Key Points
The preferred therapy for UCD is complete surgical resection.
Unresectable asymptomatic UCD may be observed; symptomatic UCD requires rituximab ± steroids or anti–interleukin-6 antibody.
Abstract
Castleman disease (CD) includes a group of rare and heterogeneous disorders with characteristic lymph node histopathological abnormalities. CD can occur in a single lymph node station, which is referred to as unicentric CD (UCD). CD can also involve multicentric lymphadenopathy and inflammatory symptoms (multicentric CD [MCD]). MCD includes human herpesvirus-8 (HHV-8)–associated MCD, POEMS-associated MCD, and HHV-8−/idiopathic MCD (iMCD). The first-ever diagnostic and treatment guidelines were recently developed for iMCD by an international expert consortium convened by the Castleman Disease Collaborative Network (CDCN). The focus of this report is to establish similar guidelines for the management of UCD. To this purpose, an international working group of 42 experts from 10 countries was convened to establish consensus recommendations based on review of treatment in published cases of UCD, the CDCN ACCELERATE registry, and expert opinion. Complete surgical resection is often curative and is therefore the preferred first-line therapy, if possible. The management of unresectable UCD is more challenging. Existing evidence supports that asymptomatic unresectable UCD may be observed. The anti–interleukin-6 monoclonal antibody siltuximab should be considered for unresectable UCD patients with an inflammatory syndrome. Unresectable UCD that is symptomatic as a result of compression of vital neighboring structures may be rendered amenable to resection by medical therapy (eg, rituximab, steroids), radiotherapy, or embolization. Further research is needed in UCD patients with persisting constitutional symptoms despite complete excision and normal laboratory markers. We hope that these guidelines will improve outcomes in UCD and help treating physicians decide the best therapeutic approach for their patients.
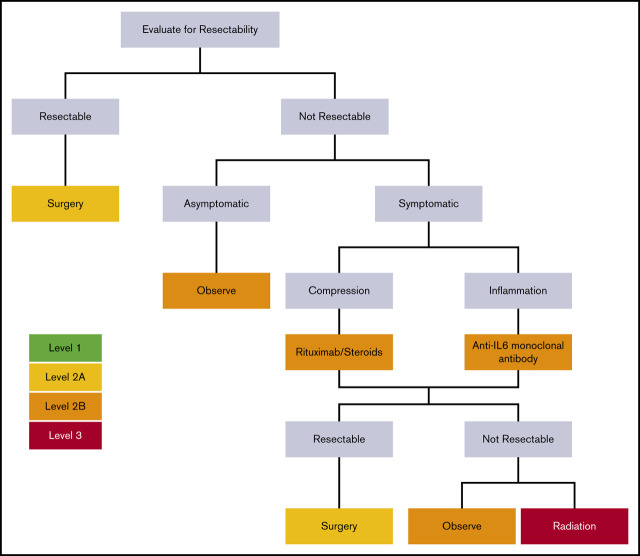
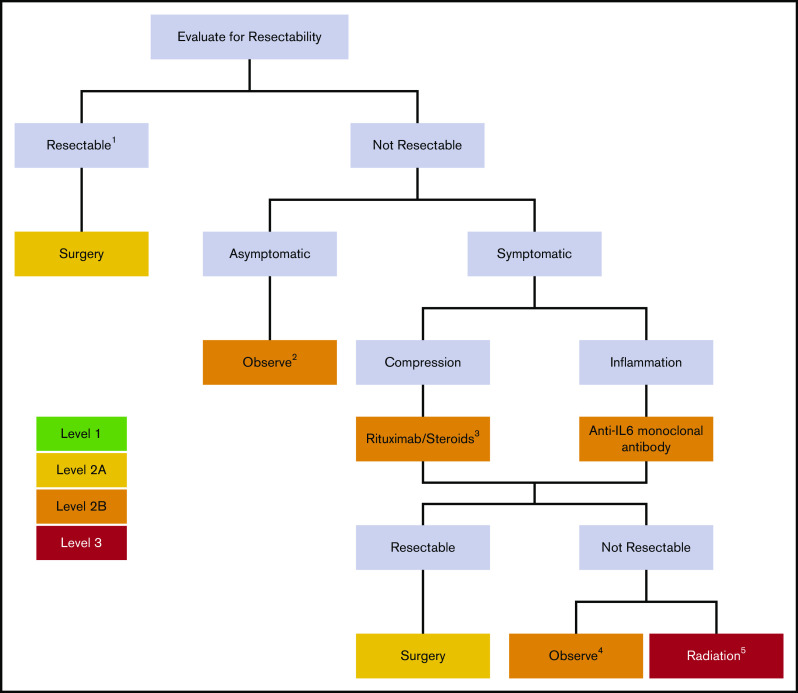
Visual Abstract
Introduction
Castleman disease (CD) comprises a heterogeneous group of disorders involving a broad lymph node histopathological spectrum and is classified as unicentric (UCD) or multicentric CD (MCD). Classically, MCD presents with lymphadenopathy affecting multiple lymph node stations and is associated with systemic symptoms, such as fever, weight loss, and fatigue, driven by interleukin-6 (IL-6) and other cytokines. MCD has been subclassified into human herpesvirus-8 (HHV-8)–associated MCD, POEMS-associated MCD, and HHV-8−/idiopathic MCD (iMCD).
UCD, which involves a single enlarged lymph node or multiple enlarged lymph nodes within a single lymph node station, was first described by Castleman and Towne1 in a patient with a mediastinal mass in 1954 and soon thereafter by Castleman et al2 in a series of 12 cases in 1956. The disease typically behaves in an indolent fashion, and enlargement of lymph nodes is gradual. Patients can be diagnosed at any age (range, 2-84 years), with a median age of diagnosis of 34 years and possibly a mild preponderance of female patients.3 There are no known epidemiological factors that predispose to the development of UCD. The incidence of UCD has been estimated at 16 to 19 per million in the US population, which translates to 5000 to 6000 patients per year.4 UCD is virtually always HHV-8−, but rare positive cases have been reported, and these should be categorized and managed as localized HHV-8–associated CD.5-8 Frequently, the diagnosis of UCD is incidental, and the lymphadenopathy is often asymptomatic. However, some patients present with symptoms resulting from compression of vital structures (eg, airways, neurovascular bundles, or ureters), whereas others will experience iMCD-like inflammatory syndromes. In a large series of UCD cases, the most common sites of involvement were the mediastinum (29%), neck (23%), abdomen (21%), and retroperitoneum (17%).5 UCD can also occur in the axilla and inguinal regions as well as orbits, nasopharynx, and small bowel.9-12
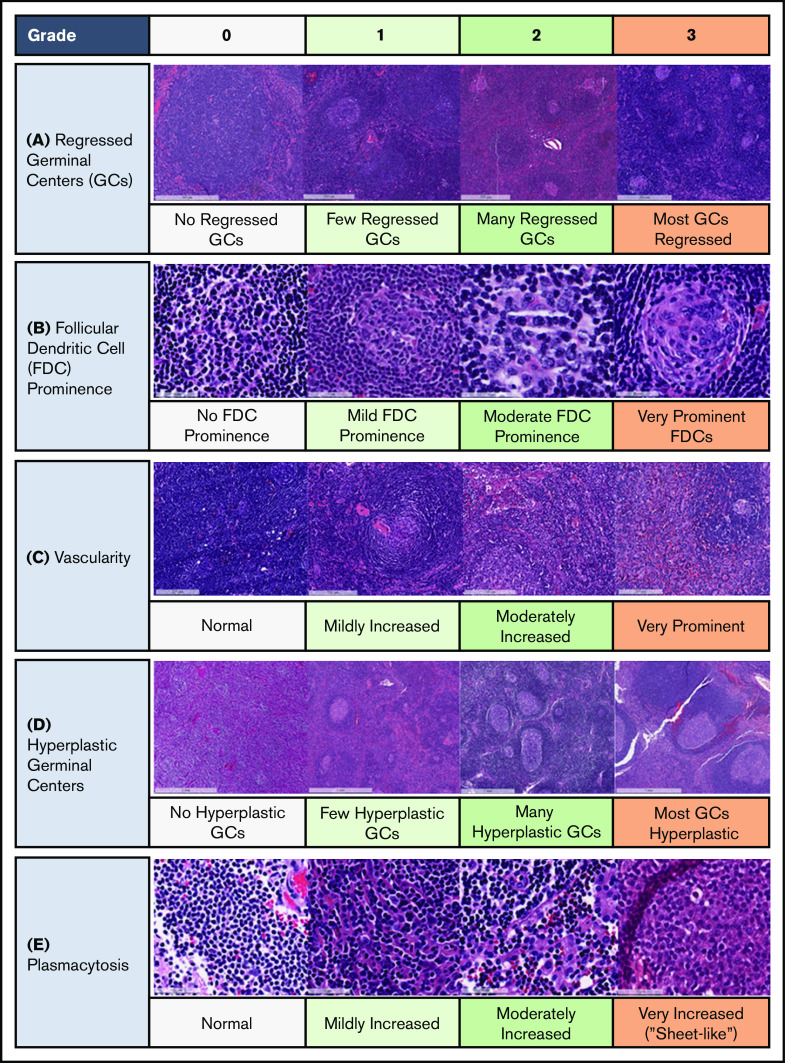
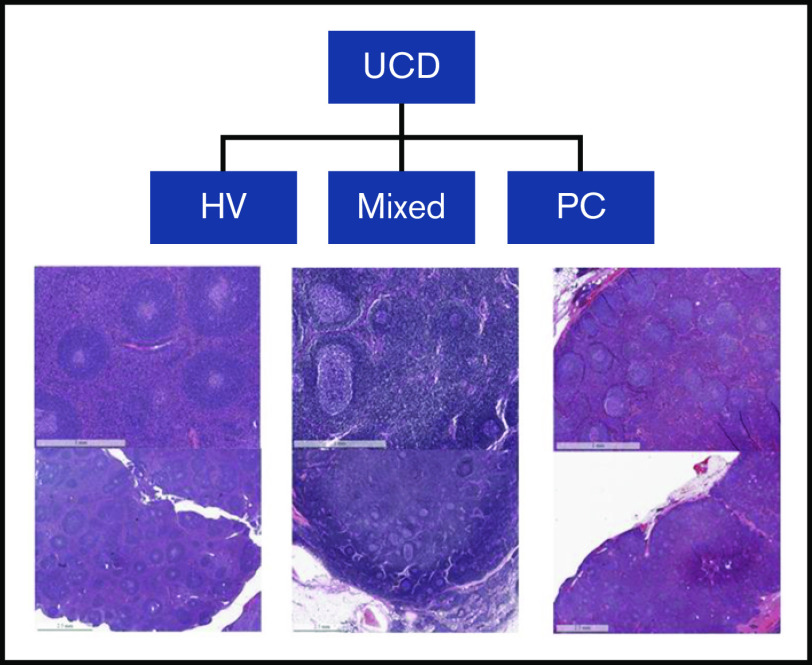
Histopathological features of lymph nodes in UCD range from what is considered to be hyaline vascular (HV) histopathology to plasmacytic (PC) histopathology, with a mixed subgroup in between that exhibits both features. HV histopathological features are most often described in UCD, and these patients do not typically have constitutional symptomatology or excess cytokine secretion.13-16 The lymph nodes show follicular hyperplasia with abnormal atretic germinal centers, increased vascularity with hyalinization, prominent and/or dysplastic follicular dendritic cells (FDCs), and expanded mantle zones in an onion-skin appearance. Often there are radially penetrating blood vessels causing a lollipop appearance, multiple germinal centers within the same mantle zone referred to as twinning or budding, tight aggregates of plasmacytoid dendritic cells, and architectural disruption with obliterated sinuses. No interfollicular plasmacytosis is present in HV UCD. An estimated 10% to 20% of UCD cases are considered to have PC histopathology, involving variably sized germinal centers, interfollicular plasmacytosis, and occasionally systemic inflammatory symptoms. Patients with PC UCD or mixed UCD often demonstrate iMCD-like symptoms, such as night sweats, fever, anorexia, or weight loss, as well as abnormal laboratory markers, such as anemia, elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), hypoalbuminemia, or hypergammaglobulinemia.13,15-19 Occasionally, AA amyloidosis as well as non–amyloidosis-related renal disease can occur with UCD, mainly in the PC subtype.20-23 Life expectancy is usually not changed after the diagnosis of UCD. However, patients with UCD are at increased risk of developing paraneoplastic pemphigus (PNP), bronchiolitis obliterans (BO), AA amyloidosis, vascular neoplasms (eg, FDC sarcoma [FDCS]), and possibly lymphomas.23-26
