Abstract
Context:
Lung cancer is frequent and mortal cancer. The predicting mortality may be helpful for cancer management.
Aim:
The purpose of the study was to evaluate the role of baseline C-reactive protein (CRP)/albumin ratio (CAR) in relation to hospital mortality, the setting of advanced stage non-small cell lung cancer (NSCLC).
Materials and Methods:
The present study is a retrospective analysis and included 77 adult patients with Stage IV NSCLC who were hospitalized for supportive care. All patients are divided into two groups as survivors and nonsurvivors. CAR on the admission was compared between groups. The correlation between CAR and the death time was investigated. The cutoff level of CAR was calculated, and patients with a high level were described in two groups.
Results:
For all participants, the mean age was 63.0 ± 9.9 years, and the median values of CRP and albumin levels were 15.3 mg/dl (1–51.5) and 5.7 g/dl (0.02–22.7), respectively. CAR was significantly lower in the survivor group. By receiver operation curve analysis, the cutoff levels of CRP and CAR were determined as 10.8 and 3.5, respectively. The odds ratio of mortality was 3.85 (1.49–9.94 95% confidence interval [CI], P = 0.006) for higher than cutoff levels of CAR. The odds ratio was 3.38 (1.32–8.65 95% CI, P = 0.01) for higher CRP levels. There was a significant but weak negative correlation between the time of death and both CRP and CAR in the nonsurvivor group (r = −0.46, P = 0.002; r = −0.48, P = 0.001, respectively).
Conclusion:
The present study showed that CAR was significantly increased in nonsurvivors. CAR may be a cheap, easy, and effective tool for predicting the death and its time of hospitalized NSCLC patients.
Keywords: Albumin, C-reactive protein, lung cancer, mortality
INTRODUCTION
Lung cancer is still a major death cause from cancer, and non-small cell lung cancer (NSCLC) accounts for approximately 85% of lung cancer patients.[1]
The predicting of mortality is crucial for disease management. Many studies have tried to find the best predictor for mortality. These predictors such as tumor stage, C-reactive protein (CRP)/albumin ratio (CAR), neutrophil/lymphocyte ratio (NLR), and platelet/lymphocyte ratio (PLR) were described by different trials.[2,3,4]
CRP reflects systemic inflammatory response. CRP/CAR was found as a prognostic factor for septic patients,[5] hepatocellular carcinomas,[6] esophageal squamous cell carcinoma,[7] and colorectal adenocarcinomas.[8] Systemic inflammation was associated with disease progression and worse outcomes according to findings of these trials.
The studies that were designed with CAR, often research for survival analysis. There is a lack of knowledge about the relation between CAR on the 1st day of admission and mortality in that hospitalization. The aim of this study was to evaluate the role of baseline CAR in relation to hospital mortality in the setting of advanced stage NSCLC.
MATERIALS AND METHODS
The retrospective study included 77 adult patients with Stage IV NSCLC that were admitted in Kırıkkale University, School of Medicine, Department of Medical Oncology, for supportive and palliative care between January 2018 and January 2019 were evaluated. Forty-one patients died, and 36 patients discharged from the hospital. Discharged patients were defined as “Survivors;” and deceased patients were defined as “Nonsurvivors.” Medical records of laboratory parameters such as complete blood cell parameters, especially CRP and albumin levels, on the 1st day of hospitalization were noted. Neutrophil/lymphocyte and PLRs were calculated. The time of death after the admission was calculated as day. CAR was calculated by CRP/albumin formula. Between two groups, baseline characteristics and CAR were compared. The correlation between the day of death after admission and CAR was evaluated. The cutoff levels of CAR were calculated, and the risk of mortality was tried to determine.
Statistical analysis
For all statistical analysis, IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. (Armonk, NY: IBM Corp.) was used. Normally distributed values were given as mean ± standard deviation, whereas abnormally distributed values were given as median (minimum–maximum). The Mann–Whitney U-test was performed for two group comparisons. The receiver operation curve (ROC) analysis was used for detecting a cutoff level of significant values. The Fisher's exact test was used, and the odds ratio was calculated according to cutoff levels between the two groups. Spearman's analysis was used for correlations. P < 0.05 was considered statistically significant.
Ethical consideration
The approval has been obtained from the Ethical Committee, Kırıkkale University.
