Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has critically affected healthcare delivery in the United States. Little is known on its impact on the utilization of emergency department (ED) services, particularly for conditions that might be medically urgent. The objective of this study was to explore trends in the number of outpatient (treat and release) ED visits during the COVID-19 pandemic.
Methods
We conducted a cross-sectional, retrospective study of outpatient emergency department visits from January 1, 2019 to August 31, 2020 using data from a large, urban, academic hospital system in Utah. Using weekly counts and trend analyses, we explored changes in overall ED visits, by patients' area of residence, by medical urgency, and by specific medical conditions.
Results
While outpatient ED visits were higher (+6.0%) in the first trimester of 2020 relative to the same period in 2019, the overall volume between January and August of 2020 was lower (−8.1%) than in 2019. The largest decrease occurred in April 2020 (−30.4%), followed by the May to August period (−12.8%). The largest declines were observed for visits by out-of-state residents, visits classified as non-emergent, primary care treatable or preventable, and for patients diagnosed with hypertension, diabetes, headaches and migraines, mood and personality disorders, fluid and electrolyte disorders, and abdominal pain. Outpatient ED visits for emergent conditions, such as palpitations and tachycardia, open wounds, syncope and collapse remained relatively unchanged, while lower respiratory disease-related visits were 67.5% higher in 2020 relative to 2019, particularly from March to April 2020. However, almost all types of outpatient ED visits bounced back after May 2020.
Conclusions
Overall outpatient ED visits declined from mid-March to August 2020, particularly for non-medically urgent conditions which can be treated in other more appropriate care settings. Our findings also have implications for insurers, policymakers, and other stakeholders seeking to assist patients in choosing more appropriate setting for their care during and after the pandemic.
Keywords: COVID-19, Emergency department, Healthcare utilization, Non-urgent visits
1. Introduction
The spread of the coronavirus disease 2019 (COVID-19) in spring of 2020 led to a sudden inflow of patients with acute respiratory symptoms to hospitals in the United States. Many state officials issued stay at home orders, and restricted elective medical and surgical procedures to redirect constrained hospital resources to COVID-19 patients. Uncertainty on the spread of COVID-19 and changing recommendations in the following months generated confusion and fear among many residents and disconnected many patients from potentially necessary health care [[1], [2], [3]]. One particularly hard-hit area were emergency departments (EDs), which serve as a safety net for many patients and generally treat individuals with acute conditions. However, more than one-third of all ED visits are estimated to be non-urgent and can be treated in other care settings [[4], [5], [6]]. Common reasons for ED utilization for non-urgent conditions include convenience and timely access to care, lack of alternatives, discrepancies in patient-provider perceptions, lapse of care management, and the need for a second-opinion [4,6,7]. The legal mandate to treat all patients in the ED, independent of their ability to pay, may further contribute to care seeking in such settings [4,6,7].
As shelter in place orders and fear of COVID-19 spread across the country, one could expect ED use to decline if people choose to forgo or postpone their non-urgent care needs or use other care settings. Although postponed or foregone care can result in impaired or even detrimental short- and long-term health outcomes, particularly for high-risk patients, reductions in care for non-urgent visits may provide the opportunity to shift resources to urgent care seekers. A current report indicates that patients are more likely to call their primary care provider or the hospital help line before deciding to seek care in the ED during the ongoing pandemic [3]. Early evidence indeed suggests that outpatient, ED visits, and hospital admissions declined by up to 60% from February to April 2020 in some parts of the country, followed by a bounce back after June [2,[8], [9], [10], [11], [12], [13], [14]]. However, little is known about the composition of reductions in urgent relative to non-urgent visits.
In this study, we aimed to analyze the pattern of outpatient (treat and release) ED visits between January and August 2020 compared to January through August 2019 based on the level of urgency and the spatial composition of the patients' home residence. Focusing only on outpatient ED visits allows us to identify common care events that can be classified as either urgent or non-urgent encounters using the New York University (NYU) ED algorithm, and review whether COVID-19 led to change in the proportion of urgent to non-urgent encounters. Our findings can provide critical information to stakeholders and health policymakers to develop evidence-based interventions towards a more patient focused and structurally competent healthcare system during the ongoing COVID-19 pandemic and beyond.
