Abstract
Objective:
Delayed admission of myocardial infarction (MI) patients is an important prognostic factor. In the present nationwide registry (TURKMI-2), we evaluated the treatment delays and outcomes of patients with acute MI during the Covid-19 pandemic and compaired with a recent pre-pandemic registry (TURKMI-1).
Methods:
The pandemic and pre-pandemic studies were conducted prospectively as 15-day snapshot registries in the same 48 centers. The inclusion criteria for both registries were aged ≥18 years and a final diagnosis of acute MI (AMI) with positive troponin levels. The only difference between the 2 registries was that the pre-pandemic (TURKMI-1) registry (n=1872) included only patients presenting within the first 48 hours after symptom-onset. TURKMI-2 enrolled all consecutive patients (n=1113) presenting with AMI during the pandemic period.
Results:
A comparison of the patients with acute MI presenting within the 48-hour of symptom-onset in the pre-pandemic and pandemic registries revealed an overall 47.1% decrease in acute MI admissions during the pandemic. Median time from symptom-onset to hospital-arrival increased from 150 min to 185 min in patients with ST elevation MI (STEMI) and 295 min to 419 min in patients presenting with non-STEMI (NSTEMI) (p-values <0.001). Door-to-balloon time was similar in the two periods (37 vs. 40 min, p=0.448). In the pandemic period, percutaneous coronary intervention (PCI) decreased, especially in the NSTEMI group (60.3% vs. 47.4% in NSTEMI, p<0.001; 94.8% vs. 91.1% in STEMI, p=0.013) but the decrease was not significant in STEMI patients admitted within 12 hours of symptom-onset (94.9% vs. 92.1%; p=0.075). In-hospital major adverse cardiac events (MACE) were significantly increased during the pandemic period [4.8% vs. 8.9%; p<0.001; age- and sex-adjusted Odds ratio (95% CI) 1.96 (1.20–3.22) for NSTEMI, p=0.007; and 2.08 (1.38–3.13) for STEMI, p<0.001].
Conclusion:
The present comparison of 2 nationwide registries showed a significant delay in treatment of patients presenting with acute MI during the COVID-19 pandemic. Although PCI was performed in a timely fashion, an increase in treatment delay might be responsible for the increased risk of MACE. Public education and establishing COVID-free hospitals are necessary to overcome patients’ fear of using healthcare services and mitigate the potential complications of AMI during the pandemic.
Keywords: acute myocardial infarction, COVID-19, pandemic, total ischemic time, treatment delay
Introduction
The prognosis of patients suffering from acute myocardial infarction (MI) directly depends on rapid diagnosis and early treatment. Therefore, fast transport and early admission to the hospital are crucial in improving prognosis after MI (1, 2). Patient-related factors can contribute to delays in treatment after the onset of symptoms. In addition, geographical or logistical factors or the organization of the healthcare management system can contribute to treatment delays (3, 4). The sudden outbreak of the Coronavirus Disease in 2019 (COVID-19) caused intense pressure on the community and the healthcare system. Recent observations suggest that the number of patients presenting with acute MI decreased with the emergence of the outbreak (5-5). Moreover, acute MI patients may be presenting at later stages during the pandemic due to fear of acquiring coronavirus in healthcare facilities (5-5). The extent of the delays, the stage at which the delay is prominent, and the potential effects of delays on outcomes are unclear. The Turkish Acute Myocardial Infarction (TURKMI)-2 registry was planned to assess delays in MI patient care at each step from symptom-onset to treatment. The effects of delays on in-hospital outcomes during the COVID-19 outbreak were also investigated. Data from TURKMI-2 are compared to the results from a recent nationwide registry (TURKMI-1) (12) that was conducted just prior to the pandemic.
Methods
TURKMI-2 was planned as a nationwide, observational, 15-day snapshot registry of patients presenting with acute MI during the COVID-19 pandemic. The Institutional Review Board of Ankara University Medical School, Turkey (May 2020; No: i4-225-20) and the Ministry of Health COVID-19 Scientific Board (May 2020; No: 66175679.99.E.110223) approved the protocol and informed consent was obtained from all participants.
The previous TURKMI study (clinicaltrials.gov NCT04241770) was also a 15-day registry (November 1-15, 2018) that prospectively enrolled patients with acute MI in Turkey (12, 13). All consecutive patients admitted to the hospital within 48 hours of symptom-onset were registered in TURKMI-1. Fifty cardiology centers capable of 24/7 service for primary percutaneous coronary intervention (PCI) were selected in the 12 Eurostat NUTS statistical regions of Turkey proportional to the 2018 Turkey census. The clinical characteristics and delay at each step from symptom-onset to the appropriate treatment were assessed (12). In the present study (TURKMI-2 registry), the same information was obtained from the same centers during the COVID-19 pandemic. Of note, 2 centers of the former registry did not participate in the TURKMI-2 study. Accordingly, all consecutive patients presenting with acute MI during a 15-day period (April 17-May 2, 2020) at 48 centers that participated in the TURKMI-1 registry were enrolled. The inclusion criteria were the same as the original registry: 1) aged ≥18 years, 2) a final (discharge) diagnosis of acute MI, either ST elevation MI (STEMI) or non-STEMI (NSTEMI), with positive troponin levels, and 3) written, informed consent. Patients unwilling or unable to consent were excluded. The only difference between the 2 registries in terms of the inclusion criteria was the time frame from symptom-onset to hospital admission. The TURKMI-1 registry, conducted before the pandemic outbreak, only included patients admitted to the hospital within 48-hour of the onset of symptoms. Since some delays in admission due to the pandemic were expected, we included all of the acute MI patients in the TURKMI-2, regardless of the time of symptom-onset. However, for the comparison of pre-pandemic and pandemic data, we primarily focused on the patients who were admitted to the study centers within 48-hour of symptom-onset in both registries.