RESULTS
There were 11 female and 66 male patients. For all participants, the mean age was 63.0 ± 9.9 years, and the median value of CRP and albumin levels was 15.3 mg/dl (1–51.5) and 5.7 g/dl (0.02–22.7), respectively. The age, sex, Charlson comorbidity scores, NLR, and PLR were similar by group comparisons. CAR was significantly lower in the survivor group [Table 1]. By ROC analysis, the cutoff level of CAR was determined as 3.5, and 10.8 for CRP (area under the curve: 0.75 and 0.73, respectively). The odds ratio of mortality was 3.85 (1.49–9.94 95% confidence interval [CI], P = 0.006) for higher than cutoff levels of CAR [Table 2]. The odds ratio was 3.38 (1.32–8.65 95% CI, P = 0.01) for higher CRP levels [Table 3]. There was a significant but weak negative correlation between the time of death and both CRP and CAR in the nonsurvivor group (r = −0.46, P = 0.002; r = −0.48, P = 0.001 respectively) [Figures 1 and 2].
Table 1.
Patient characteristics and laboratory values by group comparisons
| Survivor (n=36) | Nonsurvivor (n=41) | P | |
|---|---|---|---|
| Age, year | 62.8±9.9 | 63.5±10.0 | 0.71 |
| Female/male sex (n) | 4/32 | 7/34 | 0.52 |
| Diagnosis | |||
| Squamous cell carcinoma (n) | 20 | 22 | 0.94 |
| Adenocarcinoma (n) | 12 | 15 | |
| Others (n) | 4 | 4 | |
| Charlson comorbidity index | 8 (6-12) | 8 (6-11) | 0.90 |
| Time of death after admission, day | NA | 6 (1-30) | |
| CRP, mg/dl | 6.2 (0.1-39.7) | 16.1 (1.9-51.5) | <0.001 |
| Albumin, g/dl | 3.3 (1.9-4.3) | 2.8 (1.8-4.1) | <0.001 |
| CRP/albumin ratio | 2.4 (0.02-1.4) | 7 (0.36-22.7) | <0.001 |
| Neutrophil/lymphocyte ratio | 6.7 (0.3-38.4) | 10.3 (0.3-65.4) | 0.10 |
| PLR | 229 (15.00-697.4) | 234.4 (2.50-5215.80) | 0.36 |
CRP: C-reactive protein, NA: Not available, PLR: Platelet/lymphocyte ratio
Table 2.
The patient distribution according to the cutoff level
| Nonsurvivor (n) | Survivor (n) | |
|---|---|---|
| Patients with CAR ≥3.5 | 27 | 12 |
| Patients with CAR <3.5 | 14 | 24 |
CAR: C-albumin ratio
Table 3.
The patient distribution according to the cutoff level
| Survivor (n) | Nonsurvivor (n) | |
|---|---|---|
| Patient with CRP ≥10.8 | 19 | 8 |
| Patient with CRP <10.8 | 11 | 29 |
CRP: C-reactive protein
Figure 1.
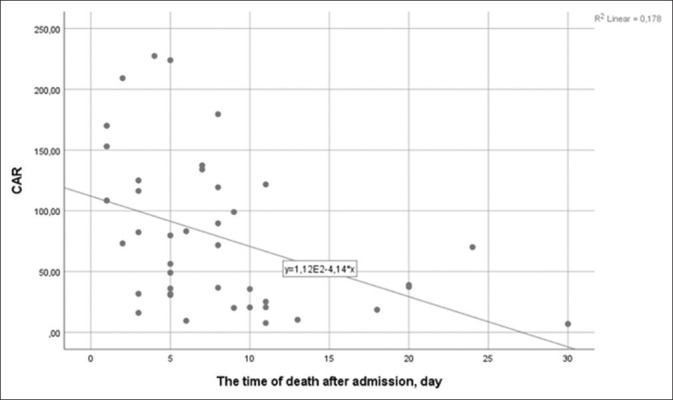
The time of death and C-reactive protein/albumin ratio
Figure 2.
