Abstract
Basicervical femoral neck fracture is an uncommon fracture that accounts for only 1.8% of all proximal femoral fractures. Previous studies have recommended that the choice of implant to treat this fracture should be similar to that of intertrochanteric fracture. However, in previous studies on basicervical fractures, the definition and treatment results of these fractures were different, and there were also debates on the implant that had to be used. Therefore, the purpose of this study was to review the studies that performed surgical treatment of basicervical femoral fractures and to assess the definition of basicervical fracture, the use of implants, and failure rates and clinical results. Study selection was based on the following inclusion criteria: (1) treatment outcome for basicervical femoral neck fracture was reported; and (2) dynamic hip screw, proximal femoral nail, or multiple screw fixation was used as treatment. PubMed Central, OVID MEDLINE, Cochrane Collaboration Library, Web of Science, EMBASE, and AHRQ databases were searched to identify relevant studies published up to March, 2020 with English language restriction. A total of 15 studies were included in this study. Differences were found in the definition of basicervical fracture, treatment results, rehabilitation protocol, and fixation failure rate. Definitions and treatment methods for basicervical fractures varied, and treatment outcomes also differed among the enrolled studies. Further research is needed that would be restricted to those fractures that conform to the definition of basicervical fracture.
Keywords: Femoral neck fractures, Fracture fixation, Hip fracture, Internal
INTRODUCTION
Basicervical femoral neck fractures are rare and account for just 1.8% of all proximal femoral fractures1). The line of a basicervical fracture goes through the base of the femoral neck at its junction with the intertrochanteric region2). Previous studies have recommended that the choice of implant to treat this fracture should be similar to that of intertrochanteric femoral fracture3). However, due to the anatomical location of the fracture line, the proximal fragment in basicervical fractures has no muscular insertion, and unlike trochanteric fractures, these fractures lack cancellous interdigitation4). Thus, the basicervical femoral neck fractures are more instable than intertrochanteric fractures3).
Recently, proximal femoral nails (PFNs) became widely used for treating intertrochanteric fractures5,6). Various types of nail devices have been developed and used. However, Watson et al.7) have suggested that PFNs are unsuitable for treatment of basicervical femoral neck fractures. They reported that basicervical fractures healed without complications only in 5 among 11 patients, whereas 6 patients had fixation failure. In addition, their study did not support a suggestion that PFNs have biomechanical advantages over dynamic hip screws (DHSs). On the other hand, Hu et al.8) treated 32 patients with basicervical fractures using cephalomedullary hip nails, and there were no cut outs and clinical results were satisfactory.
To determine the best treatment strategy for basicervical fracture, we need to investigate the treatment methods and results of previous studies. However, even the same implant was used, different studies may reach different conclusions, which makes it difficult ascertain the choice of treatment option for these fractures. Also, the radiographs presented in some studies did not appear to match the definition of this fracture1,7,8).
Therefore, the purpose of this study was to assess previous studies that used surgical treatment of basicervical femoral fractures to review the definition of a basicervical fracture, the type of treatment implants, failure rates, and clinical results.
MATERIALS AND METHODS
1. Study Eligibility Criteria
Study selection was based on the following inclusion criteria: (1) treatment outcomes (such as radiologic fracture healing period, Harris hip score [HHS], union rate, implant failure, non-union, reoperation) for a basicervical femoral neck fracture were reported; and (2) DHS, PFN, or multiple screw fixation was used as treatment. Studies were excluded if they failed to meet the above criteria.
2. Search Methods for Identification of Studies
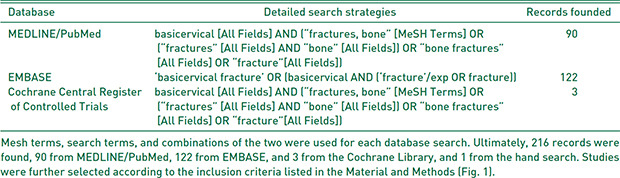
PubMed Central, OVID MEDLINE, Cochrane Collaboration Library, Web of Science, EMBASE, and AHRQ databases were searched to identify relevant studies published up to March 2020, with English language restriction. The following search terms were used: “basicervical” [All Fields] AND (“fractures, bone” [MeSH Terms] OR (“fractures” [All Fields] AND “bone” [All Fields]) OR “bone fractures” [All Fields] OR “fracture” [All Fields]) (Appendix). Manual search was also conducted for possibly related references. JIY, YC reviewed the titles, abstracts, and full texts of all potentially relevant studies independently, as recommended by the Cochrane Collaboration. Any disagreement was resolved by the fourth reviewer (HYK). We assessed the full text according to the inclusion criteria described above, and then selected eligible articles. The reviewers were not blinded to authors, institutions, or the publication.
3. Data Extraction
The following information was extracted from the included articles: authors, publication date, study design, study period, mean follow-up period, number of patients, mean age, definition of basicervical fracture, type of implants, outcome measurements, and ambulation protocol. Outcomes pooled in this analysis were radiologic fracture union time and HHS.
