.90% | |||||
| None (or history) | 85.56% | 96.74% | |||||
| Transferred from another hospital | Transfer | 17.77% | 13.90% | 0.18 | 29.53% | 22.83% | 0.02 |
| Direct admit | 82.23% | 86.10% | 70.47% | 77.17% | |||
| Use of thrombolytics | 0.85% | 2.67% | 0.03 | 9.33% | 8.70% | 0.73 | |
| Onset to hospital arrival time (minute) | Direct admit, median (q1-q3) | 89 (56-179) | 120 (60-243) | <0.01 | 91 (55-170) | 90 (56-174) | 0.40 |
| (STEMI within 24 hrs) | Transfer, median (q1-q3) | 198 (129-332) | 272 (171-435) | 0.02 | 210 (139-320) | 223 (158-409) | 0.18 |
| Hospital arrival to device time (minute) | Direct admit, median (q1-q3) | 66 (49-85) | 65 (52-96) | 0.05 | 62 (42-83) | 60 (45-83) | 0.41 |
| (STEMI within 24 hrs) | Transfer, median (q1-q3) | 39 (24-64) | 41 (25-57) | 0.50 | 39 (25-67) | 38 (27-97) | 0.31 |
| Age (years) | mean±sd | 63.3 ± 12.6 | 61.1 ± 11.9 | 0.02 | 62.6 ± 12.1 | 62.4 ± 12.8 | 0.82 |
| median (q1-q3) | 63 (55-72) | 61 (53-68) | 62 (55-71) | 62 (54-70) | |||
| 18-44 | 6.92% | 8.56% | 6.84% | 7.97% | |||
| 45-54 | 18.85% | 24.06% | 19.10% | 20.65% | |||
| 55-64 | 32.31% | 31.02% | 34.54% | 32.25% | |||
| 65-74 | 23.63% | 22.99% | 23.07% | 23.19% | |||
| 75-84 | 12.93% | 11.76% | 12.48% | 11.59% | |||
| >85 | 5.36% | 1.60% | 3.97% | 4.35% | |||
| Male | 75.96% | 76.47% | 0.87 | 71.38% | 72.46% | 0.70 | |
| Female | 24.04% | 23.53% | 28.62% | 27.54% | |||
| White (non-Hispanic) | 54.91% | 47.59% | 0.11 | 90.42% | 86.59% | 0.04 | |
| Black (non-Hispanic) | 10.94% | 16.04% | 4.63% | 5.80% | |||
| Asian | 12.34% | 12.83% | 1.45% | 0.72% | |||
| Hispanic | 15.22% | 14.44% | 2.36% | 4.35% | |||
| Other | 6.60% | 9.09% | 1.13% | 2.54% | |||
| BMI (kg/m2) | mean±sd | 28.5 ± 6.5 | 28.4 ± 5.1 | 0.69 | 30.0 ± 6.7 | 30.0 ± 6.1 | 0.93 |
| median (q1-q3) | 27.6 (24.9-31.1) | 27.7 (25.0-31.5) | 29.2 (25.9-33.1) | 29.1 (25.7-33.3) | |||
