Abstract
Background:
Although studies have demonstrated relations between obesity and incident asthma, little is known about the association of obesity with acute severity in adults hospitalized for asthma exacerbation.
Objectives:
To investigate the association of obesity with acute severity of asthma exacerbation.
Methods:
This is a retrospective cohort study using population-based data of geographically-diverse eight US states from 2010 through 2013. We included adults (age 18-54 years) hospitalized for asthma exacerbation. The outcome measures were markers of acute severity – use of mechanical ventilation (defined by non-invasive positive pressure ventilation [NIPPV] and/or invasive mechanical ventilation) and hospital length-of-stay (LOS). To determine the association of obesity with each outcome, we fit multivariable models adjusting for patient-level confounders (e.g., age, sex, race/ethnicity, primary insurance, quartiles for household income, residential status, and comorbidities) and potential patient clustering within hospitals.
Results:
Among the 72,086 patients hospitalized for asthma exacerbation, 24% were obese. Obesity was associated with a significantly higher risk of any mechanical ventilation use (8.3% vs. 5.0%; adjusted OR 1.77; 95%CI 1.63-1.92; P<0.001) driven by the higher risk of NIPPV use (7.2% vs. 3.4%; adjusted OR 2.14; 95%CI 1.96-2.35; P<0.001). Likewise, obese patients were more likely to have a hospital LOS of ≥3 days compared to non-obese patients (59.4% vs. 46.5%; adjusted OR 1.37; 95%CI 1.32-1.43; P<0.001). These findings were consistent with stratifications by age, sex, and race/ethnicity.
Conclusions:
In this population-based study of adults hospitalized for asthma exacerbation, obesity was associated with higher acute severity.
Keywords: asthma, adults, obesity, epidemiology, acute severity, hospitalization
INTRODUCTION
Asthma and obesity are major health problems, with a significant impact on the US healthcare system. The prevalence of asthma remains high, affecting 8% (18 million) of American adults.1 In addition, the burden of asthma-related healthcare utilization is substantial – approximately 385,000 annual hospitalizations with $2.3 billion direct cost each year.2 In parallel, the US has also experienced an obesity epidemic.3 It is anticipated that there will be a 33% increase in obesity prevalence over the next two decades.4
The literature has linked obesity to incident asthma5 and chronic morbidity (e.g., suboptimal asthma control, frequent exacerbations,6 and increased use of oral corticosteroids7,8). By contrast, only a few studies have examined the relations between obesity and acute asthma severity in adults.9-12 Studies of emergency department patients with asthma exacerbation have reported that, in obese adults, the risk of hospitalization – a marker for acute severity – is no different12,13 or higher9,10 than non-obese patients. However, the inferences may have been limited by the small sample sizes, confounding, and potential issues of generalizability. Despite the clinical and public importance of asthma exacerbation, the relation of obesity with in-hospital acute severity in adults remains largely unclear.
In this context, we used large, population-based, all-payer databases from eight US states to investigate the association of obesity with the markers for acute severity and in-hospital mortality in adults hospitalized for asthma exacerbation. Specifically, we hypothesized a priori that obese adults hospitalized for asthma exacerbation have higher acute severity (defined by the use of mechanical ventilations and hospital length-of-stay [LOS]) when compared to non-obese patients.
METHODS
Study Design and Setting
We performed a retrospective cohort study using the Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SIDs) from eight racially/ethnically- and geographically-diverse US states (Arkansas, California, Florida, Iowa, Nebraska, New York, Utah and Washington) from January 2010 through December 2013. The HCUP is the largest administrative longitudinal healthcare databases containing all-payer encounter-level information in the US. It is managed by the Agency for Healthcare Research and Quality and developed through a federal-state-industry partnership. The HCUP SIDs include all inpatient discharge records, regardless of source or disposition, from all acute care, non-federal, general, and other specialty hospitals within the states. Additional information of HCUP SID can be found elsewhere.14 The eight states were selected considering their geographic distribution and high data quality. The study period was chosen based on the availability of databases. This study was approved by the institutional review board of Massachusetts General Hospital.