2. Methods
2.1. Study design and data source
This was a retrospective, cross-sectional study using data from the Enterprise Data Warehouse (EDW). The EDW, managed and maintained by the University of Utah Health Science Data Resource Center, is the long-term data mart for patient medical, financial, and administrative data. The EDW integrates the historical and comprehensive medical and clinical patient records across the University of Utah Healthcare Systems for more than 2.4 million patients for all health system interactions. The data also include demographic and clinical information. EDW data from the University of Utah Health Emergency Department, which is a fully approved Level 1 Trauma facility and tertiary referral center staffed by physicians 24 h a day, 7 days a week, was used in this study. The department is one of four EDs in the city in a metropolitan area of about 1.2 million residents and has a census of about 50,000 patient visits annually and provides care for acute emergencies in all subspecialties of medicine and surgery. Patients from all over Utah, Nevada, Wyoming, Idaho and western Colorado are referred to the emergency department for definitive medical care. During the COVID-19 pandemic, all area hospitals offered COVID-19 testing and medical care with no single facility designated specifically to care for or evaluate potential COVID-19 patients.
2.2. Study outcomes
Outpatient ED visits were identified as visits to the ED of the hospital system by all patients (including children 0 to 17 years of age) who were discharged within one day from the ED. To examine changes in trends in weekly outpatient ED visit volumes, we obtained data from January 1, 2019 to August 31, 2020. We examined overall weekly outpatient ED visit trends, by patients' area of residence to identify changes in care related to the stay-at-home recommendation and other social distancing directives that took place in April 2020. We used the patients' zip code of residence to identify changes in the number of patients coming from Salt Lake City (inner-city), the rest of the state, and out of state.
The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) was used to identify the principal diagnoses and to characterize outpatient ED visits by medical urgency and by specific clinical diagnoses. To classify visits by medical urgency, we used the updated New York University (NYU) ED algorithm (Appendix 1) [15,16]. This previously validated algorithm assigns probabilities and classifies each ED visit as urgent (emergent-not preventable/avoidable: immediate care in an ED setting needed and the condition could not have been prevented/avoided with ambulatory care, such as chest pain, end stage renal disease, tachycardia, palpitations), emergent but preventable or avoidable (immediate care in an ED setting needed but the condition could have been prevented or avoided with timely and effective ambulatory care, such as dehydration, asthma with acute exacerbation, diabetes with hyper – or hypoglycemia), emergent but primary care treatable (care is needed within 12 h but could be provided in a primary care setting, such as quadrant pain, epigastric pain, abdominal pain), and non-emergent (immediate care not required within 12 h, such as headache, cough, low back pain, fatigue and weakness). Similar to previous work, we allocated each visit to one of the four categories related to emergency status when the assigned probability of the algorithm was higher than 50% for said category [17]. We also analyzed visits classified separately as injury-related by the algorithm (Appendix 1).
The Agency for Healthcare Research and Quality (AHRQ) single level Clinical Classification Software (CCS) was used to categorize outpatient ED visits into 16 expanded and clinically meaningful categories based on similarities among the individual ICD-10 codes, namely strains, sprains, and fractures; open wounds; superficial injuries; suicide and self-inflicted injuries; syncope and collapse; palpitations and tachycardia; abdominal pain; chest pain; fluid and electrolyte disorders; headaches and migraines; spondylosis, intervertebral disc disorders, and other back problems; nausea and vomiting; hypertension; diabetes; mood and personality disorders; and other lower respiratory diseases [18]. Finally, we also included information on overall inpatient ED visits (admission to the hospital through the ED).
2.3. Data analysis
We stratified data a priori into three different time periods based on the stay at home directive (January to March 2020; pre-directive: weeks 1 to 13, April 2020; directive: weeks 14 to 17, and May to August 2020; post-directive: weeks 18 to 35) and compared trends in outpatient ED visits volumes to the same periods in 2019. We then used weekly trend analyses for 2019 and 2020 to evaluate the number of outpatient ED visits that fall into one of the five categories of the NYU algorithm and the 16 CCS categories. All data analyses were performed using Stata version 16.1 (StataCorp) and SAS version 9.4 (SAS Institute) and trend graphs were generated in Microsoft Excel. The data used in this study were deidentified and the study was reviewed and approved by the institutional review board (IRB) at the University of Utah (IRB 00136921).
3. Results
From January 1, 2019 to August 31, 2020 the ED had approximately 80,000 outpatient visits. Of those, 32,937 and 30,276 occurred between January and August in 2019 and 2020, respectively, which corresponded to an 8.1% decrease in ED visits volume in 2020 (Table 1 and Fig. 1 ). Over the study period, the ED had higher shares of outpatient ED visits by adults 18 to 44 years of age (53.2%), females (53.7%), Non-Hispanic Whites (68.4%), and those with private health insurance (48.2%) or Medicaid (22.0%) coverage (Appendix 2). The most common reasons in both years for outpatient ED visits were abdominal (5.5%) and chest pain (5.4%), strains, sprains and fractures (4.0%), and fluid and electrolyte disorders (3.9%). About 31% of all outpatient ED visits were classified as emergent or were injury related, while almost 44% were primary care treatable, preventable or not emergent.
