Abstract
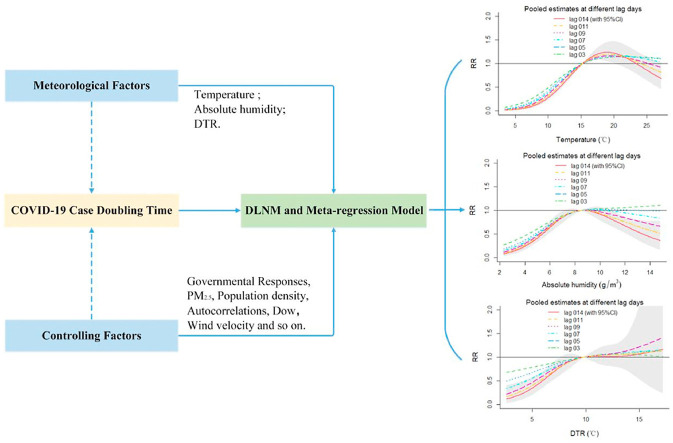
With the global lockdown, meteorological factors are highly discussed for COVID-19 transmission. In this study, national-specific and region-specific data sets from Germany, Italy, Spain and the United Kingdom were used to explore the effect of temperature, absolute humidity and diurnal temperature range (DTR) on COVID-19 transmission. From February 1st to November 1st, a 7-day COVID-19 case doubling time (Td), meteorological factors with cumulative 14-day-lagged, government response index and other factors were fitted in the distributed lag nonlinear models. The overall relative risk (RR) of the 10th and the 25th percentiles temperature compared to the median were 0.0074 (95% CI: 0.0023, 0.0237) and 0.1220 (95% CI: 0.0667, 0.2232), respectively. The pooled RR of lower (10th, 25th) and extremely high (90th) absolute humidity were 0.3266 (95% CI: 0.1379, 0.7734), 0.6018 (95% CI: 0.4693, 0.7718) and 0.3438 (95% CI: 0.2254, 0.5242), respectively. While the DTR did not have a significant effect on Td. The total cumulative effect of temperature (10th) and absolute humidity (10th, 90th) on Td increased with the change of lag days. Similarly, a decline in temperature and absolute humidity at cumulative 14-day-lagged corresponded to the lower RR on Td in pooled region-specific effects. In summary, the government responses are important factors in alleviating the spread of COVID-19. After controlling that, our results indicate that both the cold and the dry environment also likely facilitate the COVID-19 transmission.
Keywords: COVID-19, Meteorological factor, Government response index, DLNM
Graphical abstract
1. Introduction
Corona Virus Disease 2019, abbreviated as “COVID-19″, named by the World Health Organization (Wu and McGoogan, 2020; Zu et al., 2020), has been confirmed as an acute respiratory infectious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection (WHO, 2020a; Huang et al., 2020; Yu et al., 2020). Due to its fast and wide transmission world-widely, it has been recognized as a global pandemic (WHO, 2020b), which has infected 47,930,397 confirmed cases, including 1,221,781 deaths as of 5:00 pm CEST, November 5, 2020 (WHO, 2020c). Whether this global pandemic is partially influenced by the change of ambient environment is still a hot topic, which needs to be discussed continuously.
Although there is no final conclusion on the meteorological impact over the continuously growing of COVID-19 cases worldwide, it usually indicates that SARS-CoV-2 may be particularly sensitive to weather (Bashir et al., 2020; Kumar et al., 2020c; Liu et al., 2020; Tosepu et al., 2020). A preliminary laboratory test found that the survival time of new coronaviruses decreased with increasing temperature and humidity (van Doremalen et al., 2020). Besides, airborne-based virus transmission depends on the respiratory droplet size (Altamimi and Ahmed, 2020; Kumar et al., 2020b). The cold and dry weather may cause droplets drift and evaporation, which promote the dynamics of the infection transmission. In statistical analysis, a lot of studies reported that meteorological factors were closely related to the confirmed cases of COVID-19 (Chien and Chen, 2020; Halaji et al., 2020; Hon et al., 2020; Kumar et al., 2020a; Liu et al., 2020; Rabaan et al., 2020; Şahin, 2020). However, many analyses only obtained the conclusion in a simple regression model without controlling social factors and in a limited studying time period, which may lead to missed opportunities in understanding how the epidemic began and resolved. It is well acknowledged that many countries have implemented varying degrees of public health measures, including restricted assembly, traffic restrictions, family isolation and contact tracking, in order to prevent the spread of COVID-19 since its outbreak. Studies have shown that the wide spread of COVID-19 is related to the lack of intervention policy control (Briz-Redón and Serrano-Aroca, 2020; Ma et al., 2020; Prata et al., 2020; Khursheed et al., 2020). We believe that these factors such as government responses may conceal the role of meteorological factors in the COVID-19 spread. Therefore, it is necessary to adjust these factors like government responses before concluding the effects of meteorological factors on COVID-19 transmission.
So far, most researchers have used the number of daily confirmed COVID-19 as an indicator, which may be not as accurate in exploring the impact of meteorological factors on the spread of COVID-19. Muniz-Rodriguez et al. calculated the COVID-19 case doubling time (Td) to indicate the COVID-19 transmission trend, which refers to the time it takes for the total number of COVID-19 cases to double (Muniz-Rodriguez et al., 2020). Their results indicated that Td was a more sensitive indicator for the spread rate COVID-19. In addition, many indicators have been explored to indicate the role of government intervention in controlling COVID-19, such as the Baidu migration index (Hu et al., 2020), management vulnerability index (Acharya and Porwal, 2020), Google Mobility Data (Wang and Yamamoto, 2020), government response index (GRI) (Tran et al., 2020), etc. Among them, the GRI may be a better one, because it integrates 14 indicators in terms of containment and closure policies, economic policies, and health system policies (including School Closures, Workplace closing, Cancel Public Events, Restrictions on gatherings, Public Transportation, Stay at Home Order, Restrictions on Internal Movement, International Travel Controls, Income Support, Debt/contract Relief for Households, Public Information Campaigns, Testing Policy and Contact Tracing). Concerning the above issues, as many European countries are experiencing the second increasing wave of COVID-19, we hope to estimate the true impact of meteorological factors on the COVID-19 and provide scientific evidence for COVID-19 controlling. Therefore, in this study, we analyzed the effect of governmental responses on COVID-19 transmission, and used the distributed lag nonlinear model (DLNM) to study the impact of meteorological factors on COVID-19 case Td in four European countries (Germany, Italy, Spain and the United Kingdom) by controlling confounding factors like government responses, population density, air pollutants, etc.