RESULTS
1. Search Results
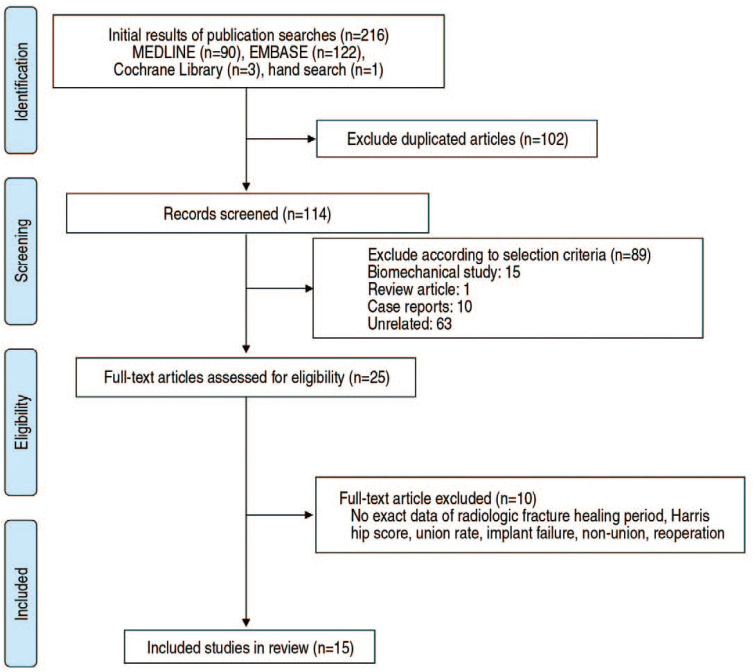
The initial search identified 432 references. However, 407 studies were excluded after screening the abstracts and titles. The remaining 25 studies underwent full-text review. Ten studies were further excluded. Details on the identification of relevant studies are shown in the flow chart of the study selection process (Fig. 1). Study design, study period, and the number of patients included in our study are summarized in Table 11,3,7,8,9,10,11,12,13,14,15,16,17,18,19).
Fig. 1. The flow chart of the study selection process.
Table 1. Study Design, Study Period, Demographic Data of Included Studies.
| Study | Design | Study period | Mean follow-up period (mo) | No. of patients | Sex (male/female) | Mean age (yr) |
|---|---|---|---|---|---|---|
| Watson et al.7) (2016) | Retrospective | 2011–2012 | 5 (2–8) | 11 | 5/6 | Not mentioned |
| TasyIkan et al.9) (2015) | Retrospective | 2006.1–2013.1 | 29.2±14.8 | 25 | 11/17 | 71±14.3 |
| Hu et al.8) (2013) | Retrospective | 2008.1–2010.6 | 28.3 (24–40) | 32 | 25/7 | 47.8 (25–71) |
| Massoud3) (2010) | Prospective | 2002.2–2007.2 | 12 | 13 | 9/4 | 68.9 (54–85) |
| Su et al.11) (2006) | Retrospective | 1992–2001 | >12 | 28 | 5/23 | 79±11 |
| Chen et al.1) (2008) | Prospective | 1992–2004 | 74.7 (24–150) | 269 | 112/157 | 73.8 (58–90) |
| Saarenpää et al.10) (2002) | Retrospective | 1989.1–1996.12 | 60 (24–120) | 30 | 11/19 | 75 in male/78 in female |
| Kuokkanen13) (1991) | Retrospective | 1977.1–1985.12 | 63 (21–111) | 6 | Not mentioned | 76.7±11.48 |
| Davis et al.12) (1990) | Retrospective | 1983.6–1985.5 | Not mentioned | 9 | Not mentioned | Not mentioned |
| Kweon et al.14) (2017) | Retrospective | 2012.7–2015.5 | 25.2 (24–31) | 15 | 6/9 | 78.14 (65–87) |
| Lee et al.15) (2018) | Retrospective | 2003.5–2016.3 | 28.2±18.6 | 69 | 17/52 | 81.3±6.6 |
| Guo et al.16) (2019) | Retrospective | 2015.1–2017.3 | 15 (12–21) | 14 | 4/10 | 67.6 (56–93) |
| Wang et al.17) (2019) | Retrospective | 2013.1–2017.2 | 22.5 | 52 | 13/39 | 75.1 (63–91) |
| Kim et al.18) (2020) | Retrospective | 2011–2014 | 26.4 (12–43.2) | 106 | 39/67 | 76.4 in DHS group/77.5 in CMN group |
| Yoo et al.19) (2019) | Retrospective | 2011.1–2016.6 | At least 12 months of follow-up | 185 | 48/137 | 78.5±7 in ITST nail, 79.5±7 in PFNA, 79.2±7.5 in Gamma |
DHS: dynamic hip screw, CMN: cephalomedullary nail, ITST: intertrochanteric/subtrochanteric, PFNA: proximal femoral nail antirotation.
