Abstract
Previous studies have found that the risk of suicide is higher in patients diagnosed with cancer than in the general population. We aimed to identify potential risk factors associated with suicide in leukemia patients by analyzing data obtained from the Surveillance, Epidemiology, and End Results (SEER) database. We screened the SEER database for leukemia patients added between 1975 and 2017, and calculated their suicide rate and standardized mortality rate (SMR) relative to the total United States population from 1981 to 2017 as a reference. Univariate and multivariate Cox regression analyses were used to determine the risk factors for suicide in leukemia patients. We collected 142,386 leukemia patients who had been added to the SEER database from 1975 to 2017, of whom 191 patients committed suicide over an observation period of 95,397 person‐years. The suicide rate of leukemia patients was 26.41 per 100,000 person‐years, and hence the SMR of the suicided leukemia patients was 2.16 (95% confidence interval [CI] = 1.85–2.47). The univariate and multivariate Cox regression analyses showed that a high risk of suicide was associated with male sex (vs. female: hazard ratio [HR] = 4.41, 95% CI = 2.93–6.63, p < 0.001), older age at diagnosis (60–69 years vs. ≤39 years: HR = 2.60, 95% CI = 1.60–4.23, p < 0.001; 70–79 years vs. ≤39 years: HR = 2.84, 95% CI = 1.72–4.68, p < 0.001; ≥80 years vs. ≤39 years: HR = 2.94, 95% CI = 1.65–5.21, p < 0.001), white race (vs. black: HR = 6.80, 95% CI = 1.69–27.40, p = 0.007), acute myeloid leukemia (vs. lymphocytic leukemia: HR = 1.59, 95% CI = 1.09–2.33, p = 0.016), unspecified and other specified leukemia (vs. lymphocytic leukemia: HR = 2.72, 95% CI = 1.55–4.75, p < 0.001), and living in a small city (vs. large city: HR = 2.10, 95% CI = 1.23–3.60, p = 0.007). Meanwhile, being a non‐Hispanic black (vs. Hispanic: HR = 0.06, 95% CI = 0.01–0.62, p = 0.019) was a protective factor for suicide. Male sex, older age at diagnosis, white race, and acute myeloid leukemia were risk factors for suicide in leukemia patients, while being a non‐Hispanic black was a protective factor. Medical workers should, therefore, provide targeted preventive measures to leukemia patients with a high risk of suicide.
Keywords: leukemia, risk factors, SEER, suicide
We aimed to identify potential risk factors associated with suicide in leukemia patients by analyzing data obtained from the Surveillance, Epidemiology, and End Results (SEER) database. Male sex, older age at diagnosis, white race, and acute myeloid leukemia were risk factors for suicide in leukemia patients, while being a non‐Hispanic black was a protective factor. Medical workers should therefore provide targeted preventive measures to leukemia patients with a high risk of suicide.
1. BACKGROUND
Suicide refers to an individual deliberately or voluntarily ending their own life under the action of complex psychological activities. 1 , 2 , 3 Suicide is a complex global social phenomenon. 4 , 5 The World Health Organization reports that 817,000 people died of suicide globally in 2016, accounting for 1.49% of the total number of deaths, and corresponding to one person committing suicide every 40 s. 6 The suicide mortality rate in the United States was 14.78 per 100,000 in 2018, which is relatively high compared with other countries. 7
The prevalence of cancer has been increasing worldwide in recent years, and it is now the third leading cause of death. 8 It was estimated that there were 18.1 million new cancer cases in 2018, with 9.6 million cancer deaths globally. 9 Cancer treatments previously focused on prolonging life, while neglected the huge losses caused by cancer patients and their families during a long course of treatment and rehabilitation, such as the financial burden and mental illness. 10 , 11 The increasing incidence of cancer is also increasing the incidence of mental illness in patients during diagnosis and treatment, such as depression, fear of cancer recurrence, and suicidal thoughts. 9 , 12 , 13 Several studies have found increases in suicidal ideation among cancer patients and that the suicide rate is higher in these patients. 2 , 3 , 4 , 14 , 15 , 16 , 17 , 18
The suicide rate in the United States is significantly higher in cancer patients than in the general population, with the suicide standardized mortality rate (SMR) reaching 4.44. 3 , 19 This situation indicates the importance of identifying the risk factors for suicide in cancer patients in order to be able to prevent their suicide behaviors. Some studies have found that male sex, white race, marital status, and other risk factors are strongly correlated with the suicide rate of patients with certain types of cancer, such as kidney cancer, breast cancer, lung cancer, and head and neck cancer. 13 , 20 , 21 , 22
Leukemia is a type of malignant proliferative disease involving hematopoietic stem cells. 23 There were 437,033 new leukemia patients identified worldwide in 2018, accounting for 2.4% of all new cancer patients and ranking 15th among new cancer patients. 9 Leukemia is a clinically common malignant tumor in the United States. 24 Several studies have analyzed potential risk factors associated with suicide in common cancers in the United States using data obtained from the Surveillance, Epidemiology, and End Results (SEER) database. 13 , 19 , 21 , 25 However, no research into the relationship between leukemia and suicide has been reported in the literature. Therefore, the purpose of this study was to identify the potential risk factors related to leukemia and suicide by analyzing the SEER database.
2. METHODS
2.1. Data source
The SEER database of the National Cancer Institute covers 30% of the United States population and is considered to be representative of that population. 26 , 27 The SEER database provides registered researchers with free access to a large amount of research materials, including patient demographic, cancer incidence, and survival data. All of the leukemia patients selected for inclusion in this study had been added to the SEER database between 1975 and 2017. We obtained permission to access the database after signing and submitting the SEER Research Data Agreement form via email. The SEER*Stat software (version 8.3.6) was used to identify relevant patients for inclusion in this study.
2.2. Study population and inclusion criteria
We collected all leukemia patients diagnosed during 1975–2017 as defined by International Classification of Disease for Oncology codes (third edition). Patients were identified using the primary site code (C42.1) and morphology codes (9800–9948) for leukemia. We considered that suicide had occurred in cases in which the cause of death was coded as “suicide and self‐mutilation.” The exclusion criteria included patients with incomplete variables and no diagnosis or microscopy findings. The information collected for all patients included the year of diagnosis, age at diagnosis, sex, race, type of leukemia, surgery status, survival period, and cause of death. The application of our selection criteria identified 142,386 leukemia patients who had been added to the SEER database from 1975 to 2017, of whom 191 had suicided. The steps used to select leukemia patients for inclusion in this study are shown in Figure 1.
FIGURE 1.