The pathogenesis of UCD is not well understood, but recent evidence suggests that it may be caused in some patients by a clonal expansion of lymph node stromal cells, including FDCs.27 FDCs are located in the germinal center of secondary follicles and interact with B cells during germinal center reaction through antigen presentation as well as chemokine and cytokine secretion. The atrophic B cell–depleted germinal centers in UCD may reflect FDC dysfunction.27-29 Recently, whole-exome sequencing revealed gain-of-function somatic mutations in the kinase domain of the PDGFRB gene in 7 of 41 UCD patients with HV histopathology; the mutations were localized to CD45− cells, likely representing stromal cells.30 No clear associations have been made between UCD and active viral infections, such as HIV or HHV-8.31 Further research is under way to investigate the etiology and pathogenesis of UCD.
The Castleman Disease Collaborative Network (CDCN) has established international consensus treatment guidelines for the treatment of iMCD. Herein, we report our recommendations for the management of UCD.
Methods
In 2016, the CDCN embarked on the establishment of treatment guidelines for UCD and iMCD based on expert opinion and review of the available literature by the Patient Care and Therapy subcommittee of its scientific advisory board. This international group of 42 participants from the United States, Japan, Hong Kong, France, the United Kingdom, Germany, Italy, Norway, and New Zealand comprises experts in hematology/oncology, hematology, hematopathology, infectious diseases, immunology, and surgery, as well as an iMCD patient. The working group first met in December 2016 in San Diego, California, with a follow-up meeting in December 2017 in Atlanta, Georgia, both during America Society of Hematology annual conferences. Three additional Web-based teleconferences were held in August 2017, November 2017, and March 2018. The iMCD guidelines were first published in 2018. Further discussion and refinement of the UCD guidelines occurred from 2018 to 2020.
All relevant English-language literature was identified through PubMed using the search term unicentric Castleman disease. Included were case series and retrospective cohort studies involving ≥5 patients in which treatments and responses were reported and a clear distinction between UCD and MCD was apparent. Literature from before 2012 was captured in the large review by Talat et al.5 Systematic literature reviews after 2012 were excluded out of concern of possible overreporting on the same patients. Articles primarily focusing on treatment of UCD complications, such as PNP or BO, were also excluded. Table 1 summarizes published data and data from the ongoing ACCELERATE natural history registry32 from the CDCN and University of Pennsylvania.12,19,33-45 The consensus focused on 2 main topics: treatment of resectable UCD and treatment of unresectable UCD. Levels of evidence were modeled after National Comprehensive Cancer Network guidelines.46
Table 1.
Data from treatment of UCD cases in published literature and ACCELERATE registry
| Therapy | Published literature, n (%)* | Ongoing CD natural history study, n (%)† |
|---|---|---|
| Surgical resection‡ | 457 | 39 |
| Evaluable | 237 | 37 |
| Response§ | 228 (96.2) | 31 (83.8) |
| Nonresponse‖ | 9 (3.8) | 6 (16.2) |
| Nonevaluable | 220 | 2 |
| Embolization | 2 | 0 |
| Evaluable | 1 | 0 |
| Response§ | 1 (100) | 0 |
| Nonresponse‖ | 0 | 0 |
| Nonevaluable | 1 | 0 |
| Rituximab ± steroids | 5 | 9 |
| Evaluable | 4 | 8 |
| Response§ | 2 (50.0) | 6 (75.0) |
| Nonresponse‖ | 2 (50.0) | 2 (25.0) |
| Nonevaluable | 1 | 1 |
| Radiotherapy | 15 | 1 |
| Evaluable | 8 | 1 |
| Response§ | 8 (100) | 1 (100) |
| Nonresponse‖ | 0 | 0 |
| Nonevaluable | 7 | 0 |
See supplemental Table 1.
Includes patients enrolled by CD-treating physicians at experienced centers in Europe or patients who self-enrolled and whose cases were reviewed by a panel of CD-treating clinicians and pathologists.
Includes complete or partial resection of lymph node.
Achieving at least 50% improvement of associated symptoms and at least 50% reduction of mass.
Achieving <50% improvement of associated symptoms or <50% reduction of mass.
Results
Diagnosis and evaluation of UCD
UCD is diagnosed after a lymph node biopsy to investigate solitary lymphadenopathy, usually on clinical suspicion of lymphoma. Figure 1 displays the spectrum of changes seen in UCD, and Figure 2 provides representative images.
Figure 1.
Spectrum of histopathological changes seen in UCD. HV histopathological subtype is characterized by the presence of regressed germinal centers (GCs) and FDC prominence, whereas the plasmacytic subtype exhibits hyperplastic GCs and profuse plasmacytosis. Mixed subtype exhibits a combination of HV and plasmacytic features. Lymph node slides were obtained prestained with hematoxylin and eosin from clinical specimens for the ACCELERATE natural history registry, scanned, and captured using Aperio Imagescope. Bars represent 60 (A,E) and 200 mm (B-D). (A) Regressed GC. (B) FDC prominence in GC. (C) Blood vessels penetrating GC demonstrate prominent vascularity. (D) Hyperplastic GC. (E) Sheet-like plasmacytosis.
Figure 2.