2. Definition of Basicervical Fracture
Definitions of basicervical fracture described in the articles included in this study are summarized in Table 2. Basicervical femoral fractures in studies of Massoud3), Chen et al.1), and Kuokkanen13) were defined as extracapsular fractures. Five studies defined basicervical fracture as a 2-part fracture7,11,14,15,17). Davis et al.12) did not mention the definition of a basicervical femoral fracture. Hu et al.8) defined basicervical fracture as a particular type of trochanteric fracture in which the fracture line can be seen radiologically to run across close to the base of the femoral neck and its junction with the intertrochanteric region. Yoo et al.19) also mentioned that it is a variant of a trochanteric fracture and a partial capsular fracture.
Table 2. Definition of Basicervical Fracture in Each Studies.
| Study | Definition of basicervical fracture | Fracture classification |
|---|---|---|
| Watson et al.7) (2016) | Two-part fracture at the base of the femoral neck that was medial to the intertrochanteric line and exited above the lesser trochanter but was more lateral than a classic transcervical fracture. | OTA/AO: A3, B1, B2 |
| TasyIkan et al.9) (2015) | Fractures that did not extend to the trochanteric site and were at the joint of the femur neck and intertrochanteric site were considered to be basicervical fractures. | Not mentioned. |
| Hu et al.8) (2013) | Basicervical intertrochanteric fractures are a particular type of trochanteric fracture in which the fracture line can be seen radiologically to cross close to the base of the femoral neck and its junction with the intertrochanteric region. | Evans Jensen : IIA, IB, IIB, III |
| Massoud3) (2010) | Basicervical fracture, defined as an extracapsular fracture, through the base of the femoral neck at its junction with the intertrochanteric region, corresponding to the AO type B2.1 femoral neck at its junction with the intertrochanteric region. | OTA/AO B2.1 |
| Su et al.11) (2006) | Proximal femoral fractures through the base of the femoral neck at its junction with the intertrochanteric region. | OTA/AO B2.1 |
| Chen et al.1) (2008) | Basicervical neck fractures are extracapsular fractures just proximal to or along the intertrochanteric line. | Not mentioned. |
| Saarenpää et al.10) (2002) | Proximal femoral fractures through the base of the femoral neck at its junction with the intertrochanteric region. | Not mentioned. |
| Kuokkanen13) (1991) | Only distinctly extracapsular fractures of the neck of the femur were included, oblique transcervical fractures and fractures of the trochanteric region were excluded. | Not mentioned. |
| Davis et al.12) (1990) | Not mentioned. | Not mentioned. |
| Kweon et al.14) (2017) | Basicervical femoral fractures were defined as two-part fractures between the base of the femoral neck and the intertrochanteric region on computed tomography scans. | Not mentioned. |
| Lee et al.15) (2018) | 2-part fracture at the base of the femoral neck that was medial to the intertrochanteric line and exited above the lesser trochanter but was more lateral than a classic transcervical fracture. | Not mentioned. |
| Guo et al.16) (2019) | A basicervical femoral neck fracture, which is located at the junction between the femoral neck and intertrochanteric region. | Not mentioned. |
| Wang et al.17) (2019) | A two-part fracture and fracture line located at the base of the femoral neck that was medial to the intertrochanteric line and exited above the lesser trochanter but was more lateral than a classic transcervical fracture. | Not mentioned. |
| Kim et al.18) (2020) | Basicervical hip fracture of the proximal part of the femur defined as a two-part fracture at the base of the femoral neck that was medial to the intertrochanteric line, exiting above the lesser trochanter but was more lateral than a classic transcervical fracture. | Not mentioned. |
| Yoo et al.19) (2019) | Partial capsular fracture, which can be a variant of a trochanteric fracture. | OTA/AO: A1 |
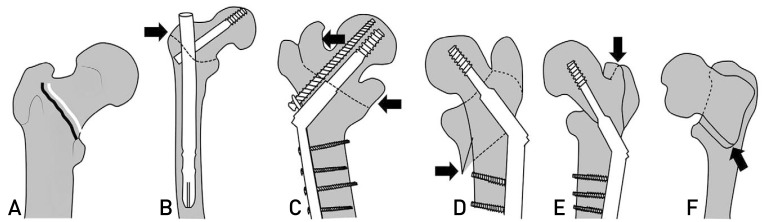
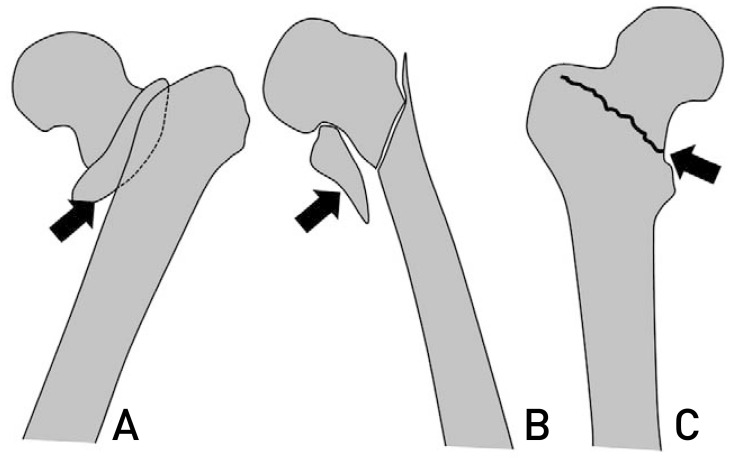
However, contrary to the definitions of basicervical fracture in some studies, fracture line in the radiographs before and after surgery presented in each study had a pattern involving the lesser or greater trochanter or disrupting the intertrochanteric line (Fig. 2)3,7,11,12,13). The radiographs of basicervical fractures presented by Yoo et al.19) and Hu et al.8) clearly involved the intertrochanteric area, in agreement with their definitions of basicervical fractures as a variant of the intertrochanteric fractures (Fig. 3). In other studies, the presented radiographs show fractures that did not invade the intertrochanteric line and are 2-part fractures (Fig. 3)14,15,16,17).