All outcomes and diagnoses were defined in accordance with the previous TURKMI-1 definitions (12-12). Patients who were admitted to emergency departments without emergency medical service (EMS) were accepted as self-transported. Major adverse cardiovascular events (MACE) were defined as the composite in-hospital endpoint of death, heart failure, or cardiogenic shock. The time variables between symptom-onset to hospital arrival obtained from each patient were the number of minutes reflecting symptom-onset to EMS contact (for those who called EMS), EMS contact to EMS arrival patient’s location, EMS arrival patient’s location to EMS arrival at the hospital, and time for transportation from a non-PCI-capable hospital to a PCI-capable study center (for transferred patients). The sum of these variables was defined as symptom-onset to hospital arrival. Door-to-balloon time was defined as the time between arrival at the study center and balloon inflation in the culprit artery for STEMI patients and, similarly, door-to-needle time was calculated for those who received fibrinolytic treatment. Total ischemic time was defined as the time from symptom-onset to balloon-inflation (or the initiation of fibrinolytic therapy) for STEMI patients. Since the indication for coronary angiography and PCI varies according to the risk categories in NSTEMI patients, the length of time from symptom-onset to arrival at the study centers was used to compare the delay in NSTEMI patients and all patients (STEMI+NSTEMI) between the 2 periods. During the study period, a lockdown was implemented for several days in major cities. Thus, the time variables were also compared between lockdown and non-lockdown periods in these major cities (Supplementary Online Material).
Statistical analysis
All of the analyses were performed using Predictive Analytics Software (PASW) for Windows, Version 18.0 (SPSS Inc., Chicago, IL, USA). Categorical variables are presented as the number and percentage and compared using chi-square or Fisher’s exact tests. Continuous variables are shown as mean and standard deviation or median and interquartile range (IQR), depending on the presence of normal distribution, and compared using an independent t-test or the Mann-Whitney U test. The risk of MACE for the pandemic versus non-pandemic periods was assessed using logistic regression analysis, adjusted for age and sex. Due to the observational nature of the registries and the second part of the study (TURKMI-2) occurring during the pandemic period, changes in the characteristics of patients admitted to the hospital between the 2 periods might create a selection bias in estimating the outcome risk. Therefore, we performed a sensitivity analysis to assess the potential selection bias. In this analysis, the period (pre-pandemic or pandemic) was modeled using a logit link function and covariates of age, sex, history of hypertension, diabetes mellitus, hyperlipidemia, smoking, coronary artery disease, and EMS use, and then inverse probability weighting was applied for the comparison of the risk of outcome between the 2 periods. The balance was assessed with standardized differences after weighting (all had ≤2%). A p value of <0.05 was considered significant.
Results
A total of 1113 patients with acute MI were admitted to the TURKMI-2 study centers during a 2-week period of the pandemic. We present the comparison of the previous TURKMI-1 and a subgroup of TURKMI-2 patients who were admitted to the study centers within 48-hour of symptom-onset. The details of the entire TURKMI-2 population in comparison with the TURKMI-1 registry are presented as supplementary material (Online text, eTable 1, and eFig. 1).
Table 1.