Representative examples of UCD. HV subtype is characterized by the presence of regressed atretic germinal centers. There is increased vascularity with hyalinization, prominence of often dysplastic FDCs, and expanded mantle zones in an onion-skin appearance. There are radially penetrating blood vessels causing a lollipop appearance, multiple germinal centers within the same mantle zone referred to as twinning or budding, tight aggregates of plasmacytoid dendritic cells, and architectural disruption with obliterated sinuses. PC subtype exhibits hyperplastic germinal centers and profuse plasmacytosis. Mixed subtype exhibits a combination of HV and PC features.
In addition to identifying histopathological features consistent with UCD, a thorough workup for conditions with overlapping histopathology is required (Table 2). It is important that a complete excisional lymph node biopsy be performed rather than a fine-needle aspirate or core biopsy. Unlike MCD with its many overlapping conditions, few diseases other than UCD and lymphomas present with a solitary enlarged lymph node with CD-like histopathology. Thymomas, progressive transformation of germinal centers, unusual morphological variants of follicular lymphoma (FL), and lymphoproliferations with regressive germinal centers, such as angioimmunoblastic T-cell lymphoma, can sometimes show histopathological features reminiscent of HV UCD. PC UCD–like histopathological features may be seen in many other conditions, such as infections, autoimmune diseases, primary or acquired immunodeficiencies, such as advanced phases of HIV-related lymphadenopathy, and malignancies, including Hodgkin lymphoma, but the lymphadenopathy is usually not unicentric.2,47-49
Table 2.
Conditions that can overlap with UCD
| Condition |
|---|
| Infectious diseases |
| HIV-related adenopathy |
| Syphilis |
| EBV infection |
| Inflammatory pseudotumor |
| Neoplasia |
| Hodgkin lymphoma |
| NHL (follicular, marginal zone, mantle cell, lymphoplasmacytic) |
| FDCS |
| Plasmacytoma |
| Autoimmunity/other |
| Systemic lupus erythematosus, rheumatoid arthritis, Felty’s syndrome |
| Follicular hyperplasia |
| Autoimmune lymphoproliferative syndrome |
| HHV-8–associated MCD or iMCD |
EBV, Epstein-Barr virus; NHL, non-Hodgkin lymphoma.
A series of laboratory and radiological investigations should be performed (Table 3). First, computed tomography (CT) of the neck, chest, abdomen, and pelvis is recommended to establish the number of lymph node stations involved and differentiate UCD from MCD. UCD should be suspected in the setting of a single persistently enlarged lymph node or multiple enlarged lymph nodes within a single lymph node station associated with moderate to intense postcontrast enhancement on CT. UCD can present in any lymph node in the body, and the size of the enlarged lymph is often more bulky than the enlarged lymph nodes seen in MCD. If >1 lymph node is enlarged, those lymph nodes, by definition, must be confined to a single lymph node region to be considered to represent UCD.
Table 3.
Recommended workup of UCD
| Assessment category | Tests |
|---|---|
| Imaging | CT-PET or CT of neck, chest, abdomen, pelvis |
| Histopathology | HV/mixed/PC |
| Immunostaining | Staining for EBER, LANA-1, and lymphoma or plasmacytoma markers if suspected |
| Clonality | IgH gene rearrangement, TCR clonality |
| Virological status | HIV serology, HHV-8 qPCR (peripheral blood) |
| Inflammatory response | CBC, renal function, liver function, CRP, ESR, fibrinogen, immunoglobulins and free light chains, albumin |
| Autoimmunity (if suspected) | ANA, rheumatoid factor |
| Monoclonal gammopathy (if suspected) | Serum protein electrophoresis with immunofixation, quantitative immunoglobulins, and bone marrow if indicated |
| Organ function (depending on location relative to neighboring vital structures) | ECHO, pulmonary function |
Workup should include excisional lymph node biopsy for histopathological examination to confirm features consistent with UCD, establish histopathological subtype, and rule out Epstein-Barr virus and HHV-8 infection by Epstein-Barr virus–encoded small RNAs (EBER) and latency-associated nuclear antigen-1 (LANA-1) staining. Blood work is helpful to exclude HIV infection, autoimmune disorders, and monoclonal gammopathy of undetermined significance/myeloma as well as measure inflammatory markers and determine organ function. CT and CT–positron emission tomography (PET) scanning help to visualize the extent of the disease. Bone marrow examination can exclude a concomitant plasma cell dyscrasia.
ANA, antinuclear antibody; CBC, complete blood count; ECHO, echocardiogram; IgH, immunoglobulin H; qPCR, quantitative polymerase chain reaction; TCR, T-cell receptor.
CT–positron emission tomography scanning may provide additional information regarding the metabolic activity of the affected lymph nodes.50 High specific uptake values should raise the suspicion of lymphoma, which is an important differential diagnosis. If suspected, immunostaining for markers of lymphoma and clonality testing should also be performed. Immunostaining for HHV-8 should also be performed to identify rare cases of HHV-8+ UCD. Clinical evaluation includes assessment for constitutional symptoms (night sweats, fever >38°C, weight loss, fatigue) and features such as fluid accumulation (peripheral edema, pleural effusion, ascites). Recommended laboratory testing comprises screening for anemia, elevated CRP and/or ESR, hypoalbuminemia, hypergammaglobulinemia, and other markers of a cytokine-induced inflammatory response. It should be noted that most cases of UCD are asymptomatic, and often no laboratory abnormalities are present. HIV serology is typically negative. As clinically indicated, further workup may require assessment for PNP, BO, and POEMS syndrome. Rare cases of UCD have light chain restriction of plasma cells, which should prompt a workup for a clonal plasma cell dyscrasia with associated POEMS syndrome.
Management of UCD
Important considerations in the management of UCD are: the location of the enlarged lymph node, the resectability of the enlarged lymph node, and the degree to which the enlarged lymph node causes symptoms by compressing neighboring anatomy or inducing a systemic inflammatory syndrome. Further consideration should also be given to cases that are currently asymptomatic but likely to become symptomatic through compression of neighboring structures if the mass continues to grow. Resectability is a subjective decision that should weigh the risks and benefits of surgery and be made in consultation between the surgeon, clinician, and patient. Multidisciplinary review is encouraged and should include surgical specialists, radiologists, pathologists, and oncologists to discuss treatment options to optimize patient outcomes.
Resectable UCD.
We recommend that all patients first be evaluated to determine whether the mass is amenable to complete surgical extirpation (Figure 3). Complete surgical excision will usually eliminate any systemic symptomatology and laboratory abnormalities, if present. A review of the literature and real-world data from the ACCELERATE study found a high response rate to surgical excision (Table 1). In their first descriptions, Castleman et al1,2 reported that surgery was an effective treatment modality, and several early series confirmed that resection is the preferred method of first-line treatment.15,16,48,51-53 Dispenzieri et al34 reported a 5-year overall survival (OS) of 91% in a series of 53 patients surgically treated at the Mayo Clinic and University of Nebraska. Talat et al5 reported a similar OS of >90% in a retrospective literature study comprising 278 UCD patients treated with surgery, with a follow-up of up to 10 years. In the Talat et al series, outcome was better when surgery was performed for peripheral lymphadenopathy rather than central lymphadenopathy located in the chest, abdomen, or pelvis. Death resulting from disease occurred in only 1 (1.5%) of 68 patients with peripheral lymphadenopathy vs 9 (6.1%) of 148 patients with central lymphadenopathy (P < .05), presumably because resection was virtually always feasible in those with peripheral lymphadenopathy. Inability to resect the involved lymph node proved the only factor predictive of a fatal outcome. In the absence of persistent systemic symptoms or concern for neighboring anatomic structures, residual small satellite lymph nodes after resection can be observed, with spontaneous involution often seen, after resection of the principal enlarged lymph node.54 Symptoms resulting from AA amyloidosis as well as non–amyloidosis-related renal disease typically improve over the ensuing years after removal of unicentric disease.20-22
Figure 3.
UCD treatment algorithm. UCD patients should be evaluated for lymph node resectability, with surgery being the preferred method of treatment. 1Consider presurgical embolization in large vascular UCD lymph nodes to render surgery safer. Follow-up CT scans, physical examination, and laboratory testing can be done at 12-month intervals. In rare patients who continue to have symptoms after complete lymph node excision, other diagnoses and/or treatments should be considered. 2Watchful observation is an option in patients with unresectable asymptomatic disease or those with nonsevere compressive symptoms. UCD patients with compression-related symptoms may benefit from medical treatment (eg, rituximab ± steroids or anti–IL-6 monoclonal antibody therapy) if inflammatory symptoms (night sweats, fevers, anorexia, weight loss) and/or laboratory abnormalities (elevated ESR, elevated CRP, or anemia) are present. 3In selected cases, embolization as alternative or adjunctive therapy should be considered. 4Observation is an option in patients who have been rendered asymptomatic by medical therapy with rituximab/steroids or anti–IL-6 monoclonal antibody therapy. 5Patients who continue to be symptomatic are candidates for radiotherapy. Alternative options include treatment with immunomodulators/immunosuppressants, such as corticosteroids, cyclosporine A, and sirolimus.