| <18.5 | 0.62% | 0.53% | 0.91% | 0.36% | |||
| 18.5-25.0 | 25.51% | 24.06% | 18.97% | 19.20% | |||
| 25.1-30.0 | 41.72% | 42.25% | 36.68% | 35.87% | |||
| 30.1-35.0 | 21.52% | 22.46% | 26.32% | 28.62% | |||
| 35.1-40.0 | 6.89% | 8.56% | 10.97% | 10.51% | |||
| >40.0 | 3.75% | 2.14% | 6.15% | 5.43% | |||
| Ejection fraction | < 20% | 2.87% | 2.14% | 0.60 | 1.51% | 3.99% | 0.02 |
| 20%-29% | 9.59% | 9.09% | 7.63% | 7.25% | |||
| 30%-39% | 18.15% | 14.97% | 14.37% | 12.68% | |||
| ≥40% | 69.39% | 73.80% | 76.49% | 76.09% | |||
| Shock | Refractory | 5.89% | 3.21% | 0.05 | 2.55% | 2.54% | 0.51 |
| Nonrefractory | 4.34% | 1.60% | 3.69% | 5.07% | |||
| None | 89.77% | 95.19% | 93.76% | 92.39% | |||
| Anoxic brain injury | 2.05% | 0.00% | 0.05 | 2.46% | 0.72% | 0.07 | |
| Cardiac arrest | 8.18% | 2.67% | <0.01 | 9.20% | 5.80% | 0.06 | |
| Cerebrovascular disease | Stroke, occlusion, cerebrovascular procedure performed | 5.25% | 2.14% | 0.06 | 4.60% | 5.43% | 0.53 |
| No symptoms or only TIA | 94.75% | 97.86% | 95.40% | 94.57% | |||
| Peripheral vascular disease | 3.84% | 1.60% | 0.12 | 5.04% | 4.71% | 0.81 | |
| Chronic lung disease | Severe | 0.03% | 0.53% | 0.17 | 0.41% | 0.72% | 0.03 |
| Moderate | 0.56% | 0.53% | 0.79% | 0.00% | |||
| Mild | 2.52% | 2.14% | 4.95% | 8.33% | |||
| None | 96.89% | 96.79% | 93.85% | 90.94% | |||
| Heart failure | Current | 7.77% | 7.49% | 0.70 | 4.76% | 4.35% | 0.67 |
| Past | 1.91% | 1.07% | 1.76% | 1.09% | |||
| None | 90.33% | 91.44% | 93.48% | 94.57% | |||
| Diabetes mellitus | With insulin | 8.33% | 6.95% | 0.65 | 9.14% | 8.70% | 0.68 |
| With oral | 17.27% | 13.90% | 13.68% | 12.32% | |||
| With diet | 1.32% | 1.07% | 1.32% | 1.45% | |||
| With other or no meds | 4.84% | 5.88% | 3.75% | 5.43% | |||
| None | 68.25% | 72.19% | 72.11% | 72.10% | |||
| Creatinine and dialysis | <1.2 mg/dl | 69.33% | 70.59% | 0.39 | 72.52% | 71.01% | 0.83 |