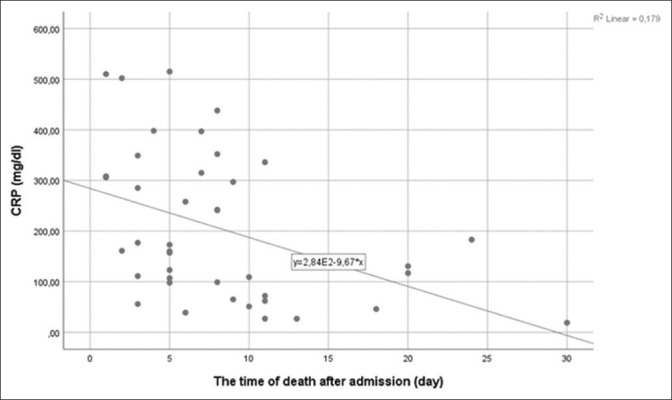
The time of death and C-reactive protein
DISCUSSION
The present study showed that both CRP and CAR were higher in the nonsurvivors from NSCLC, and increased CRP might be related to early mortality. These results may reflect which systemic inflammation can be more serious in the deceased patients, and serious inflammation may affect survival and death time. CAR is easily obtained from serum; it is cheap and frequent performing test. CAR may be predictive for mortality of advanced stage NSCLC patients. Furthermore, CAR may be more predictive than CRP for mortality.
Our study may be the first study that compares CAR on the 1st day of hospitalization between survivor and nonsurvivor groups of NSCLC inpatients. We have not encountered any trial with a similar design by literature review.
Chronic systemic inflammation plays a key role in tumor progression and carcinogenesis.[9] Recent studies showed that CRP and albumin levels had a relationship with inflammatory markers such as interleukin (IL)-6.[10,11] Increased CRP levels could affect tumor growth and worsen cancer. Inflammatory cytokines such as IL-6 can induce the proliferation of breast cancer and colon cancer cells.[12,13] Furthermore, inflammation could induce affecting genomic destabilization, promoting proliferative signaling, invasion, and metastasis; and changing responses to chemotherapeutic agents. All of these factors may cause poorer prognosis.[14,15,16]
The CAR may reflect not only inflammatory conditions but also the nutritional status of cancer patients. Both malnutrition may affect CRP and albumin levels. Inflammation and nutrition relations had been demonstrated by many studies. It was demonstrated which the nutritional supports could decrease the CAR, reduce inflammation, and improve immune status.[17,18,19] Therefore, the CAR could be used to evaluate nutritional status. Moreover, perhaps, the hospital mortality of NSCLC patients may be related to both inflammation and malnutrition.
The CAR has been investigated for survival analysis. Zhang et al.[20] showed that CAR can predict long-term disease progression and death in patients with operable NSCLC independently. Investigators have discussed this condition with inflammation and malnutrition mechanisms too. In this study, NLR has found as predictable for disease outcomes. They thought that increasing of neutrophils and decreasing of lymphocytes may cause cytokine activation, restrain lymphocyte associate killing. Furthermore, our study design was different, but NLR was similar in study groups.
Ni et al.[21] compared prognostic factors such as Glasgow prognostic score, NLR, PLR, and CAR in advanced NSCLC patients. They have found that CAR may be a better prognostic factor than the other inflammatory markers. They discussed the mechanism of adverse outcomes about CAR that was unclear. However, they thought it could be related to the IL-6/JAK-STAT signaling pathway.
Koh and Lee[22] studied the prognostic impact of CAR on the overall survival of patients with advanced NSCLC receiving palliative chemotherapy. CAR has found as an independent prognostic factor in patients, especially with advanced lung adenocarcinomas receiving platinum-based chemotherapy.
This study has several limitations. Once, retrospective design with the Turkish population and single-institution results are some of them. The sample size was small. Also, CRP and albumin can be influenced by numerous factors such as infections, nutrition, and diabetes. The other inflammatory markers could not be researched.