2. Method
2.1. Data collection
2.1.1. COVID-19 data and transmission index
From February 1st through November 1st, 2020, we collected information on confirmed cases in 42 provincial regions. The above data was taken from the websites of national health departments (https://github.com/topics/covid-19). In this study, an exponential model involving the number and time of confirmed cases was considered: doubling time (Td). The Td is defined as the time it takes for the total number of COVID-19 cases to double, which is an index to evaluate the spread rate of the epidemic (Muniz-Rodriguez et al., 2020; Zhou et al., 2020). Considering that the average incubation period of COVID-19 is 7 days (Muniz-Rodriguez et al., 2020; Zhou et al., 2020), we choose 7 days as the interval of the exponential model. Then the equation of Td given by:
| (eq1) |
Where represents the cumulative number of diagnosed on the day of the study, and represents the cumulative number of diagnosed after an interval of 7 days.
2.1.2. Meteorological data
The daily meteorological data came from the “Wheat-A″ data system (http://www.xiaomaiya.cc/). Based on longitude and latitude, the meteorological data of 326 weather stations were matched with regions. Daily meteorological data included average/minimum/maximum temperature, dew-point temperature and average wind velocity. Absolute humidity was calculated indirectly through vapor pressure, using the Clausius–Clapeyron relation (Shaman and Kohn, 2009). Briefly, we first calculated the actual vapor pressure using daily dew-point temperature. Then, absolute humidity (AH) is derived by vapor pressure (Davis et al., 2016), which is described as equations (eq2), (eq3):
| (eq2) |
| (eq3) |
Where denote the actual vapor pressure; refers to the saturated water vapor pressure (6.112 hPa) at temperature (0 °C); represents the latent heat of water evaporation (2257 kJ/kg); is the gas constant of water vapor [287 J/(kg·°C)]; means daily ambient temperature (°C); means daily dew-point temperature (°C).
2.1.3. Fine particles, population density and GRI
Environmental fine particles (PM2.5), population density and GRI data were collected simultaneously. Daily PM2.5 data were downloaded from the “Air Matters” (https://air-matters.com/zh-Hans/index.html). The information about population density was obtained from the European Statistical System (https://ec.europa.eu/eurostat/databrowser/view/demo_r_d3dens/default/map?lang=en), which are available in the supplementary materials. The data on GRI were downloaded from GitHub Covid-policy-tracker (https://github.com/OxCGRT/covid-policy-tracker), which integrated 14 indicators in terms of containment and closure policies, economic policies, and health system policies: School Closures, Workplace closing, Cancel Public Events, Restrictions on gatherings, Public Transportation, Stay at Home Order, Restrictions on Internal Movement, International Travel Controls, Income Support, Debt/contract Relief for Households, Public Information Campaigns, Testing Policy and Contact Tracing (Thomas Hale et al., 2020). The index was adjusted from 0 to 100 (100 = the strictest).
2.2. Statistical analysis
Firstly, we used Pearson correlation analysis to explore the relationship between meteorological factors and daily Td. Then, based on the published research (Runkle et al., 2020), we established DLNM models to evaluate the effects of meteorological factors on the daily Td. Meanwhile, we controlled PM2.5, population density, GRI, residual autocorrelation (Imai et al., 2015) and other confounding factors in the models. To allow for over-dispersion of COVID-19 in transmission, a quasi-Poisson regression was used as the connection function of the model. The model used three independent research variables: temperature, absolute humidity and diurnal temperature range (DTR). The relative risk (RR) of the Td was estimated by the 90th, 75th, 25th and 10th percentiles values relative to the median of each meteorological factors. This method is suitable for assessing the intermittent changes (e.g., meteorological) in the risk of a rare and acute outcome (i.e., COVID-19 transmission) within a short period (Armstrong et al., 2019; Runkle et al., 2020). We conducted this research using the “dlnm” package in R4.0.1. The modified DLNM models are shown in equations (eq4), (eq5), (eq6):
| (eq4) |
| (eq5) |
| (eq6) |
Where t is the observation date; refers to the regions; is the expected value of the Td observed in region on day t; is the intercept; is the regression coefficient; represents the two-dimensional matrix of meteorological factors and lag days and the natural cubic spline function with 3 degrees of freedom was used; We defined 14 days as the maximum lag days; denotes the smoother based on natural regression splines; , , and are the three-day moving average of temperature (df = 6), PM2.5 (df = 3), absolute humidity (df = 3) and wind velocity (df = 3), respectively; is the COVID-19 count of logarithmic conversion on t-1 to control potential sequential autocorrelations; denotes the number of people living on land per unit area; is the GRI at single 14-day-lagged; means the day of week was controlled as a categorical variable; indicates region fixed effects to control for any observable and unobservable characteristics over time that could confound results, such as differences in social, economic and cultural activities, etc. (Amuakwa-Mensah et al., 2017).
After establishing the DLNM model, we used the random effects model of meta-analysis to pool the national-specific effects of the meteorological factors. We examined the cumulative lag effects of meteorological factors at 10th and 90th percentiles on Td under different lag exposure (lag 03, lag 05, lag 07, lag 09, lag 011 and lag 014). The meta-analysis was based on R software “meta” package.
As our design of including multiple regions, we further investigated the region-specific effect estimates of meteorological factors on Td in 42 regions and applied a multivariate meta-analysis to combine the overall effect estimates obtained from the region-specific effect estimates. In short, we used a two-stage analysis. Firstly, DLNM models were applied to each region's data to obtain region-specific effect estimates. Secondly, we applied a multivariate meta-regression model to combine the overall effect estimates (Gasparrini and Armstrong, 2013). The multivariate meta-regression analysis was fitted with R software using the “mvmeta” package.
Besides, we conducted a sensitivity analysis by changing the interval of the exponential model (eq (1)) to assess the effect of meteorological factors on Td at different time intervals (5 and 9 days) in the DLNM models (eq 4 - eq (6)).