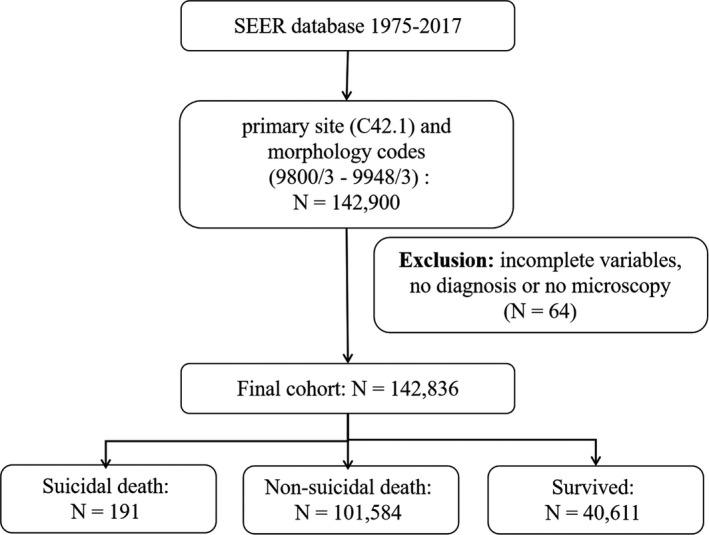
The flow diagram of leukemia patient selection
2.3. Statistical analysis
We divided the patients into the following three groups to allow basic data comparisons: suicidal death, non‐suicidal death, and survival. The chi‐square test was used to compare suicide rates among patients in the different groups. We used the Web‐Based Injury Statistics Query and Reporting System of the United States Centers for Disease Control and Prevention (CDC) 7 to calculate the SMR values for suicide in each group, with the general population of the United States from 1981 to 2018 used as the reference. The 95% confidence interval (CI) of the SMR was obtained using Byar's approximation. 28 Subsequent univariate and multivariate Cox regression analyses were used to generate raw and adjusted hazard ratios (HR) and their associated 95% CI for identifying potential risk factors for suicide. All statistical analyses were performed using R software (version 3.6.3). All tests were double‐sided and had a significance criterion of p < 0.05.
3. RESULTS
3.1. Baseline characteristics of the patients
The 142,386 identified leukemia patients included 81,600 males (57.3%). While 191 patients died of suicide (0.13%), 101,574 patients died of other causes (71.34%) and 40,611 survived (28.53%). Most of the entire study population was older than 60 years (65.1%), white (86.3%), non‐Latin (94.4%), non‐Hispanic whites (81.1%), had lymphocytic leukemia (50.7%), and lived in a city (62.2%). The distribution was similar for the 191 suicided patients. The basic demographic data of each group of leukemia patients are presented in Table 1.
TABLE 1.
Baseline characteristics of leukemia patients (1975–2017)
| Variables | Overall N (%) | Suicidal death N (%) | Non‐suicidal death N (%) | Survived N (%) |
|---|---|---|---|---|
| Patients | 142,386 | 191 | 101,584 | 40,611 |
| Year of diagnosis | ||||
| 1975–1984 | 23,382 (16.4%) | 40 (21.0%) | 22,110 (21.8%) | 1232 (3.0%) |
| 1985–1994 | 28,200 (19.8%) | 44 (23.0%) | 25,075 (24.7%) | 3081 (7.6%) |
| 1995–2004 | 34,324 (24.1%) | 42 (22.0%) | 26,657 (26.2%) | 7625 (18.8%) |
| 2005–2017 | 56,480 (39.7%) | 65 (34.0%) | 27,742 (27.3%) | 28,673 (70.6%) |
| Sex | ||||
| Male | 81,600 (57.3%) | 164 (85.9%) | 58,140 (57.2%) | 23,296 (57.4%) |
| Female | 60,786 (42.7%) | 27 (14.1%) | 43,444 (42.8%) | 17,315 (42.6%) |
| Age at diagnosis | ||||
| ≤39 | 22,098 (15.5%) | 28 (14.7%) | 9377 (9.2%) | 12,693 (31.3%) |
| 40–49 | 9287(6.5%) | 13 (6.8%) | 5208 (5.1%) | 4066 (10.0%) |
| 50–59 | 18,324 (12.9%) | 21 (11.0%) | 11,098 (10.9%) | 7205 (17.7%) |
| 60–69 | 29,198 (20.5%) | 52 (27.2%) | 20,675 (20.4%) | 8471 (20.9%) |
| 70–79 | 34,407 (24.2%) | 48 (25.1%) | 28,640 (28.2%) | 5719 (14.1%) |
| ≥80 | 29,072 (20.4%) | 29 (15.2%) | 26,586 (26.2%) | 2457 (6.1%) |
| Race | ||||
| White | 122,819 (86.3%) | 185 (96.9%) | 88,518 (87.1%) | 34,116 (84.0%) |
| Black | 10,402 (7.3%) | 2 (1.0%) | 7513 (7.4%) | 2887 (7.1%) |
| Other | 8263 (5.8%) | 4 (2.1%) | 5400 (5.3%) | 2859 (7.0%) |
| Unknown | 902 (0.6%) | 0 (0.0%) | 153 (0.2%) | 749 (1.9%) |
| Race Latino | ||||
| Latino | 7912 (5.6%) | 13 (6.8%) | 4471 (4.4%) | 3428 (8.4%) |
| Non‐Latino | 134,474 (94.4%) | 178 (93.2%) | 97,113 (95.6%) | 37,183 (91.6%) |
| Race Hispanic | ||||
| Hispanic | 7712 (5.4%) | 13 (6.8%) | 4471 (4.4%) | 3428 (8.4%) |
| Non‐Hispanic White | 115,506 (81.1%) | 173 (90.6) | 84,425 (83.1%) | 30,908 (76.1%) |
| Non‐Hispanic Black | 10,269 (7.2%) | 2 (1.0%) | 7444 (7.3%) | 2823 (7.0%) |
| Non‐Hispanic Asian | 7336 (5.2%) | 3 (1.6%) | 4857 (4.8%) | 2476 (6.1%) |
