A high incidence of heat illness during the COVID-19 pandemic would burden the emergency care system because of difficulties in differentiating these two conditions due to their similar symptoms and lack of specific differential diagnostic procedures [1]. Heat illness is a growing health concern in Japan. In 2018, 95,137 patients with heat illness were transported by ambulance [2]. Additionally, mass gathering events in summer, such as the Tokyo Olympic and Paralympic Games (Tokyo 2020 Games) in the mid-summer of 2021, may further increase the incidence.
This paper discusses the potential burden of heat illness imposed on the emergency care system during the COVID-19 pandemic in usual days and mass gathering events based on the data of COVID-19 and heat illness in Tokyo in 2020 summer.
Differentiating heat illness and COVID-19 is challenging for several reasons. First, they share the major clinical symptoms (e.g. hyperthermia, fatigue, headache, myalgia, dyspnoea, tachypnoea, nausea, vomiting, and disturbed consciousness) [1], and heat illness is diagnosed considering clinical symptoms and exposure to high temperatures [3]. Dysgeusia and dysosmia, although specific to COVID-19, do not appear in all patients. Second, no specific biomarkers exist to diagnose them; however, renal dysfunction or inflammatory reactions may be useful to differentiating them among selected populations (non-emergent mild to moderate cases) [4]. Third, although a history of close contact with COVID-19 patients supports its diagnosis, even without such a history, COVID-19 cannot be completely ruled out because pre-symptomatic patients can transmit the virus [5]. Furthermore, negative results of diagnostic tests for COVID-19, chest computed tomography (CT) and reverse transcriptase polymerase chain reaction (RT-PCR) test, cannot decisively exclude COVID-19 when pre-test odds of having COVID-19 is high during the pandemic. Both tests have a negative likelihood ratio of approximately 0.33 [1,6], meaning that their negative results reduce the odds to approximately one-third of the pre-test level.
Consequently, patients with heat illness, even after negative results of CT or a single RT-PCR test, may be admitted to a negative-pressure isolation room as COVID-19-suspected cases. Subsequent several consecutive negative RT-PCR results and observation of the clinical course can remove the suspected status. Then, few isolation rooms (the number is limited in Japan, particularly in secondary-level hospitals) would be occupied with confirmed or suspected COVID-19 cases, resulting in reduced capacities of hospitals to treat more COVID-19-suspected cases.
Such burdens on the emergency care system can be evaluated based on the ease of patient transfer in pre-hospital settings because of the following characteristics of the Japanese system. The ambulance services perform triage at the scene, select an appropriate hospital depending on the patient's conditions, and request the hospital to accept the patient [7]. The hospital may decline the request based on their treatment abilities and bed vacancies. Tightened emergency care resources would increase the declines.
The Tokyo Metropolitan Government monitors the number of difficult-to-transfer cases as an indicator of the burden to the emergency care system [8]. The difficult-to-transfer cases are defined as patients who require five times or more requests or 20 min or longer requesting procedures; this definition excludes severe cases whose transfer requests are sent via special communication paths. For the difficult-to-transfer cases, coordination mechanisms are invoked.
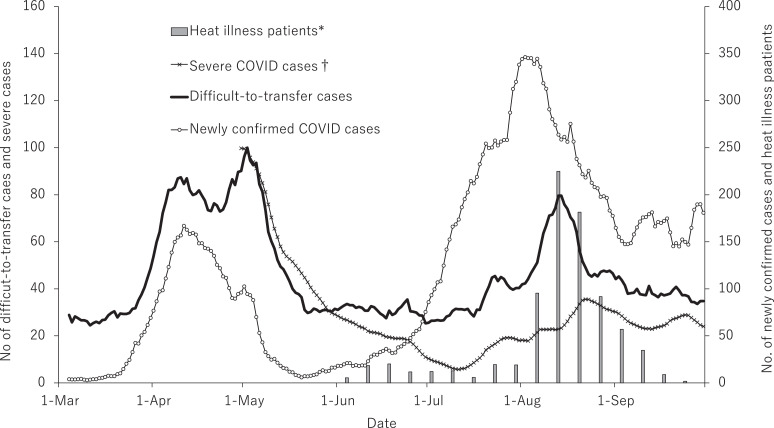
The number of difficult-to-transfer cases increased during the two waves of COVID-19 outbreak during April–May and July–September in 2020 in Tokyo (Fig. 1). The first increase corresponded to increased severe COVID-19 cases requiring mechanical ventilation or extracorporeal membrane oxygenation [8], whose number can represent hospitalized (moderate to severe) cases. A large number of such cases occupied the isolation rooms and depleted medical resources (e.g. personal protection equipment), reducing the hospitals’ care capacities. After the first wave subsided, the number of difficult-to-transfer cases steadied down to the normal level.