3. Results
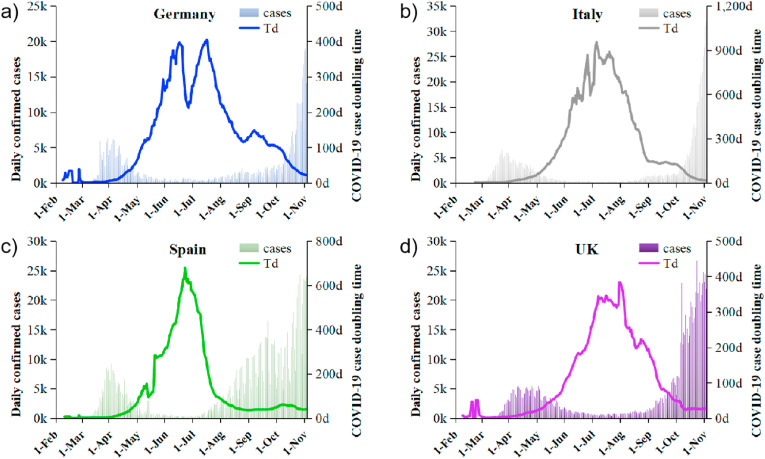
In total, 1,508,094 COVID-19 confirmed cases were included in this study from February 1st through November 1st, 2020. The change of COVID-19 new cases exhibited a temporal characteristic, showing two increasing waves till November. The first peak observed in spring (March–May) in these four countries corresponded to shorter Td, while the second increasing wave observed much stronger since August compared with the first one (with a rapid increase since early July in Spain) (Fig. 1 ). With the latest data, we could find that the confirmed COVID-19 cases were still on the rising trend, which have not reached the peak so far.
Fig. 1.
The trend of total COVID-19 daily confirmed case counts and the COVID-19 case doubling time in Germany (a), Italy (b), Spain (c) and UK (d) from February 1st through November 1st, 2020.
3.1. Correlation between the Td and variables
Pearson correlation analysis of daily Td and meteorological factors for four countries from February 1st through November 1st, 2020 were shown in Table. 1 , Fig.S1-S3 and Fig.S6-S8. Temperature in four countries had similar patterns, all showed positive associations with Td (rGermany = 0.66, rItaly = 0.64, rSpain = 0.47, rUK = 0.75, respectively), similar to the correlation between absolute humidity and the Td (rGermany = 0.55, rItaly = 0.50, rSpain = 0.25, rUK = 0.67, respectively). However, the correlations between diurnal temperature range (DTR) and Td were weak in Germany, Italy and Spain (rGermany = 0.07, rItaly = 0.10, rSpain = 0.12, respectively), while the correlation in the UK was not statistically significant (rUK = −0.01, p > 0.05). There was a negative correlation between population density and Td in four countries, but the correlation was higher in the UK (Table. 1 and Fig.S4). In linear regression analysis, the GRI at single 14-day-lagged was highly positively correlated with Td (except for Italy) (Table. 1 and Fig.S5), indicating the GRI is an important factor in controlling COVID-19.
Table 1.
Pearson correlations between the variables and the log (Td).
| Variables | Germany | Italy | Spain | The United Kingdom |
|---|---|---|---|---|
| Temperature | 0.66a | 0.64a | 0.47a | 0.75a |
| Absolute humidity | 0.55a | 0.50a | 0.25a | 0.67a |
| DTR | 0.07a | 0.10a | 0.12a | −0.01 |
| Population density | −0.34 | −0.30 | −0.02 | −0.97a |
| GRI lag14 | 0.65a | −0.05a | 0.68a | 0.62a |
p < 0.05. Td: the COVID-19 case doubling time; log (Td): the common logarithm of the Td; DTR, diurnal temperature range; GRI lag14: the government response index at single 14-day-lagged.
3.2. Effects of meteorological factors on Td
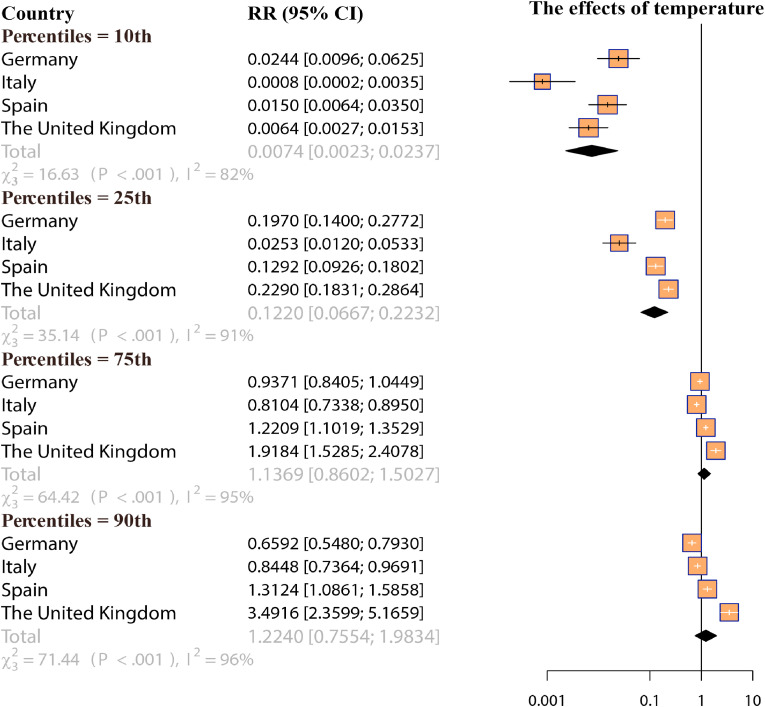