| Non‐Hispanic American Indian Native | 761 (0.5%) | 0 (0.0%) | 449 (0.4%) | 312 (0.8%) |
| Non‐Hispanic unknown race | 802 (0.6%) | 0 (0.0%) | 138 (0.1%) | 664 (1.6%) |
| Type of leukemia | ||||
| Lymphoid leukemia | 72,132 (50.7%) | 111 (58.1%) | 43,857 (43.2%) | 28,164 (69.4%) |
| Acute myeloid leukemia | 41,290 (29.0%) | 38 (19.9%) | 35,111 (34.6%) | 6141 (15.1%) |
| Chronic myeloproliferative diseases | 15,247 (10.7%) | 22 (11.5%) | 10,257 (10.1%) | 4968 (12.2%) |
| Myelodysplastic syndrome and other myeloproliferative | 3838 (2.7%) | 3 (1.6%) | 3274 (3.2%) | 561 (1.4%) |
| Unspecified and other specified leukemia | 9879 (6.9%) | 17 (8.9%) | 9085 (8.9%) | 777 (1.9%) |
| Surgery performed | ||||
| Yes | 81,180 (57.0%) | 93 (48.7%) | 46,384 (45.7%) | 34,703 (85.5%) |
| No | 61,206 (43.0%) | 98 (51.3%) | 55,200 (54.3%) | 5908 (14.5%) |
| Primary diseases | ||||
| Yes | 107,367 (75.4%) | 147 (77.0%) | 74,604 (73.4%) | 32,616 (80.3%) |
| No | 35,019 (24.6%) | 44 (23.0%) | 26,980 (26.6%) | 7995 (19.7%) |
| Chemotherapy | ||||
| Yes | 71,857 (50.5%) | 91 (47.6%) | 51,211 (50.4%) | 20,555 (50.6%) |
| No | 70,529 (49.5%) | 100 (52.4%) | 50,373 (49.6%) | 20,056 (49.4%) |
| Household income | ||||
| <$50,000 | 10,412 (7.3%) | 13 (6.8%) | 6518 (6.4%) | 3881 (9.6%) |
| $55,000–$74,999 | 52,348 (36.8%) | 63 (33.0%) | 33,197 (32.7%) | 19,088 (47.0%) |
| >$75,000 | 42,529 (26.9%) | 53 (27.7%) | 27,378 (27.0%) | 15,098 (37.2%) |
| Unknown | 37,097 (26.0%) | 62 (32.5%) | 34,491 (33.9%) | 2544 (6.2%) |
| Living area a | ||||
| Large city | 58,952 (41.4%) | 62 (32.5%) | 36,985 (36.4%) | 21,905 (53.9%) |
| Medium city | 22,170 (15.6%) | 25 (13.1%) | 13,621 (13.4%) | 8524 (21.0%) |
| Small city | 7513 (5.3%) | 17 (8.9%) | 4801 (4.7%) | 2695 (6.6%) |
| Suburbs | 7960 (5.6%) | 13 (6.8%) | 5510 (5.4%) | 2437 (6.0%) |
| Rural | 7629 (5.4%) | 10 (5.2%) | 5296 (5.2%) | 2323 (5.8%) |
| Unknown | 38,162 (26.8%) | 64 (33.5%) | 35,371 (34.8%) | 2727 (6.7%) |
Large city, Counties in metropolitan areas of 1 million pop; Medium city, Counties in metropolitan areas of 250,000 to 1 million pop; Small city, Counties in metropolitan areas of lt 250 thousand pop; Suburbs, Nonmetropolitan counties adjacent to a metropolitan area; Rural, Nonmetropolitan counties not adjacent to a metropolitan area; Unknown, Unknown/missing/no match/Not 1990–2017.
3.2. Suicide rates and SMRs for the leukemia patients
The 142,386 leukemia patients included 191 patients who committed suicide over an observation period of 723,261 person‐years, giving a suicide rate of 26.41 per 100,000 person‐years. During the same period, the suicide rate in the general United States population was 12.24 per 100,000 person‐years, 7 and so the SMR was 2.16 (95% CI = 1.85–2.47). The suicide rate was higher for the following characteristics than in the corresponding general United States population: male sex (SMR = 2.04: 95% CI = 1.75–2.39), older age at diagnosis (60–69 years: SMR = 2.40, 95% CI = 1.77–3.10; 70–79 years: SMR = 2.64, 95% CI = 1.97–3.54; ≥80 years: SMR = 2.99, 95% CI = 1.94–4.17), and white race (SMR = 2.11, 95% CI = 1.81–2.43). The suicide rate for the following characteristics did not differ from that in the corresponding general United States population: middle‐aged (40–49 years: SMR = 1.12, 95% CI = 0.58–1.85, p = 0.687; 50–59 years: SMR = 0.98, 95% CI = 0.62–1.53, p = 0.943), black race (SMR = 0.80, 95% CI = 0.11–3.61, p = 0.999), Asian race (SMR = 0.73, 95% CI = 0.73–2.19, p = 0.607), and living in a rural area (SMR = 2.38, 95% CI = 1.20–4.60, p = 0.054). The data for the suicide rate and SMR of the leukemia patients are presented in Table 2.
TABLE 2.