UCD should be managed in the first-line setting with surgery in both children and adults. Parez et al55 reported 72 pediatric cases who fared well with surgery (n = 70) or radiotherapy (n = 2). Taken together, these and other reports provide level 2A evidence establishing surgical resection as the treatment of choice for UCD.19,37,45,56-59 Surgical resection is the most appropriate first-line intervention, according to uniform panel consensus. No high-quality randomized controlled trials exist to substantiate a level 1 grade recommendation. Recurrences after complete resection are uncommon, although they have occasionally been described.12,13,45,53,60,61 Recurrent UCD should be managed according to the algorithm described in Figure 3 and surgically excised, if feasible. Follow-up with yearly CT scan imaging studies for 5 years is therefore recommended. Thereafter, imaging should be clinically driven based upon suspicion of disease recurrence.50,62
The average size of the lymphadenopathy in UCD is larger than that in MCD (5.5 vs 3.8 cm).5 These larger lymph nodes can be more challenging to remove, not only because of their size but also because of the increased vascularity of UCD, which can cause severe perioperative bleeding.63-65 Typically, dominant feeding vessels are present, and several investigators have used preoperative embolization to render surgery safer.66-76 We recommend, based on level 2B evidence, that consideration be given to presurgical embolic devascularization of large UCD lymph nodes with high risk of bleeding.
Unresectable UCD.
Occasionally, a UCD lymph node may be unresectable because of size or location. This is frequently encountered in the setting of a mediastinal mass that is close to a main bronchus or major blood vessel. If surgery is not possible or too morbid, further treatment is dependent upon the presence of symptoms resulting from compression of neighboring structures or systemic inflammation (Figure 3). When possible, expert advice should be sought to identify the most appropriate therapy for a given patient.
Asymptomatic unresectable UCD.
The management of unresectable UCD requires a judicial approach. The lymphadenopathy in patients with UCD can remain stable or grow slowly over time. There is consensus that a careful watch-and-wait approach can be adopted in patients with normal laboratory values who are currently asymptomatic and unlikely to develop future symptoms resulting from compression of neighboring structures if the mass continues to grow (level 2B evidence).17,19,77 Selected patients who are currently asymptomatic but likely to develop symptoms if the mass continues to grow may need to be treated more aggressively, as if they have compression-related symptomatic unresectable UCD. We recommend regular CT scan monitoring at 12-month intervals as well as annual physical examination and laboratory investigations.
Compression-related symptomatic unresectable UCD.
Several therapeutic options are available if the lymphadenopathy is causing compressive symptoms but cannot be surgically removed. Partial resection to debulk the disease without achieving complete removal can yield good results, but follow-up is required to monitor for growth, with the frequency of follow-up individualized by the location, degree of partial resection, and degree of compression of neighboring structures.15,48,53,62 There have been case reports in which UCD lymph nodes have been rendered amenable to surgery through medical therapy with rituximab with or without steroids. In selected cases, there may be a role for embolization as adjunctive or alternative therapy.
There have been no systematic studies to evaluate the most effective approach in these patients (Table 1).13,69,78,79 In a recent series, 21 patients with unresectable UCD received a variety of therapies, including steroids, chemotherapy, rituximab, and tocilizumab; 7 went on to have successful surgery.19 Overall, the available evidence and consensus opinion (level 2B) support the use of rituximab with or without steroids to reduce the size of compression-related symptomatic unresectable UCD. Any persisting lymphadenopathy should be surgically resected, if feasible. Patients who have unresectable disease after medical therapy but are rendered asymptomatic can be observed. Those remaining symptomatic are candidates for radiotherapy (as described in “Persistent symptomatic unresectable UCD”).
Inflammation-related symptomatic unresectable UCD.
We consider any symptomatic UCD with inflammatory symptoms (night sweats, fevers, anorexia, weight loss) and/or laboratory abnormalities (elevated ESR, elevated CRP, or anemia) to be inflammation related. IL-6 is the well-established driver of symptomatology in most iMCD patients and rare UCD patients with inflammation-related symptoms and laboratory abnormalities. Early studies correlated local production of IL-6 with the systemic manifestations seen in a minority of patients with UCD, because lymph node excision resulted in relief of symptoms along with a decrease in serum IL-6 levels.80-82 However, levels of IL-6 and other inflammatory mediators have not been systematically studied in a large number of UCD cases. Anti–IL-6 agents siltuximab and tocilizumab have been thoroughly studied in iMCD and found to be effective. There is consensus among the panel that it is appropriate to treat inflammation-related symptomatic unresectable UCD with siltuximab or tocilizumab, if elevated CRP/ESR or anemia is present, before considering extensive surgery or radiotherapy (level 2B).83 However, it should be pointed out that limited data exist regarding the effectiveness of this approach.19,84 Any persisting lymphadenopathy should be surgically resected, if feasible. As with compression-related unresectable UCD, patients who continue to have unresectable UCD lymphadenopathy after treatment with anti–IL-6 monoclonal antibody therapy but have become otherwise asymptomatic can be observed. Patients with ongoing troublesome symptomatology should be considered for radiotherapy (as described in “Persistent symptomatic unresectable UCD”), with rituximab with or without steroids being an alternative therapeutic option.
Persistent symptomatic unresectable UCD.
Among unresectable UCD patients with persistent symptoms and lymphadenopathy despite therapies directed at the compression- or inflammation-related symptoms, radiotherapy is an alternative treatment modality (Table 1). Several early case reports attest to the potential utility of radiotherapy in UCD.53,85-90 Chronowski et al91 reported on a small series of 4 patients, 3 of whom achieved complete resolution after irradiation with doses in the order of 4000 cGy. Chan et al92 identified 17 cases of unresectable UCD in the literature treated with similar doses of radiotherapy.53,85,87,88,90,91,93-98 Thirteen achieved disease control, with 7 patients attaining a partial response and 6 a complete response. At a median follow-up of 20 months, only 1 had died as a result of progressive disease. In general, radiotherapy was well tolerated, although 1 patient was reported to have developed PNP.95 However, there is no uniform consensus among the panel members that therapeutic irradiation is desirable (level 3). Radiotherapy does carry the concern of late sequelae, which temper enthusiasm for its routine application in a benign disorder, especially in younger patients.
An alternative approach to radiotherapy for unresectable UCD patients with persistent symptoms and lymphadenopathy is treatment with immunomodulators/immunosuppressants, such as corticosteroids, cyclosporine A, and sirolimus, which are more commonly used for iMCD. However, limited data exist on these treatment approaches (level 3).
Follow-up evaluations.
After completion of the initially planned treatment, patients should be evaluated to determine the disease response to treatment and should be followed longitudinally for relapse and complications. One to 3 months after the initial therapy, the response to treatment should be documented by history, physical examination, laboratory studies, and imaging.
After excision, patients are followed annually with CT and laboratory studies, which include complete blood count, lactate dehydrogenase, and chemistries with liver and renal function and electrolytes, albumin, CRP, and quantitative immunoglobulins. Annual imaging may be discontinued after 5 years if the patient remains disease free.
Patients with persisting symptoms after complete surgical resection.
Occasionally, patients continue to report symptoms after complete surgical extirpation that include persisting fatigue, lethargy, and other constitutional symptoms. These patients should be reevaluated to ensure that an alternative diagnosis, such as iMCD, autoimmune condition, endocrinopathy, depression, chronic fatigue syndrome, or fibromyalgia, was not missed, which may be responsible for the symptoms. Appropriate testing (eg, antinuclear antibody, ESR, CRP, cytokine panel) can help to underpin the presence of an unrecognized disorder giving rise to inflammatory symptomatology. Absent an alternative etiology to explain these symptoms, the systemic therapy approaches described in “Inflammation-related symptomatic unresectable UCD” could be considered, although additional research is needed to assess their use in this setting.
An intermediate of CD.
There has been recent recognition that patients can present with a clinical picture that seems to fall between UCD (1 enlarged lymph node or 1 station of enlarged lymph nodes) and iMCD (>1 station of enlarged lymph nodes, and often >5 stations, with cytokine-driven systemic inflammation). Specifically, these patients often have enlarged lymph nodes in 2 to 3 adjacent lymph node stations, but they lack sufficient clinical and laboratory abnormalities to meet the iMCD diagnostic criteria. These cases have been tentatively described as regional or oligocentric CD. More research is needed, but we felt it was important to recognize this entity in this report, because it may require different treatments than iMCD. In fact, the clinical and pathological features of regional CD resemble those of UCD closely.83 Based on the current limited experiences of the panel and lack of available peer-reviewed evidence, we believe that surgical removal or debulking should be considered (level 2B) over extensive morbid surgeries and systemic therapies, particularly cytotoxic chemotherapies, if possible.19,83 This more conservative approach avoids long-term adverse effects and is prudent given the often indolent clinical course. However, regional CD with inflammatory symptoms may benefit from treatment according to the iMCD treatment algorithm, particularly when exhibiting the PC histopathological subtype.