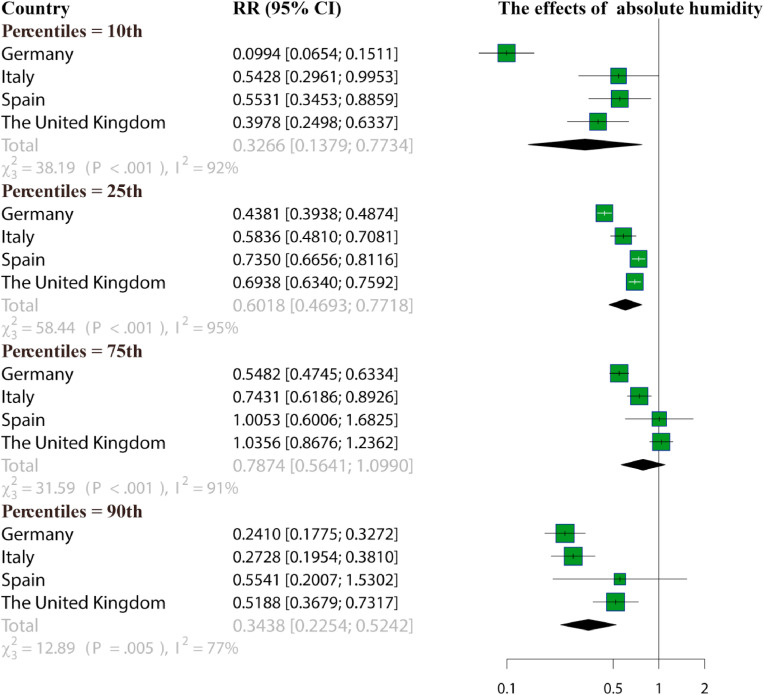
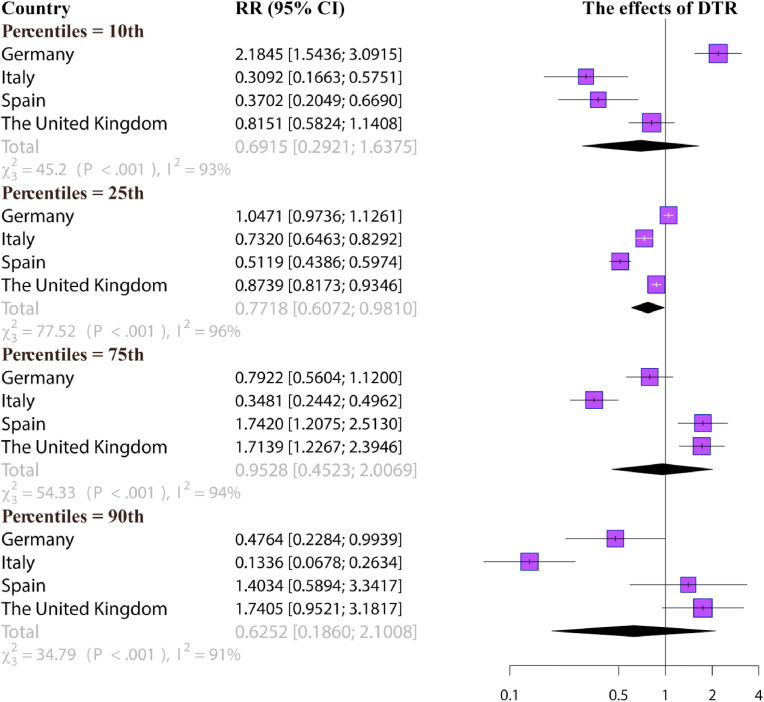
Fig. 2, Fig. 3, Fig. 4 show the results of the meta-analysis about the RR of Td associated with different percentiles values (10th, 25th, 75th and 90th) of temperature, absolute humidity and DTR at cumulative 14-day-lagged. In the regional analysis, the most significant effect of lower temperature (10th) on Td was found in Italy (RR = 0.0008, 95% CI: 0.0002, 0.0035). In the pooled analysis, compared with the median of each meteorological factors, lower temperatures (10th and 25th) had a greater impact on Td. The RR of temperature in the 10th and 25th percentiles were 0.0074 (95% CI: 0.0023, 0.0237) and 0.1220 (95% CI: 0.0667, 0.2232), respectively. Similar to the temperature, the effect of low absolute humidity on Td was significant. There was the most significant effect of lower humidity (10th) on Td in Germany (RR = 0.0944, 95% CI: 0.0654, 0.1511). The RR of Td at 10th percentile and 25th percentile were 0.3266 (95% CI: 0.1379, 0.7734) and 0.6018 (95% CI: 0.4693, 0.7718). Meanwhile, the significant effect of extremely high humidity was also observed at the 90th percentile of absolute humidity (RR = 0.3438, 95% CI: 0.2254, 0.5242). However, the effect estimates of DTR on Td were not statistically significant.
Fig. 2.
A meta-analysis for the relative risk (95% confidence interval) of the COVID-19 case doubling time associated with different percentiles values (10th, 25th, 75th and 90th) of temperature at cumulative 14-day-lagged.
Fig. 3.
A meta-analysis for the relative risk (95% confidence interval) of the COVID-19 case doubling time associated with different percentiles values (10th, 25th, 75th and 90th) of absolute humidity at cumulative 14-day-lagged.
Fig. 4.
A meta-analysis for the relative risk (95% confidence interval) of the COVID-19 case doubling time associated with different percentiles values (10th, 25th, 75th and 90th) of diurnal temperature range at cumulative 14-day-lagged. DTR, diurnal temperature range.
3.3. Cumulative lag effects of meteorological factors
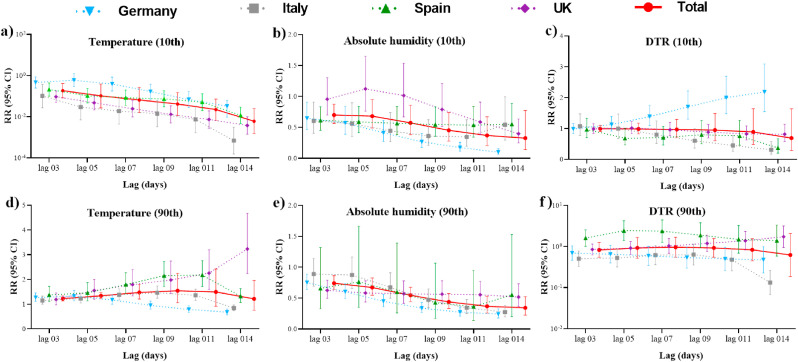
Fig. 5 presents the RR for the cumulative effect of Td under different lag exposure (lag 03, lag 05, lag 07, lag 09, lag 011 and lag 014) at 10th and 90th percentiles of temperature, absolute humidity and DTR. Temperature with 10th percentile showed an enhanced cumulative effect on the Td as the lag days change, while temperature with 90th percentile showed a non-significant cumulative effect. The cumulative effect of absolute humidity on Td decreased in the exposure at 10th and 90th percentiles, peaking at cumulative 14 days. The cumulative lag effect of DTR was not significant.