Table 1.
Emergency department visits from January 1 to August 31 in 2019 and 2020
| Total |
January to March |
April |
May to August |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| Number of outpatient ED visits | 63,213 | 32,937 | 30,276 | 12,053 | 12,780 | 4017 | 2794 | 16,867 | 14,702 |
| Area of residence (%) | |||||||||
| Inner City | 26,584 (42.1) | 13,638 (41.4) | 12,946 (42.8) | 5023 (41.7) | 5326 (41.7) | 1653 (41.2) | 1257 (45.0) | 6962 (41.3) | 6363 (43.3) |
| Inner State; not inner city | 32,106 (50.8) | 16,686 (50.7) | 15,420 (50.9) | 6077 (50.4) | 6582 (51.5) | 2045 (50.9) | 1430 (51.2) | 8564 (50.8) | 7408 (50.4) |
| Out of State | 4523 (7.2) | 2613 (7.9) | 1910 (6.3) | 953 (7.9) | 872 (6.8) | 319 (7.9) | 107 (3.8) | 1341 (8.0) | 931 (6.3) |
| NYU ED Algorithm Classification (%) | |||||||||
| Emergent - Not preventable/avoidable | 11,076 (17.5) | 5844 (17.7) | 5232 (17.3) | 2093 (17.4) | 2295 (18.0) | 754 (18.8) | 451 (16.1) | 2997 (17.8) | 2486 (16.9) |
| Emergent - Preventable/avoidable | 1812 (2.9) | 1075 (3.3) | 737 (2.4) | 417 (3.5) | 396 (3.1) | 141 (3.5) | 73 (2.6) | 517 (3.1) | 268 (1.8) |
| Emergent - Primary Care Treatable | 12,923 (20.4) | 6796 (20.6) | 6127 (20.2) | 2549 (21.1) | 2589 (20.3) | 862 (21.5) | 560 (20.0) | 3385 (20.1) | 2978 (20.3) |
| Not Emergent | 13,587 (21.5) | 6846 (20.8) | 6741 (22.3) | 2557 (21.2) | 2865 (22.4) | 856 (21.3) | 625 (22.4) | 3433 (20.4) | 3251 (22.1) |
| Injuries | 8338 (13.2) | 4400 (13.4) | 3898 (12.9) | 1563 (13.0) | 1462 (11.4) | 496 (12.3) | 343 (12.3) | 2381 (14.1) | 2093 (14.2) |
| Clinical conditions (%) | |||||||||
| Emergent & Injuries | |||||||||
| Chest pain | 3397 (5.4) | 1788 (5.4) | 1609 (5.3) | 653 (5.4) | 634 (5.0) | 221 (5.5) | 169 (6.0) | 914 (5.4) | 806 (5.5) |
| Strains, sprains, and fractures | 2425 (3.8) | 1304 (4.0) | 1121 (3.7) | 485 (4.0) | 463 (3.6) | 160 (4.0) | 91 (3.3) | 659 (3.9) | 567 (3.9) |
| Lower respiratory disease | 2097 (3.3) | 784 (2.4) | 1313 (4.3) | 310 (2.6) | 583 (4.6) | 109 (2.7) | 169 (6.0) | 365 (2.2) | 561 (3.8) |
| Open wounds | 2013 (3.2) | 966 (2.9) | 1047 (3.5) | 313 (2.6) | 309 (2.4) | 108 (2.7) | 107 (3.8) | 545 (3.2) | 631 (4.3) |
| Suicide and self-inflicted injuries | 1558 (2.5) | 738 (2.2) | 820 (2.7) | 274 (2.3) | 304 (2.4) | 103 (2.6) | 75 (2.7) | 361 (2.1) | 441 (3.0) |
| Superficial injuries | 1283 (2.0) | 686 (2.1) | 597 (2.0) | 207 (1.7) | 218 (1.7) | 85 (2.1) | 41 (1.5) | 394 (2.3) | 338 (2.3) |
| Syncope & Collapse | 672 (1.1) | 353 (1.1) | 319 (1.1) | 138 (1.1) | 147 (1.2) | 44 (1.1) | 21 (0.8) | 171 (1.0) | 151 (1.0) |