| ≥1.2 and ≤1.5 mg/dl | 21.23% | 24.06% | 19.54% | 20.29% | |||
| >1.5 and ≤2.0 mg/dl | 5.34% | 2.67% | 5.29% | 6.52% | |||
| >2.0 mg/dl | 2.96% | 2.14% | 1.86% | 1.81% | |||
| On dialysis | 1.14% | 0.53% | 0.79% | 0.36% | |||
| Malignant ventricular arrhythmia | 2.52% | 0.53% | 0.09 | 2.27% | 1.09% | 0.20 | |
| Stent thrombosis at admission | 2.43% | 3.74% | 0.23 | 2.49% | 2.17% | 0.75 | |
| Prior PCI | 17.65% | 18.72% | 0.71 | 16.23% | 15.22% | 0.66 | |
| Prior cardiac surgery | 3.61% | 1.07% | 0.07 | 3.09% | 2.17% | 0.39 | |
| Prior organ transplant | 0.29% | 0.53% | 0.44 | 0.50% | 0.72% | 0.65 | |
| Left main narrowing | 4.22% | 2.14% | 0.16 | 3.31% | 2.54% | 0.49 | |
| Number of coronary arteries narrowed | 3 | 16.92% | 14.44% | 0.37 | 9.99% | 7.61% | 0.42 |
| 2 | 32.13% | 29.41% | 29.40% | 31.16% | |||
| 1 | 50.95% | 56.15% | 60.61% | 61.23% | |||
Results
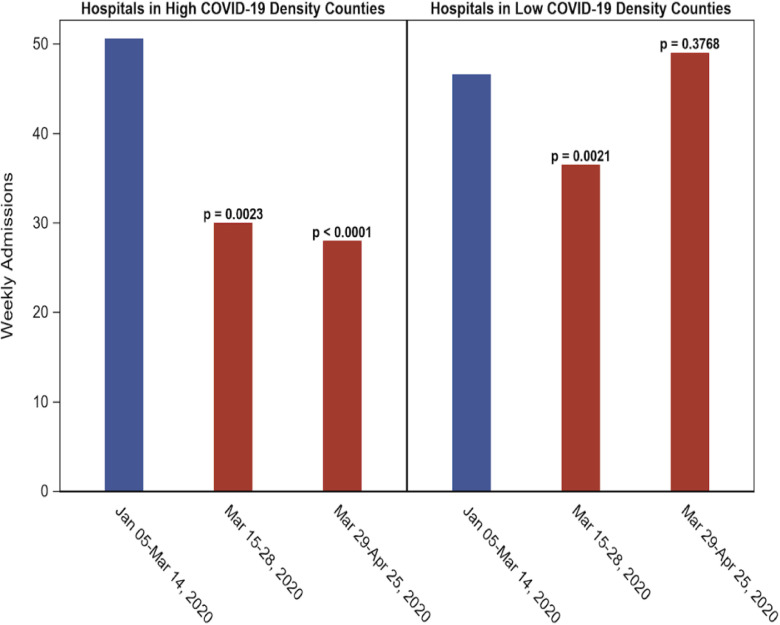
The mean number of STEMI PCI procedures performed per week was significantly higher in the 2020 prepandemic period than in the pandemic study period (97.2 vs 73.5, p <0.0001), a decrease of 24%.However, in HD counties, the decrease between the 2 periods was 43% (p <0.0001), but in the LD counties, the decrease was only 4% (p = 0.64), see Figure 1 . In HD counties, the weekly mean number of STEMI PCI procedures performed during the first 2 weeks of the pandemic study period was very similar to the weekly number performed in the final 4 weeks (30.0 vs 28.0). In LD counties, there was a decrease of 22% (p = 0.002) in the first 2 weeks in the pandemic study period compared with the prepandemic period, but in the last 4 weeks of the 6-week period, the STEMI PCI procedures performed per week actually exceeded the weekly average in the 10-week prepandemic period (49.0 vs 46.6 procedures per week).
Figure 1.