Study Population
We included all adult patients (age 18-54 years) who had an unplanned hospitalization with a principal diagnosis of asthma, defined by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code of 493.xx.9 We included only the first hospitalization for asthma exacerbation for each patient during the study period. We excluded patients who were underweight (defined as ICD-9-CM codes: 783.2, 783.21, 783.22, and v85.0)15 as these patients may represent a unique phenotype compared with normal or overweight counterparts.16,17 Additionally, we excluded patients who were aged ≥55 years, due to the difficulty of distinguishing asthma from chronic obstructive pulmonary disease (COPD),9 and those who left hospital against medical advice.
Measurements
The databases include patient characteristics such as demographics (age, sex, race/ethnicity), primary insurance type, quartiles for estimated median household income, patient residence, ICD-9-CM diagnoses, patient comorbidities, procedures, hospital course, and disposition. Quartile classifications of estimated median household income of residents were based on the patient’s ZIP code. Patient comorbidities were measured by the Elixhauser comorbidity measures,11,18 a method of identifying comorbidities based on the ICD-9-CM diagnoses. The residential status was defined according to the National Center for Health Statistics.
Primary Exposure
The primary exposure was obesity, as defined by ICD-9-CM diagnosis codes of 278.00, 278.01, v85.31-v85.39, and v85.41-85.45.19-21 These ICD-9-CM codes have a high specificity and positive predictive value to identify obesity (both >90%).22
Outcome Measures
The primary outcome measures were markers of acute severity – the use of mechanical ventilation (defined by non-invasive positive pressure ventilation [NIPPV] and/or invasive mechanical ventilation) and hospital LOS. The secondary outcome measure was in-hospital mortality during the hospitalization for asthma exacerbation. The use of NIPPV was identified by ICD-9-CM procedure code 93.90; the use of invasive mechanical ventilation was identified by the codes of 96.04 and 96.70-96.72.23
Statistical Analysis
We compared the patient characteristics between the obesity and non-obesity groups by using chi-squared and Wilcoxon signed rank test as appropriate. To examine the association between obesity and each outcome, we fit unadjusted and adjusted logistic regression models for each of the binomial responses with the use of generalized estimating equations accounting for potential clustering of patients within hospitals. In the primary analysis, we modeled hospital LOS as a binomial response based on the median LOS (i.e., ≤2 days vs. ≥3 days). The cutoff value of 3 days was decided based on previous literature of patients hospitalized for asthma exacerbation where the overall mean hospital LOS being 2.7 days.24 Additionally, the overall median LOS was 3 days in our data. In the adjusted models, we adjusted for age, sex, race/ethnicity, primary insurance, quartiles for household income, residential status, patient comorbidities (29 Elixhauser comorbidity measures18 and arrhythmia11), hospital state, and calendar year. A set of potential confounders was chosen a priori based on clinical plausibility and a priori knowledge.
To examine the robustness of inferences, we performed series of sensitivity analyses. First, we repeated the analysis with stratification by age (<40 and ≥40 years), sex, and race/ethnicity (Non-Hispanic white, Non-Hispanic black, and Hispanic). Next, to examine the association between obesity and hospital LOS as a count variable, we fit unadjusted and adjusted negative binominal regression models with the use of generalized estimating equations. This model has advantages of need not to define an arbitrary cutoff point of LOS and accounts for overdispersion of data. Finally, to estimate the average causal effect of obesity on each outcome, we used stabilized inverse probability weighting (stabilized IPW).25 Weighting the inverse probability to have an exposure (obesity) creates a synthetic sample where the exposure becomes independent from measured baseline covariates. Consequently, in the synthetic sample, obese and non-obese individuals become exchangeable. While conventional IPW may have a greater variability of the estimated effects in subjects with a very low or high probability score, stabilized IPW enables us to directly estimate both the main effect and variance from conventional regression models.25 All analyses were performed by STATA 14.0 (STATA Corp, College Station, TX). All P values were two-tailed and considered statistically significant with P<0.05.