| Palpitations and tachycardia | 559 (0.9) | 243 (0.7) | 316 (1.0) | 91 (0.8) | 133 (1.0) | 37 (0.9) | 27 (1.0) | 115 (0.7) | 156 (1.1) |
| Non-Emergent; Preventable/Avoidable; Primary Care Treatable | |||||||||
| Abdominal pain | 3483 (5.5) | 1641 (5.0) | 1842 (6.1) | 603 (5.0) | 693 (5.4) | 206 (5.1) | 126 (4.5) | 832 (4.9) | 1023 (7.0) |
| Fluid and electrolyte disorders | 2227 (3.5) | 1297 (3.9) | 930 (3.1) | 383 (3.2) | 441 (3.5) | 162 (4.0) | 115 (4.1) | 752 (4.5) | 374 (2.5) |
| Headaches (including migraines) | 2020 (3.2) | 1118 (3.4) | 902 (3.0) | 395 (3.3) | 372 (2.9) | 132 (3.3) | 79 (2.8) | 591 (3.5) | 451 (3.1) |
| Spondylosis; intervertebral disc disorders; other back problems | 2020 (3.2) | 1086 (3.3) | 934 (3.1) | 384 (3.2) | 373 (2.9) | 124 (3.1) | 80 (2.9) | 578 (3.4) | 481 (3.3) |
| Nausea & Vomiting | 1018 (1.6) | 577 (1.8) | 441 (1.5) | 193 (1.6) | 195 (1.5) | 81 (2.0) | 28 (1.0) | 303 (1.8) | 218 (1.5) |
| Hypertension | 712 (1.1) | 461 (1.4) | 251 (0.8) | 226 (1.9) | 117 (0.9) | 47 (1.2) | 33 (1.2) | 188 (1.1) | 101 (0.7) |
| Mood and personality disorders | 711 (1.1) | 431 (1.3) | 280 (0.9) | 148 (1.2) | 139 (1.1) | 41 (1.0) | 34 (1.2) | 242 (1.4) | 107 (0.7) |
| Diabetes | 509 (0.8) | 300 (0.9) | 209 (0.7) | 131 (1.1) | 109 (0.9) | 31 (0.8) | 19 (0.7) | 138 (0.8) | 81 (0.6) |
| Covid-19 | 305 (0.5) | – | 305 (1.0) | – | – | – | 51 (1.8) | – | 254 (1.7) |
| Number of inpatient ED visits | 16,651 | 8562 | 8089 | 3159 | 3080 | 1086 | 765 | 4317 | 4244 |
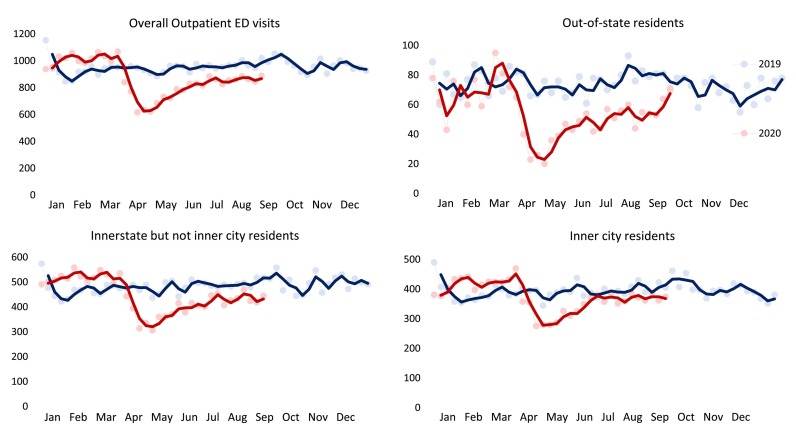
Fig. 1.
Trends in overall weekly outpatient ED visits and by area of residence from January 1, 2019 to August 31, 2020.
In the first trimester of 2020, weekly volumes of outpatient ED visits were higher in 2020 than in 2019 (+6.0%), though weekly visit volume decreased sharply beginning the last week of March (week 13 of 2020) and flattened in April 2020 (−30.4% overall and −32.8% in the third week compared to the same period in 2019) (Table 1, Fig. 1). Outpatient ED visits bounced back beginning in May, but weekly visits in the May to August period were still lower compared to 2019 (−12.8%). In terms of patient's place of residence, visits by out-of-state patients dropped most sharply in March through May (−66.5% in April 2020 compared to 2019) and were still around 30% below the weekly trends observed in 2019 from June to August 2020. Inner city and in-state residents consistently visited the ED, as weekly visits were only trending slightly lower compared to 2019.