Fig. 2. The radiographs in included studies. (A) Normal bony structure of the proximal femoral head. The intertrochanteric line is shown in black and the line of the basicervical fracture in white. (B) Schematic figure depicting a radiograph in the study of Watson et al.7). The fracture line started in the inferior area of the intertrochanteric line (black arrow). (C) Schematic figure showed the radiograph in study of Massoud.3) The fracture line crossed the intertrochanteric line (black arrow). (D) Schematic figure depicting the radiograph in the study of Davis et al.12) The lesser trochanteric area was involved in the fracture (black arrow). (E) Schematic figure depicting the radiograph in the study of Kuokkanen.13) Fracture involved the greater trochanter (black arrow). (F) Schematic figure depicting the radiograph in the study of Su et al.11). The inferior area of the fracture line involved the intertrochanteric line (black arrow). Fractures not matching the definition of basicervical fracture.
Fig. 3. The radiographs in included studies. (A) Schematic figure depicting the radiograph in the study of Hu et al.8). Proximal fragment included part of the lesser trochanter (black arrow). (B) Schematic figure depicting the radiograph in the study of Yoo et al.19). The lesser trochanter fragment is displaced (black arrow). (C) Schematic figure depicting the radiograph in the study of Lee et al.15). They showed radiograph of a 2-part basicervical fracture (black arrow).
3. Implants
Implants used for basicervical femoral neck fracture treatment in the identified studies are summarized in Table 3. Eleven studies used cephalomedullary nails were used3,7,8,9,12,14,15,16,17,18,19), and 8 studies used DHS1,3,10,11,12,13,15,18). Only 1 study used cancellous screws3), and 5 studies compared different implants3,12,15,18,19). The types of cephalomedullary nails were a single screw, blade, and two integrated screws, and there were studies using additional anti-rotational cancellous screws for fixation with DHS. A very high failure rate was observed when cancellous screws were used3).
Table 3. Type of Implants in Each Studies.
| Study | Type of implant | Character | Antirotational effect |
|---|---|---|---|
| Watson et al.7) (2016) | CMN | No blade type, 1 cephalomedullary screw | − |
| TasyIkan et al.9) (2015) | PROFIN nails (TST Inc., Istanbul, Turkey) with 2 cephalomedullary screw | No blade type, 2 cephalomedullary screw | + |
| Hu et al.8) (2013) | PFNA (DePuy Synthes, Solothurn, Switzerland) | Blade type | − |
| Massoud3) (2010) | Gamma nail or DHS or cancellous screws | No blade type | −* |
| Su et al.11) (2006) | DHS+antirotational cancellous screw | No blade type | + |
| Chen et al.1) (2008) | DHS±antirotational cancellous screw | No blade type | ± |
| Saarenpää et al.10) (2002) | DHS-antirotational cancellous screw | No blade type | − |
| Kuokkanen13) (1991) | DHS | No blade type | − |
| Davis et al.12) (1990) | DHS or γ-nail | No blade type | − |
| Kweon et al.14) (2017) | Gamma3 CMN (Stryker, Kalamazoo, MI, USA) | No blade type | + |
| Lee et al.15) (2018) | DHS or PFNA (DePuy Synthes) | Blade type in CMN group | ± |
| Guo et al.16) (2019) | PFNA (DePuy Synthes) | Blade type | + |
| Wang et al.17) (2019) | PFNA (DePuy Synthes) | Blade type | + |
| Kim et al.18) (2020) | DHS or CMN (Gamma-3 nail (Stryker, Kiel, Germany), Zimmer natural nail (Zimmer, Warsaw, IN, USA), ITST nail (Zimmer), PFNA (DePuy Synthes), InterTAN nail (Smith-Nephew, Memphis, TN, USA) | Single screw type, blade type and two integrated screw type in CMN group | ± |
| Yoo et al.19) (2019) | ITST nail (Zimmer), PFNA (DePuy Synthes), Gamma 3 CMN (Stryker Trauma GmbH, Schoenkirchen, Germany) | Single screw type, blade type | ± |
CMN: cephallomedullary nail, PFNA: proximal femoral nail-antirotation, DHS: dynamic hip screw, ITST: intertrochanteric/subtrochanteric.
*Cancellous screw was excluded in this review due to high failure rate.