Characteristics, time delays, and in-hospital outcomes in patients with acute myocardial infarction admitted within the first 48 hours of symptom onset during the pandemic and pre-pandemic periods
| Characteristics | TURKMI-1 (Pre-pandemic registry) | TURKMI-2 (Pandemic registry) | P-All | P-NSTEMI | P-STEMI | ||||
|---|---|---|---|---|---|---|---|---|---|
| All (n=1872) | NSTEMI (n=1161) | STEMI (n=711) | All (n=991) | NSTEMI (n=506) | STEMI (n=485) | ||||
| Age, years | 62 (53-71) | 63 (54-72) | 60 (51-70) | 60 (51-69) | 61 (52-71) | 58 (49-66) | <0.001 | 0.050 | 0.012 |
| Age, years | 62 (13) | 63 (13) | 60 (14) | 60 (13) | 62 (12) | 59 (13) | |||
| Female | 492 (26.3) | 333 (28.7) | 159 (22.4) | 236 (23.8) | 138 (27.3) | 98 (20.2) | 0.149 | 0.557 | 0.373 |
| Hypertension (self-reported) | 922 (49.3) | 649 (55.9) | 273 (38.4) | 499 (50.4) | 278 (54.9) | 221 (45.6) | 0.575 | 0.717 | 0.013 |
| Diabetes | 633 (33.8) | 432 (37.2) | 201 (28.3) | 335 (33.8) | 184 (36.4) | 151 (31.1) | 0.996 | 0.742 | 0.286 |
| Smoking | 914 (48.8) | 513 (44.2) | 401 (56.4) | 432 (43.6) | 184 (36.4) | 248 (51.1) | 0.008 | 0.003 | 0.073 |
| Hypercholesterolemia (self-reported) | 215 (11.5) | 148 (12.7) | 67 (9.4) | 256 (25.8) | 148 (29.2) | 108 (22.3) | <0.001 | <0.001 | <0.001 |
| History of coronary artery disease | 528 (28.2) | 406 (35) | 122 (17.2) | 283 (28.7) | 190 (37.8) | 93 (19.3) | 0.767 | 0.273 | 0.346 |
| Infarct localization | |||||||||
| Anterior | - | - | 340 (48.1) | - | - | 238 (49.1) | - | - | 0.739 |
| Inferior (±posterior) | - | - | 367 (51.9) | - | - | 247 (50.9) | |||
| Mode of Admission to hospital (study center) | |||||||||
| By Ambulance | 213 (11.7) | 88 (7.8) | 125 (17.9) | 205 (20.7) | 77 (15.2) | 128 (26.4) | <0.001 | <0.001 | <0.001 |
| Transfer from a non-PCI-capable hospital | 694 (38.1) | 419 (37.3) | 275 (39.3) | 391 (39.5) | 185 (36.6) | 206 (42.5) | 0.477 | 0.772 | 0.281 |
| Self-transport | 915 (50.2) | 616 (54.9) | 299 (42.8) | 395 (39.9) | 244 (48.2) | 151 (31.1) | <0.001 | .0013 | <0.001 |
| Mode of admission to study center for those | |||||||||
| transferred from a non-PCI-capable center | |||||||||
| By Ambulance | - | - | - | 131 (34) | 59 (32.6) | 72 (35.3) | - | - | - |
| Self-transport | - | - | - | 254 (66) | 122 (67.4) | 132 (64.7) | |||
| Time delays | |||||||||
| Symptom-onset to EMS call, min | 52.5 (15-170) | 67.5 (15-290) | 32.5 (15-120) | 90 (30-240) | 125 (30-315) | 80 (30-195) | 0.001 | 0.080 | 0.003 |
| EMS call to EMS arrival, min | 15 (10-20) | 15 (10-20) | 15 (10-20) | 15 (10-20) | 15 (10-20) | 15 (15-20) | <0.001 | 0.103 | <0.001 |
| Time delay for those transferred from a | 169 (99-300) | 235.5 (120-390) | 120 (63-180) | 180 (90-296) | 265 (135-390) | 120 (60-186.5) | 0.691 | 0.084 | 0.710 |
| non-PCI-capable hospital, min | |||||||||
| Symptom-onset to hospital (study center) arrival, min | 215.5 (90-473) | 295 (120-582.5) | 150 (70-300) | 270 (120-630) | 419 (180-840) | 185 (100-360) | <0.001 | <0.001 | <0.001 |
| Transferred from a non-PCI-capable center | 332 (180-635) | 424 (260-763) | 240 (145-365) | 390 (210-690) | 512 (360-930) | 240 (167-453) | 0.036 | <0.001 | 0.125 |
| Directly admitted to the study center | 135 (60-370) | 180 (74-450) | 100 (56-240) | 181 (90-550) | 275 (120-785) | 145 (70-303) | <0.001 | <0.001 | <0.001 |
| (by EMS or self-transport) | |||||||||
| In-hospital procedures and times | |||||||||
| Coronary angiography | 1758 (93.9) | 1054 (90.8) | 704 (99) | 871 (87.9) | 396 (78.3) | 475 (97.9) | <0.001 | <0.001 | 0.122 |
| Fibrinolytic therapy | - | - | 13 (1.8) | - | - | 11 (2.3) | - | - | 0.594 |
| PCI | 1374 (73.4) | 700 (60.3) | 674 (94.8) | 682 (68.8) | 240 (47.4) | 442 (91.1) | 0.010 | <0.001 | 0.013 |
| Door-to-needle time, min | 30 (15-60) | ||||||||
| Door-to-balloon time, min | - | - | 37 (25-65) | - | - | 40 (25-68) | - | - | 0.448 |
| Total ischemic time, min | - | - | 195 (115-331) | - | - | 245 (149-469) | - | - | <0.001 |
| Time from arrival to study center to | - | 1050 (300-2095) | - | - | 501.5 (134-1225) | - | - | <0.001 | - |
| Coronary angiography for NSTEMIs | |||||||||
| In-hospital outcomes | |||||||||
| MACE (death, heart failure, or cardiogenic shock) | 90 (4.8) | 40 (3.4) | 50 (7.0) | 88 (8.9) | 30 (5.9) | 58 (12.0) | <0.001 | 0.020 | 0.004 |
| Death | 71 (3.8) | 33 (2.8) | 38 (5.3) | 31 (3.1) | 8 (1.6) | 23 (4.7) | 0.361 | 0.126 | 0.642 |
| Heart failure or cardiogenic shock | 53 (2.8) | 23 (2) | 30 (4.2) | 82 (8.3) | 28 (5.5) | 54 (11.1) | <0.001 | <0.001 | <0.001 |
Data were expressed as mean (SD), median (interquartile range), or n (%). EMS - emergency medical service call; MACE - major adverse cardiac events; MI - myocardial infarction; NSTEMI - non-ST elevation MI; PCI - percutaneous coronary intervention; STEMI - ST elevation MI
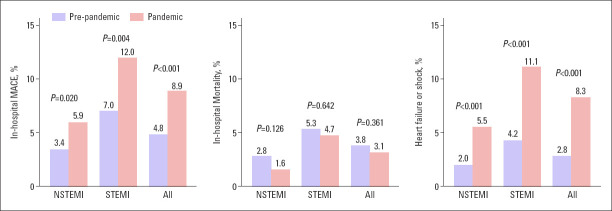
Figure 1.