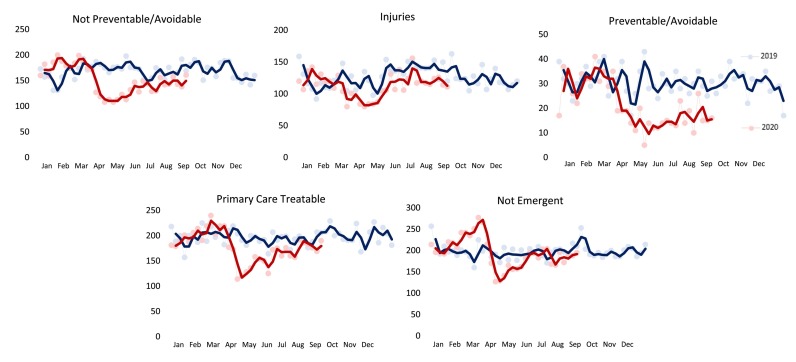
In terms of outpatient ED visits classified in the five NYU algorithm types, those visits classified as preventable or avoidable exhibited the largest decline (−48.2%) in April 2020 compared to the trend in 2019 (Table 1, Fig. 2 ). Primary care treatable and not preventable/avoidable outpatient ED visits were roughly 35% to 40% lower in April 2020 compared to the April 2019. Non-emergent visits drastically increased between February and March 2020 (+34.8% from week 7 to 11 of 2020 compared to the same weeks in 2019) and then dropped sharply in April. During May through August 2020 all visit types increased, except preventable/avoidable visits. By the end of August 2020, overall weekly visit numbers were generally only 11.3% lower compared to August 2019.
Fig. 2.
Trends in weekly outpatient ED visits by medical urgency classified by the NYU ED algorithm from January 1, 2019 to August 31, 2020.
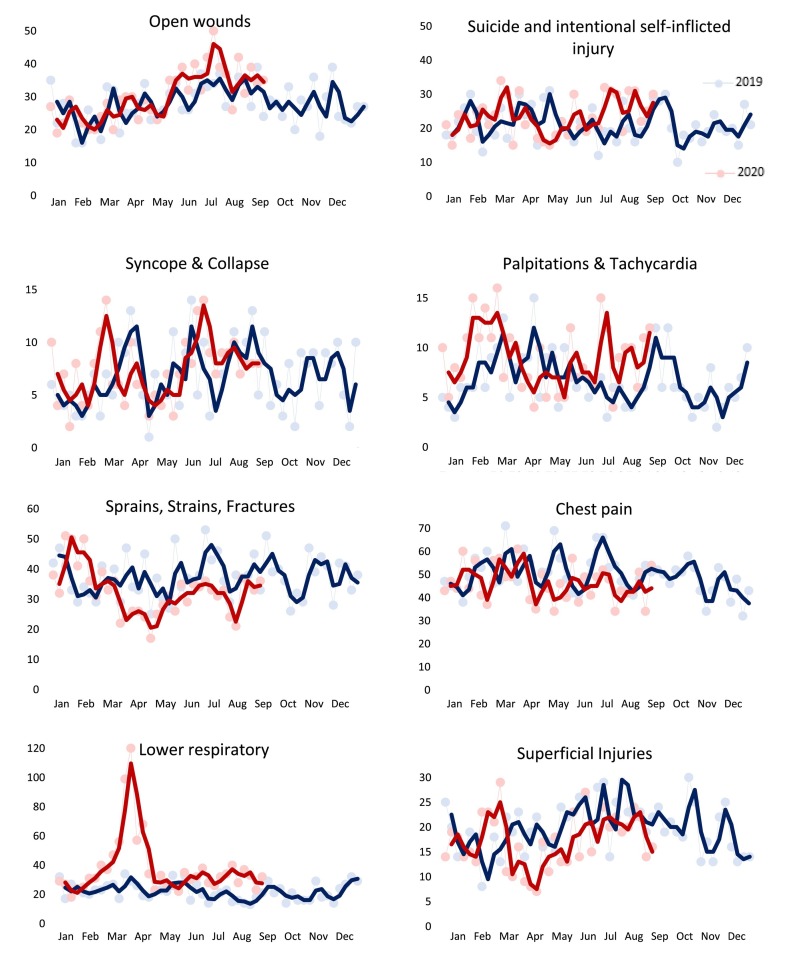
Fig. 3 displays trends for eight clinical categories that can be characterized as emergent. Small changes in visits occurred before, during, and after the first COVID-19 case on March 6 in Utah for most of the clinical categories. Outpatient visits related to sprains, strains, and fractures (−23.3%) and superficial injuries (−33.3%) declined from mid-March to the end of April compared to the same period in 2019 but displayed an upward trend after May. Only outpatient ED visits for lower respiratory diseases increased substantially in February and March (+135.5%), with a 400.0% increase in the last week of March compared to 2019 and remained consistently higher (+67.5%) in all of 2020 compared to 2019. We also observed 305 outpatient ED encounters for patients diagnosed with COVID-19.