RESULTS
We identified 72,086 patients hospitalized for asthma exacerbation in the eight US states from January 2010 through December 2013. Overall, the median age was 43 years (IQR, 33-49 years), 70.2% were female, and 44.7% were non-Hispanic white. Among these, 17,479 patients (24.3%) were obese. The patient characteristics differed by obesity status. For example, obese patients were more likely to be female, Medicare beneficiaries, and living in lower household income areas compared to non-obese patients (all P<0.001). Additionally, obese patients were more likely to have several comorbidities, such as congestive heart failure, depression, and diabetes (all P<0.001), compared to non-obese patients.
Figure 1 illustrates the unadjusted and adjusted associations between obesity and each outcome. Obesity was associated with a significantly higher risk of overall mechanical ventilation use (8.3% vs. 5.0%; unadjusted OR 1.89; 95% CI 1.76-2.03; P<0.001). This association remained significant after adjusting for patient-level potential confounders (age, sex, race/ethnicity, primary insurance, quartiles for household income, residential status, patient comorbidities, hospital state, and calendar year) and potential clustering of patients within hospitals. When dividing overall mechanical ventilation use into NIPPV and invasive mechanical ventilation, obesity was associated with a significantly higher risk of NIPPV use in both unadjusted (7.2% vs. 3.4%; unadjusted OR 2.53; 95% CI 2.32-2.75; P<0.001) and adjusted (adjusted OR 2.14; 95% CI 1.96-2.35; P<0.001) models. There was no statistically significant association with risk of invasive mechanical ventilation use in the adjusted model (P=0.12). As for hospital LOS, obese patients were more likely to have a hospital LOS of ≥3 days compared to non-obese patients (59.4% vs. 46.5%; adjusted OR 1.37; 95% CI 1.32-1.43; P<0.001). The number of asthma deaths was low (n=116), which limited statistical power, but, there was no significant difference in in-hospital mortality between obesity and non-obesity groups (0.15% vs. 0.16%, respectively; P=0.97).
Figure 1. Unadjusted and adjusted associations of obesity with acute severity markers of asthma exacerbation and in-hospital mortality.
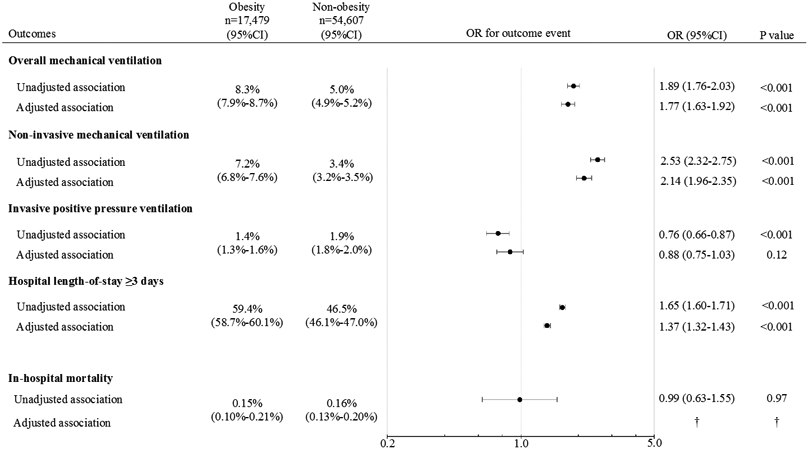
In patients hospitalized for asthma exacerbation, obese patients were more likely to have makers of higher acute severity, including any mechanical ventilation use, non-invasive mechanical ventilation use, and hospital length-of-stay of ≥3 days, when compared to non-obesity. These associations remained significant after adjusting for the potential confounders and potential clustering within the hospitals. The number of asthma deaths was low (n=116), which limited statistical power, but there was no significant association between obesity and in-hospital mortality.