Decreased number of the patients with acute myocardial infarction during the pandemic (TURKMI-2) compared to the non-pandemic period (TURKMI-1) in the patient cohort admitted to the study centers within 48 hours of symptom onset
MI - myocardial infarction, NSTEMI - non-ST elevation MI, STEMI - ST elevation MI
Characteristics of the TURKMI-1 and TURKMI-2 registries
Table 1 displays the baseline characteristics, delays, and in-hospital outcomes of the patients in the pre-pandemic and pandemic periods. There were no significant differences between the 2 registries in terms of the sex, the presence of diabetes mellitus or hypertension, history of coronary artery disease, or the MI location.
Change in the number of admissions
Among the patients registered in the TURKMI-2, 991 patients were admitted to the hospital within 48-hour of symptom-onset (51.1% NSTEMI and 48.9% STEMI). A total of 1872 patients were enrolled in the TURKMI-1 (62.0% NSTEMI and 38.0% STEMI). Acute MI admissions decreased by 47.1% during the pandemic time frame studied. This reduction in admission was more prominent in patients with NSTEMI compared with STEMI (56.4% vs. 31.8%, respectively, Fig. 1).
EMS call and delays
EMS transport significantly increased during the pandemic period (11.7% vs. 20.7%; p<0.001), though EMS transport use was very low in both registries. Changes in EMS transport were similar in NSTEMI and STEMI patients. The time elapsed between symptom-onset to EMS call was significantly prolonged in the pandemic period (median 52.5 min vs 90 min, p<0.001 for all; 67.5 min vs. 125 min for NSTEMI, p=0.080; 32.5 min vs. 80 min for STEMI, p=0.003). Though the difference between EMS arrivals was not “clinically’’ significant; and the median time was 15 minutes for both NSTEMI and STEMI patients in both periods. The median time for EMS arrival to the hospital was 20 min vs. 19 min for NSTEMI patients and 20 min vs. 20 min for STEMI patients in the TURKMI-1 and the TURKMI-2 studies, respectively. Moreover, there were no statistically significant differences in the time delay for patients who were transferred from a non-PCI-capable hospital when the pre-pandemic and pandemic periods were compared.
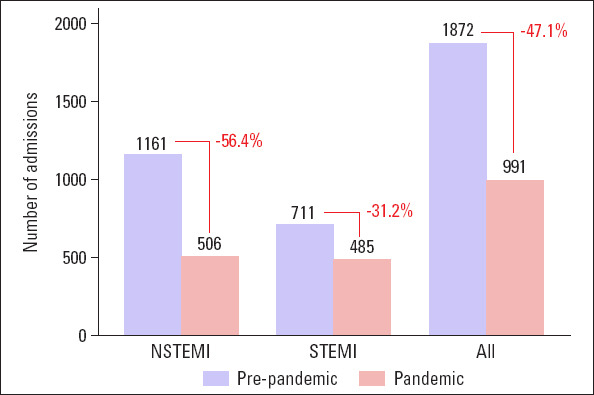
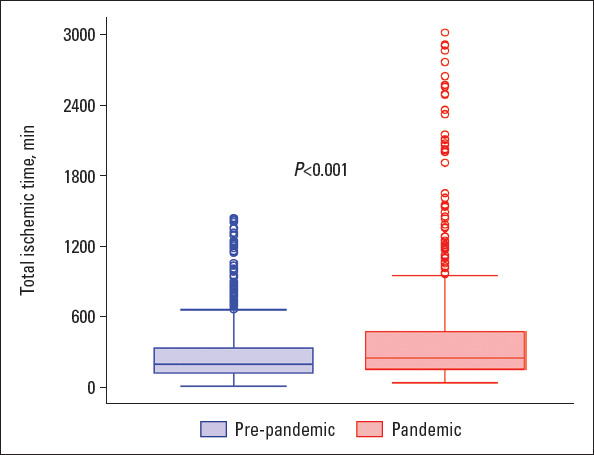
The time elapsed between symptom-onset to study center arrival was significantly longer during the pandemic compared with the pre-pandemic period (median arrival delay: 215.5 min vs. 270 min in total, p<0.001) and was more prominent in the NSTEMI group. The total ischemic time for patients with STEMI who were treated with PCI was significantly longer during the pandemic period compared with the pre-pandemic period (Fig. 2). However, the door-to-balloon time was similar between the 2 registries. Time delays at each step for STEMI patients transferred directly to the study centers using EMS are presented in Figure 3. Of note, the time from hospital arrival to coronary angiography for NSTEMI patients was significantly less during the pandemic period (median 1050 min for TURKMI-1 vs. 502 min for TURKMI-2; p=0.001).