4. Radiologic Fracture-healing Period, Harris Hip Score, and Ambulation
Radiologic fracture-healing period, HHS, and ambulation status are summarized in Table 4. The reported healing period ranged from 8 to 24 weeks. Five studies that used HHS reported good results, with an average score of 80 or better1,3,9,16,17). Different protocols were used to start ambulation. In the study of Hu et al.8), partial weight bearing was permitted at 8 weeks postoperatively. In the study of Massoud3), patients were allowed to walk using crutches and toe touching until the absence of pain and a good callus was observed on radiographs.
Table 4. Radiologic Fracture Healing Time, Postoperative HHS, and Ambulation in Each Studies.
| Study | Radiologic fracture healing time (wk) | Mean HHS | Ambulation |
|---|---|---|---|
| Watson et al.7) (2016) | Not mentioned. | Not mentioned. | Immediate weight-bearing as tolerated. |
| TasyIkan et al.9) (2015) | 10.5 (8–14) | 81.2±21.3 | Mobilized with weight-bearing on postoperative day 1. |
| Hu et al.8) (2013) | 14.7 (8–24) | 86.5 (75–96) | The patients were permitted to get out of bed and sit in a wheelchair on the third postoperative day. Partial weight-bearing started about 8 weeks postoperatively. The actual time was determined by the extent of fracture healing. Weight-bearing was gradually increased as tolerated. |
| Massoud3) (2010) | 11.5 (9–15) | Not mentioned. | Patients were allowed to walk using crutches and toe touching until the absence of pain and a good callus had been observed on radiographs. Then, progressive weight bearing was started. However, if the reduction was considered as not good, partial weight bearing was allowed only when the callus bridged the fracture gap. |
| Chen et al.1) (2008) | 16.5 (14–24) | 80 (68–88) | From the first postoperative day, all patients started weight-bearing walking as tolerable with a walker. |
| Kweon et al.14) (2017) | 19.2 (12–40) | Not mentioned. | Sitting was allowed from the first postoperative day, and wheelchair usage and partial weight bearing was instructed between the 3rd and the 7th postoperative days depending on the degree of reduction, systemic condition and pain. Partial weight bearing with a walker was allowed from the 2nd postoperative week and full weight bearing from the 6th postoperative week. |
| Lee et al.15) (2018) | 28.2±18.6 | Not mentioned. | After surgery, a tolerable range of motion of the hip was immediately permitted, and wheelchair ambulation was started at two or three days postoperatively. Patients walked with protected weight-bearing and used assistive devices (wheelchair, walker, crutches, or cane) 3–10 days after the operation. As their walking ability improved, their assistive devices were changed appropriately by a physical therapist. |
| Guo et al.16) (2019) | Not mentioned. | 85.7±3.1 | The patients were encouraged to sit on the bed and exercise their lower limb muscles for the first 24 hours. Until 8 weeks postoperatively, the patients were encouraged to perform partial weight-bearing ambulation with assistance. After 8 weeks postoperatively, full weight-bearing ambulation was started at 20 kg with an incremental increase of 5 kg per week when evidence of complete fracture union was present. |
| Wang et al.17) (2019) | 19.6 (12–28) | 84.9 (65–99) | Not mentioned. |
| Yoo et al.19) (2019) | 18.7 (12–40) in ITST nail, 17.6 (12–24) in PFNA, 19.9 (12–36) in Gamma 3 CMN | Not mentioned. | Approximately 2–3 days postoperatively, when the patients could tolerate weight-bearing in a sitting position, the patients were asked to try to stand using a tilt table. Walking was allowed when the pain became tolerable. Restricted weight-bearing was taught and initiated by touching approximately 20 kg on a scale; the patients were allowed to walk using the parallel bar or rolling walker. Various weight-bearing training exercises were performed not based on the reduction or bone quality but only based on the subject’s pain level and medical condition. |
HHS: Harris hip score, ITST: intertrochanteric/subtrochanteric, PFNA: proximal femoral nail antirotation, CMN: cephalomedullary nail.
5. Treatment Results and Failures
Treatment results, including failures, are summarized in Table 5. Only 7 studies did not clearly define fracture collapse and failure of fixation3,7,11,15,16,17,19). Watson et al.7) reported fracture union rate (45%), implant failure rate (45%), and nonunion rate (5%). Su et al.11) reported that 75% patients had severe collapse. In a study by Lee et al.15), collapse occurred in 26.1% of the patients and the cut-out rate was 8.6%. On the other hand, there were no collapse, nonunion, or total hip arthroplasty conversion cases in 6 studies3,8,9,14,16,17).