Total percutaneous coronary intervention procedures for ST-elevation myocardial infarction by week in New York in prepandemic and pandemic periods in high-density and low-density COVID-19 counties.
When compared with the same time period 1 year before, there were 33% fewer (p <0.0001) STEMI PCI procedures per week during the pandemic study period. Also, there was no significant weekly change in the number of PCIs performed for STEMI patients during the prepandemic period (adjusted R2 = 0.08, p =0.22).
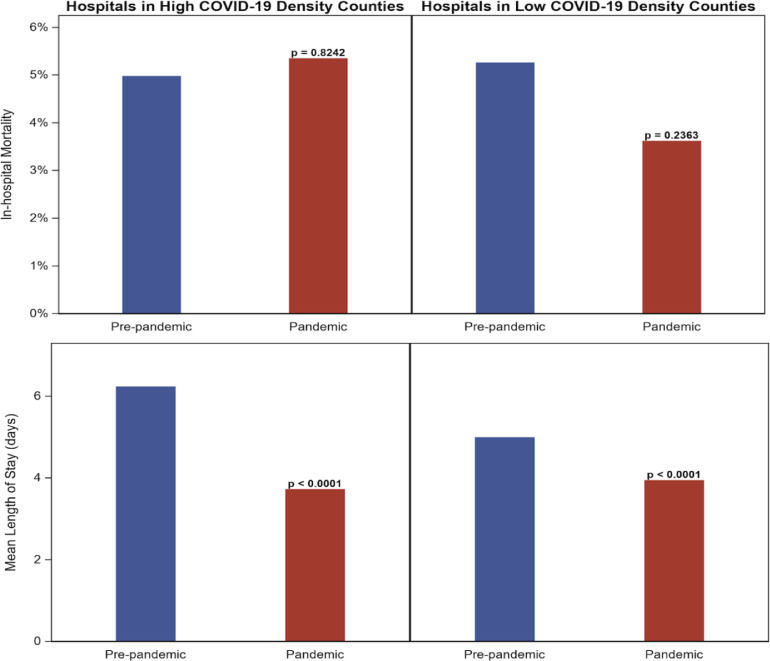
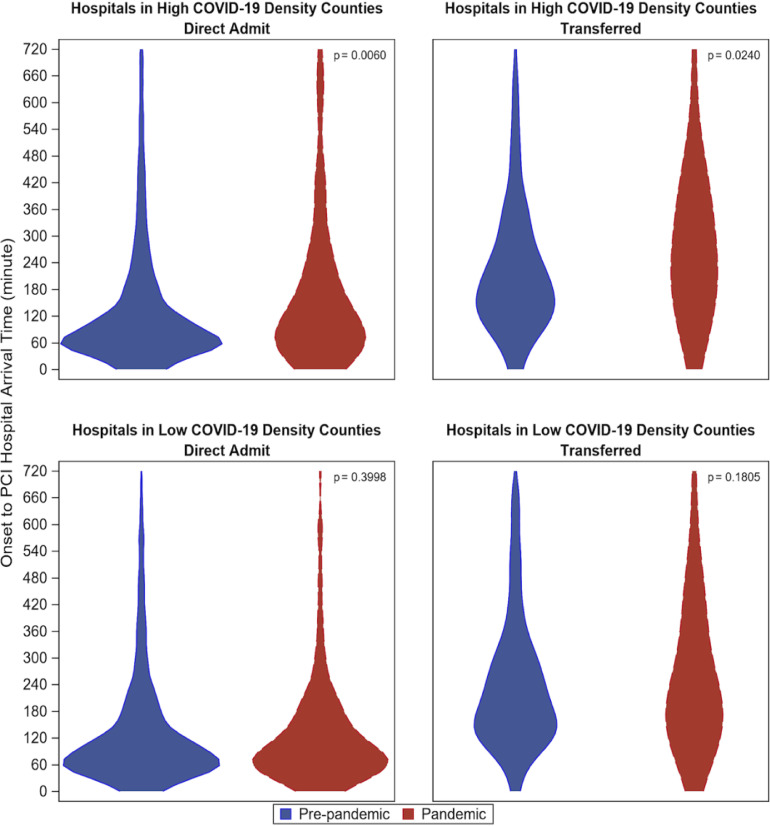
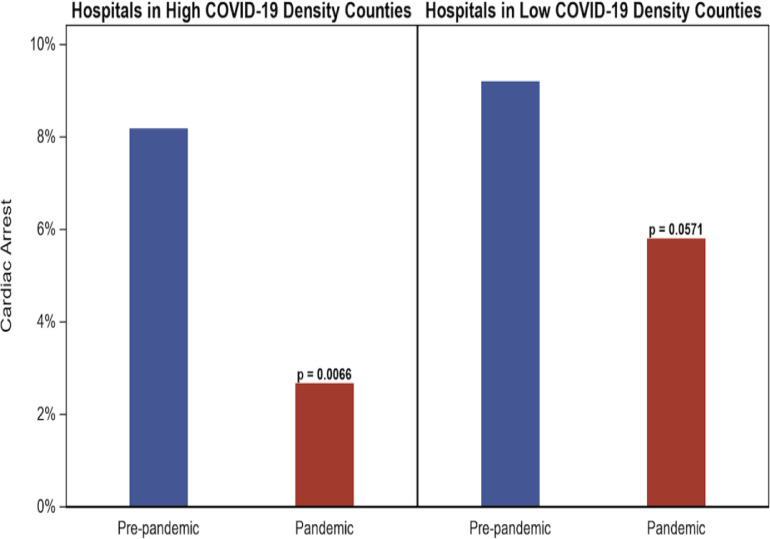
Table 1 examines differences in HD and LD counties between pandemic and extended prepandemic (January 1, 2019 to March 14, 2020) periods in mortality, length of stay, transfer rates, use of thrombolytics, times from symptom onset to arrival at the hospital, door to balloon times, and numerous patient risk factors. There was no difference in in-hospital mortality rates in the 2 periods for either HD or LD counties but the pandemic period was associated with a shorter mean length of stay in both HD and LD counties (see Table 1 and Figure 2 ). Also, there was a lower rate of transfers from other hospitals in LD, but not HD counties (22.8% vs 29.5%, p = 0.02). Patients directly admitted and patients transferred to PCI hospitals in HD counties, but not LD counties, had longer times from symptom onset to arrival at the PCI hospital (see Table 1 and Figure 3 ). There was no difference in door to balloon times between pandemic and prepandemic periods for hospitals in either HD or LD counties, but hospitals in HD counties used more thrombolytic therapy before PCI during the pandemic period. Also, patients in HD hospitals were less likely to present with cardiac arrest during the pandemic period (Table 1 and Figure 4 ).
Figure 2.