Figure 2.
The total ischemic times for patients with ST elevation myocardial infarction who were treated with percutaneous coronary intervention were significantly longer during the pandemic period compared with the pre-pandemic period (median 195 min for TURKMI-1 vs. 245 min for TURKMI-2; p<0.001)
Figure 3.
Comparison of treatment delays in patients admitted with acute myocardial infarction during the pandemic (TURKMI-2) and pre-pandemic (TURKMI-1) periods. Time to treatment was significantly lengthened due to patient-related delays in the pandemic period. Meanwhile, symptom-to-EMS call, EMS call-to-EMS arrival, EMS arrival at the hospital, and door-to-balloon times were similar in the pre-pandemic and pandemic periods
EMS - emergency medical service
In-hospital management and outcomes
There was a significant reduction in the overall frequency of coronary angiography during the pandemic period compared to the pre-pandemic period. However, the reduction was significant only in the NSTEMI group. The frequency of PCI decreased significantly in both NSTEMI and STEMI patients during the pandemic. However, when STEMI patients who were admitted to the hospital within the guideline-recommended time frame of 12 hours were evaluated, there was no significant drop in the frequency of PCI treatment between the pre-pandemic and pandemic periods (574, 94.9% vs. 387, 92.1%, respectively; p=0.075). Meanwhile, the rate of fibrinolytic treatment was very low and statistically similar in the two registries. Of note, the number of patients who received fibrinolytic therapy was very low (13 and 11 patients in the pre-pandemic and pandemic period, respectively); therefore, we excluded these patients from the analysis of in-hospital timings.
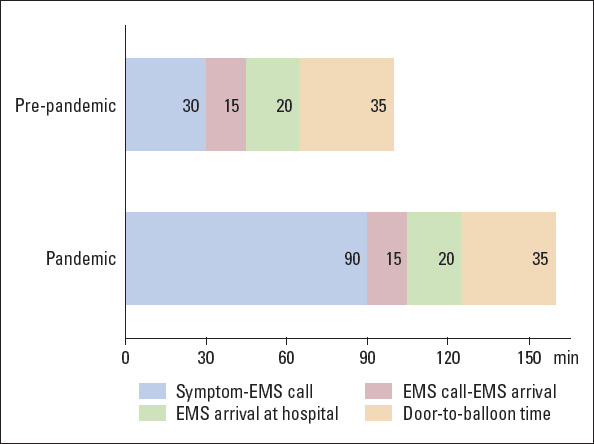
MACE was more common in the pandemic period compared to the pre-pandemic period (Fig. 4). The age- and sex-adjusted risk of MACE was 2 times higher in the pandemic period compared to the pre-pandemic period due to the increased risk of heart failure or cardiogenic shock [Odds ratio (95% confidence interval) was 1.96 (1.20–3.22) for NSTEMI, p=0.007 and 2.08 (1.38–3.13) for STEMI, p<0.001]. Sensitivity analysis for potential selection bias did not change the main outcome findings [Odds ratios and confidence intervals were 1.97 (1.18–3.30), p<0.010 for NSTEMI; and 1.79 (1.18–2.70), p=0.006 for STEMI].
Figure 4.
Comparison of the in-hospital major adverse events (defined as death, cardiogenic shock, or heart failure) between the pre-pandemic (TURKMI-1) and pandemic (TURKMI-2) periods
MACE - major adverse cardiac events, NSTEMI - non-ST elevation myocardial infarction STEMI - ST elevation myocardial infarction
Effect of lockdown period
The enrolment period of the TURKMI-2 registry covered a total of 8 days of lockdown circumstances. A comparison of patients admitting during the lockdown versus non-lockdown days is presented in the supplementary online text and eTable 2.
Discussion
Data from two nationwide TURKMI registries collected before and during the pandemic provide important insights into the impact of the COVID-19 pandemic on patients presenting with acute MI. Our results are based on the largest acute MI population studied during the COVID-19 outbreak. The results show that acute MI admissions decreased by 47.1%, with a significant treatment delay due to increased time from symptom-onset to EMS call or symptom-onset to first medical contact. These findings reflect patient-related delays during the pandemic (Fig. 3). The significant decrease (47.1%) in the number of acute MI admissions was consistent with previous reports of a 30–48.4% average reduction in acute MI presentations since the emergence of the COVID-19 outbreak (6, 8, 9, 15-20). The reduction was more pronounced in patients with NSTEMI (56.4%) compared with STEMI (31.8%), probably due to the symptom severity leading to patients seeking medical care.
The use of EMS transport was significantly greater during the pandemic compared with the pre-pandemic period. The increased use of EMS may have been due to several factors. Fear of acquiring COVID-19 may have led patients with more severe symptoms to seek medical attention via EMS. Also, the low EMS usage during the TURKMI-1 period was made public and the increased EMS use may be the effects of the successful awareness campaigns. Furthermore, restrictions on self-transport during lockdown may have contributed to the increased use of EMS.