Fig. 1.
Trends in difficult-to-transfer patients in emergency medical services in relation to the waves of COVID-19 and heat illness in Tokyo between March and September 2020.
Data on the number of heat illness patients were obtained from Fire and Disaster Management Agency [2]; data on the number of coronavirus disease (COVID-19) patients (total and severe) and difficult-to-transfer patients were derived from the Tokyo Metropolitan Government [8]. We calculated and indicated 7-day moving average for the number of COVID-19 patients and difficult-to-transfer patients.
*For heat illness patients, weekly total number was the only available data (Monday to Sunday); therefore, daily average number in each week was calculated (indicated as a bar chart) on the midweek days (Thursday).
†Data on severe cases in March and April were not available because the definition of “severe” was determined on 27 April 2020.
The second increase started in late July, whereas the second wave of COVID-19 in Tokyo started in June. This discrepancy is due to fewer severe COVID-19 cases than in the first-wave period, which reflected a great increase in RT-PCR tests to detect minor cases [8]. The number of difficult-to-transfer cases corresponded well with the number of patients with heat illness transported by ambulance. Heat illness patients, rather than COVID-19 cases, occupied the isolation rooms.
Before the pandemic, the emergency care system in Tokyo had capacities to manage the increasing number of patients with heat illness. There was no increase in the number of difficult-to-transfer patients in summer until 2019 despite the considerable number of patients with heat illness transported by ambulance. The medical care provision plans for the Tokyo 2020 Games have also considered the risk of a large incident of heat illness [9,10]. Heat illness prevention measures and disaster management and mass casualty incident plans have been prepared to manage even the worst-case scenario of 50–60 patients with heat illness in one competition venue [9].
However, this pandemic forces us to reconsider the presupposition of the medical care planning for summer in both usual days and mass gathering events. The pandemic complicates the heat illness management, necessitating additional resources. If we are to conduct the game in the 2021 summer as planned without complete pandemic containment, we must allocate far more medical care resources than what was planned before the pandemic.
Author Contributions
All authors equally contributed to manuscript preparation.
Declaration of Interests
None declared.
Funding support
None.
References
- 1.Working group on heatstroke medical care during the COVID-19 epidemic Heatstroke management during the COVID‐19 epidemic: recommendations from the experts in Japan. Acute Med Surg. 2020;7(1):e560. doi: 10.1002/ams2.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fire and Disaster Management Agency. Heat illness information. 2020. https://www.fdma.go.jp/disaster/heatstroke/post3.html (Accessed 3 October 2020). in Japanese.
- 3.Gauer R., Meyers B.K. Heat-related illnesses. Am Fam Phys. 2019;99(8):482–489. [PubMed] [Google Scholar]
- 4.Obinata H., Yokobori S., Ogawa K. Indicators of acute kidney injury as biomarkers to differentiate heatstroke from coronavirus disease 2019: a retrospective multicenter analysis. J Nippon Med Sch. 2020 doi: 10.1272/jnms.JNMS.2021_88-107. (in press) [DOI] [PubMed] [Google Scholar]
- 5.Ferretti L., Wymant C., Kendall M. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368(6491):eabb6936. doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watson J., Whiting P.F., Brush J.E. Interpreting a covid-19 test result. BMJ. 2020;369:m1808. doi: 10.1136/bmj.m1808. [DOI] [PubMed] [Google Scholar]
- 7.Onuki T., Nakahara S., Fujita T., Miyake Y., Sakamoto T. End-of-life care provided in emergency medical system in Japan. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.07.069. (in press) [DOI] [PubMed] [Google Scholar]
- 8.Tokyo Metropolitan Government. Updates on COVID-19 in Tokyo. 2020. https://stopcovid19.metro.tokyo.lg.jp/en (Accessed 5 October 2020).
- 9.Task force on disaster and emergency medical care system in the Tokyo Olympic and Paralympic games. Heatstroke Jpn Soc Emerg Med. 2018 http://2020ac.com/documents/ac/04/2/4/2020AC_JSEM_heatstroke,ver1.1_20191010.pdf (Accessed 19 November 2020). in Japanese. [Google Scholar]
- 10.The Academic Consortium on Emergency Medical Service and Disaster Response Plan during the Tokyo Olympic and Paralyimpic Games in 2020. Proposal for constructing medical and first responding system in event-site during the Tokyo Olympic and Paralympic games in 2020. 2018 http://2020ac.com/documents/acEn/05/1/4/2020AC_site_proposal_EN_20180712.pdf (Accessed 19 November 2020).