Fig. 3.
Trends in weekly outpatient ED visits by medically urgent conditions from January 1, 2019 to August 31, 2020.
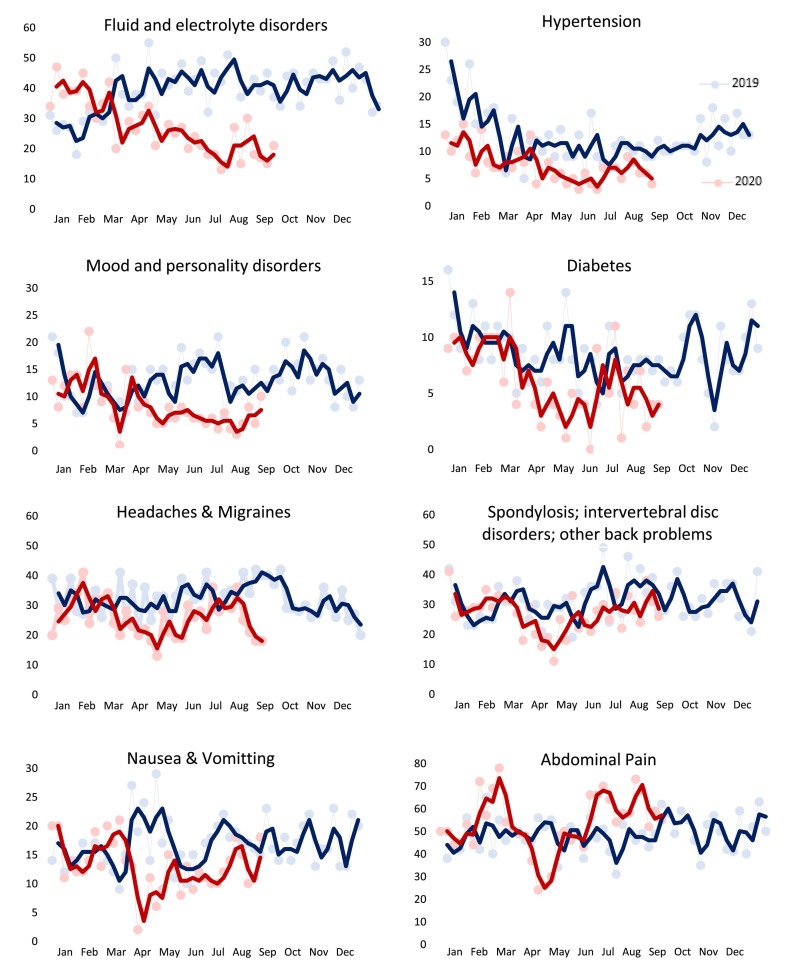
Among the less-urgent clinical categories displayed in Fig. 4 , outpatient ED visits for fluid and electrolyte disorders, hypertension, diabetes and mood and personality disorders decreased the most after March 2020 and continued to be below 2019 volumes through August 2020. A reduction in outpatient visits for spondylosis, intervertebral disc and back problems (−27.0%), nausea and vomiting (−42.2%), and headaches and migraines (−32.5%) persisted between April and May 2020 relative to the same period in 2019. One outlier were abdominal pain conditions, which were much higher in January through March 2020 (+19.0%), strongly declined between March and April 2020 (−44.0%) and increased in June 2020 (+56.4%) to levels far above the 2019 visit counts.
Fig. 4.
Trends in weekly outpatient ED visits by less medically urgent conditions from January 1, 2019 to August 31, 2020.
Finally, in terms of inpatient visits coming from the ED, 8562 and 8089 visits occurred from January to August in 2019 and 2020 respectively, which corresponds to a modest 5.5% decline. The decline was driven by a 29.6% decrease in April 2020 compared to April 2019, while the pre- and post-directive study period volumes remained similar between 2019 and 2020 (Table 1).
4. Discussion
The results indicate that outpatient ED visits in the emergency department of a large, academic, urban hospital system decreased in 2020 compared to 2019 and that the decline was driven by both emergent and non-emergent ED visits. Upon further separating outpatient ED visits into 8 urgent and 8 non-urgent categories, we found that urgent lower respiratory conditions increased 6-fold in April 2020, while other non-urgent conditions decreased in volume. Although the overall volume continued to be lower in August 2020 compared to August 2019 (−11%), outpatient ED visits exhibited an increasing trend beginning in May that peaked in July 2020.