Table 5. Last Follow-up Results of Each Studies.
| Study | Definition of failure | Union rate | Cutout or collapse | Nonunion | Reoperation |
|---|---|---|---|---|---|
| Watson et al.7) (2016) | Failure of fixation was defined as collapse of the fracture and movement of the position of the lag screw in the femoral head, or nonunion of the fracture (no sign of healing radiographically or clinically at 6 months postoperatively). | 5/11 | 5/11 | 1/11 | 3-arthroplasty 1-refuse 1-expire |
| TasyIkan et al.9) (2015) | Not mentioned. | 28/28 | 0 | 0 | 0 |
| Hu et al.8) (2013) | Not mentioned. | 28/28 | 0 | 0 | 0 |
| Massoud3) (2010) | Technical failures were defined as lag screw penetration or cut-out of the femoral head, excessive displacement, e.g., femoral shaft medialization, implant breakage or loosening, intra or postoperative femoral shaft fracture or non-union. Lag screw migration without femoral head penetration or cut-out was not regarded as a technical failure. Downward displacement of the proximal fragment without cut-outs or DRS (alone) penetration of the femoral head were not considered technical failures. | 13/13 | 0 | 0 | 0 |
| Su et al.11) (2006) | Fracture collapse was defined as the length of the protrusion of the compression screw from the lateral edge of the barrel relative to the entire length of the lag screw. | 24/28 | 21/28 | 1/28 | 2-hemiarthroplasty 1-implant removal 1-bone graft with screw fixation |
| Chen et al.1) (2008) | Not mentioned. | 263/269 | 2/269 | 4/269 | 4-bone graft with DHS change 2 cutout->THA |
| Saarenpää et al.10) (2002) | Not mentioned. | 16/19 | 1/19-cancellous screw cutout | 2/19-cancellous screw | 1-THA 1-remove 1-girdle stone |
| Kuokkanen13) (1991) | Not mentioned. | 5/6 | 0 | 1/6-infective nonunion | Not mentioned. |
| Davis et al.12) (1990) | Not mentioned. | 7/9 | 2/9 | 0 | Not mentioned. |
| Kweon et al.14) (2017) | Not mentioned. | 15/15 | 0 | 0 | 0 |
| Lee et al.15) (2018) | Fixation failure was defined as reoperation, such as conversion to hip arthroplasty. To determine a collapse of fracture site, the sliding distance of fracture site through hip screw or blade was measured, and a collapse of more than 5 mm was defined as collapse of fracture site. | 63/69 | 6/69 (cutout), 18/69 (collapse) | Not mentioned. | 6-THA |
| Guo et al.16) (2019) | The patients were monitored for complications, such as femoral neck shortening, screw protrusion, screw cutout, nonunion (defined as a fracture with no sign of healing radiographically or clinically at 12 months postoperatively), and avascular necrosis. | 14/14 | 0 | 0 | 0 |
| Wang et al.17) (2019) | The major postoperative complications were identified as cut-out/cut-through, hardware-related femoral fracture, nonunion of the fracture, movement of the position of the lag screw in the femoral head, and varus development as a result of collapse. | 52/52 | 0 | 0 | 0 |
| Kim et al.18) (2020) | Not mentioned. | Not mentioned. | 3/67 (CMN group) | Not mentioned. | 5 (no mentions about reoperation method) |
| Yoo et al.19) (2019) | Cut-out was defined as penetration through the femoral head that was visible on X-ray, while cut-through was defined as the perforation of the femoral head from centric movement and without lateral movement by the lag screw. Significant sliding of the lag screw was defined arbitrarily by the authors, as an irritation sign due to the prominent lateral impingement without deep or superficial infection, as a lag screw sliding distance ≥10 mm in the plain X-ray or the removal of the lag screw due to one or both reasons. The excessive angular change was also arbitrarily defined as 10。or more. | 57/60 in ITST nail, 53/57 in PFNA, 67/68 in Gamma 3 CMN | 3/60 in ITST nail, 4/57 in PFNA, 1/68 in Gamma 3 CMN | Not mentioned. | Not mentioned. |
DRS: derotational screw, DHS: dynamic hip screw, THA: total hip arthroplasty, CMN: cephalomedullary nail, ITST: intertrochanteric/subtrochanteric, PFNA: proximal femoral nail antirotation.
DISCUSSION
Although the studies included in this study had similar definitions regarding where the line of the basicervical fracture is located in the medial of the intertrochanteric line, the definitions of the basicervical fractures differed among the studies in whether they are accompanied by comminution or are extra- or intracapsular fracture. In addition, radiographs presented in each study were inconsistent with the definition of basicervical fractures in the same study. Due to this, the proportion of basicervical fractures among all hip fractures varies among the studies. Kim et al.18) reported a prevalence of basicervical fractures of 4.5%. In the study of Lee et al.15), 2.4% of hip fractures were basicervical fractures. On the other hand, in the study of Guo et al.16), only 17 out of 2,291 femoral neck fracture patients had basicervical fractures (0.74%). It is difficult to provide the exact definition and location of the basicervical fracture using the previously used fracture classification method10,20). Considering the extracapsular location, large fracture angle, and the absence of muscular attachment to the proximal fragment, basicervical fractures have to be classified as AO type B2.12,3,10,21). Other studies have reported that AO type A2.1, A2.2, and A2.3 or Jensen type 3-5 with rotational instability of the headneck fragment or Jensen type 1-2 are similar to each other22,23,24). Although many studies have evaluated the fracture type by using simple radiographs, three-dimensional computed tomography might be necessary for accurate diagnosis10,25). The radiographs presented in each study differ in the type of implant, fracture union, and fixation failure, but the fracture line consistently disrupts the intertrochanteric line or involves the lesser trochanter and greater trochanter. Because of this, patients with intertrochanteric fractures were enrolled in each study, which make the results of treatment difficult to interpret.