Abbreviations: CI, confidence interval; OR, odds ratio
† Adjusted model was not constructed because of the relatively few number of in-hospital mortality (n=116)
In the sensitivity analyses, these results persisted with stratification by age, sex, and race/ethnicity (Supplemental Table 1) except for a lower risk of invasive mechanical ventilation use among obese men. While there were some statistically significant interactions of obesity with age and sex in the setting of large sample size (Supplemental Table 2), there was no substantial heterogeneity (or clinically meaningful interactions) in the observations across the age, sex, and race/ethnicity strata. Likewise, the associations were also consistent across the median household income and patient residence strata (Supplemental Table 3). Additionally, consistent with the primary analysis, the analysis modeling hospital LOS as a count variable (Supplemental Table 4) also showed that obese patients had a significantly longer hospital LOS, corresponding to a 24% increase (95%CI 22%-27% increase) in the unadjusted model and 13% increase (95%CI 11%-16% increase) in the adjusted model. Lastly, in the analysis using the stabilized IPW method, the results were consistent with the primary analysis, suggesting the causal association of obesity with acute severity of asthma exacerbation (Supplemental Table 5).
DISCUSSION
By analyzing population-based data from 72,086 patients hospitalized for asthma exacerbation in eight US states, we found that obese patients had significantly higher acute severity, including overall mechanical ventilation use and longer hospital LOS, when compared to non-obese patients. In contrast, there was no significant difference in in-hospital mortality between obese and non-obese patients although the number of asthma deaths was very low, which limited statistical power. These associations were consistent across the several sensitivity analyses with different statistical assumptions, including stabilized IPW. To the best of our knowledge, this is the first study that has investigated the relations of obesity with acute severity in adults hospitalized for asthma exacerbation.
Consistent with our inferences, within the limited literature, studies in the emergency department setting have reported the association of obesity and higher acute severity.9,10 For example, a US-based multicenter chart-review study of 1,227 emergency department adult patients with asthma exacerbation reported that obesity was associated with a higher risk of hospitalization compared to non-obese adults.9 Similarly, another single-center study of 426 adults with asthma exacerbation in Uruguay also reported significant obesity-hospitalization risk associations.10 Likewise, an analysis of administrative data of US children (aged 2-18 years) hospitalized for asthma exacerbation demonstrated that obesity is associated with a higher risk of mechanical ventilation use and longer hospital LOS.26 In addition, the literature of all-cause hospitalizations has also documented that obese individuals have longer hospital LOS through an increased prevalence of comorbidities, complications, and longer recovery.27,28 Our study corroborates these prior studies, and extends them by demonstrating, in a large population-based dataset, the robust association between obesity and acute severity in patients hospitalized for asthma exacerbation.
The underlying mechanism(s) of the observed obesity-acute severity relation warrants investigation. The literature has linked obesity to increased systemic inflammation by adipocyte-derived pro-inflammatory mediators (e.g., leptin),29-31 increased airway obstruction and inflammation,32-34 decreased corticosteroid responsiveness,35-39 altered gut microbiome modulating host immune response,40 obesity-associated restrictive ventilatory patterns and reduced expiratory reserve volume,41 and higher prevalence of comorbidities (e.g., gastroesophageal reflux). Prior studies of bariatric surgery – the most effective weight reduction measure – and asthma have shown that bariatric surgery improves airway hyperresponsiveness in obese asthmatics,42 and that bariatric surgery reverses the obesity-related increased pro-inflammatory mediator profiles,29 both supporting the obesity-asthma morbidity causal link. Each of these mechanisms may affect this particular population to develop altered pulmonary pathophysiology and higher acute severity resulting in higher use of mechanical ventilation and longer LOS.43,44 Interestingly, our study showed no significant association between obesity and the risk of invasive mechanical ventilation use even with sufficient statistical power (1,303 outcome events). This observation might be explained, at least in part, by the possibility that clinicians were more reluctant to attempt tracheal intubations on obese patients because obesity is a known risk factor for difficult intubation and extubation.45-48
We found no significant associations between obesity and in-hospital mortality despite the observed obesity-acute severity association. While a study of adults (aged >40 years) hospitalized with several conditions (e.g., asthma, cardiovascular diseases, cancer) reported that a higher body mass index (BMI) was associated with an increased risk of in-hospital mortality,49 a meta-analysis of 17 studies has shown that obesity is associated with favorable survival outcomes in other respiratory conditions, such as COPD.50 This apparent discrepancy in the literature might be partially attributable to the differences in study population, study designs, settings, or any combination of these factors. Alternatively, a limited statistical power from the low rate of in-hospital mortality among obese and non-obese patients in the present study (0.15% vs. 0.16%) may be an explanation for not detecting a statistically significant difference in this outcome measure. The potential protective effect of obesity on asthma merits further research.