Our results are similar in magnitude to those in a recent report on outpatient visits, which found a decline of almost 60% in March and April and a subsequent increase in visits through June [14]. The sharp decline in mid-March through April can be partially explained by patients' responding to intensive communication and outreach efforts and avoiding the risks of contracting COVID-19, shutdowns, and the stay at home directive in the state of Utah from March 27 through the first week of May. Reduced mobility of residents might further explain the large declines in ED visits from out-of-state residents and reductions in visits for many medical conditions that require urgent care, but commonly occur during outdoor activities (such as sprains, strains, fractures, and superficial injuries). Uncertainty and concerns about the risk of contracting the virus may have also led patients to postpone or forego care, particularly for conditions that are less medically urgent [3]. In contrast, visits for lower respiratory diseases were consistently higher beginning in early March of 2020.
Despite the fact that outpatient visits for many urgent conditions remained relatively stable during the pandemic, similar to previous work, we found large declines in overall inpatient ED visits in April 2020 compared to April 2019 and declines in outpatient ED visits classified as not preventable/avoidable [8,12]. These findings raise concerns about the short- and long-term patient health outcomes, particularly for individuals with acute conditions such as stroke and myocardial infarction, which require immediate hospital treatment. However, the underlying reasons for the decrease in not preventable/avoidable ED visits might be completely different relative to less urgent outpatient visits, so we note that inpatient ED visits require further investigation in the future.
Our conservative estimates suggest that more than 40% of all ED visits in 2020 were classified as non-urgent, consistent with national estimates and the existing ED literature [[4], [5], [6]]. In particular, the eight clinical conditions that fall within the non-emergent, preventable or primary care treatable categories accounted for almost half of the overall decrease in ED visits volume in 2020. This implies that patients are often able to evaluate the medical urgency of their condition [19,20]. However, for many patients ED may be the only option for care [20].
Of particular note is the relative steady trend in volume after May 2020, though lower compared to the 2019 period, of mood and personality disorders visits. This finding could be related to the rapid uptake, expansion and reimbursement of telemedicine services during the COVID-19 pandemic, which commonly serve patients with mental health conditions [[21], [22], [23]]. While we cannot establish a definitive assessment on whether patients avoided emergency care for less urgent conditions, including mental health, or substituted ED care with other care settings, such as primary care or telemedicine, the results highlight the potential to divert large levels of avoidable ED visits to other care settings. This is especially important as the second wave of COVID-19 in Winter may be exacerbated by the flu season.
The ongoing pandemic offers critical insight into individuals' care seeking behavior and the opportunity to rapidly redesign emergency care delivery [24]. Policymakers and providers should emphasize interventions and efforts to enhance primary care capacity, expand health insurance coverage, and extend telemedicine services to provide timely access to healthcare while simultaneously intensifying patient triage in the ED, and improve post-discharge care coordination [2,3,25]. Health authorities should also reach out to communities with educational material, resources and guidance to aid the determination of the appropriate location for care, since forgoing or delaying necessary care during the pandemic raises concerns about long-term adverse health outcomes particularly for high-risk and vulnerable individuals, while simultaneously causing staggering losses and financial hardships on hospitals.
4.1. Limitations
Our study is not without limitations. First, we used data from one emergency department and thus our findings are of limited external validity. In addition, despite the changes in ED visits, the use of emergency department data does not enable us to determine whether patients visited other healthcare facilities or went completely untreated. We also note that the use of the NYU ED algorithm with dichotomous indicators underestimates the prevalence of clinical conditions based on medical urgency, although we were able to classify around 80% of all ED visits.
5. Conclusion
In 2020, outpatient ED visits declined in a large, academic, urban hospital system in Utah from mid-March to April, particularly for non-urgent medical conditions. Visit volume increased after May 2020, highlighting the need for rapid and tailored interventions to raise patients' awareness on other outlets for non-urgent care as hospital systems remain focused on caring for large volumes of COVID-19 patients.
Author contributions
Study concept: TVG. Study design: TVG, JB, BU. Data acquisition: JB. Data analyses: TVG, JB, BU. Interpretation of the data: TVG, JB, DB, MJM, HA, BU. Drafting and review of the manuscript: TVG, JB, DB, MJM, HA, BU.
Funding
None.
Declaration of Competing Interest
All authors report not conflict of interest.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2020.12.009.