Suicide rates and SMRs among patients with leukemia (1975–2017)
| Variables | Suicidal death | Person‐years | Suicide rate per 100,000 person‐years | p | SMR b | 95%CI | |
|---|---|---|---|---|---|---|---|
| Patients | 191 | 723,261 | 26.41 | <0.001*** | 2.16 | (1.85, 2.47) | |
| Year of diagnosis | |||||||
| 1975–1984 | 40 | 132,341 | 30.22 | <0.001*** | 2.47 | (1.79, 3.4) | |
| 1985–1994 | 44 | 181,675 | 24.22 | <0.001*** | 1.98 | (1.45, 2.68) | |
| 1995–2004 | 42 | 216,971 | 19.36 | 0.003** | 1.58 | (1.12, 2.1) | |
| 2005–2017 | 65 | 192,274 | 33.81 | <0.001*** | 2.76 | (2.09, 3.45) | |
| Sex | |||||||
| Male | 164 | 410,443 | 39.96 | <0.001*** | 2.04 | (1.75, 2.39) | |
| Female | 27 | 312,818 | 8.63 | 0.006** | 1.68 | (1.11, 2.46) | |
| Age at diagnosis | |||||||
| ≤39 | 28 | 215,668 | 12.98 | 0.023* | 1.53 | (1.03, 2.25) | |
| 40–49 | 13 | 67,476 | 19.27 | 0.687 | 1.12 | (0.58, 1.85) | |
| 50–59 | 21 | 118,604 | 17.71 | 0.943 | 0.98 | (0.62, 1.53) | |
| 60–69 | 52 | 149,110 | 34.87 | <0.001*** | 2.40 | (1.77, 3.1) | |
| 70–79 | 48 | 119,131 | 40.29 | <0.001*** | 2.64 | (1.97, 3.54) | |
| ≥80 | 29 | 53,272 | 54.44 | <0.001*** | 2.99 | (1.94, 4.17) | |
| Race | |||||||
| White | 185 | 632,876 | 29.23 | <0.001*** | 2.11 | (1.81, 2.43) | |
| Black | 2 | 45,831 | 4.36 | 0.999 | 0.80 | (0.11, 3.61) | |
| Other | 4 | 39,266 | 10.19 | 0.455 | 1.45 | (0.36, 3.41) | |
| Unknown | 0 | 5288 | 0.00 | — | — | — | |
| Race Latino | |||||||
| Latino | 13 | 42,402 | 30.66 | 0.001** | 2.57 | (1.38, 4.45) | |
| Non‐Latino | 178 | 680,859 | 26.14 | <0.001*** | 2.19 | (1.84, 2.48) | |
| Race Hispanic | |||||||
| Hispanic | 13 | 42,402 | 30.66 | <0.001*** | 2.57 | (1.38, 4.45) | |
| Non‐Hispanic white | 173 | 592,237 | 29.21 | <0.001*** | 2.45 | (2.06, 2.79) | |
| Non‐Hispanic Black | 2 | 45,158 | 4.43 | 0.099 | 0.37 | (0.04, 1.2) | |
| Non‐Hispanic Asian | 3 | 34,244 | 8.76 | 0.607 | 0.73 | (0.15, 2.19) | |
| Non‐Hispanic American Indian Native | 0 | 4350 | — | — | — | — | |
| Non‐Hispanic Unknown Race | 0 | 4871 | — | — | — | — | |
| Type of leukemia | |||||||
| Lymphoid leukemia | 111 | 529,480 | 20.96 | <0.001*** | 1.76 | (1.4, 2.06) | |
| Acute myeloid leukemia | 38 | 90,990 | 41.76 | <0.001*** | 3.50 | (2.44, 4.74) | |
| Chronic myeloproliferative diseases | 22 | 74,387 | 29.58 | <0.001*** | 2.48 | (1.53, 3.7) | |
| Myelodysplastic syndrome and other myeloproliferative | 3 | 7619 | 39.38 | 0.032* | 3.30 | (0.6, 8.77) | |
| Unspecified and other specified leukemia | 17 | 20,784 | 81.79 | <0.001*** | 6.86 | (3.3, 9.07) | |
| Surgery performed | |||||||
| Yes | 93 | 346,125 | 26.87 | <0.001*** | 2.25 | (1.79, 2.71) | |
| No | 98 | 377,136 | 25.99 | <0.001*** | 2.18 | (1.73, 2.6) | |
| Primary diseases | |||||||
| Yes | 147 | 549,586 | 26.75 | <0.001*** | 2.24 | (1.85, 2.58) | |
| No | 44 | 173,676 | 25.33 | <0.001*** | 2.12 | (1.52, 2.81) | |
| Chemotherapy | |||||||
| Yes | 91 | 362,790 | 25.08 | <0.001*** | 2.05 | (1.63, 2.48) | |
| No | 100 | 360,472 | 27.74 | <0.001*** | 2.27 | (1.85, 2.76) | |
| Household income | |||||||
| <$50,000 | 13 | 40,995 | 31.71 | <0.001*** | 2.59 | (1.38, 4.45) | |
| $55,000–$74,999 | 63 | 246,589 | 25.55 | <0.001*** | 2.09 | (1.61, 2.69) | |
| >$75,000 | 53 | 216,490 | 24.48 | <0.001*** | 2.00 | (1.52, 2.67) | |
| Unknown | 62 | 219,187 | 28.29 | <0.001*** | 2.31 | (1.43, 2.53) | |
| Living area a | |||||||
| Large city | 62 | 284,755 | 21.77 | <0.001*** | 1.83 | (1.36, 2.27) | |
| Medium city | 25 | 103,006 | 24.27 | <0.001*** | 2.03 | (1.24, 2.84) | |
| Small city | 17 | 37,331 | 45.54 | <0.001*** | 3.82 | (1.98, 5.44) | |
| Suburbs | 13 | 37,094 | 35.05 | 0.003** | 2.94 | (1.38, 4.45) | |
| Rural | 10 | 35,260 | 28.36 | 0.054 | 2.38 | (1.2, 4.6) | |
| Unknown | 64 | 225,816 | 28.34 | <0.001*** | 2.38 | (1.76, 2.92) | |
Large city, Counties in metropolitan areas of 1 million pop; Medium city, Counties in metropolitan areas of 250,000 to 1 million pop; Small city, Counties in metropolitan areas of lt 250 thousand pop; Suburbs, Nonmetropolitan counties adjacent to a metropolitan area; Rural, Nonmetropolitan counties not adjacent to a metropolitan area; Unknown, Unknown/missing/no match/Not 1990–2017.
SMR, standardized mortality ratio: Compared with the suicide rates of the general US population based on the Centers for Disease Control and Prevention's Web‐based Injury Statistics Query and Reporting System (1981–2017).
p < 0.05.
p < 0.01.
p < 0.001.
Since the CDC does not have data on the suicide mortality rate of the general population from 1975 to 1980, the population suicide benchmark from 1981 to 1983 was used in this study to adjust the suicide rate of leukemia patients from 1975 to 1980. 7 It was found that between 1975 and 2017, the SMR for suicide in leukemia patients in the United States fluctuated between 1.0 and 4.0. The changes in SMR of suicide in leukemia patients are shown in Figure 2.
FIGURE 2.
