With great interest, we read the observational study by Lammers et al., in which hydroxychloroquine (HCQ) was associated with a 53% risk reduction of transfer to the ICU in patients hospitalised with COVID-19 (Lammers et al., 2020). Given the limited number of effective drugs available, these results are of utmost interest. We think additional requirements need to be met before drawing the conclusion that HCQ is beneficial.
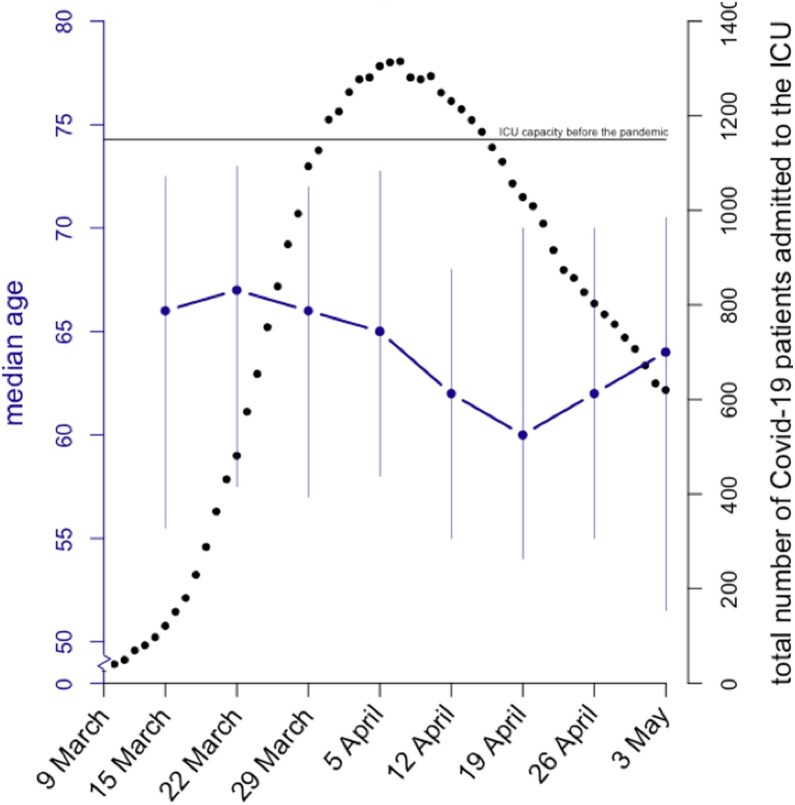
First, the median age of patients at ICU admission decreased during the first wave of COVID-19 in the Netherlands, as illustrated by Dutch data from the CAPACITY registry (Figure 1 ), indicating changing characteristics of the ICU population over time (Linschoten and Asselbergs, 2020). All analyses were stratified by ICU restriction. However, in the presence of ICU restriction, for medical reasons or patient preference, analyses on the outcome ‘transfer to ICU’ are limited to patients without ICU restriction, which is likely to have been a particularly selected group. Limiting the analyses to this subgroup might have a considerable impact on the generalisability of the results.
Figure 1.
Total number of patients with Covid-19 admitted to the ICU in the Netherlands (indicated by black dots) during the first wave between 9 March and 3 May 2020 (based on publicly available data from the NICE foundation (Nationale Intensive Care Evaluatie, 2020)). The median age of ICU admitted patients (indicated by blue dots, blue vertical bars interquartile ranges) declined during that period (based on data of 1182 patients from the Dutch CAPACITY registry (Linschoten and Asselbergs, 2020)). The blue dots indicate median age of the patients admitted to the ICU at that date and the six leading days. Prior to the COVID-19 pandemic, there were 1150 ICU beds in the Netherlands (indicated by the black line).
Second, there were strong regional differences in infection rates in the Netherlands. Consideration of ICU restriction policies could have happened earlier in the geographic regions with higher infection rates and thereby greater admission rates. These regional differences provoked the need to transfer patients to hospitals in other areas. Patients were transferred only if it was anticipated that there was a chance of recovery. It is therefore plausible that the exclusion of transferred patients in the study by Lammers et al. introduces a selection bias. Moreover, regional differences in infection rates might by chance also coincide with local protocols on the use of HCQ, chloroquine or no treatment.
Third, it is unclear whether the exposure was defined based on centre of admission or based on received treatment. Propensity score matching was used to balance covariates across levels of exposure, but no information on propensity score distribution nor trimming was provided. Moreover, if received treatment was the exposure, immortal time bias may play a role since median time to HCQ administration was one day. Consequently, those who were treated had a median survival of at least one day, whereas those untreated were at risk of ICU transfer directly from admission (Lévesque et al., 2010). Furthermore, follow-up was stopped once a patient was admitted to the ICU and ICU mortality ignored. Finally, discharge from hospital should also have been treated as a competing risk for mortality and for ICU admission (Andersen et al., 2012).
Before determining whether this study can contribute to establishing whether HCQ is useful in the treatment of COVID-19, these issues need to be addressed.
Conflict of interest
None.
Ethical approval
Not applicable.
Funding
ML is supported by the Alexandre Suerman Stipend of the University Medical Centre Utrecht. FWA is supported by University College London Hospitals National Institute for Health Research Biomedical Research and Cardiovasculair Onderzoek Nederland 2015-12 eDETECT.
References
- Andersen P.K., Geskus R.B., de Witte T., Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. 2012;41(3):861–870. doi: 10.1093/ije/dyr213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lammers A.J.J., Brohet R.M., Theunissen R.E.P., Koster C., Rood R., Verhagen D.W.M., et al. Early hydroxychloroquine but not chloroquine use reduces ICU admission in COVID-19 patients. Int J Infect Dis. 2020;101(December):283–289. doi: 10.1016/j.ijid.2020.09.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lévesque L.E., Hanley J.A., Kezouh A., Suissa S. Problem of immortal time bias in cohort studies: example using statins for preventing progression of diabetes. BMJ. 2010;340(March):b5087. doi: 10.1136/bmj.b5087. [DOI] [PubMed] [Google Scholar]
- Linschoten M., Asselbergs F.W. CAPACITY-COVID: a European Registry to determine the role of cardiovascular disease in the COVID-19 pandemic. Eur Heart J. 2020;41(May (19)):1795–1796. doi: 10.1093/eurheartj/ehaa280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nationale Intensive Care Evaluatie . 2020. Covid-19 infecties op de IC’s.https://stichting-nice.nl/covid-19-op-de-ic.jsp [Google Scholar]