Fig. 5.
The cumulative lag effects on the COVID-19 case doubling time with the 10th percentile (a, b, c) and the 90th percentile (d, e, f) of meteorological factors under different lag exposure periods (lag 03, lag 05, lag 07, lag 09, lag 011 and lag 014). Total: a meta-analysis of relative risk across four countries; DTR, diurnal temperature range.
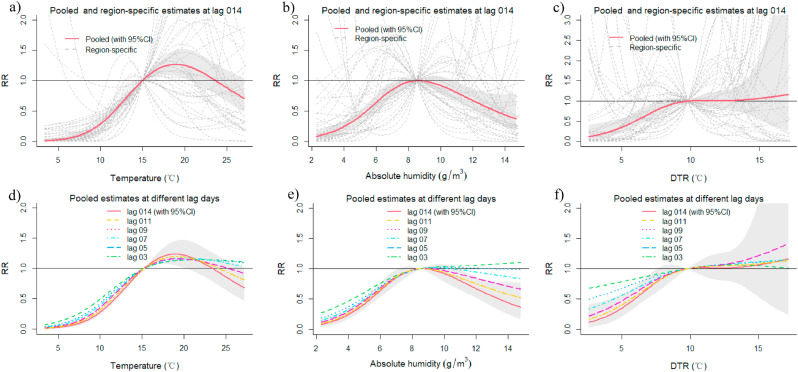
3.4. Multivariate meta-regression analysis and sensitivity analysis
The overall estimates from the region-specific effects are similar to the country-specific effects (Fig. 6 ), indicating that low temperature and low absolute humidity may be a factor leading to shorter Td in four European countries, resulting in a faster spread of the virus. In the sensitivity analysis, the associations between meteorological factors and the Td of different time intervals (5 and 9 days) were robust. The low temperature and extreme absolute humidity have a greater impact on the COVID-19 Td (Table.S1-S2), indicating that they likely favor the COVID-19 transmission.
Fig. 6.
The region-specific effect (lag 014) and the overall estimates effect under different lag exposure periods of temperature (a, d), absolute humidity (b, e) and diurnal temperature range (c, f). DTR, diurnal temperature range.
4. Discussion
COVID-19 is a widely transmitted respiratory disease, which has been listed as a pandemic by the World Health Organization (WHO, 2020b). Since the outbreak of COVID-19, the arguments over whether the ambient environment could affect its transmission have continuously been a hot topic worldwide. To date, no consistent evidence has been reached with varying study periods, countries/regions with varying climate and weather, and the lack of controlling confounding factors like population density, government intervention policies, etc. To solve these issues, we used the DLMN statistic model to quantitatively evaluate the effects of meteorological factors on COVID-19 transmission during a longer period and controlled the bias from government intervention policies in a form of GRI. Our results indicated that government responses are important factors in controlling COVID-19 pandemic. After controlling government responses and other confounding factors, we found that both the lower temperature and the lower absolute humidity had a greater impact on the COVID-19 case Td.
Although there was a bit difference in the RR in analysis of the association between meteorological factors and Td, but their associations were quit similar, all indicated the positive effect of lower temperature and lower humidity on COVID-19 transmission. This is consistent with those reported in other geographical locations (Bashir et al., 2020; Ma et al., 2020; Tosepu et al., 2020; Xie and Zhu, 2020). With the arriving of winter in these four European countries, the second increasing wave of COVID-19 confirmed cases were much more strong compared to the first one, which better proved that COVID-19 transmission was related to low temperature. An experimental study reported that the SARS-CoV-2 virus was highly stable at 4 °C, but sensitive to heat (van Doremalen et al., 2020). At 4 °C, there was only around a 0.7 log-unit reduction of infectious titer on day 14, but the time for virus inactivation reduced to 5 min (Chin et al., 2020), when the incubation temperature increased to 70 °C. That is, the high temperature is not conducive to the survival of the virus. Besides, it is known that respiratory viruses (such as influenza) can survive longer in a cold environment (Martinez, 2018). Similar virus like SARS-CoV and MERS-CoV were also reported to maintain stronger infectivity at low temperatures on a solid surface, whether it was droplet state or aerosol state (van Doremalen et al., 2013; Casanova et al., 2010; Kim et al., 2007). Besides, the body's resistance become relatively weak under cold stress (Shaw, 2016), particularly, the phagocytosis function of alveolar macrophage was depressed in an environment with lower temperature (Luo et al., 2017), which may also explain the higher confirmed COVID-19 cases and the shorter Td. Therefore, combined with the more obvious effect of lower temperature in cumulative analysis, our results indicated that the lower temperature is significantly beneficial to the transmission and survival of coronavirus.
Previous studies were usually under a linear regression framework, showing that there was a significant negative correlation between humidity and COVID-19 cases (Sarkodie and Owusu, 2020), which need to be confirmed with more precise statistic model. Islam et al. regarded humidity as a driver of SARS-CoV-2 transmission, and a higher COVID-19 transmission rate was reported in specific humidity ranged from 6 to 9 g/kg (Islam et al., 2020; Runkle et al., 2020b). In line with these studies, we found that extreme (high and low) absolute humidity have a greater impact on the COVID-19 Td, which were still robust in pooled analysis for the four European countries. When the humidity in the air is low, the virus forms small aerosol particles, which increases the risk of viral transmission and reduces immunity (Sarkodie and Owusu, 2020). It's reported that up to 3 h are needed for 2-μm aerosol particles to settle to the ground, while 10 μm aerosol particles only take about 10-min (Marr et al., 2019), the long stay of the virus in the air increase the risk of infection in others. In this study, we found the cumulative effect of lower humidity was obviously significant on Td. This means the longer stable dry environment would promote the long stay of SARS-CoV-2 and shorten the Td, which in turn increases the transmission of COVID-19. In addition, the mucociliary of the nasal cavity and upper respiratory tract have important interception and cleaning functions, but dry air can damage their epithelial structure (Arja I. Hälinen, 2000). To sum up, the dry environment can increase the spread of the virus and facilitate COVID-19 transmission. Also, studies have shown that a considerable number of people infected with COVID-19 suffer from underlying diseases (such as diabetes, hypertension, coronary heart disease, etc.) (Emami et al., 2020). Since extremely high humidity is also a risk factor for chronic diseases like cardiovascular disease in the elderly (Zeng et al., 2017), which may explain why it is also related to the shorter Td. In summary, we believe that a longer sustained dry environment may increase the spread of COVID-19, which need to be stressed in government interventions.