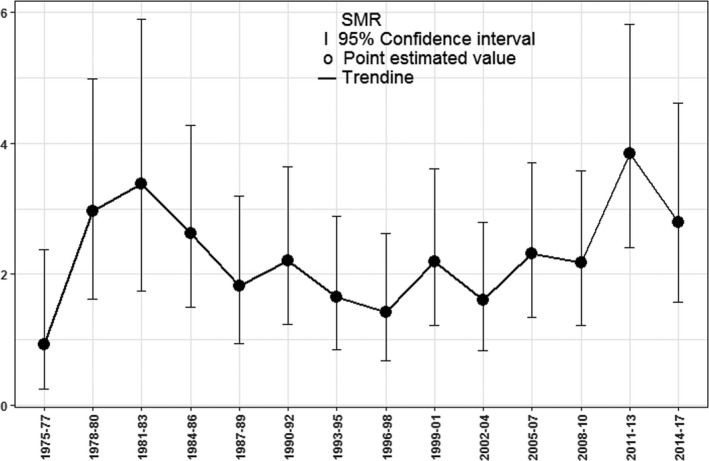
Standardized mortality ratio of suicide for leukemia patients (1975–2017)
3.3. Factors associated with suicide
The univariate analysis showed that the factors associated with a higher risk of suicide were male sex (vs. female: HR = 4.41, 95% CI = 2.93–6.63, p < 0.001), older age at diagnosis (60–69 years vs. ≤39 years: HR = 2.60, 95% CI = 1.60–4.23, p < 0.001; 70–79 years vs. ≤39 years: HR = 2.84, 95% CI = 1.72–4.68, p < 0.001; ≥80 years vs. ≤39 years: HR = 2.94, 95% CI = 1.65–5.21, p < 0.001), white race (vs. black: HR = 6.80, 95% CI = 1.69–27.40, p = 0.007), leukemia type (acute myeloid leukemia vs. lymphocytic leukemia: HR = 1.59, 95% CI = 1.09–2.33, p = 0.016; unspecified and other specified leukemia vs. lymphocytic leukemia: HR = 2.72, 95% CI = 1.55–4.75, p < 0.001), and living in a small city (vs. large city: HR = 2.10, 95% CI = 1.23–3.60, p = 0.007). Meanwhile, being a non‐Hispanic black (vs. Hispanic: HR = 0.15, 95% CI = 0.03–0.66, p = 0.013) was associated with a lower risk of suicide. The multivariate Cox regression analysis showed that the factors associated with a higher risk of suicide were male sex (vs. female: HR = 4.73, 95% CI = 3.13–7.11, p < 0.001), older age at diagnosis (60–69 year vs. ≤39 years: HR = 2.89, 95% CI = 1.73–4.81, p < 0.001; 70–79 years vs. ≤39 years: HR = 3.36, 95% CI = 1.98–5.69, p < 0.001; ≥80 years vs. ≤39 years: HR = 3.85, 95% CI = 2.10–7.04, p < 0.001), white race (vs. black: HR = 5.90, 95% CI = 1.46–23.84, p = 0.013), leukemia type (acute myeloid leukemia vs. lymphocytic leukemia: HR = 2.27, 95% CI = 1.53–3.37, p < 0.001; unspecified and other specified leukemia vs. lymphocytic leukemia: HR = 3.21, 95% CI = 1.82–5.66, p < 0.001), and living in a small city (vs. large city: HR = 2.16, 95% CI = 1.18–3.95, p = 0.012). Meanwhile, being non‐Hispanic (non‐Hispanic black vs. Hispanic: HR = 0.06, 95% CI = 0.01–0.62, p = 0.019; non‐Hispanic Asian vs. Hispanic: HR = 0.23, 95% CI = 0.13–0.85, p = 0.032) was associated with a lower risk of suicide. The risk factors related to suicide in leukemia patients are presented in Table 3. A subsequent Cox survival regression analysis revealed that the risk of suicide was higher in male leukemia patients than in female patients (Figure 3).
TABLE 3.
Univariable and multivariable analysis for suicide of leukemia patients
| Variables | Univariable analysis | Multivariable analysis | ||
|---|---|---|---|---|
| HR(95%CI) | p | HR(95%CI) | p | |
| Year of diagnosis | ||||
| 1975–1984 | Reference | Reference | ||
| 1985–1994 | 0.89 (0.57–1.40) | 0.616 | 0.87 (0.50–1.51) | 0.619 |
| 1995–2004 | 0.72 (0.46–1.14) | 0.165 | 0.53 (0.21–1.38) | 0.192 |
| 2005–2017 | 0.99 (0.64–1.53) | 0.977 | 0.70 (0.25–1.97) | 0.493 |
| Sex | ||||
| Female | Reference | Reference | ||
| Male | 4.41 (2.93–6.63) | <0.001*** | 4.73 (3.13–7.11) | <0.001*** |
| Age at diagnosis | ||||
| ≤39 | Reference | Reference | ||
| 40–49 | 1.41 (0.71–2.79) | 0.33 | 1.35 (0.68–2.70) | 0.391 |
| 50–59 | 1.32 (0.73–2.38) | 0.356 | 1.37 (0.75–2.50) | 0.303 |
| 60–69 | 2.60 (1.60–4.23) | <0.001*** | 2.89 (1.73–4.81) | <0.001*** |
| 70–79 | 2.84 (1.72–4.68) | <0.001*** | 3.36 (1.98–5.69) | <0.001*** |
| ≥80 | 2.94 (1.65–5.21) | <0.001*** | 3.85 (2.10–7.04) | <0.001*** |
| Race | ||||
| Black | Reference | Reference | ||
| White | 6.80 (1.69–27.40) | 0.007** | 5.90 (1.46–23.84) | 0.013* |
| Other | 2.43 (0.45–13.28) | 0.305 | 2.46 (0.45–13.48) | 0.298 |
| Unknown | — | — | — | — |
| Race Latino | ||||
| Latino | Reference | Reference | ||
| Non‐Latino | 1.12 (0.62–2.01) | 0.702 | 1.22 (0.65–2.28) | 0.530 |
| Race Hispanic | ||||
| Hispanic | Reference | Reference | ||
| Non‐Hispanic White | 1.00 (0.56–1.79) | 0.998 | 0.80 (0.43–1.48)) | 0.993 |
| Non‐Hispanic Black | 0.15 (0.03–0.66) | 0.013* | 0.06(0.01–0.62) | 0.019* |
| Non‐Hispanic Asian | 0.31 (0.09–1.08) | 0.067 | 0.23(0.13–0.85) | 0.032* |
| Non‐Hispanic American Indian Native | — | — | — | — |
| Non‐Hispanic Unknown Race | — | — | — | — |
| Type of leukemia | ||||
| Lymphoid leukemia | Reference | Reference | ||
| Acute myeloid leukemia | 1.59 (1.09–2.33) | 0.016* | 2.27 (1.53–3.37) | <0.001*** |
| Chronic myeloproliferative diseases | 1.24 (0.78–1.98) | 0.366 | 1.60 (0.99–2.56) | 0.052 |
| Myelodysplastic syndrome and other myeloproliferative | 1.32 (0.42–4.12) | 0.634 | 1.13 (0.35–3.59) | 0.838 |
| Unspecified and other specified leukemia | 2.72 (1.55–4.75) | <0.001*** | 3.21 (1.82–5.66) | <0.001*** |
| Surgery performed | ||||
| Yes | 1.05 (0.78–1.42) | 0.748 | 1.43 (0.68–3.02) | 0.339 |
| No | Reference | Reference | ||
| Primary diseases | ||||
| Yes | 1.03 (0.73–1.44) | 0.88 | 1.34 (0.95–1.90) | 0.098 |
| No | Reference | Reference | ||
| Chemotherapy | ||||
| Yes | 0.862 (0.65–1.15) | 0.312 | 0.88 (0.66–1.17) | 0.370 |
| No | Reference | Reference | ||
| Household income | ||||
| <$50,000 | Reference | Reference | ||
| $55,000–$74,999 | 1.00 (0.69–1.45) | 0.996 | 1.27 (0.83–1.95) | 0.279 |
| >$75,000 | 1.19 (0.66–2.17) | 0.564 | 1.04 (0.54–2.00) | 0.904 |
| Unknown | 1.12 (1.77–1.63) | 0.548 | 0.51 (0.11–2.46) | 0.402 |
| Living area a | ||||
| Large city | Reference | Reference | ||
| Medium city | 1.06 (0.66–1.69) | 0.821 | 1.03 (0.63–1.68) | 0.903 |
| Small city | 2.10 (1.23–3.60) | 0.007** | 2.16 (1.18–3.95) | 0.013* |
| Suburbs | 1.59 (0.88–2.90) | 0.127 | 1.48 (0.78–2.83) | 0.234 |
| Rural | 1.29 (0.66–2.52) | 0.455 | 1.23 (0.58–2.65) | 0.592 |
| Unknown | 1.29 (0.77–1.87) | 0.174 | 2.51 (0.57–10.96) | 0.223 |
Large city, Counties in metropolitan areas of 1 million pop; Medium city, Counties in metropolitan areas of 250,000 to 1 million pop; Small city, Counties in metropolitan areas of lt 250 thousand pop; Suburbs, Nonmetropolitan counties adjacent to a metropolitan area; Rural, Nonmetropolitan counties not adjacent to a metropolitan area; Unknown, Unknown/missing/no match/Not 1990–2017.