Appendix A. Supplementary data
Suppelementary material 1
Suppelementary material 2
References
- 1.Fuchs V. Healthcare policy after the COVID-19 pandemic. JAMA. 2020;324(3):233–234. doi: 10.1001/jama.2020.10777. [DOI] [PubMed] [Google Scholar]
- 2.Jeffery M.M., D’Onofrio G., Paek H. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the CoViD-19 pandemic in the US. JAMA Intern Med. 2020 Oct 1;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong L.E., Hawkins J.E., Langness S. NEJM Catalyst Innovations in Care Delivery. 2020 May 14. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. [DOI] [Google Scholar]
- 4.Uscher-Pines L., Pines J., Kellermann A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 5.Durand A.C., Gentile S., Devictor B. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med. 2011 Mar 1;29(3):333–345. doi: 10.1016/j.ajem.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Giannouchos T.V., Washburn D.J., Kum H.C. Predictors of multiple emergency department utilization among frequent emergency department users in 3 states. Med Care. 2020 Feb 24;58(2):137–145. doi: 10.1097/MLR.0000000000001228. [DOI] [PubMed] [Google Scholar]
- 7.Brousseau D.C., Nimmer M.R., Yunk N.L. Nonurgent emergency-department care: analysis of parent and primary physician perspectives. Pediatrics. 2011 Feb 1;127(2):e375–e381. doi: 10.1542/peds.2010-1723. [DOI] [PubMed] [Google Scholar]
- 8.Baum A., Schwartz M.D. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartnett K.P., Kite-Powell A., DeVies J. Impact of the COVID-19 Pandemic on Emergency Department Visits — United States, January1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6923e1. 699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiFazio L.T., Curran T., Bilaniuk J.W. The impact of the COVID-19 pandemic on hospital admissions for trauma and acute care surgery. Am Surgeon. 2020 Aug;86(8):901–903. doi: 10.1177/0003134820939904. [DOI] [PubMed] [Google Scholar]
- 12.Birkmeyer J.D., Barnato A., Birkmeyer N. 2020 September 24. The Impact Of The COVID-19 Pandemic On Hospital Admissions In The United States. Health Aff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solomon M.D., McNulty E.J., Rana J.S. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 14.Mehrotra A., Chernew M., Linetsky D. The impact of the COVID-19 pandemic on outpatient visits: Changing patterns of care in the newest COVID-19 hot spots. New York (NY): Commonwealth Fund. https://www.commonwealthfund.org/publications/2020/aug/impact-covid-19-pandemic-outpatient-visits-changing-patterns-care-newest Available from:
- 15.Billings J., Parikh N., Mijanovich T. Emergency department use in New York City: a substitute for primary care? Issue Brief (Commonwealth Fund) 2000;(433):1–5. Nov 1. [PubMed] [Google Scholar]
- 16.Johnston K.J., Allen L., Melanson T.A., Pitts S.R. A “patch” to the NYU emergency department visit algorithm. Health Serv Res. 2017 Aug;52(4):1264–1276. doi: 10.1111/1475-6773.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ballard D.W., Price M., Fung V. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010 Jan;48(1) doi: 10.1097/MLR.0b013e3181bd49ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Healthcare Cost and Utilization Project (HCUP) HCUP Clinical Classifications Software (CCS) for ICD-10. Rockville, MD: Agency for Healthcare Research and Quality. 2006–2009. https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp Available from: [PubMed]
- 19.Lowthian J.A., Smith C., Stoelwinder J.U. Why older patients of lower clinical urgency choose to attend the emergency department. Intern Med J. 2013 Jan;43(1):59–65. doi: 10.1111/j.1445-5994.2012.02842.x. [DOI] [PubMed] [Google Scholar]
- 20.Northington W.E., Brice J.H., Zou B. Use of an emergency department by nonurgent patients. Am J Emerg Med. 2005 Mar 1;23(2):131–137. doi: 10.1016/j.ajem.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020 Apr 30;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 22.Verma S. Early impact of CMS expansion of medicare telehealth during COVID-19. Health Affairs Blog July. 2020 Jul;15:15. doi: 10.1377/hblog20200715.454789. [DOI] [Google Scholar]
- 23.Barnett M.L., Ray K.N., Souza J., Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018 Nov 27;320(20):2147–2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Metzl J.M., Maybank A., De Maio F. Responding to the COVID-19 pandemic: the need for a structurally competent health care system. JAMA. 2020;324(3):231–232. doi: 10.1001/jama.2020.9289. [DOI] [PubMed] [Google Scholar]
- 25.Shachar C., Engel J., Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323(23):2375–2376. doi: 10.1001/jama.2020.7943. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Suppelementary material 1
Suppelementary material 2