In-hospital mortality and length of stay for patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction in high-density and low-density COVID-19 counties in New York: May 1, 2019-March 14, 2020 vs March 15, 2020-April 25, 2020.
Figure 3.
Time from symptom onset to arrival for patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction in high-density and low-density COVID-19 counties in New York: May 1, 2019-March 14, 2020 vs March 15, 2020-April 25, 2020.
Figure 4.
Preprocedure cardiac arrest for patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction in high-density and low-density COVID-19 counties in New York: May 1, 2019-March 14, 2020 vs March 15, 2020-April 25, 2020.
After adjustment for numerous patient risk factors using logistic regression, we found that the mortality rate for the pandemic period was not significantly different from the mortality rate in the prepandemic period in either HD or LD counties (odds ratio [OR] = 0.92 (0.32, 2.69) and OR = 0.73 (0.33, 1.58), respectively). Almost all (18 of 19) STEMI PCI patients with confirmed COVID-19 were in HD counties, and 3 of those patients (16.7%) died. Patients who were confirmed to have COVID-19 in HD counties had significantly higher mortality than other STEMI patients (OR = 18.3 [3.2, 104.3]), but the 17 patients who were suspected but not confirmed to have COVID-19 did not (3 deaths, OR = 6.0 (0.96, 37.4). No confirmed or suspected STEMI PCI patients with COVID-19 died in LD counties.
Discussion
We found that there was a significant 24% decrease in the weekly number of PCIs performed for STEMI patients in New York State during the first 6 weeks of the COVID-19 pandemic compared with a 10-week period preceding the pandemic, but that this decrease was highly dependent on whether the county was a high- or low-density COVID-19 county (43% vs 4% decrease). It is possible that large decreases in the use of PCI for STEMI could be related to patients presenting to the hospital but not undergoing PCI. However, in an earlier unpublished survey of 41 of the 51 hospitals in this study that tracked numbers of STEMI arrivals without PCI in addition to STEMI patients who underwent PCI, we found that the percentage of STEMI patients who underwent PCI decreased only from 91.4% in the prepandemic period to 89.7% in the pandemic period.
It is also possible that there have been fewer STEMIs during the pandemic because of a less frenetic lifestyle, reduced driving, and decreases in pollution.13 However, the fact that the reduction in total STEMI PCIs in LD counties was negligible suggests that there were not substantially fewer patients with STEMIs in those areas. Thus, we conclude that the most likely reason for the decrease in STEMI PCIs in HD counties is that many STEMI patients avoided or delayed initiation of care. Other studies have hypothesized this,14, 15, 16, 17 but our separate analyses of HD and LD counties supply evidence for this hypothesis.
Unlike STEMI PCI patients in LD counties, we found that patients in HD counties experienced longer times from symptom onset to arrival at the hospital during the pandemic, perhaps because of very busy emergency medical services or because of patient delays in seeking care. Patients in HD counties were also less likely to have presented with a cardiac arrest. This could have happened because they died before being admitted as a result of travel delays or the fear of contracting COVID-19.
For both HD and LD counties, lengths of stay were significantly lower, and risk-adjusted mortality rates were no different in the pandemic study period. The lower lengths of stay suggest that care for these patients may have been abbreviated as a result of concerns about having sufficient capacity for COVID-19 patients, or concerns about patients being infected by COVID-19 while in the hospital. Although in-hospital mortality rates were no different in the pandemic period, the potential mortality impact on STEMI PCI patients during the pandemic could be better discerned with access to short- and medium-term mortality rates after discharge, but those vital statistics data are not yet available. Notably, there was no difference in door to balloon times in either HD or LD counties, which is remarkable given the challenges hospitals were confronted with during the pandemic. We also found that STEMI patients undergoing PCI with COVID-19 were rare but had significantly higher in-hospital mortality rates. It should be noted that most asymptomatic patients in the pandemic study period were not tested for COVID-19 due to the limited testing availability at the time. Therefore, the impact of asymptomatic COVID-19 on PCI outcomes is unknown.