Disorders associated with UCD.
A number of disorders can present in conjunction with UCD or arise after UCD. These include PNP, Hodgkin disease (HD) or NHL, and FDCS. A survey of the French registry of CD showed that 18% of UCD patients had a complicating disorder.19
PNP.
UCD associated with PNP deserves special mention, because it is life threatening and often accompanied by progressive BO.99 The frequency of this associated disorder seems to be particularly high in the Asian population.100 PNP and BO typically occur in the setting of the HV histopathologic subtype of UCD, sometimes associated with stroma-rich features.41 Complete surgical removal of UCD should be performed in patients with UCD and PNP; this has been reported to often halt or reverse the PNP.100,101 BO has a high fatality rate, despite treatment with a variety of agents alone or in combination, including corticosteroids, rituximab, cyclosporine A, and cyclophosphamide.25,99,102,103 The expert panel agrees that therapy with an anti–IL-6 monoclonal antibody has limited anecdotal efficacy in PNP.
FDCS.
FDCS is a rare form of sarcoma arising from FDCs that can cooccur with the HV histopathologic subtype of UCD.104-106 In a large single-institution series of 66 patients with FDCS, 6 were found to have UCD, and in 2, the diagnosis of UCD preceded that of FDCS. The preferred therapy for localized FDCS is resection, and additional consolidative radiotherapy should be considered for local control.107,108 Chemotherapy is recommended for metastatic FDCS.
Lymphoma.
Distinguishing lymphoma from UCD can be challenging. HD has been reported in patients with UCD; however, the UCD plasmacytic-like histopathological changes may simply represent reactive changes secondary to the HD. UCD and HD are most frequently observed in the same lymph node, emphasizing the need for complete surgical excision.109 A few cases of UCD preceding HD have been described.109-113 A review of 23 cases reported in the literature revealed that 21 cases were described as having PC histopathology, and 2 had mixed histopathology.109 A majority of the HD patients had B symptoms. PC UCD–like lymph node changes may be due to IL-6 and other cytokines produced by Reed-Sternberg cells. Occasionally, CD-like changes are found in a distant lymph node, which can delay the diagnosis of HD.
In contrast, NHL is more often associated with UCD with HV histopathology. In a series reporting NHL and UCD cooccurrence, NHL was less commonly present in the same lymph node as UCD (37%) and was instead found in different anatomical areas (72%).114 Both B- and T-cell lymphomas have been described to cooccur with UCD. FL with features reminiscent of HV UCD may be present in some patients as an unusual morphological variant of FL that may create diagnostic difficulties.114 Taken together, the precise relationship between UCD and both HD and NHL remains unclear. Regardless, the risk of having an HD or NHL diagnosis concurrently or subsequent to a UCD diagnosis seems to be low.
Therapy for UCD and NHL or HD should primarily be dictated by the lymphoma and may include excision, radiotherapy, and chemotherapy.
Discussion
The present consensus guidelines for UCD complement the previous recommendations for iMCD. It is important to accurately diagnose UCD by ruling out conditions with overlapping histopathology, distinguishing UCD from iMCD, and evaluating the resectability and symptomatology associated with each case. We recommend complete surgical resection as the preferred intervention for UCD whenever possible. Recurrence of UCD after complete surgical removal is rare. Occasionally, the distinction between UCD and iMCD is not clearly delineated, with some patients exhibiting more regional lymphadenopathy. These patients typically have a more indolent clinical course and may benefit from UCD-directed rather than iMCD-directed treatment. The most challenging scenario in UCD is that of unresectable UCD. These cases require a judicial approach, with some benefiting from medical cytoreduction followed by surgery and others better served with surgical debulking followed by careful observation. Unresectable asymptomatic UCD patients may also be managed with surveillance alone. In patients with unresectable UCD and inflammation-related symptomatology, anti–IL-6 therapy may be effective. Radiotherapy is an acceptable alternative for unresectable UCD but should probably be avoided in younger patients when possible. Further research is urgently needed into the most effective approaches for unresectable UCD, regional CD, and anti–IL-6 refractory iMCD patients. The CDCN international ACCELERATE natural history registry32 collects data regarding the clinical characteristics, therapies, and outcomes of all forms of CD to advance knowledge regarding this complex and heterogeneous disorder. The University of Pennsylvania and CDCN are also able to consent, coordinate, and receive excess lymph node tissue from clinically warranted lymph node biopsies for research purposes.115 The ACCELERATE registry and lymph node biospecimens support ongoing clinical and translational research efforts, with the twin goals of strengthening the evidence base to help physicians in selecting optimal treatment approaches and identifying new rational therapeutic modalities, particularly for patients with unresectable UCD.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgment
The CDCN coordinated the meetings. The authors of the guidelines had full responsibility for the consensus: building process/methods, data interpretations, treatment recommendations, and writing of the report.
Footnotes
Requests for data sharing should be e-mailed to the corresponding author.
Authorship
Contribution: D.C.F., F.v.R., S.K.P., and S.P. wrote the paper, analyzed data, and designed research; and F.v.R., E.O., G.S., P.V., M.L., A.D., M.I., S.P., S.S., M.S., R.W., D.W., I.M., J.B., N.M., W.B., K.S.E.-J., A.F., M.J.L., S.C., S.K.P., A.G., S.N., K.Y., R.K., T.S.U., C.C., A.C., and D.C.F. wrote the paper.
Conflict--interest disclosure: A.D. receives research support from Celgene, Takeda, Alnylam, Caelum, and Pfizer and serves in an advisory capacity for Janssen, Prothena, and Akcea. D.C.F. has received grant funding from EUSA Pharma and Janssen Pharmaceuticals for the ACCELERATE natural history registry (registered at www.clinicaltrials.gov as #NCT02817997) and has received study drug from Pfizer for a clinical trial of sirolimus (registered at www.clinicaltrials.gov as #NCT03933904). R.K. receives research funding from Genentech, Merck Serono, Pfizer, Boehringer Ingelheim, TopAlliance, Takeda, Incyte, Debiopharm, Medimmune, Sequenom, Foundation Medicine, Konica Minolta, Grifols, Omniseq, and Guardant; receives consultant and/or speaker fees and/or serves on an advisory board for X-Biotech, Neomed, Pfizer, Actuate Therapeutics, Roche, Turning Point Therapeutics, TD2/Volastra, and Bicara Therapeutics, Inc.; has an equity interest in IDbyDNA and CureMatch, Inc.; serves on the boards of CureMatch, Inc., and CureMetrix; and is a cofounder of CureMatch, Inc. E.O. receives consulting fees and serves on an advisory board for EUSA Pharma. S.S. serves on the European Advisory Board for EUSA. G.S. receives consultant and/or speaker fees and/or serves on an advisory board for EUSA Pharma, Janssen, and Takeda. T.S.U. receives research support from Celgene/Bristol-Myers Squibb, Roche, and Merck and serves as a consultant for Seattle Genetics. F.v.R. receives research support from Janssen Pharmaceuticals and consultant fees from EUSA Pharma. R.W. has received research funding from Janssen Pharmaceuticals and served on advisory boards for Janssen Pharmaceuticals. D.W., on behalf of the University of Washington, received research support from Janssen Pharmaceuticals for a role in the central pathology review for the 2014 van Rhee et al Lancet Oncology work. The remaining authors declare no competing financial interests.
Correspondence: Frits van Rhee, University of Arkansas for Medical Sciences, Myeloma Center, 4301 W Markham #816, Little Rock, AR 72205; e-mail: vanrheefrits@uams.edu.