However, previous findings are inconsistent due to a few possible reasons (Xie and Zhu, 2020; Yao et al., 2020; Briz-Redón and Serrano-Aroca, 2020; Jahangiri et al., 2020). Firstly, the temperature range varied greatly with studies due to the short study period. Secondly, many studies are cross-sectional at the national level and there is a large degree of heterogeneity among different countries (Tobías and Molina, 2020). And in some time-series studies, researchers used the temperature of the capital city to reflect the average exposure temperature for one country, which leads to large exposure misclassification. Thirdly, regulations and human behaviors play a great role in the spread speed of COVID-19, e.g., contact tracking, quarantine strategy, the implementation ability of COVID-19 control policy, urbanization rate and the availability of medical resources (Bherwani et al., 2020; Jahangiri et al., 2020; Mukherjee et al., 2020; Bherwani et al., 2020; Jahangiri et al., 2020; Mukherjee et al., 2020). In this study, we conducted the DLMN analysis for a long period (from February 1st through November 1st, 2020), covering two increasing waves of COVID-19 confirmed cases and controlling factors like population density, GRI, etc. GRI integrates 14 indicators in terms of containment and closure policies, economic policies, and health system policies (including School Closures, Workplace closing, Cancel Public Events, Restrictions on gatherings, Public Transportation, Stay at Home Order, Restrictions on Internal Movement, International Travel Controls, Income Support, Debt/contract Relief for Households, Public Information Campaigns, Testing Policy and Contact Tracing). Thus, our models likely provide better estimates of meteorological factors on the COVID-19 spread by filtering out the impact of regulation and behavior.
A previous study indicated that the impact of environmental factors on virus transmission should be characterized using a dynamic model (such as the susceptible-exposed-infectious-recovered [SEIR] model), because infectiousness estimated from a traditional model is biased by confounding from environmental variables (Shi et al., 2020). However, the SEIR model has some limitations in its application. Firstly, the SEIR model needs to input the daily number of susceptible, exposed, infectious and removed individuals. These detailed data reports are incomplete in many countries or regions. Secondly, the SEIR model may lead to a deviation of output results due to different input parameter estimations (such as contact rate and infection rate) (He et al., 2020). For example, several studies used the SEIR model to evaluate the relationship between meteorological conditions (temperature and relative humidity) and COVID-19 in China, but the results were inconsistent due to the different input parameters of their models (Pan et al., 2021; Guo et al., 2020; Shi et al., 2020). Besides, to allow for over-dispersion of COVID-19 data, some studies used the generalized linear model with negative binomial distribution to fit the relationship between environmental factors and COVID-19 based on R software with “MASS” package (Liu et al., 2020; J Wang et al., 2020). A limitation of the generalized linear model is that it can't fit the nonlinear-lagged effects between environmental factors and COVID-19. And the previous study showed that both the quasi-Poisson distribution and negative binomial distribution regression model can be used for overdispersal data, and the quasi-Poisson distribution is a better fit to the overall variance-mean relationship (Ver Hoef and Boveng, 2007). Considering the above factors, the DLNM model with quasi-Poisson distribution is the most suitable for this study.
Although we have adjusted population density and GRI, there are still many restrictions that should not be ignored. In this study, our evidence is limited to modeling studies based on parameter assumptions with current incomplete case data. But the transmission of COVID-19 may be affected by many factors, including governmental interventions, social contact, population mobility, population vulnerability and so on. Therefore, this problem should be examined in future research. Secondly, Td is the time needed to double the number of infected people. As an indicator of COVID-19 transmission, it will change with the degree of infection and the implementation of human intervention with the passage of time. Only paying attention to the Td is not enough to accurately reflect the real situation of COVID-19 transmission. Therefore, our research results need to be further discussed. Thirdly, we only have analyzed the data from four countries covering nine months, which may not be enough to study the COVID-19 change trend at global level. Even so, the conclusion based on the present study at least provides new clues for understanding the relationship between the spread of COVID-19 and temperature and humidity.
5. Conclusion
In summary, the government responses are important factors in alleviating the spread of COVID-19. Our results indicate that both the cold and the dry environment also likely facilitate the COVID-19 transmission after controlling the bias from population density, government response policies, air pollutants and other factors in long study periods covering two increasing waves of COVID-19 in four European countries. This study used data from February 1st to November 1st, which provide strong scientific evidence for the importance of stressing the cold weather effect on COVID-19 transmission with the arriving colder season. In particular, we observed that the confirmed case of COVID-19 are still madly increasing in the Northern Hemisphere, so we strongly suggest to provide more public health resources and governmental interventions on the controlling of COVID-19 in this cold season. Besides, studies covering the entire earth in a longer period are urgently needed to quantify the combined effects of meteorological factors and policy interventions on the spread of COVID-19. By doing that, we hope to find the most effective intervention in controlling the COVID-19, particularly before the vaccinating of an effective vaccine against this tricky virus.
Credit author statement
Shihua Fu, Writing – original draft, Software, Data curation. Bo Wang, Writing – original draft, Software, Data curation. Ji Zhou, Methodology, Supervision, Conceptualization. Xiaocheng Xu, Methodology, Visualization. Jiangtao Liu, Methodology, Visualization. Yueling Ma, Formal analysis. Lanyu Li, Methodology, Visualization. Xiaotao He, Data curation. Sheng Li, Validation. Jingping Niu, Investigation. Bin Luo, Project administration. Bin Luo, Conceptualization, Writing – review & editing. Kai zhang, Conceptualization, Writing – review & editing.
Ethics approval and consent to participate
All data is public, there is no patient contact, and no PIN is required. Therefore, the study does not require ethical approval.
Consent for publication
Not applicable.