The study has some important limitations. First, it was limited to 51 volunteers (78%) among the 65 hospitals that perform PCI in New York State because mandatory reporting was suspended during the pandemic, so the results may not reflect the entire statewide experience. It is possible that hospitals that were the most beleaguered by the pandemic were less likely to voluntarily report data and that has caused us to underestimate the impact of the pandemic. In fact, although almost all (21 of 23) hospitals from LD counties contributed data, a lower percentage (30 of 42) hospitals in HD counties contributed data.
Another limitation is that the outcome measure used was in-hospital mortality. We would have preferred to have used in-hospital/30-day mortality because it is arguably a better measure of short-term outcome.18 A shorter length of stay during the pandemic period may have resulted in deaths shortly after discharge. We could not use in-hospital/30-day mortality because vital statistics data are not yet available for matching to obtain deaths after discharge.
In conclusion, the first 6 weeks of the pandemic period were associated with a large decrease in the number of STEMI patients undergoing PCI in HD, but not LD, counties. The decrease in STEMI PCI procedures appears to be primarily related to fewer patients with STEMI being admitted to hospitals in HD COVID-19 areas rather than STEMI patients in the hospital not undergoing PCI or changes in lifestyle and pollution levels leading to a reduction in STEMI incidence. This information could prove to be valuable in focusing future efforts to persuade STEMI patients to seek lifesaving care in PCI-capable hospitals. STEMI patients undergoing PCI in HD counties during the pandemic also experienced longer times from symptom onset to arrival at the hospital, which suggests that patients may have delayed seeking care, although longer times could also be related to ambulances that were busy transporting COVID patients. STEMI PCI patients during the pandemic were less likely to have cardiac arrests than their prepandemic counterparts. Although speculative, it is possible that this is because they died at home or in ambulances during the pandemic.
Author Contributions
Hannan: Conceptualization, methodology, writing-original draft, supervision, project administration; Wu: Software, formal analysis; Cozzens: Conceptualization, methodology, writing-review and editing ; Friedrich: Conceptualization, methodology, writing-review and editing; Tamis-Holland: Conceptualization, methodology, writing-review and editing; Jacobs: Conceptualization, methodology, writing-review and editing; Ling: Conceptualization, methodology, writing-review and editing ; King: Conceptualization, methodology, writing-review and editing; Venditti: Conceptualization, methodology, writing-review and editing ; Walford: Conceptualization, methodology, writing-review and editing; Berger: Conceptualization, methodology, writing-review and editing; Kirtane: Conceptualization, methodology, writing-review and editing; Kamran: Conceptualization, methodology, writing-review and editing.
Disclosures
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Relationships with Industry: Dr. King is a member of the Data Safety Monitoring Board for Harvard Clinical Research Institute, Duke University, Capicor, Inc., Merck & Company and Stentys. Dr. Jacobs is a site PI for Abbott Vascular and AstraZeneca. Dr Kirtane reports Institutional funding to Columbia University and/or Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, ReCor Medical. In addition to research grants, institutional funding includes fees paid to Columbia University and/or Cardiovascular Research Foundation for speaking engagements and/or consulting; no speaking/consulting fees were personally received. Personal: Travel Expenses/Meals from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron.
Acknowledgment
The authors would like to thank the 51 hospitals and their cardiac catheterization laboratories for their efforts to voluntarily submit PCI data in the midst of the COVID-19 pandemic.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.amjcard.2020.11.033.