The types of implants used for fixation of the basicervical fractures were very diverse, and treatment results such as fixation failure rate and collapse rate of the fracture site were also very different. It remains difficult to fully trust the results of each study or to discuss the superiority or the effectiveness of a particular implant, because the question remains as to whether the subjects enrolled in each study met the definition of basicervical fracture. Femoral neck fractures lead to rotational instability of the proximal fragment22,26,27). Therefore, the single-screw type of cephalomedullary fixation dose not achieve accurate reduction or stable fixation. On the other hand, an intertrochanteric fracture has more rotational stability than a femoral neck fracture. However, there is still controversy on rotational instability of the proximal fragment in patients with basicervical fractures in which the head-neck fragment does not involve the trochanteric area with a long inferior cortical extension. On the basis of biomechanical test for the basicervical fracture, Blair et al.2) have reported no difference in torsional stability between a sliding hip screw alone and a sliding hip screw combined with an anti-rotational cancellous screw. However, Massoud3) have suggested that an anti-rotational screw should be added to control rotational instability after surgery because the lag screw has potential to rotate the rotationally unstable femoral head during its insertion. Authors of recent reports included in this study argue that the antirotational effect of implant should be taken into account when selecting an implant for the fixation of these rotationally unstable fractures14,15,16,17,18,19).
The main variables for radiological evaluation of basicervical fractures were the presence of collapse, cut-out of the screw, and nonunion. Each study had a different view on whether collapse should be interpreted as failure. Su et al.11) did not define collapse as a fixation failure. Although the rate of collapse was very high (75%) in their study due to the protrusion of a compression screw, only three cases had revision due to fixation failure associated with varus malunion. There was no evidence to clinically determine the failure because functional assessment of patients with severe collapse was not reported separately. Varus collapse was also observed by Tasylkan et al.9) and Hu et al.8), but was not included in the failure category. Tasylkan et al.9) did not include varus unions of 10-20 degrees in the failure category either. However, Watson et al.7) did include collapse in the definition of fixation failure. They reported a much higher failure rate than in other studies. In addition, problems such as short follow-up period, selection bias, and lack of analysis of cephalomedullary screw position might have caused their high failure rate.
Some studies described collapse and varus as fixation failure. Although there was no definitive evidence of rotational stability of the proximal fragment in patients with basicervical femoral neck fractures, there was no difference in results between patients treated with DHS only and those treated with DHS and an antirotation cancellous screw. There was no difference in torsional stability in a mechanical test either between DHS and DHS with a cancellous screw2). The main mechanism of failure seemed to be collapse to varus or a slide to the axis of the cephalomedullary screw2,11,12,28). The shape of the section of the basicervical femoral neck is oval and does not rotate easily in the distal fragment. Because the proximal part of the fracture site is smaller than the distal part, the possibility of impaction of the proximal part into the distal part of the marrow is high. Su et al.11) found a high rate of sliding of the cephalomedullary screw. Therefore, anatomical structure appears to contribute to failure. In addition, when a proximal cephalomedullary nail was used, the proximal fragment might have unevenly slide, leading to varus collapse. This seems to be a likely mechanism of a high failure rate in Watson et al.'s study7). However, factors affecting collapse of a fracture site, such as reduction quality, tip-apex distance, insertion position of the cephalomedullary screw, and time of weight bearing might vary1,7). Some studies showed good results after treatment of basicervical fractures with cephalomedullary nails9,10). Further studies on the treatment outcomes in patients with basicervical fractures treated by using PFNs are needed.
A limitation of this study was that meta-analysis of treatment results or fixation failure for each implant was not possible due to the heterogeneity of the included reports.
CONCLUSION
Definitions of and treatment methods for basicervical fractures varied, and treatment outcomes also differed among the enrolled studies. Further research is needed that would be restricted to those fractures that conform to the definition of basicervical fracture.