Availability of data and materials
All COVID-19 daily confirmed cases were collected from the official websites of national or regional health departments from February 1st through November 1st, 2020, which are publicly available. The meteorological datasets used and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request. The population density datasets, particulate matter datasets and government response index datasets used and/or analyzed during the current study are available from the open-access websites. For additional details, please see Supplementary data.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank the other participants of the study for their valuable contributions. The authors would also like to thank the investigators and the staff of the public data for making the study possible. This project was supported by the Fundamental Research Funds for the Central Universities, Lanzhou University, China (lzujbky-2020-sp21); the Novel Coronavirus Disease Science and Technology Major Project in Gansu Province (20YF2FA028).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110596.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Acharya R., Porwal A. A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study. Lancet Glob Health. 2020;8(9):e1142–e1151. doi: 10.1016/S2214-109X(20)30300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altamimi A., Ahmed A.E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. Journal of Infection and Public Health. 2020;13(5):704–708. doi: 10.1016/j.jiph.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amuakwa-Mensah F., Marbuah G., Mubanga M. Climate variability and infectious diseases nexus: evidence from Sweden. Infect Dis Model. 2017;2(2):203–217. doi: 10.1016/j.idm.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arja I., Hälinen R.O.S.A. Combined respiratory effects of cold air with SO(2) or NO(2) in single 1-hour exposures of hyperventilating Guinea pigs. Inhal. Toxicol. 2000;12(8):693–713. doi: 10.1080/08958370050085147. [DOI] [PubMed] [Google Scholar]
- Armstrong B., Sera F., Vicedo-Cabrera A.M., Abrutzky R., Åström D.O., Bell M.L., Chen B.Y., de Sousa Z.S.C.M., Correa P.M., Dang T.N. The role of humidity in associations of high temperature with mortality: a multicountry, multicity study. Environ. Health Perspect. 2019;127(9) doi: 10.1289/EHP5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal, Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bherwani H., Gupta A., Anjum S., Anshul A., Kumar R. Exploring dependence of COVID-19 on environmental factors and spread prediction in India. npj Climate and Atmospheric Science. 2020;3(1):38. doi: 10.1038/s41612-020-00142-x. [DOI] [Google Scholar]
- Briz-Redón Á., Serrano-Aroca Á. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728:138811. doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien L., Chen L. Meteorological impacts on the incidence of COVID-19 in the U.S. Stochastic environmental research and risk assessment : research journal. 2020. 1, 6. [DOI] [PMC free article] [PubMed]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020;1(1):e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis R.E., McGregor G.R., Enfield K.B. Humidity: a review and primer on atmospheric moisture and human health. Environ. Res. 2016;144:106–116. doi: 10.1016/j.envres.2015.10.014. [DOI] [PubMed] [Google Scholar]
- Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1):e35. [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A., Armstrong B. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med. Res. Methodol. 2013;13:1. doi: 10.1186/1471-2288-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X., Zhang H., Zeng Y. Transmissibility of COVID-19 in 11 major cities in China and its association with temperature and humidity in Beijing, Shanghai, Guangzhou, and Chengdu. Infectious Diseases of Poverty. 2020;9(1):87. doi: 10.1186/s40249-020-00708-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halaji M., Farahani A., Ranjbar R., Heiat M., Dehkordi F.S. Emerging coronaviruses: first SARS, second MERS and third SARS-CoV-2: epidemiological updates of COVID-19. Infez Med. 2020;28(Suppl. 1):6–17. [PubMed] [Google Scholar]
- Hale Thomas, Webster Sam, Petherick Anna, Phillips Toby, Kira Beatriz. Blavatnik School of Government; 2020. https://github.com/OxCGRT/covid-policy-tracker Oxford COVID-19 Government Response Tracker. [Google Scholar]
- He S., Peng Y., Sun K. SEIR modeling of the COVID-19 and its dynamics. Nonlinear Dynam. 2020;101(3):1667–1680. doi: 10.1007/s11071-020-05743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hon K.L., Leung K., Leung A., Sridhar S., Qian S., Lee S.L., Colin A.A. Overview: the history and pediatric perspectives of severe acute respiratory syndromes: novel or just like SARS. Pediatr. Pulmonol. 2020;55(7):1584–1591. doi: 10.1002/ppul.24810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu J.X., He G.H., Liu T., Xiao J.P., Rong Z.H., Guo L.C., Zeng W.L., Zhu Z.H., Gong D.X., Yin L.H., others [Risk assessment of exported risk of COVID-19 from Hubei Province] Zhonghua Yufang Yixue Zazhi. 2020;54(4):362–366. doi: 10.3760/cma.j.cn112150-20200219-00142. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., others Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai C., Armstrong B., Chalabi Z., Mangtani P., Hashizume M. Time series regression model for infectious disease and weather. Environ. Res. 2015;142:319–327. doi: 10.1016/j.envres.2015.06.040. [DOI] [PubMed] [Google Scholar]
- Islam N., Bukhari Q., Jameel Y., Shabnam S., Erzurumluoglu A.M., Siddique M.A., Massaro J.M., D'Agostino R.S. COVID-19 and climatic factors: a global analysis. Environ. Res. 2020;110355 doi: 10.1016/j.envres.2020.110355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahangiri M., Jahangiri M., Najafgholipour M. The sensitivity and specificity analyses of ambient temperature and population size on the transmission rate of the novel coronavirus (COVID-19) in different provinces of Iran. Sci. Total Environ. 2020;728 doi: 10.1016/j.scittenv.2020.138872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khursheed A., Alam S., Tyagi V.K., Nagpure A.S., Khan A.A., Gaur R.Z., Singh S., Bhattacharya P., Mukherjee S., Kumar M. Future liasing of the lockdown during COVID-19 pandemic: the dawn is expected at hand from the darkest hour. Groundwater for Sustainable Development. 2020;11 doi: 10.1016/j.gsd.2020.100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.W., Ramakrishnan M.A., Raynor P.C., Goyal S.M. Effects of humidity and other factors on the generation and sampling of a coronavirus aerosol. Aerobiologia. 2007;23(4):239–248. doi: 10.1007/s10453-007-9068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Kuroda K., Dhangar K. The most eagerly awaited summer of the Anthropocene: a perspective of SARS-CoV-2 decay and seasonal change. Groundwater for Sustainable Development. 2020;11 doi: 10.1016/j.gsd.2020.100400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Mazumder P., Mohapatra S., Kumar Thakur A., Dhangar K., Taki K., Mukherjee S., Kumar Patel A., Bhattacharya P., Mohapatra P., others A chronicle of SARS-CoV-2: seasonality, environmental fate, transport, inactivation, and antiviral drug resistance. J. Hazard Mater. 