p < 0.05.
p < 0.01.
p < 0.001.
FIGURE 3.
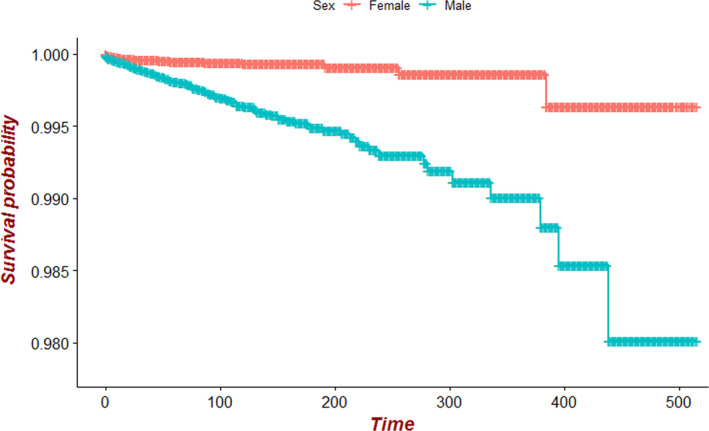
Comparison chart of survival curves of male and female leukemia patients
4. DISCUSSION
Multiple studies have confirmed that the suicide mortality rate is higher in cancer patients than in the general population. 3 , 4 , 17 Innos K reported that the suicide rate in Estonian cancer patients was higher than that in the general population, 29 while Crocetti E found the same result for Italian cancer patients. 16 The suicide rate is about twofold higher in cancer patients than the general population in the United States. 19 Using the SEER database, we found that the suicide rate of leukemia patients in the United States from 1975 to 2017 was approximately 26.41 per 100,000 person‐years, compared to 12.24 per 100,000 person‐years in the general population, giving an SMR of 2.16 (95% CI = 1.85–2.47), which is similar to the result that other cancer patients have a higher suicide rate than the general population. 19 The important risk factors for suicide in leukemia patients include male sex, older age at diagnosis, white race, and acute myeloid leukemia.
We found that the proportion of male leukemia patients in the United States is similar to that of females (Table 1), whereas most suicided leukemia patients are males (85.9%), with a suicide rate of 39.96 per 100,000 person‐years, compared to 8.63 per 100,000 person‐years in female leukemia patients (p < 0.001) (Table 2). In addition, male leukemia patients in the United States are more likely to commit suicide than are than female patients, with an HR of 4.41 (Table 3), which is similar to the suicide rates for male patients with other cancers. 19 , 30 Despite the similar prevalence rates of male and female leukemia patients, the much higher suicide rate in male leukemia patients may be related to the poor ability of males to withstand psychological pressures and their tendency for self‐directed violence. 31 , 32
We found that most of the leukemia patients were older than 60 years (65.1%), and the suicide rate was higher in this age group (60–69 years vs. ≤39 years: HR = 2.60, 95% CI = 1.60–4.23, p < 0.001; 70–79 years vs. ≤39 years: HR = 2.84, 95% CI = 1.72–4.68, p < 0.001; ≥80 years vs. ≤39 years: HR = 2.94, 95% CI = 1.65–5.21, p < 0.001) (Table 3). In general, the incidence rates of leukemia and suicide increased with the age of the patients, which is consistent with previous studies of elderly patients having other types of cancer. 22 , 33 , 34 The higher suicide rates of elderly leukemia patients might be related to their quality of life, outlook about life and death, and psychological condition such as the presence of depression. 11 , 35 , 36
Previous research has shown that the suicide rate among cancer patients in the United States is highest for whites and lowest for blacks. 37 , 38 Our results similarly found that among all racial groups in the United States, the risk of suicide was on average 6.80‐fold higher for whites than for blacks (95% CI = 1.69–27.40, p = 0.007) (Table 3). Compared with Hispanics, the suicide rates of non‐Hispanic blacks and non‐Hispanic Asians were 15% and 31% lower, respectively (Table 3). These results indicate that being white is a risk factor for suicide, while being black is a protective factor, which might be related to differences in the level of knowledge and culture among racial groups, religious beliefs, and economic conditions. 12 , 36 , 39 , 40
We also found that acute myeloid leukemia and unspecified and other specified leukemia were high‐risk factors for suicide in leukemia patients. In the SEER database, most of the leukemia patients in the United States have lymphocytic leukemia (50.7%) who also account for the majority of suicided patients (58.1%), and their SMR is also higher than in the general population (SMR = 1.76, 95% CI = 1.40–2.06) (Tables 1 and 2). However, compared with lymphoid leukemia, patients with acute myeloid leukemia had a 2.27‐fold higher risk of suicide (95% CI = 1.53–3.37, p < 0.001), while among those with unspecified and other specified leukemia it was 3.21‐fold higher (95% CI = 1.82–5.66, p < 0.001) (Table 3). The prognosis varies with the type of cancer, and this often causes changes in many characteristics of affected patients, such as physical status, psychological status, and quality of life, which in turn lead to an increased risk of suicide. 19 , 36 Acute myelogenous leukemia often occurs in young adults, and the disease progresses rapidly, 41 with some patients dying within a few months after the disease onset. 42 The unspecified and other specified leukemia have unclear disease types, poor treatment effects, and short survival times. 43 The low remission rate for these two types of leukemia patients exerts huge economic pressures and psychological burdens on them. Resulting factors such as discrimination, inferiority, and depression have led to their high suicide rate compared with other types of leukemia patients. 44