Appendix. Supplementary materials
References
- 1.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodríguez-Leor O, Cid-Alvarez B, Ojeda S, Rodriguez-Leor O, Cid-Álvarez B, Pérez de Prado A, Rossello X, Ojeda S, Serrador A, López-Palop R, Martín-Moreira SJ, Rumoroso JR, Cequier Á, Ibáñez B, Cruz-González I, Romaguera R, Moreno R, Working Group on the Infarct Code of the Interventional Cardiology Association of the Spanish Society of Cardiology Investigators. Villa M, Ruíz-Salmerón R, Molano F, Sánchez C, Muñoz-García E, Íñigo L, Herrador J, Gómez-Menchero A, Gómez-Menchero A, Caballero J, Ojeda S, Cárdenas M, Gheorghe L, Oneto J, Morales F, Valencia F, Ruíz JR, Diarte JA, Avanzas P, Rondán J, Peral V, Pernasetti LV, Hernández J, Bosa F, Lorenzo PLM, Jiménez F, Hernández JMT, Jiménez-Mazuecos J, Lozano F, Moreu J, Novo E, Robles J, Moreiras JM, Fernández-Vázquez F, Amat-Santos IJ, Gómez-Hospital JA, García-Picart J, Blanco BGD, Regueiro A, Carrillo-Suárez X, Tizón H, Mohandes M, Casanova J, Agudelo-Montañez V, Muñoz JF, Franco J, Del Castillo R, Salinas P, Elizaga J, Sarnago F, Jiménez-Valero S, Rivero F, Oteo JF, Alegría-Barrero E, Sánchez-Recalde Á, Ruíz V, Pinar E, Pinar E, Planas A, Ledesma BL, Berenguer A, Fernández-Cisnal A, Aguar P, Pomar F, Jerez M, Torres F, García R, Frutos A, Nodar JMR, García K, Sáez R, Torres A, Tellería M, Sadaba M, Mínguez JRL, Merchán JCR, Portales J, Trillo R, Aldama G, Fernández S, Santás M, Pérez MPP. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 4.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;19:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braiteh N, Rehman W, Alom M, Skovira V, Breiteh N, Rehman I, Yarkoni A, Kahsou H, Rehman A. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic. 2020;DOI.org/10.1016/j.ahj.2020.05.009. [DOI] [PMC free article] [PubMed]
- 6.Coughlan JJ, Chongpresertpon M, Arockiam S, Arnas S, Kiernan J. COVID-19 and STEMI: a snapshot analysis of presentation patterns during a pandemic. Int J Cardiol Heart Vasc. 2020 doi: 10.1016/j.ijcha.2020.100546. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stefanini GG, Motorfano M, Trabattoni D, Andreini D, Ferrante G, Ancona M, Metra M, Curello S, Maffeo D, Pero G, Cacucci M, Assanelli E, Bellini B, Russo F, Ielasi A, Tespili M, Danzi GB, Vandoni P, Bollati M, Barbieri L, Oreglia J, Lettieri C, Cremonesi A, Carugo S, Reimers B, Condorelli G, Chieffo A. ST-elevation in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141:2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C. Reductions of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. 10.1093;eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD Vaduganathan M. Fewer hospitalization for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76:280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gluckman TJ, Wilson MA, Chiu S-T, Penny BW, Chepuri VB, Waggoner JW, Spinelli KJ. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3629. Published online August 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Available at:https://github.com/nytimes/covid-19-data/blob/master/us-counties.csv. Accessed August 6, 2020.
- 12.Bernstein L, Sellers FS. Patients with heart attacks, strokes and even appendicitis vanish from hospitals. Washington Post. Available at:https://www.washingtonpost.com/health/patients-withheart-attacks-strokes-and-even-appendicitisvanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html. Accessed July 16, 2020.
- 13.Neville S, Bounds A, Dickie M, Cocco F, Staton B. Empty non-coronavirus beds raise fears that sickest are avoiding NHS. Financial Times. Available at: https://www.ft.com/content/d5ac0a79-6647-4f49-bb64-d1cc66362043. Accessed July 16, 2020.
- 14.Krumholz HM. Where have all the heart attacks gone? The New York Times. Available at:https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heartattack-stroke.html. Accessed July 16, 2020.
- 15.Sheth K. Hospital admissions for strokes appear to have plummeted, a doctor says, a possible sign people are afraid to seek critical help. Washington Post. Available at:https://www.washingtonpost.com/national/health-science/hospital-admissions-for-strokes-appear-to-haveplummeted-a-doctors-says-a-possible-sign-peopleare-afraid-to-seek-critical-help/2020/04/08/2048b886-79ac-11ea-b6ff-597f170df8f8_story.html. Accessed July 16, 2020.
- 16.Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377:732–740. doi: 10.1016/S0140-6736(10)62296-9. [DOI] [PubMed] [Google Scholar]
- 17.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, Sharifzadehgan A, Waldmann V, Beganton F, Narayanan K, Lafont A, Bougouin W, Jouven X. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. doi.org/10.1016.S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.New York State Department of Health; 2019. Percutaneous Coronary Interventions in New York State: 2014-2016.https://www.health.ny.gov/statistics/diseases/cardiovascular/docs/pci_2014-2016.pdf Available at: Accessed on July 7, 20. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.