Our results demonstrated a significant delay from symptom-onset to EMS calls for patients transported by ambulance and symptom-onset to hospital admission time for those who used self-transport. However, there were no “clinically” significant delays between the pre-pandemic and pandemic periods in terms of the EMS call to EMS arrival or the EMS arrival to hospital admission. The door-to-balloon time did not significantly change during the pandemic period. Overall, these results indicate that EMS and in-hospital care of patients with STEMI did not change during the pandemic period. Accordingly, our main findings indicate that the major time delay leading to a significantly prolonged treatment delay was patient-related (Fig. 3). Several studies have evaluated the delay in first medical contact or door-to-balloon time; (6, 10, 16-18, 21) however, only 1 study, which included 9 patients during the pandemic, assessed all of the stages from symptom-onset to balloon dilatation (17). Our study provides detailed information about delays at each step in a large nationwide population. The patient-related delay probably arose from the fear of contracting COVID-19 in the EMS ambulance or the hospital. Therefore, only patients with more severe symptoms eventually sought medical care and admittance to healthcare services. This fact is probably the explanation for the more pronounced drop observed in the number of NSTEMI cases compared with STEMI during the pandemic period. However, such a fear causing a refrain from seeking medical attention could be a primary denominator of increased mortality and heart failure in future as the delay in the treatment is the major determinant of infarct size and survival.
The percentage of patients who underwent coronary angiography significantly declined during the pandemic only in NSTEMI patients. The proportion of patients who underwent PCI decreased in both the NSTEMI and STEMI groups; however, the reduction was substantial only in NSTEMI patients. The low referral to coronary procedures for NSTEMI patients might be due to the preferential selection of patients with high-risk characteristics for invasive procedures during the pandemic period. PCI rates were not decreased in STEMI patients who were admitted to the study centers within 12 hours of symptom-onset, reflecting the maintenance of guideline-recommended practice during the pandemic. Therefore, we suggest that the overall decrease in PCI rates was probably due to the late admission of patients during the COVID-19 breakout.
In NSTEMI patients, the duration between hospital arrival and coronary angiography was significantly shorter in the pandemic cohort compared with the pre-pandemic cohort. This may be due to the efforts to decrease the length of hospital stay. Additionally, the deferral of elective invasive procedures may have shortened the wait-time for elective coronary procedures in NSTEMI patients. Furthermore, patients with subtle or mild symptoms hesitated to seek care during pandemic conditions. Therefore, these patients were admitted later than the appropriate time frame with more serious symptoms, i.e. most NSTEMI patients probably presented after their condition has deteriorated. Patients would then have presented with relatively high risk, which required rapid intervention, shortening the time between hospital arrival and coronary angiography.
Another major finding of this study was that MACE were increased significantly during the pandemic period. The proportion of patients with MACE was significantly higher in the pandemic period mainly due to increased heart failure or cardiogenic shock. The increased risk of MACE may have been caused by the prolonged treatment delay in the pandemic period. There were no differences in mortality between the 2 registries. The marked increase in mortality, since the emergence of the outbreak, cannot be fully explained by COVID-19 alone, which raises the possibility of patients dying of acute coronary events due to medical care avoidance (22). As the present study included only patients who arrived alive at the study centers, some patients with high-risk characteristics for mortality were eliminated, which may have resulted in a survival bias.
To the best of knowledge, our study is the first to report a comparison of the lockdown and non-lockdown days during the pandemic period. There were no substantial differences with regard to EMS use, delays, or development of MACE between the lockdown and non-lockdown days in the major cities (n=15) of the TURKMI-2 study. Further details on the impact of lockdown are presented in the Supplementary Online Material.
Study limitation
The lack of seasonal synchronization between the registries is a limitation of the study. However, previous studies have shown that the effects of seasonal variations on prevalence, outcomes, or characteristics of acute MI presentations are <10% (23). A second limitation of the study is the source of time data. The time measurements were obtained from the patients, their relatives, and during the hospitalization period, from the attending physicians. There might be an accurate recall problem. However, as the same method was used in both registries, the effect on the comparison of the delays should be negligible. A third limitation is that the pandemic may have affected patient behavior when seeking medical care and, as in all observational studies, changes in patient characteristics may lead to a biased estimation of the outcome risk. Although the sensitivity analysis did not change the main results, we cannot completely exclude potential bias. A fourth limitation is the preference of PCI-capable centers for conducting the registries, which may have led to the low number of patients receiving fibrinolytic therapy. However, we deliberately selected the PCI-capable centers because these centers constitute the widespread practice in Turkey. We assumed that patients with MI were eventually admitted to these centers within 48 hours of symptom-onset. Finally, this study was conducted within a 2-week period 1 month after the detection of the first COVID-19 cases in Turkey. Therefore, the results may not be generalizable to other countries. However, the human response to disasters, such as fear of contracting with COVID-19 in the pandemic, is unique.
Conclusion
The TURKMI-2 study, as the largest, relevant nationwide registry, revealed that admissions of acute MI were almost halved during the pandemic compared with the pre-pandemic period. Time to treatment was significantly prolonged, largely due to patient-related delays during the pandemic period. Door-to-balloon time was not affected. Accordingly, the in-hospital MACE rate was increased significantly. Therefore, specific measures, such as increasing public awareness and establishing COVID-free hospitals, may reduce the fear of acquiring infection and mitigate the potential complications of acute MI during the pandemic.