Finally, as shown in Figure 1, we found that the SMR for suicide among leukemia patients peaked in the 1980s and 2010s, and reached a nadir during 1975–1977 (SMR = 0.93, 95% CI = 0.25–2.37). Because the CDC lacks data on suicide mortality for the general population before 1980, the suicide rate of leukemia patients from 1975 to 1980 was adjusted to the population suicide benchmark from 1981 to 1983, 7 which may have reduced the adjusted SMRs. Although the SMR of leukemia patients generally fluctuated between 1.5 and 3.0 after the 1980s, it peaked in the 2010s at 3.84 (95% CI = 2.41–5.82). This may be related to factors such as financial crises, high medical costs, declining quality of life, and psychological burden. 45 , 46
Previous research has confirmed that some interventions can help to prevent suicide, 5 and that the suicide behavior of cancer patients is affected by various factors such as the psychological status, economic status, and religious beliefs. 34 , 45 Psychological factors such as depression are especially important risk factors for suicide. 12 Our research results indicated that the suicide rate of leukemia patients is higher than that of the general population. In order to reduce suicide in leukemia patients, psychiatric evaluations should be applied to this population. Some tools are available for identifying the risk of depression, including the Baker Depression Scale. 31 Providing psychological treatment to patients with leukemia at risk of depression can help to reduce the risk of suicide, as can the application of active treatment, improving their quality of life, and strengthening communication between family members. 47
Our research was subject to some limitations. We used SEER*Stat software (version 8.3.6) to collect patient information, but some information is currently missing from the system, such as the marital status, medication status, chemotherapy status, social factors, and psychological factors. These factors may impact suicide, and so the lacking data might have biased the risk assessments of suicide factors in leukemia patients. In this study, we collected leukemia patients from 1975 to 2017 who may have affected their health or even committed suicide due to the psychiatric illness. The SEER database is unable to obtain information on the diagnosis of leukemia patients with psychiatric, which affects the results of the study. Moreover, the SEER database only collects data from a proportion of cancer patients in the United States. Therefore, the suicide risk of leukemia patients should also be assessed in other countries.
5. CONCLUSIONS
We have investigated the risk of suicide in leukemia patients and the underlying independent risk factors. Male sex, older age at diagnosis, white race, and acute myeloid leukemia were found to be significant risk factors for suicide in leukemia patients, while being a non‐Hispanic black was a protective factor. Medical workers can use our research results to screen leukemia patients with a higher risk of suicide and apply targeted preventive measures to them.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Haohui Yu and Yulin Huang performed statistical analysis and data interpretation. Haohui Yu, Ke Cai, and Jun Lyu contributed to the study concept and study design. Haohui Yu and Yulin Huang performed literature research and data extraction. Ke Cai and Jun Lyu were responsible for the quality control of data and algorithms. All authors contributed to writing of the manuscript and approved the final version.
Yu H, Cai K, Huang Y, Lyu J. Risk factors associated with suicide among leukemia patients: A Surveillance, Epidemiology, and End Results analysis. Cancer Med. 2020;9:9006–9017. 10.1002/cam4.3502
Haohui Yu and Ke Cai contributed equally to the work.
DATA AVAILABILITY STATEMENT
We obtained permission to access the database after signing and submitting the SEER Research Data Agreement form via email. We used SEER*Stat software (version 8.3.6) to identify US leukemia patients who were added to the SEER database (http://seer.cancer.gov). All statistical analyses were performed using R software (version 3.6.3, http://www.r‐project.org/).
REFERENCES
- 1. Louhivuori KA, Hakama M. Risk of suicide among cancer patients. Am J Epidemiol. 1979;109:59–65. [DOI] [PubMed] [Google Scholar]
- 2. Allebeck P, Bolund C, Ringback G. Increased suicide rate in cancer patients. A cohort study based on the Swedish Cancer‐Environment Register. J Clin Epidemiol. 1989;42:611–616. [DOI] [PubMed] [Google Scholar]
- 3. Misono S, Weiss NS, Fann JR, et al. Incidence of suicide in persons with cancer. J Clin Oncol. 2008;26:4731–4738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Allebeck P, Bolund C. Suicides and suicide attempts in cancer patients. Psychol Med. 1991;21:979–984. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization . Preventing suicide: a global imperative. 2014.