POTENTIAL LIMITATIONS
The study has several potential limitations. First, the lack of information on BMI may have underestimated the prevalence of obesity. The sensitivity of ICD-9-CM codes for identifying obesity is shown to be poor,51,52while the specificity and positive predictive value for identifying obesity are both ≥90%.22 It is possible that those classified as obese had a very high BMI, and that our inferences of obese patients having a higher acute severity may not be generalizable to patients with mild-to-moderate obesity. Second, as with any observational studies, the observed associations may be confounded by unmeasured factors, such as smoking status, chronic severity of asthma, and institutional variability in resource use. Additionally, the observed associations between obesity and acute severity markers of asthma exacerbation remained significant after accounting for patient clustering at the hospital-level. Further, the significant associations persisted in the stabilized IPW, supporting causality in the association of interest. Third, the studied data were not a random sample of the entire population in the US. However, the data were racially/ethnically- and geographically-diverse. In addition, the eight states together represent approximately 30% of the US population53, thereby supporting the generalizability of our inferences. Finally, as our study sample consisted of patients hospitalized for asthma exacerbation, our inferences may not be generalizable to patients with less severe asthma exacerbations. However, our findings remain highly relevant to the population of approximately 400,000 US adults hospitalized for asthma each year, involving high morbidity and healthcare utilization.2
CONCLUSIONS
By analyzing population-based data from 72,086 patients hospitalized for asthma exacerbation, we found that obese patients were more likely to have a higher acute severity – i.e., overall mechanical ventilation use and a longer hospital LOS – in comparison with non-obese patients. These associations persisted after adjusting for potential confounders and across the sensitivity analyses with different statistical assumptions. Our findings should facilitate further research into the mechanisms underlying the observed obesity-acute severity link to develop therapeutic interventions in this high-risk population. Lastly, our observations also underscore the importance of continued public health campaigns against obesity, which might curb asthma-related healthcare utilization.
Supplementary Material
Table 1.
Characteristics of patients hospitalized for asthma exacerbation, according to obesity status
| Obesity | Non-obesity | ||
|---|---|---|---|
| Characteristics | n=17,479 (24.3%) |
n=54,607 (75.7%) |
P value |
| Age (year), median (IQR) | 45 (37-50) | 43 (32-49) | <0.001 |
| Female sex | 13,798 (79.0) | 36,586 (67.3) | <0.001 |
| Race/ethnicity | <0.001 | ||
| Non-Hispanic white | 7,667 (45.3) | 23,199 (44.5) | |
| Non-Hispanic black | 5,154 (30.4) | 14,154 (27.2) | |
| Hispanic | 3,225 (19.1) | 10,855 (20.8) | |
| Others | 887 (5.2) | 3,877 (7.4) | |
| Primary health insurance | <0.001 | ||
| Medicare | 3,030 (17.4) | 6,000 (11.0) | |
| Medicaid | 6,387 (36.6) | 18,271 (33.5) | |
| Private | 5,069 (29.0) | 17,399 (31.9) | |
| No insurance | 2,033 (11.6) | 9,214 (16.9) | |
| No charge | 333 (1.9) | 1,208 (2.2) | |
| Others | 613 (3.5) | 2,489 (4.6) | |
| Median household income quartile | <0.001 | ||
| 1 (lowest) | 6,921 (41.4) | 19,408 (37.8) | |
| 2 | 4,161 (24.9) | 12,691 (24.7) | |
| 3 | 3,497 (20.9) | 11,363 (22.1) | |
| 4 (highest) | 2,125 (12.7) | 7,940 (15.5) | |
| Patient residence | 0.90 | ||
| Metropolitan | 16,148 (92.7) | 50,369 (92.7) | |
| Non-metropolitan | 1,270 (7.3) | 3,978 (7.3) | |
| Selected comorbidities* | |||
| Congestive heart failure | 1,767 (10.1) | 1,766 (3.2) | <0.001 |
| Depression | 3,097 (17.7) | 6,941 (12.7) | <0.001 |