CONCLUSION
The present study showed that CRP and CAR were significantly increased in deceased patients by comparing survivors. CAR may be slightly more predictive than CRP. CAR may be a cheap, easy, and effective tool for predicting the death of hospitalized NSCLC patients. Further larger investigations are needed to clarify for explaining the role of inflammation on cancer mortality and time of death.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6:149–63. doi: 10.2217/fon.09.136. [DOI] [PubMed] [Google Scholar]
- 3.Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Fushiya N, et al. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer. 2012;107:988–93. doi: 10.1038/bjc.2012.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ikeguchi M, Urushibara S, Shimoda R, Yamamoto M, Maeta Y, Ashida K. Inflammation-based prognostic scores and nutritional prognostic index in patients with locally-advanced unresectable colorectal cancer. World J Surg Oncol. 2014;12:210. doi: 10.1186/1477-7819-12-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ranzani OT, Zampieri FG, Forte DN, Azevedo LC, Park M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013;8:e59321. doi: 10.1371/journal.pone.0059321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22:803–10. doi: 10.1245/s10434-014-4048-0. [DOI] [PubMed] [Google Scholar]
- 7.Zhao Q, Chen S, Feng JF. A novel inflammation-based prognostic index for patients with esophageal squamous cell carcinoma: Neutrophil lymphocyte ratio/albumin ratio. Oncotarget. 2017;8:103535–42. doi: 10.18632/oncotarget.21989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol. 2016;23:900–7. doi: 10.1245/s10434-015-4948-7. [DOI] [PubMed] [Google Scholar]
- 9.Hanahan D, Weinberg RA. Hallmarks of cancer: The next generation. Cell. 2011;144:646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 10.Cehreli R, Yavuzsen T, Ates H, Akman T, Ellidokuz H, Oztop I. Can inflammatory and nutritional serum markers predict chemotherapy outcomes and survival in advanced stage nonsmall cell lung cancer patients? Biomed Res Int. 2019;2019:1648072. doi: 10.1155/2019/1648072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou T, Zhan J, Hong S, Hu Z, Fang W, Qin T, et al. Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep. 2015;5:10481. doi: 10.1038/srep10481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zacarias-Fluck MF, Morancho B, Vicario R, Luque Garcia A, Escorihuela M, Villanueva J, et al. Effect of cellular senescence on the growth of HER2-positive breast cancers. J Natl Cancer Inst. 2015;107:djv020. doi: 10.1093/jnci/djv020. [DOI] [PubMed] [Google Scholar]
- 13.Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009;15:103–13. doi: 10.1016/j.ccr.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–44. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 15.Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15:e493–503. doi: 10.1016/S1470-2045(14)70263-3. [DOI] [PubMed] [Google Scholar]
- 16.Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: Crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13:759–71. doi: 10.1038/nrc3611. [DOI] [PubMed] [Google Scholar]
- 17.Alberici Pastore C, Paiva Orlandi S, González MC. Association between an inflammatory-nutritional index and nutritional status in cancer patients. Nutr Hosp. 2013;28:188–93. doi: 10.3305/nh.2013.28.1.6167. [DOI] [PubMed] [Google Scholar]
- 18.de Silva JA, de Trindade EB, de Fabre ME, Menegotto VM, Gevaerd S, da Buss ZS, et al. Fish oil supplement alters markers of inflammatory and nutritional status in colorectal cancer patients. Nutr Cancer. 2012;64:267–73. doi: 10.1080/01635581.2012.643133. [DOI] [PubMed] [Google Scholar]
- 19.Long H, Yang H, Lin Y, Situ D, Liu W. Fish oil-supplemented parenteral nutrition in patients following esophageal cancer surgery: Effect on inflammation and immune function. Nutr Cancer. 2013;65:71–5. doi: 10.1080/01635581.2013.741761. [DOI] [PubMed] [Google Scholar]
- 20.Zhang F, Ying L, Jin J, Chen K, Zhang N. The C-reactive protein/albumin ratio predicts long-term outcomes of patients with operable non-small cell lung cancer. Oncotarget. 2017;8:8835–42. doi: 10.18632/oncotarget.13053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ni XF, Wu J, Ji M, Shao YJ, Xu B, Jiang JT, et al. Effect of C-reactive protein/albumin ratio on prognosis in advanced non–small-cell lung cancer. Asia Pac J Clin Oncol. 2018;14:402–9. doi: 10.1111/ajco.13055. [DOI] [PubMed] [Google Scholar]
- 22.Koh YW, Lee HW. Prognostic impact of C-reactive protein/albumin ratio on the overall survival of patients with advanced nonsmall cell lung cancers receiving palliative chemotherapy. Medicine (Baltimore) 2017;96:E6848. doi: 10.1097/MD.0000000000006848. [DOI] [PMC free article] [PubMed] [Google Scholar]