Acknowledgments:
Statistical analyses were conducted by Omega CRO, Ankara, Turkey. The same electronic case report forms and data capture program were used for both registries (OpenClinica LLC and collaborators, Waltham, MA, USA, hosted by Omega CRO, Ankara, Turkey). Both TURKMI registries are investigator-initiated trials sponsored by the Turkish Society of Cardiology, which receives major unrestricted funding from Astra-Zeneca Company for this project. The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
TURKMI-2 Study Group: Abant Izzet Baysal University: Mehmet Cosgun, Mehmet Inanir, Osman Yasin Yalçin, Yilmaz Gunes; Adana City Hospital: Abdullah Yildirim, Omer Genc, Ibrahim Halil Kurt; Adiyaman University: Ramazan Asoglu; Aksaray University: Sinan Inci; Ankara University: Mustafa Kilickap; Ankara City Hospital, Cagrı Yayla, Mehmet Akif Erdol, Mustafa Cetin, Ahmet Goktuğ Ertem, Ender Ornek; Antalya Training and Research Hospital : Gulsum Meral Yılmaz Oztekin, Ahmet Genc; Batman State Hospital: Mesut Gitmez; Bursa Yuksek Ihtisas Training and Research Hospital; Veysi Can, Soner Aksuyek, Hasan Ari; Canakkale Onsekiz Mart University; Emine Gazi; Cukurova University; Anil Akray, Onur Sinan Deveci; Denizli State Hospital: Okan Er; Diyarbakir Gazi Yasargil Training and Research Hospital: Onder Ozturk; Ege University: Aytac Candemir, Meral Kayikçioglu, Oguz Yavuzgil; Erzincan Binali Yildirim University: Eftal Murat Bakirci, Husnu Degirmenci; Harran University: Halil Fedai, Feyzullah Besli; Istanbul Bagcılar Training and Research Hospital: Orhan Ince, Emirhan Hancıoglu; Istanbul Bakirkoy Sadi Konuk Training and Research Hospital: Ersan Oflar, Ibrahim Faruk Akurk, Nihan Turhan Çaglar; Istanbul Bezmi Alem University: İlke Celikkale Hatice Aylin Yamac Halac; Istanbul Haseki Training and Research Hospital: Muhsin Kalyoncuoglu; Istanbul Kartal Kosuyolu Training and Research Hospital: Cagri Kafkas, Dogancan Ceneli, Nesri Danisman, Mesut Karatas, Cevat Kirma; Istanbul Mehmet Akif Ersoy Training and Research Hospital: Arda Guler, Cemil Can, Arda Can Dogan, Ahmet Arif Yalcin, Alkim Ateslioguz; Istanbul International Sisli Kolan Hospital: Mustafa Kemal Erol; Istanbul Siyami Ersek Training and Research Hospital: Can Baba Arin, Furkan Durak; Istanbul University Cardiology Institute; Umit Yasar Sinan; Izmir Tepecik Training and Research Hospital: Murat Kücükokur, Oner Ozdogan; Kahramanmaras Sutcu Imam University: Ekrem Aksu, Musa Dagli; Kayseri Training and Research Hospital: Eyüp Ozkan, Ziya Simsek; Kırıkkale Yuksek Ihtisas Training and Research Hospital: Cengiz Sabanoğlu; Kutahya Health Science University: Fatih Kahraman, Taner Sen, Mehmet Ali Astarcioglu; Malatya Training and Research Hospital: Ibrahim Aktas; Marmara University: Mustafa Kursat Tigen, Murat Sunbul; Mersin University: Ayça Arslan, Ahmet Celik; Mustafa Kemal University: Oguz Akkus; Necmettin Erbakan University: Yakup Alsancak; Osmangazi University: Muhammet Dural, Kadir Ugur Mert; Mugla Yucelen Hospital: Nuri Kose; Pamukkale University: Ismail Dogu Kiliç; Recep Tayyip Erdogan University: Muhammed Mursel Ogutveren, Nadir Emlek; Sakarya University: Ibrahim Kocayigit; Samsun Training and Research Hospital: Mustafa Yenerçag, Ahmet Yanik; Trabzon Ahi Evran Training and Research Hospital: Ihsan Dursun, Omer Faruk Çitrakoglu; Trakya University: Utku Zeybey, Servet Altay; Urfa Mehmet Akif Inan Training and Research Hospital: Sadettin Selcuk Baysal; Van Training and Research Hospital: Nesim Aladag, Remzi Sarikaya, Abdulcebbar Sipas; Van Yuzuncu Yil University: Haşim Tüner, Mustafa Tuncer, Ramazan Duz; Yalova State Hospital: Ismail Ungan.
Conflict of interest: Dr. Kayıkçıoğlu reports grants from Astra Zeneca, during the conduct of the study; grants from Aegerion, other from Astra Zeneca, other from Menarini, non-financial support and other from Abbott, outside the submitted work; Dr. Aktaş, Dr. Kılıçkap, Dr. Zeybey, Dr. İnci, Dr. Er, Dr. Kahraman, Dr. Yayla, Dr. Kafkas, Dr. Yıldırım, Dr. Can, Dr. Erol, Dr. Yalçın, Dr. Güler, Dr. Genç, and Dr. Arın report non-financial support from Astra Zeneca, during the conduct of the study.