| Diabetes | 5,915 (33.8) | 6,734 (12.3) | <0.001 |
| Drug abuse | 1,064 (6.1) | 4,835 (8.9) | <0.001 |
| Hypertension | 9,292 (53.2) | 15,421 (28.2) | <0.001 |
| Renal failure | 644 (3.7) | 1,017 (1.9) | <0.001 |
| Hospital state | <0.001 | ||
| Arkansas | 471 (2.7) | 1,739 (3.2) | |
| California | 3,287 (18.8) | 8,753 (16.0) | |
| Florida | 6,516 (37.3) | 16,544 (30.3) | |
| Iowa | 382 (2.2) | 1,147 (2.1) | |
| Nebraska | 199 (1.1) | 836 (1.5) | |
| New York | 5,286 (30.2) | 21,296 (39.0) | |
| Utah | 171 (1.0) | 930 (1.7) | |
| Washington | 1,167 (6.87) | 3,362 (6.2) | |
| Hospitalization year | 0.054 | ||
| 2010 | 19,828 (36.3) | 6,301 (36.1) | |
| 2011 | 15,282 (28.0) | 4,865 (27.8) | |
| 2012 | 10,511 (19.3) | 3,286 (18.8) | |
| 2013 | 8,986 (16.5) | 3,027 (17.3) |
Data are shown as n (%) unless otherwise specified
Abbreviation: IQR, interquartile range
Selected from 29 Elixhauser comorbidity measures and arrhythmia
Acknowledgements:
S.K.L was supported by grants from World Bank and Kamiyama Foundation. A.H. was supported by grants from Fulbright Scholarship.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Funding: This study was supported by the grant R01 HS-023305 (Camargo) from the Agency for Healthcare Research and Quality (Rockville, MD). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Abbreviations:
- BMI
body mass index
- COPD
chronic obstructive pulmonary disease
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- IPW
Inverse probability weighting
- LOS
length-of-stay
- NIPPV
non-invasive positive pressure ventilation
- OR
odds ratio
- SID
State Inpatient Databases
Footnotes
Conflict of Interest: Dr. Camargo has provided asthma-related consulting services to AstraZeneca, GlaxoSmithKline, Novartis, and Teva. Dr. Hasegawa has received grants for asthma-related research from Novartis and Teva. The other authors have no relevant financial relationships to disclose.
This article has supplement data, which are accessible in the online repository at http://www.jaci-inpractice.org
REFERENCES
- 1.Most recent asthma data. Center for Disease Control and Prevention; 2015; https://www.cdc.gov/asthma/most_recent_data.htm. Accessed May 24, 2017. [Google Scholar]
- 2.HCUPNet. US Department of Health and Human Services. Agency for Healthcare Research and Quality; http://hcupnet.ahrq.gov/. Accessed May 24, 2017. [Google Scholar]
- 3.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015(219):1–8. [PubMed] [Google Scholar]
- 4.Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563–570. [DOI] [PubMed] [Google Scholar]
- 5.Camargo CA Jr., Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159(21):2582–2588. [DOI] [PubMed] [Google Scholar]
- 6.Schatz M, Zeiger RS, Zhang F, Chen W, Yang SJ, Camargo CA Jr., Overweight/obesity and risk of seasonal asthma exacerbations. J Allergy Clin Immunol Pract. 2013;1(6):618–622. [DOI] [PubMed] [Google Scholar]
- 7.Quinto KB, Zuraw BL, Poon KY, Chen W, Schatz M, Christiansen SC. The association of obesity and asthma severity and control in children. J Allergy Clin Immunol. 2011;128(5):964–969. [DOI] [PubMed] [Google Scholar]
- 8.Taylor B, Mannino D, Brown C, Crocker D, Twum-Baah N, Holguin F. Body mass index and asthma severity in the national asthma survey. Thorax. 2008;63(1):14–20. [DOI] [PubMed] [Google Scholar]
- 9.Hasegawa K, Tsugawa Y, Lopez BL, Smithline HA, Sullivan AF, Camargo CA Jr. Body mass index and risk of hospitalization among adults presenting with asthma exacerbation to the emergency department. Ann Am Thorac Soc. 2014;11(9):1439–1444. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigo GJ, Plaza V. Body mass index and response to emergency department treatment in adults with severe asthma exacerbations: a prospective cohort study. Chest. 2007;132(5):1513–1519. [DOI] [PubMed] [Google Scholar]