References
- 1.Castleman B, Towne VW. Case records of the Massachusetts General Hospital; weekly clinicopathological exercises; founded by Richard C. Cabot. N Engl J Med. 1954;251(10):396-400. [DOI] [PubMed] [Google Scholar]
- 2.Castleman B, Iverson L, Menendez VP. Localized mediastinal lymphnode hyperplasia resembling thymoma. Cancer. 1956;9(4):822-830. [DOI] [PubMed] [Google Scholar]
- 3.Talat N, Schulte KM. Castleman’s disease: systematic analysis of 416 patients from the literature. Oncologist. 2011;16(9):1316-1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munshi N, Mehra M, van de Velde H, Desai A, Potluri R, Vermeulen J. Use of a claims database to characterize and estimate the incidence rate for Castleman disease. Leuk Lymphoma. 2015;56(5):1252-1260. [DOI] [PubMed] [Google Scholar]
- 5.Talat N, Belgaumkar AP, Schulte KM. Surgery in Castleman’s disease: a systematic review of 404 published cases. Ann Surg. 2012;255(4):677-684. [DOI] [PubMed] [Google Scholar]
- 6.Theate I, Michaux L, Squifflet JP, Martin A, Raphael M. Human herpesvirus 8 and Epstein-Barr virus-related monotypic large B-cell lymphoproliferative disorder coexisting with mixed variant of Castleman’s disease in a lymph node of a renal transplant recipient. Clin Transplant. 2003;17(5):451-454. [DOI] [PubMed] [Google Scholar]
- 7.Sotrel A, Castellano-Sanchez AA, Prusmack C, Birchansky S, Brathwaite C, Ragheb J. Castleman’s disease in a child presenting with a partly mineralized solitary meningeal mass. Pediatr Neurosurg. 2003;38(5):232-237. [DOI] [PubMed] [Google Scholar]
- 8.Caselli E, Padovani D, Di Carlo R, et al. Parotid localized Castleman’s disease and HHV-8 infection: a case report. Head Neck Surg. 2008;265(3):377-380. [DOI] [PubMed] [Google Scholar]
- 9.Akram W, Degliuomini J, Wallack MK, Huang S, Okechukwu E, Eric T. Unicentric Castleman’s disease masquerading as a carcinoid tumor of the small intestine. Am Surg. 2016;82(9):e287-e289. [PubMed] [Google Scholar]
- 10.Kang D, Lee J, Lee H, Baek S. Unicentric Castleman’s disease in the orbit: a case report. Indian J Ophthalmol. 2015;63(6):555-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai MH, Pai HH, Yen PT, Huang TS, Ho YS. Nasopharyngeal Castleman’s disease. J Formos Med Assoc. 1996;95(11):877-880. [PubMed] [Google Scholar]
- 12.He X, Wang Q, Wu Y, et al. Comprehensive analysis of 225 Castleman’s diseases in the oral maxillofacial and neck region: a rare disease revisited. Clin Oral Investig. 2018;22(3):1285-1295. [DOI] [PubMed] [Google Scholar]
- 13.Yu L, Tu M, Cortes J, et al. Clinical and pathological characteristics of HIV- and HHV-8-negative Castleman disease. Blood. 2017;129(12):1658-1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cronin DM, Warnke RA. Castleman disease: an update on classification and the spectrum of associated lesions. Adv Anat Pathol. 2009;16(4):236-246. [DOI] [PubMed] [Google Scholar]
- 15.Keller AR, Hochholzer L, Castleman B. Hyaline-vascular and plasma-cell types of giant lymph node hyperplasia of the mediastinum and other locations. Cancer. 1972;29(3):670-683. [DOI] [PubMed] [Google Scholar]
- 16.Herrada J, Cabanillas F, Rice L, Manning J, Pugh W. The clinical behavior of localized and multicentric Castleman disease. Ann Intern Med. 1998;128(8):657-662. [DOI] [PubMed] [Google Scholar]
- 17.Soumerai JD, Sohani AR, Abramson JS. Diagnosis and management of Castleman disease. Cancer Control. 2014;21(4):266-278. [DOI] [PubMed] [Google Scholar]
- 18.Frizzera G. Castleman’s disease and related disorders. Semin Diagn Pathol. 1988;5(4):346-364. [PubMed] [Google Scholar]
- 19.Boutboul D, Fadlallah J, Chawki S, et al. Treatment and outcome of unicentric Castleman disease: a retrospective analysis of 71 cases. Br J Haematol. 2019;186(2):269-273. [DOI] [PubMed] [Google Scholar]
- 20.Ruggieri G, Barsotti P, Coppola G, et al. Membranous nephropathy associated with giant lymph node hyperplasia. A case report with histological and ultrastructural studies. Am J Nephrol. 1990;10(4):323-328. [DOI] [PubMed] [Google Scholar]
- 21.Mandreoli M, Casanova S, Vianelli N, Pasquali S, Zucchelli P. Remission of nephrotic syndrome due to AA amyloidosis and initiation of glomerular repair after surgical resection of localized Castleman’s disease. Nephron. 2002;90(3):336-340. [DOI] [PubMed] [Google Scholar]
- 22.Lachmann HJ, Gilbertson JA, Gillmore JD, Hawkins PN, Pepys MB. Unicentric Castleman’s disease complicated by systemic AA amyloidosis: a curable disease. QJM. 2002;95(4):211-218. [DOI] [PubMed] [Google Scholar]
- 23.Fayand A, Boutboul D, Galicier L, et al. Epidemiology of Castleman disease associated with AA amyloidosis: description of 2 new cases and literature review. Amyloid. 2019;26(4):197-202. [DOI] [PubMed] [Google Scholar]
- 24.Raza HA, Nokes BT, Rosenthal AC, et al. Unicentric castleman disease complicated by paraneoplastic bronchiolitis obliterans and pemphigus. Respir Med Case Rep. 2018;25:129-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohzono A, Sogame R, Li X, et al. Clinical and immunological findings in 104 cases of paraneoplastic pemphigus. Br J Dermatol. 2015;173(6):1447-1452. [DOI] [PubMed] [Google Scholar]
- 26.Gerald W, Kostianovsky M, Rosai J. Development of vascular neoplasia in Castleman’s disease. Report of seven cases. Am J Surg Pathol. 1990;14(7):603-614. [DOI] [PubMed] [Google Scholar]
- 27.Chang KC, Wang YC, Hung LY, et al. Monoclonality and cytogenetic abnormalities in hyaline vascular Castleman disease. Mod Pathol. 2014;27(6):823-831. [DOI] [PubMed] [Google Scholar]
- 28.Cokelaere K, Debiec-Rychter M, De Wolf-Peeters C, Hagemeijer A, Sciot R. Hyaline vascular Castleman’s disease with HMGIC rearrangement in follicular dendritic cells: molecular evidence of mesenchymal tumorigenesis. Am J Surg Pathol. 2002;26(5):662-669. [DOI] [PubMed] [Google Scholar]
- 29.Pauwels P, Dal Cin P, Vlasveld LT, Aleva RM, van Erp WF, Jones D. A chromosomal abnormality in hyaline vascular Castleman’s disease: evidence for clonal proliferation of dysplastic stromal cells. Am J Surg Pathol. 2000;24(6):882-888. [DOI] [PubMed] [Google Scholar]
- 30.Li Z, Lan X, Li C, et al. Recurrent PDGFRB mutations in unicentric Castleman disease. Leukemia. 2019;33(4):1035-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nabel CS, Sameroff S, Shilling D, et al. Virome capture sequencing does not identify active viral infection in unicentric and idiopathic multicentric Castleman disease. PLoS One. 2019;14(6):e0218660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Castleman Disease Collaborative Network ACCELERATE natural history study. Available at: www.CDCN.org/ACCELERATE. Accessed 3 March 2020.
- 33.Beckham TH, Yang JC, Chau KW, Noy A, Yahalom J. Excellent outcomes with surgery or radiotherapy in the management of Castleman disease including a case of oligocentric disease. Clin Lymphoma Myeloma Leuk. 2020;20(10):685-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dispenzieri A, Armitage JO, Loe MJ, et al. The clinical spectrum of Castleman’s disease. Am J Hematol. 2012;87(11):997-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jiang JP, Shen XF, Du JF, Guan WX. A retrospective study of 34 patients with unicentric and multicentric Castleman’s disease: experience from a single institution. Oncol Lett. 2018;15(2):2407-2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lan X, Li Z, Zhang M. Analysis of clinical characteristics and prognosis factors of 71 cases with HIV-negative Castleman’s disease: hypoproteinemia is an unfavorable prognostic factor which should be treated appropriately. J Cancer Res Clin Oncol. 2018;144(7):1265-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luo JM, Li S, Huang H, et al. Clinical spectrum of intrathoracic Castleman disease: a retrospective analysis of 48 cases in a single Chinese hospital. BMC Pulm Med. 2015;15:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prakash G, Bal A, Malhotra P, et al. Presentation and outcome of Castleman’s disease in immunocompetent hosts. Indian J Hematol Blood Transfus. 2016;32(4):468-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sopfe J, Endres A, Campbell K, et al. Castleman disease in pediatrics: insights on presentation, treatment, and outcomes from a two-site retrospective cohort study. Pediatr Blood Cancer. 2019;66(5):e27613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Uysal B, Demiral S, Gamsiz H, Dincoglan F, Sager O, Beyzadeoglu M. Castleman’s disease and radiotherapy: a single center experience. J Cancer Res Ther. 2015;11(1):170-173. [DOI] [PubMed] [Google Scholar]
- 41.Wang L, Nong L, Li F, et al. Predominant stroma-rich feature in hyaline vascular variant of Castleman disease is associated with paraneoplastic pemphigus. Am J Clin Pathol. 2020;154(3):403-413. [DOI] [PubMed] [Google Scholar]
- 42.Wang S, Chen S, Xu J, Cai S. Clinicopathological characteristics of unicentric retroperitoneal Castleman’s disease: a study of 14 cases. World J Surg Oncol. 2016;14(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang J, Li C, Lv L, et al. Clinical and experimental study of Castleman disease in children. Pediatr Blood Cancer. 2015;62(1):109-114. [DOI] [PubMed] [Google Scholar]
- 44.Zhang X, Rao H, Xu X, et al. Clinical characteristics and outcomes of Castleman disease: a multicenter study of 185 Chinese patients. Cancer Sci. 2018;109(1):199-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou N, Huang CW, Huang C, Liao W. The characterization and management of Castleman’s disease. J Int Med Res. 2012;40(4):1580-1588. [DOI] [PubMed] [Google Scholar]
- 46.National Comprehensive Cancer Network NCCN guidelines and clinical resources. https://www.nccn.org/professionals/physician_gls/categories_of_consensus.aspx. Accessed 3 March 2020.