Peer-review: Internally peer-reviewed.
Authorship contributions: Concept – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap; Design – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap; Supervision – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap; Fundings – None; Materials – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap; Data collection and/or processing – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap; Analysis and/or interpretation – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap, A.G., A.Y., F.K., V.C., S.İ., S.S.B., O.E., U.Z., Ç.K., Ç.Y., C.B.A., İ.A., A.A.Y., Ö.G.; Literature search – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap, A.G., A.Y., F.K., V.C., S.İ., S.S.B., O.E., U.Z., Ç.K., Ç.Y., C.B.A., İ.A., A.A.Y., Ö.G.; Writing – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap; Critical review – M.K.Erol, M.Kayıkçıoğlu, M.Kılıçkap, A.G., A.Y., F.K., V.C., S.İ., S.S.B., O.E., U.Z., Ç.K., Ç.Y., C.B.A., İ.A., A.A.Y., Ö.G.
References
- 1.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation:The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–77. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 2.Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation:Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 3.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction:every minute of delay counts. Circulation. 2004;109:1223–5. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 4.Wijns W, Naber CK. Reperfusion delay in patients with high-risk ST-segment elevation myocardial infarction: every minute counts, much more than suspected. Eur Heart J. 2018;39:1075–7. doi: 10.1093/eurheartj/ehy069. [DOI] [PubMed] [Google Scholar]
- 5.Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, et al. Fewer Hospitalizations for Acute Cardiovascular Conditions During the COVID-19 Pandemic. J Am Coll Cardiol. 2020;76:280–8. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Firouzi A, Baay M, Mazayanimonfared A, Pouraliakbar H, Sadeghipour P, Noohi F, et al. Effects of the COVID-19 Pandemic on the Management of Patients With ST-Elevation Myocardial Infarction in a Tertiary Cardiovascular Center. Crit Pathw Cardiol. 2020 doi: 10.1097/HPC.0000000000000228. 10.1097/HPC.0000000000000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic:a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6:210–6. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, et al. The Covid-19 Pandemic and the Incidence of Acute Myocardial Infarction. N Engl J Med. 2020;383:691–3. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 9.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–3. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamadeh A, Aldujeli A, Briedis K, Tecson KM, Sanz-Sánchez J, Al Dujeili M, et al. Characteristics and Outcomes in Patients Presenting With COVID-19 and ST-Segment Elevation Myocardial Infarction. Am J Cardiol. 2020;131:1–6. doi: 10.1016/j.amjcard.2020.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erol MK, Kayıkçıoğlu M, Kılıçkap M. Rationale and design of the Turkish acute myocardial infarction registry: The TURKMI Study. Anatol J Cardiol. 2020;23:169–75. doi: 10.14744/AnatolJCardiol.2019.57522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erol MK, Kayıkçıoğlu M, Kılıçkap M, Arın CB, Kurt IH, Aktaş I, et al. Baseline clinical characteristics and patient profile of the TURKMI registry:Results of a nation-wide acute myocardial infarction registry in Turkey. Anatol J Cardiol. 2020;24:43–53. doi: 10.14744/AnatolJCardiol.2020.69696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Writing Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction; ESC Committee for Practice Guidelines (CPG). Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–67. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 15.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. SocietàItaliana di Cardiologia and the CCU Academy investigators group. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–8. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coughlan JJ, Chongprasertpon N, Arockiam S, Arnous S, Kiernan TJ. COVID-19 and STEMI:A snapshot analysis of presentation patterns during a pandemic. Int J Cardiol Heart Vasc. 2020:100546. doi: 10.1016/j.ijcha.2020.100546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdelaziz HK, Abdelrahman A, Nabi A, Debski M, Mentias A, Choudhury T, et al. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: Insights from a British cardiac center. Am Heart J. 2020;226:45–8. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2871–2. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Legutko J, Niewiara Ł, Bartuś S, Dobrzycki S, Gąsior M, Gierlotka M, et al. Decline in the number of coronary angiography and percutaneous coronary intervention procedures in patients with acute myocardial infarction in Poland during the coronavirus disease 2019 pandemic. Kardiol Pol. 2020;78:574–6. doi: 10.33963/KP.15393. [DOI] [PubMed] [Google Scholar]
- 20.De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020;383:88–9. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammad TA, Parikh M, Tashtish N, Lowry CM, Gorbey D, Forouzandeh F, et al. Impact of COVID-19 pandemic on ST-elevation myocardial infarction in a non-COVID-19 epicenter. Catheter Cardiovasc Interv. 2020 doi: 10.1002/ccd.28997. 10.1002/ccd.28997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Docherty K, Butt J, de Boer R, Dewan P, Koeber L, Maggioni A, et al. Excess deaths during the Covid-19 pandemic: An international comparison. medRxiv. 2020 04.21.20073114. [Google Scholar]
- 23.Nagarajan V, Fonarow GC, Ju C, Pencina M, Laskey WK, Maddox TM, et al. Seasonal and circadian variations of acute myocardial infarction: Findings from the Get With The Guidelines-Coronary Artery Disease (GWTG-CAD) program. Am Heart J. 2017;189:85–93. doi: 10.1016/j.ahj.2017.04.002. [DOI] [PubMed] [Google Scholar]