- 11.Thompson NR, Fan Y, Dalton JE, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015;53(4):374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeh KH, Skowronski ME, Coreno AJ, et al. Impact of obesity on the severity and therapeutic responsiveness of acute episodes of asthma. J Asthma. 2011;48(6):546–552. [DOI] [PubMed] [Google Scholar]
- 13.Thomson CC, Clark S, Camargo CA Jr., Investigators M. Body mass index and asthma severity among adults presenting to the emergency department. Chest. 2003;124(3):795–802. [DOI] [PubMed] [Google Scholar]
- 14.Overview of the State Inpatient Databases (SID). Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; https://www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed May 24, 2017. [Google Scholar]
- 15.Li TY, Rana JS, Manson JE, et al. Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Circulation. 2006;113(4):499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lambert AA, Putcha N, Drummond MB, et al. Obesity is associated with increased morbidity in moderate to severe COPD. Chest. 2017;151(1):68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fox KM, Brooks JM, Gandra SR, Markus R, Chiou CF. Estimation of cachexia among cancer patients based on four definitions. J Oncol. 2009;2009:693458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 19.Goto T, Hirayama A, Faridi MK, Camargo CA Jr., Hasegawa K. Association of bariatric surgery with risk of infectious diseases: A self-controlled case series analysis. Clin Infect Dis. 2017. [DOI] [PubMed] [Google Scholar]
- 20.Hasegawa K, Tsugawa Y, Chang Y, Camargo CA Jr. Risk of an asthma exacerbation after bariatric surgery in adults. J Allergy Clin Immunol. 2015;136(2):288–294 e288. [DOI] [PubMed] [Google Scholar]
- 21.Shimada YJ, Tsugawa Y, Brown DF, Hasegawa K. Bariatric Surgery and Emergency Department Visits and Hospitalizations for Heart Failure Exacerbation: Population-Based, Self-Controlled Series. J Am Coll Cardiol. 2016;67(8):895–903. [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43(4):1424–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindenauer PK, Stefan MS, Shieh MS, Pekow PS, Rothberg MB, Hill NS. Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Intern Med. 2014;174(12):1982–1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krishnan V, Diette GB, Rand CS, et al. Mortality in patients hospitalized for asthma exacerbations in the United States. Am J Respir Crit Care Med. 2006;174(6):633–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okubo Y, Nochioka K, Hataya H, Sakakibara H, Terakawa T, Testa M. Burden of obesity on pediatric inpatients with acute asthma exacerbation in the United States. J Allergy Clin Immunol Pract. 2016;4(6):1227–1231. [DOI] [PubMed] [Google Scholar]
- 27.Hauck K, Hollingsworth B. The impact of severe obesity on hospital length of stay. Med Care. 2010;48(4):335–340. [DOI] [PubMed] [Google Scholar]
- 28.Zizza C, Herring AH, Stevens J, Popkin BM. Length of hospital stays among obese individuals. Am J Public Health. 2004;94(9):1587–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sideleva O, Suratt BT, Black KE, et al. Obesity and asthma: an inflammatory disease of adipose tissue not the airway. Am J Respir Crit Care Med. 2012;186(7):598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dixon AE, Johnson SE, Griffes LV, et al. Relationship of adipokines with immune response and lung function in obese asthmatic and non-asthmatic women. J Asthma. 2011;48(8):811–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strunk RC, Colvin R, Bacharier LB, et al. Airway obstruction worsens in young adults with asthma who become obese. J Allergy Clin Immunol Pract. 2015;3(5):765–771 e762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peters JI, McKinney JM, Smith B, Wood P, Forkner E, Galbreath AD. Impact of obesity in asthma: evidence from a large prospective disease management study. Ann Allergy Asthma Immunol. 2011;106(1):30–35. [DOI] [PubMed] [Google Scholar]