- 6. Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019;364:l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention . Injury statistics query and reporting system. https://www.cdc.gov/injury/wisqars/fatal.html
- 8. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30. [DOI] [PubMed] [Google Scholar]
- 9. Bray F, Ferlay J, Soerjomataram I, et al. Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 10. Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health. 2000;90:1885–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zaorsky NG, Churilla TM, Egleston BL, et al. Causes of death among cancer patients. Ann Oncol. 2017;28:400–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Anguiano L, Mayer DK, Piven ML, et al. A literature review of suicide in cancer patients. Cancer Nurs. 2012;35:E14–E26. [DOI] [PubMed] [Google Scholar]
- 13. Osazuwa‐Peters N, Simpson MC, Zhao L, et al. Suicide risk among cancer survivors: head and neck versus other cancers. Cancer. 2018;124(20):4072–4079. [DOI] [PubMed] [Google Scholar]
- 14. Fox BH, Stanek EJ 3rd, Boyd SC, et al. Suicide rates among cancer patients in Connecticut. J Chronic Dis. 1982;35(2):89–100. [DOI] [PubMed] [Google Scholar]
- 15. Storm HH, Christensen N, Jensen OM. Suicides among Danish patients with cancer: 1971 to 1986. Cancer. 1992;69(6):1507–1512. [DOI] [PubMed] [Google Scholar]
- 16. Crocetti E, Arniani S, Acciai S, et al. High suicide mortality soon after diagnosis among cancer patients in central Italy. Br J Cancer. 1998;77(7):1194–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bjorkenstam C, Edberg A, Ayoubi S, et al. Are cancer patients at higher suicide risk than the general population? Scand J Public Health. 2005;33(3):208–214. [DOI] [PubMed] [Google Scholar]
- 18. Robson A, Scrutton F, Wilkinson L, et al. The risk of suicide in cancer patients: a review of the literature. Psychooncology. 2010;19(12):1250–1258. [DOI] [PubMed] [Google Scholar]
- 19. Zaorsky NG, Zhang Y, Tuanquin L, et al. Suicide among cancer patients. Nat Commun. 2019;10(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Guo C, Zheng W, Zhu W, et al. Risk factors associated with suicide among kidney cancer patients: a Surveillance, Epidemiology, and End Results analysis. Cancer Med. 2019;8(11):5386–5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gaitanidis A, Alevizakos M, Pitiakoudis M, et al. Trends in incidence and associated risk factors of suicide mortality among breast cancer patients. Psychooncology. 2018;27(5):1450–1456. [DOI] [PubMed] [Google Scholar]
- 22. Rahouma M, Kamel M, Abouarab A, et al. Lung cancer patients have the highest malignancy‐associated suicide rate in USA: a population‐based analysis. ecancer 2018;12:859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jeha GM, Wesley T, Cataldo VD. Novel translocation in acute myeloid leukemia: case report and review of risk‐stratification and induction chemotherapy in patients with acute myeloid leukemia. J Hematol. 2020;9(1–2):13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sung H, Siegel RL, Rosenberg PS, et al. Emerging cancer trends among young adults in the USA: analysis of a population‐based cancer registry. Lancet Public Health. 2019;4(3):e137–e147. [DOI] [PubMed] [Google Scholar]
- 25. Saad AM, Gad MM, Al‐Husseini MJ, et al. Suicidal death within a year of a cancer diagnosis: a population‐based study. Cancer. 2019;125(6):972–979. [DOI] [PubMed] [Google Scholar]
- 26. Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarkers Prev. 1999;8(12):1117–1121. [PubMed] [Google Scholar]
- 27. Yang J, Li YJ, Liu QQ, et al. Brief introduction of medical database and data mining technology in big data era. J Evid‐Based Med. 2020;13(1):57–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Breslow NE, Day NE. Statistical methods in cancer research. Volume II–The design and analysis of cohort studies. IARC Sci Publ. 1987;(82):1–406. [PubMed] [Google Scholar]
- 29. Innos K, Rahu K, Rahu M, et al. Suicides among cancer patients in Estonia: a population based study. Eur J Cancer. 2003;39(15):2223–2228. [DOI] [PubMed] [Google Scholar]
- 30. Shen J, Zhu M, Li S, et al. Incidence and risk factors for suicide death among kaposi's sarcoma patients: a surveillance, epidemiology, and end results analysis. Med Sci Monit. 2020;26:e920711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Klaassen Z, Goldberg H, Chandrasekar T, et al. Changing trends for suicidal death in patients with bladder cancer: a 40+ year population‐level analysis. Clin Genitourin Cancer. 2018;16(3):206–212. [DOI] [PubMed] [Google Scholar]
- 32. Kendal WS. Suicide and cancer: a gender‐comparative study. Ann Oncol. 2007;18(2):381–387. [DOI] [PubMed] [Google Scholar]
- 33. Turaga KK, Malafa MP, Jacobsen PB, et al. Suicide in patients with pancreatic cancer. Cancer. 2011;117(3):642–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Henson KE, Brock R, Charnock J, et al. Risk of suicide after cancer diagnosis in England. JAMA Psychiatry. 2019;76(1):51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yaskin J. Nervous symptoms at earliest manifestations of cancer of the pancreas. JAMA. 1931;96:1664–1668. [Google Scholar]
- 36. Jayakrishnan TT, Sekigami Y, Rajeev R, et al. Morbidity of curative cancer surgery and suicide risk. Psychooncology. 2017;26(11):1792–1798. [DOI] [PubMed] [Google Scholar]
- 37. Curtin SC, Warner M, Hedegaard H. Suicide Rates for Females and Males by Race and Ethnicity: United States, 1999 and 2014. NCHS Health E‐Stat. Hyattsville, MD: National Center for Health Statistics; 2016. [Google Scholar]
- 38. Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322(20):1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ahn MH, Park S, Lee HB, et al. Suicide in cancer patients within the first year of diagnosis. Oncology. 2015;24(5):601–607. [DOI] [PubMed] [Google Scholar]
- 40. Akizuki N, Shimizu K, Asai M, et al. Prevalence and predictive factors of depression and anxiety in patients with pancreatic cancer: a longitudinal study. Jpn J Clin Oncol. 2016;46(1):71–77. [DOI] [PubMed] [Google Scholar]
- 41. Rose‐Inman H, Kuehl D. Acute leukemia. Emerg Med Clin North Am. 2014;32(3):579–596. [DOI] [PubMed] [Google Scholar]
- 42. Alfayez M, Borthakur G. Checkpoint inhibitors and acute myelogenous leukemia: promises and challenges. Expert Rev Hematol. 2018;11(5):373–389. [DOI] [PubMed] [Google Scholar]
- 43. Savage SA, Dufour C. Classical inherited bone marrow failure syndromes with high risk for myelodysplastic syndrome and acute myelogenous leukemia. Semin Hematol. 2017;54(2):105–114. [DOI] [PubMed] [Google Scholar]
- 44. Solh M, Solomon S, Morris L, et al. Extramedullary acute myelogenous leukemia. Blood Rev. 2016;30(5):333–339. [DOI] [PubMed] [Google Scholar]
- 45. John Mann J, Metts AV. The economy and suicide. Crisis. 2017;38(3):141–146. [DOI] [PubMed] [Google Scholar]
- 46. Rizzo RF. Physician‐assisted suicide in the United States: the underlying factors in technology, health care and palliative medicine–part one. Theor Med Bioeth. 2000;21(3):277–289. [DOI] [PubMed] [Google Scholar]
- 47. Banyasz A, Wells‐Di Gregorio SM. Cancer‐related suicide: a biopsychosocial existential approach to risk management. Psychooncology. 2018;27(11):2661–2664. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We obtained permission to access the database after signing and submitting the SEER Research Data Agreement form via email. We used SEER*Stat software (version 8.3.6) to identify US leukemia patients who were added to the SEER database (http://seer.cancer.gov). All statistical analyses were performed using R software (version 3.6.3, http://www.r‐project.org/).