- 47.Krishnan J, Danon AD, Frizzera G. Reactive lymphadenopathies and atypical lymphoproliferative disorders. Am J Clin Pathol. 1993;99(4):385-396. [DOI] [PubMed] [Google Scholar]
- 48.Frizzera G, Peterson BA, Bayrd ED, Goldman A. A systemic lymphoproliferative disorder with morphologic features of Castleman’s disease: clinical findings and clinicopathologic correlations in 15 patients. J Clin Oncol. 1985;3(9):1202-1216. [DOI] [PubMed] [Google Scholar]
- 49.McCarty MJ, Vukelja SJ, Banks PM, Weiss RB. Angiofollicular lymph node hyperplasia (Castleman’s disease). Cancer Treat Rev. 1995;21(4):291-310. [DOI] [PubMed] [Google Scholar]
- 50.Hill AJ, Tirumani SH, Rosenthal MH, et al. Multimodality imaging and clinical features in Castleman disease: single institute experience in 30 patients. Br J Radiol. 2015;88(1049):20140670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Flendrig J, Schillings PHM. Benign giant lymphoma: the clinical signs and symptoms and the morphological aspects. Folia Med (Plovdiv). 1969;12:119-120. [Google Scholar]
- 52.Kasantikul V, Panyavoravut V, Benjavongkulchai S, Panichabhongse V.. Castleman’s disease: a clinicopathologic study of 12 cases. J Med Assoc Thai. 1997;80(3):195-201. [PubMed] [Google Scholar]
- 53.Bowne WB, Lewis JJ, Filippa DA, et al. The management of unicentric and multicentric Castleman’s disease: a report of 16 cases and a review of the literature. Cancer. 1999;85(3):706-717. [DOI] [PubMed] [Google Scholar]
- 54.van Rhee F, Stone K, Szmania S, Barlogie B, Singh Z. Castleman disease in the 21st century: an update on diagnosis, assessment, and therapy. Clin Adv Hematol Oncol. 2010;8(7):486-498. [PubMed] [Google Scholar]
- 55.Parez N, Bader-Meunier B, Roy CC, Dommergues JP. Paediatric Castleman disease: report of seven cases and review of the literature. Eur J Pediatr. 1999;158(8):631-637. [DOI] [PubMed] [Google Scholar]
- 56.Ye B, Gao SG, Li W, et al. A retrospective study of unicentric and multicentric Castleman’s disease: a report of 52 patients. Med Oncol. 2010;27(4):1171-1178. [DOI] [PubMed] [Google Scholar]
- 57.Chen CH, Liu HC, Tung KY, Lee JJ, Liu CL, Liu TP. Surgical outcome of superficial and deep Castleman disease. ANZ J Surg. 2007;77(5):339-343. [DOI] [PubMed] [Google Scholar]
- 58.Ko SF, Ng SH, Hsieh MJ, et al. Castleman disease of the pleura: experience with eight surgically proven cases. Ann Thorac Surg. 2003;76(1):219-224. [DOI] [PubMed] [Google Scholar]
- 59.Mohanna S, Sanchez J, Ferrufino JC, Bravo F, Gotuzzo E. Characteristics of Castleman’s disease in Peru. Eur J Intern Med. 2006;17(3):170-174. [DOI] [PubMed] [Google Scholar]
- 60.Kim JH, Jun TG, Sung SW, et al. Giant lymph node hyperplasia (Castleman’s disease) in the chest. Ann Thorac Surg. 1995;59(5):1162-1165. [DOI] [PubMed] [Google Scholar]
- 61.Mitsos S, Stamatopoulos A, Patrini D, George RS, Lawrence DR, Panagiotopoulos N. The role of surgical resection in unicentric Castleman’s disease: a systematic review. Adv Respir Med. 2018;86(1):36-43. [DOI] [PubMed] [Google Scholar]
- 62.Olscamp G, Weisbrod G, Sanders D, Delarue N, Mustard R. Castleman disease: unusual manifestations of an unusual disorder. Radiology. 1980;135(1):43-48. [DOI] [PubMed] [Google Scholar]
- 63.Ko SF, Hsieh MJ, Ng SH, et al. Imaging spectrum of Castleman’s disease. AJR Am J Roentgenol. 2004;182(3):769-775. [DOI] [PubMed] [Google Scholar]
- 64.Kwon S, Lee KS, Ahn S, Song I, Kim TS. Thoracic Castleman disease: computed tomography and clinical findings. J Comput Assist Tomogr. 2013;37(1):1-8. [DOI] [PubMed] [Google Scholar]
- 65.Bonekamp D, Horton KM, Hruban RH, Fishman EK. Castleman disease: the great mimic. Radiographics. 2011;31(6):1793-1807. [DOI] [PubMed] [Google Scholar]
- 66.Walter JF, Rottenberg RW, Cannon WB, Sheridan LA, Pizzimenti J, Orr JT. Giant mediastinal lymph node hyperplasia (Castleman’s disease): angiographic and clinical features. AJR Am J Roentgenol. 1978;130(3):447-450. [DOI] [PubMed] [Google Scholar]
- 67.Lanier BJ, Cummings CW. Giant lymphoid hyperplasia presenting as a highly vascularized parapharyngeal mass. Otolaryngol Head Neck Surg. 1982;90(4):426-430. [DOI] [PubMed] [Google Scholar]
- 68.Williams HR, Millner PA, Coral A. Castleman’s disease of the erector spinae muscle. Skeletal Radiol. 1998;27(11):637-640. [DOI] [PubMed] [Google Scholar]
- 69.Safford SD, Lagoo AS, Mahaffey SA. Preoperative embolization as an adjunct to the operative management of mediastinal Castleman disease. J Pediatr Surg. 2003;38(9):E21-E23. [DOI] [PubMed] [Google Scholar]
- 70.Newlon JL, Couch M, Brennan J. Castleman’s disease: three case reports and a review of the literature. Ear Nose Throat J. 2007;86(7):414-418. [PubMed] [Google Scholar]
- 71.Robert JH, Sgourdos G, Kritikos N, Didier D, Terraz S. Preoperative embolization of hypervascular Castleman’s disease of the mediastinum. Cardiovasc Intervent Radiol. 2008;31(1):186-188. [DOI] [PubMed] [Google Scholar]
- 72.Swee W, Housseini AM, Angle JF, et al. Preoperative embolization of Castleman’s disease using microspheres. Ann Thorac Surg. 2009;88(6):1999-2001. [DOI] [PubMed] [Google Scholar]
- 73.Sánchez de Toledo Sancho J, Fàbrega Sabaté J, Marhuenda Irastorza C, et al. Castleman disease [in Spanish]. An Pediatr (Barc). 2005;63(1):68-71. [DOI] [PubMed] [Google Scholar]
- 74.Sanchez-Ros-Sanchez A, Infante-Cossio P, Gonzalez-Garcia A, Borrero-Martin JJ. Preoperative embolization for the treatment of cervical Castleman disease. J Craniofac Surg. 2012;23(3):e257-e259. [DOI] [PubMed] [Google Scholar]
- 75.Nagano S, Yokouchi M, Yamamoto T, et al. Castleman’s disease in the retroperitoneal space mimicking a paraspinal schwannoma: a case report. World J Surg Oncol. 2013;11:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gorospe L, Valdebenito-Montecino AP, Muñoz-Molina GM. Preoperative embolization of mediastinal Castleman’s disease presenting with stroke. Asian Cardiovasc Thorac Ann. 2017;25(2):158-159. [DOI] [PubMed] [Google Scholar]
- 77.Wong RSM. Unicentric Castleman disease. Hematol Oncol Clin North Am. 2018;32(1):65-73. [DOI] [PubMed] [Google Scholar]
- 78.Bandera B, Ainsworth C, Shikle J, Rupard E, Roach M. Treatment of unicentric Castleman disease with neoadjuvant rituximab. Chest. 2010;138(5):1239-1241. [DOI] [PubMed] [Google Scholar]
- 79.Estephan FF, Elghetany MT, Berry M, Jones DV Jr.. Complete remission with anti-CD20 therapy for unicentric, non-HIV-associated, hyaline-vascular type, Castleman’s disease. Cancer Invest. 2005;23(2):191. [PubMed] [Google Scholar]
- 80.Yoshizaki K, Matsuda T, Nishimoto N, et al. Pathogenic significance of interleukin-6 (IL-6/BSF-2) in Castleman’s disease. Blood. 1989;74(4):1360-1367. [PubMed] [Google Scholar]
- 81.Leger-Ravet MB, Peuchmaur M, Devergne O, et al. Interleukin-6 gene expression in Castleman’s disease. Blood. 1991;78(11):2923-2930. [PubMed] [Google Scholar]
- 82.Post GR, Bell RC, Rjoop A, Lobo RH, Yuan Y, Post SR. Diagnostic utility of interleukin-6 expression by immunohistochemistry in differentiating Castleman disease subtypes and reactive lymphadenopathies. Ann Clin Lab Sci. 2016;46(5):474-479. [PubMed] [Google Scholar]