- 34.Fantuzzi G Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005;115(5):911–919; quiz 920. [DOI] [PubMed] [Google Scholar]
- 35.Parameswaran K, Todd DC, Soth M. Altered respiratory physiology in obesity. Can Respir J. 2006;13(4):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stream AR, Sutherland ER. Obesity and asthma disease phenotypes. Curr Opin Allergy Clin Immunol. 2012;12(1):76–81. [DOI] [PubMed] [Google Scholar]
- 37.Peters-Golden M, Swern A, Bird SS, Hustad CM, Grant E, Edelman JM. Influence of body mass index on the response to asthma controller agents. Eur Respir J. 2006;27(3):495–503. [DOI] [PubMed] [Google Scholar]
- 38.Sutherland ER, Lehman EB, Teodorescu M, Wechsler ME, National Heart L, Blood Institute's Asthma Clinical Research N. Body mass index and phenotype in subjects with mild-to-moderate persistent asthma. J Allergy Clin Immunol. 2009;123(6):1328–1334 e1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Forno E, Lescher R, Strunk R, et al. Decreased response to inhaled steroids in overweight and obese asthmatic children. J Allergy Clin Immunol. 2011;127(3):741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gibson PG. Obesity and asthma. Ann Am Thorac Soc. 2013;10 Suppl:S138–142. [DOI] [PubMed] [Google Scholar]
- 41.Franssen FM, O'Donnell DE, Goossens GH, Blaak EE, Schols AM. Obesity and the lung: 5. Obesity and COPD. Thorax. 2008;63(12):1110–1117. [DOI] [PubMed] [Google Scholar]
- 42.Dixon AE, Pratley RE, Forgione PM, et al. Effects of obesity and bariatric surgery on airway hyperresponsiveness, asthma control, and inflammation. J Allergy Clin Immunol. 2011;128(3):508–515 e501-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dixon AE, Holguin F, Sood A, et al. An official american thoracic society workshop report: obesity and asthma. Proc Am Thorac Soc. 2010;7(5):325–335. [DOI] [PubMed] [Google Scholar]
- 44.Suratt BT, Ubags NDJ, Rastogi D, et al. An official American Thoracic Society workshop report: Obesity and metabolism. An emerging frontier in lung health and disease. Ann Am Thorac Soc. 2017;14(6):1050–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92(5):1229–1236. [DOI] [PubMed] [Google Scholar]
- 46.Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists task force on management of the difficult airway. Anesthesiology. 2013;118(2):251–270. [DOI] [PubMed] [Google Scholar]
- 47.Juvin P, Lavaut E, Dupont H, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003;97(2):595–600, table of contents. [DOI] [PubMed] [Google Scholar]
- 48.Cavallone LF, Vannucci A. Review article: Extubation of the difficult airway and extubation failure. Anesth Analg. 2013;116(2):368–383. [DOI] [PubMed] [Google Scholar]
- 49.Akinyemiju T, Meng Q, Vin-Raviv N. Association between body mass index and in-hospital outcomes: Analysis of the nationwide inpatient database. Medicine (Baltimore). 2016;95(28):e4189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo Y, Zhang T, Wang Z, et al. Body mass index and mortality in chronic obstructive pulmonary disease: A dose-response meta-analysis. Medicine (Baltimore). 2016;95(28):e4225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Golinvaux NS, Bohl DD, Basques BA, Fu MC, Gardner EC, Grauer JN. Limitations of administrative databases in spine research: a study in obesity. Spine J. 2014;14(12):2923–2928. [DOI] [PubMed] [Google Scholar]
- 52.Martin BJ, Chen G, Graham M, Quan H. Coding of obesity in administrative hospital discharge abstract data: accuracy and impact for future research studies. BMC Health Serv Res. 2014;14:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.United States Census Bureau. Annual estimates of the resident population for the United States, regions, states, and Puerto Rico: April 1, 2010 to July 1, 2016 (NST-EST2016-01). https://www.census.gov/data/tables/2016/demo/popest/state-total.html. Accessed Sep 15, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