Appendix
Detailed Search Strategies for Each Database
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Chen CY, Chiu FY, Chen CM, Huang CK, Chen WM, Chen TH. Surgical treatment of basicervical fractures of femur--a prospective evaluation of 269 patients. J Trauma. 2008;64:427–429. doi: 10.1097/01.ta.0000239255.47280.6f. [DOI] [PubMed] [Google Scholar]
- 2.Blair B, Koval KJ, Kummer F, Zuckerman JD. Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop Relat Res. 1994;(306):256–263. [PubMed] [Google Scholar]
- 3.Massoud EI. Fixation of basicervical and related fractures. Int Orthop. 2010;34:577–582. doi: 10.1007/s00264-009-0814-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imren Y, Gurkan V, Bilsel K, et al. Biomechanical comparison of dynamic hip screw, proximal femoral nail, cannulated screw, and monoaxial external fixation in the treatment of basicervical femoral neck fractures. Acta Chir Orthop Traumatol Cech. 2015;82:140–144. [PubMed] [Google Scholar]
- 5.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 7.Watson ST, Schaller TM, Tanner SL, Adams JD, Jeray KJ. Outcomes of low-energy basicervical proximal femoral fractures treated with cephalomedullary fixation. J Bone Joint Surg Am. 2016;98:1097–1102. doi: 10.2106/JBJS.15.01093. [DOI] [PubMed] [Google Scholar]
- 8.Hu SJ, Yu GR, Zhang SM. Surgical treatment of basicervical intertrochanteric fractures of the proximal femur with cephalomeduallary hip nails. Orthop Surg. 2013;5:124–129. doi: 10.1111/os.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.TasyIkan L, Ugutmen E, Sanel S, Soylemez MS, Ozkan K, Solakoglu C. Short-term results of surgical treatment with cephalomedullary nails for basicervical proximal femoral fractures. Acta Orthop Belg. 2015;81:427–434. [PubMed] [Google Scholar]
- 10.Saarenpää I, Partanen J, Jalovaara P. Basicervical fracture--a rare type of hip fracture. Arch Orthop Trauma Surg. 2002;122:69–72. doi: 10.1007/s004020100306. [DOI] [PubMed] [Google Scholar]
- 11.Su BW, Heyworth BE, Protopsaltis TS, et al. Basicervical versus intertrochanteric fractures: an analysis of radiographic and functional outcomes. Orthopedics. 2006;29:919–925. doi: 10.3928/01477447-20061001-04. [DOI] [PubMed] [Google Scholar]
- 12.Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990;72:26–31. doi: 10.1302/0301-620X.72B1.2298790. [DOI] [PubMed] [Google Scholar]
- 13.Kuokkanen HO. Treatment options for basicervical fractures of the femoral neck. A clinical follow-up. Acta Orthop Belg. 1991;57:162–168. [PubMed] [Google Scholar]
- 14.Kweon SH, Lee SH, Kook SH, Choi YC. Outcomes of cephalomedullary nailing in basicervical fracture. Hip Pelvis. 2017;29:270–276. doi: 10.5371/hp.2017.29.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YK, Yoon BH, Hwang JS, Cha YH, Kim KC, Koo KH. Risk factors of fixation failure in basicervical femoral neck fracture: which device is optimal for fixation? Injury. 2018;49:691–696. doi: 10.1016/j.injury.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Guo J, Dong W, Jin L, et al. Treatment of basicervical femoral neck fractures with proximal femoral nail antirotation. J Int Med Res. 2019;47:4333–4343. doi: 10.1177/0300060519862957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Q, Gu XH, Li X, et al. Management of low-energy basicervical proximal femoral fractures by proximal femoral nail anti-rotation. Orthop Surg. 2019;11:1173–1179. doi: 10.1111/os.12579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim JT, Ha YC, Park CH, Yoo JI, Kim TY. Single screw type of lag screw results higher reoperation rate in the osteosynthesis of basicervical hip fracture. J Orthop Sci. 2020;25:152–155. doi: 10.1016/j.jos.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Yoo J, Kim S, Choi J, Hwang J. Gamma 3 U-Blade lag screws in patients with trochanteric femur fractures: are rotation control lag screws better than others? J Orthop Surg Res. 2019;14:440. doi: 10.1186/s13018-019-1427-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deneka DA, Simonian PT, Stankewich CJ, Eckert D, Chapman JR, Tencer AF. Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures. J Orthop Trauma. 1997;11:337–343. doi: 10.1097/00005131-199707000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979;61:216–221. [PubMed] [Google Scholar]
- 22.Swiontkowski MF. Intracapsular fractures of the hip. J Bone Joint Surg Am. 1994;76:129–138. doi: 10.2106/00004623-199401000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Pervez H, Parker MJ, Pryor GA, Lutchman L, Chirodian N. Classification of trochanteric fracture of the proximal femur: a study of the reliability of current systems. Injury. 2002;33:713–715. doi: 10.1016/s0020-1383(02)00089-x. [DOI] [PubMed] [Google Scholar]
- 24.Jensen JS. Classification of trochanteric fractures. Acta Orthop Scand. 1980;51:803–810. doi: 10.3109/17453678008990877. [DOI] [PubMed] [Google Scholar]
- 25.Shoda E, Kitada S, Sasaki Y, et al. Proposal of new classification of femoral trochanteric fracture by three-dimensional computed tomography and relationship to usual plain X-ray classification. J Orthop Surg (Hong Kong) 2017;25:2309499017692700. doi: 10.1177/2309499017692700. [DOI] [PubMed] [Google Scholar]
- 26.Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J Orthop. 2008;42:3–12. doi: 10.4103/0019-5413.38574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith FB. Effects of rotatory and valgus malpositions on blood supply to the femoral head; observations at arthroplasty. J Bone Joint Surg Am. 1959;41:800–815. [PubMed] [Google Scholar]
- 28.Ort PJ, LaMont J. Treatment of femoral neck fractures with a sliding compression screw and two Knowles pins. Clin Orthop Relat Res. 1984;(190):158–162. [PubMed] [Google Scholar]