2020 doi: 10.1016/j.jhazmat.2020.124043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Taki K., Gahlot R., Sharma A., Dhangar K. A chronicle of SARS-CoV-2: Part-I - epidemiology, diagnosis, prognosis, transmission and treatment. Sci. Total Environ. 2020;734 doi: 10.1016/j.scitotenv.2020.139278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T., others Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scittenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo B., Liu J., Fei G., Han T., Zhang K., Wang L., Shi H., Zhang L., Ruan Y., Niu J. Impact of probable interaction of low temperature and ambient fine particulate matter on the function of rats alveolar macrophages. Environ. Toxicol. Pharmacol. 2017;49:172–178. doi: 10.1016/j.etap.2016.12.011. [DOI] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marr L.C., Tang J.W., Van Mullekom J., Lakdawala S.S. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface. 2019;16(150) doi: 10.1098/rsif.2018.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez M.E. The calendar of epidemics: seasonal cycles of infectious diseases. PLoS Pathog. 2018;14(11) doi: 10.1371/journal.ppat.1007327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee S., Mazumder P., Joshi M., Joshi C., Dalvi S.V., Kumar M. Biomedical application, drug delivery and metabolic pathway of antiviral nanotherapeutics for combating viral pandemic: a review. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.110119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muniz-Rodriguez K., Fung I.C., Ferdosi S.R., Ofori S.K., Lee Y., Tariq A., Chowell G. Severe acute respiratory syndrome coronavirus 2 transmission potential, Iran, 2020. Emerg. Infect. Dis. 2020;26(8):1915–1917. doi: 10.3201/eid2608.200536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan J., Yao Y., Liu Z., Meng X., Ji J.S., Qiu Y., Wang W., Zhang L., Wang W., Kan H. Warmer weather unlikely to reduce the COVID-19 transmission: an ecological study in 202 locations in 8 countries. Sci. Total Environ. 2021;753 doi: 10.1016/j.scitotenv.2020.142272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabaan A.A., Al-Ahmed S.H., Haque S., Sah R., Tiwari R., Malik Y.S., Dhama K., Yatoo M.I., Bonilla-Aldana D.K., Rodriguez-Morales A.J. SARS-CoV-2, SARS-CoV, and MERS-COV: a comparative overview. Infez Med. 2020;28(2):174–184. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PubMed] [Google Scholar]
- Runkle J.D., Sugg M.M., Leeper R.D., Rao Y., Matthews J.L., Rennie J.J. Short-term effects of specific humidity and temperature on COVID-19 morbidity in select US cities. Sci. Total Environ. 2020;740 doi: 10.1016/j.scittenv.2020.140093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkodie S.A., Owusu P.A. Impact of meteorological factors on COVID-19 pandemic: evidence from top 20 countries with confirmed cases. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.110101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw S.P. Seasonality and selective trends in viral acute respiratory tract infections. Med. Hypotheses. 2016;86:104–119. doi: 10.1016/j.mehy.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., Zhao C., Li X., Liu W., He M., Tang S., Xi S. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobías A., Molina T. Is temperature reducing the transmission of COVID-19 ? Environ. Res. 2020;186 doi: 10.1016/j.envres.2020.109553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O.A.I., Lestari H., Bahar H., Asfian P. Correlation between weather and covid-19 pandemic in jakarta, Indonesia. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran T., Le T.H., Nguyen T., Hoang V.M. Rapid response to the COVID-19 pandemic: vietnam government's experience and preliminary success. J Glob Health. 2020;10(2) doi: 10.7189/Jogh.10.020502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Munster V.J. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18(38) doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., others Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ver Hoef J.M., Boveng P.L. Quasi-Poisson vs. negative binomial regression: how should we model overdispersed count data? Ecology. 2007;88(11):2766–2772. doi: 10.1890/07-0043.1. [DOI] [PubMed] [Google Scholar]
- Wang H.Y., Yamamoto N. Using a partial differential equation with Google Mobility data to predict COVID-19 in Arizona. Math. Biosci. Eng. 2020;17(5):4891–4904. doi: 10.3934/mbe.2020266. [DOI] [PubMed] [Google Scholar]
- Wang J., Li W., Yang B., Cheng X., Tian Z., Guo H. Impact of hydrological factors on the dynamic of COVID-19 epidemic: a multi-region study in China. Environ. Res. 2020;110474 doi: 10.1016/j.envres.2020.110474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) Clinical characteristics of covid-19 in China. N. Engl. J. Med. 2020;382(19):1859–1862. doi: 10.1056/NEJMc2005203. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) 2020. Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11th March 2020.https://who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- World Health Organization (WHO) 2020. Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard.https://covid19.who.int/ [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., Wang W. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55(5):2000517. doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu F., Du L., Ojcius D.M., Pan C., Jiang S. Measures for diagnosing and treating infections by a novel coronavirus responsible for a pneumonia outbreak originating in Wuhan, China. Microb. Infect. 2020;22(2):74–79. doi: 10.1016/j.micinf.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng J., Zhang X., Yang J., Bao J., Xiang H., Dear K., Liu Q., Lin S., Lawrence W.R., Lin A., others Humidity may modify the relationship between temperature and cardiovascular mortality in zhejiang Province, China. Int. J. Environ. Res. Publ. Health. 2017;14(11) doi: 10.3390/ijerph14111383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L., Liu J., Dong X., McGoogan J.M., Wu Z. COVID-19 seeding time and doubling time model: an early epidemic risk assessment tool. Infectious diseases of poverty. 2020;9(1):76. doi: 10.1186/s40249-020-00685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zu Z.Y., Di Jiang M., Xu P.P., Chen W., Ni Q.Q., Lu G.M., Zhang L.J. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020;296(2):E15–E25. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All COVID-19 daily confirmed cases were collected from the official websites of national or regional health departments from February 1st through November 1st, 2020, which are publicly available. The meteorological datasets used and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request. The population density datasets, particulate matter datasets and government response index datasets used and/or analyzed during the current study are available from the open-access websites. For additional details, please see Supplementary data.