- 83.Oksenhendler E, Boutboul D, Fajgenbaum D, et al. The full spectrum of Castleman disease: 273 patients studied over 20 years. Br J Haematol. 2018;180(2):206-216. [DOI] [PubMed] [Google Scholar]
- 84.Abid MB, Peck R, Abid MA, et al. Is tocilizumab a potential therapeutic option for refractory unicentric Castleman disease? Hematol Oncol. 2018;36(1):320-323. [DOI] [PubMed] [Google Scholar]
- 85.Weisenburger DD, DeGowin RL, Gibson P, Armitage JO. Remission of giant lymph node hyperplasia with anemia after radiotherapy. Cancer. 1979;44(2):457-462. [DOI] [PubMed] [Google Scholar]
- 86.Nordstrom DG, Tewfik HH, Latourette HB. Giant lymph node hyperplasia: a review of literature and report of two cases of plasma cell variant responding to radiation therapy. Int J Radiat Oncol Biol Phys. 1978;4(11-12):1045-1048. [DOI] [PubMed] [Google Scholar]
- 87.Fitzpatrick PJ, Brown TC. Angiofollicular lymph node hyperplasia. Can Med Assoc J. 1968;99(25):1259-1262. [PMC free article] [PubMed] [Google Scholar]
- 88.Stokes SH, Griffith RC, Thomas PR. Angiofollicular lymph node hyperplasia (Castleman’s disease) associated with vertebral destruction. Cancer. 1985;56(4):876-879. [DOI] [PubMed] [Google Scholar]
- 89.Sethi T, Joshi K, Sharma SC, Gupta BD. Radiation therapy in the management of giant lymph node hyperplasia. Br J Radiol. 1990;63(752):648-650. [DOI] [PubMed] [Google Scholar]
- 90.Veldhuis GJ, van der Leest AH, de Wolf JT, de Vries EG, Vellenga E. A case of localized Castleman’s disease with systemic involvement: treatment and pathogenetic aspects. Ann Hematol. 1996;73(1):47-50. [DOI] [PubMed] [Google Scholar]
- 91.Chronowski GM, Ha CS, Wilder RB, Cabanillas F, Manning J, Cox JD. Treatment of unicentric and multicentric Castleman disease and the role of radiotherapy. Cancer. 2001;92(3):670-676. [DOI] [PubMed] [Google Scholar]
- 92.Chan KL, Lade S, Prince HM, Harrison SJ. Update and new approaches in the treatment of Castleman disease. J Blood Med. 2016;7:145-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nordstrom DG, Tewfik HH, Latourette HB. Plasma cell giant lymph node hyperplasia responding to radiation therapy. AJR Am J Roentgenol. 1978;130(1):169-171. [DOI] [PubMed] [Google Scholar]
- 94.Massey GV, Kornstein MJ, Wahl D, Huang XL, McCrady CW, Carchman RA. Angiofollicular lymph node hyperplasia (Castleman’s disease) in an adolescent female. Clinical and immunologic findings. Cancer. 1991;68(6):1365-1372. [DOI] [PubMed] [Google Scholar]
- 95.Neuhof D, Debus J. Outcome and late complications of radiotherapy in patients with unicentric Castleman disease. Acta Oncol. 2006;45(8):1126-1131. [DOI] [PubMed] [Google Scholar]
- 96.Li YM, Liu PH, Zhang YH, et al. Radiotherapy of unicentric mediastinal Castleman’s disease. Chin J Cancer. 2011;30(5):351-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Matthiesen C, Ramgopol R, Seavey J, Ahmad S, Herman T. Intensity modulated radiation therapy (IMRT) for the treatment of unicentric Castlemans disease: a case report and review of the use of radiotherapy in the literature. Radiol Oncol. 2012;46(3):265-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Miranda FA, Faria VH, Arruda GV, Silva LG. Radiation therapy in the treatment of unicentric Castleman’s disease. J Bras Pneumol. 2013;39(1):116-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nikolskaia OV, Nousari CH, Anhalt GJ. Paraneoplastic pemphigus in association with Castleman’s disease. Br J Dermatol. 2003;149(6):1143-1151. [DOI] [PubMed] [Google Scholar]
- 100.Zhang J, Qiao QL, Chen XX, et al. Improved outcomes after complete resection of underlying tumors for patients with paraneoplastic pemphigus: a single-center experience of 22 cases. J Cancer Res Clin Oncol. 2011;137(2):229-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fang Y, Zhao L, Yan F, Cui X, Xia Y, Duren A. A critical role of surgery in the treatment for paraneoplastic pemphigus caused by localized Castleman’s disease. Med Oncol. 2010;27(3):907-911. [DOI] [PubMed] [Google Scholar]
- 102.Maldonado F, Pittelkow MR, Ryu JH. Constrictive bronchiolitis associated with paraneoplastic autoimmune multi-organ syndrome. Respirology. 2009;14(1):129-133. [DOI] [PubMed] [Google Scholar]
- 103.Dong Y, Wang M, Nong L, et al. Clinical and laboratory characterization of 114 cases of Castleman disease patients from a single centre: paraneoplastic pemphigus is an unfavourable prognostic factor. Br J Haematol. 2015;169(6):834-842. [DOI] [PubMed] [Google Scholar]
- 104.Chan JK, Tsang WY, Ng CS. Follicular dendritic cell tumor and vascular neoplasm complicating hyaline-vascular Castleman’s disease. Am J Surg Pathol. 1994;18(5):517-525. [DOI] [PubMed] [Google Scholar]
- 105.Chan AC, Chan KW, Chan JK, Au WY, Ho WK, Ng WM. Development of follicular dendritic cell sarcoma in hyaline-vascular Castleman’s disease of the nasopharynx: tracing its evolution by sequential biopsies. Histopathology. 2001;38(6):510-518. [DOI] [PubMed] [Google Scholar]
- 106.Chan JK, Fletcher CD, Nayler SJ, Cooper K. Follicular dendritic cell sarcoma. Clinicopathologic analysis of 17 cases suggesting a malignant potential higher than currently recognized. Cancer. 1997;79(2):294-313. [PubMed] [Google Scholar]
- 107.Jain P, Milgrom SA, Patel KP, et al. Characteristics, management, and outcomes of patients with follicular dendritic cell sarcoma. Br J Haematol. 2017;178(3):403-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gounder M, Desai V, Kuk D, et al. Impact of surgery, radiation and systemic therapy on the outcomes of patients with dendritic cell and histiocytic sarcomas. Eur J Cancer. 2015;51(16):2413-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Larroche C, Cacoub P, Soulier J, et al. Castleman’s disease and lymphoma: report of eight cases in HIV-negative patients and literature review. Am J Hematol. 2002;69(2):119-126. [DOI] [PubMed] [Google Scholar]
- 110.Maheswaran PR, Ramsay AD, Norton AJ, Roche WR. Hodgkin’s disease presenting with the histological features of Castleman’s disease. Histopathology. 1991;18(3):249-253. [DOI] [PubMed] [Google Scholar]
- 111.Brice P, Marolleau JP, D’Agay MF, Epardeau B, Gisselbrecht C. Autoimmune hemolytic anemia disclosing Hodgkin’s disease associated with Castleman’s disease. Nouv Rev Fr Hematol. 1991;33(3):273-274. [PubMed] [Google Scholar]
- 112.Molinié V, Périé G, Mélo I, Melo C, Audouin J, Diebold J. Association of Castleman’s disease and Hodgkin’s disease. Eight cases and review of the literature [in French]. Ann Pathol. 1994;14(6):384-391. [PubMed] [Google Scholar]
- 113.Zarate-Osorno A, Medeiros LJ, Danon AD, Neiman RS. Hodgkin’s disease with coexistent Castleman-like histologic features. A report of three cases. Arch Pathol Lab Med. 1994;118(3):270-274. [PubMed] [Google Scholar]
- 114.Pina-Oviedo S, Wang W, Vicknair E, Manning JT Jr., Medeiros LJ. Follicular lymphoma with hyaline-vascular Castleman disease-like follicles and CD20 positive follicular dendritic cells. Pathology. 2017;49(5):544-547. [DOI] [PubMed] [Google Scholar]
- 115.Castleman Disease Collaborative Network Donate tissue samples. Available at: www.CDCN.org/samples. Accessed 3 March 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.