Abstract
Post-mortem swabs for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) RNA detection have been recommended by several Scientific Committees and Institutions as a standard procedure for post-mortem assessment of potential Coronavirus Disease-19 (COVID-19) related deaths. To date there is no data about the SARS-CoV-2 RNA detectability period in human bodies after death. The present case documents the persistence of SARS-CoV-2 RNA in the upper respiratory tract 35-days after death. Post-mortem swabs could be used as a valuable tool in preventive evaluation of the risks-benefits ratio associated with autopsy execution. SARS-CoV-2 RNA post-mortem detection could have a key diagnostic role in deaths lacking medical assistance, unattended deaths, and patients with multiple comorbidities.
Based on the present report, staged post-mortem swabs should be performed even after a long post-mortem interval.
Keywords: SARS-CoV-2, COVID-19, Post-mortem swab, Post-mortem diagnosis, Biosafety, Autopsy
1. Introduction
Since December 2019 until today, the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) pandemic has caused more than 1,300,000 deaths worldwide [1]. The diagnosis of acute infection is carried out in the vast majority of cases through the search of the viral ribonucleic acid (RNA) on respiratory specimens, primarily by means of the rhino- or oropharyngeal swabs.
In living people, respiratory droplets and interpersonal physical contacts are known to be the main routes of transmission, while conjunctival and bronchial epithelium are considered portals for infection [2]. However, human coronaviruses have been shown to persist on inanimate surfaces up to 9 days [3].
Generally, a large amount of viruses may remain in deceased people and be detected by polymerase-chain-reaction (PCR) amplification [4].
There is no evidence of correlation between amplifiable SARS-CoV-2 RNA detected in respiratory swabs and infectious risk. Till now, none of the alleged cases of Coronavirus Disease-19 (COVID-19) transmission from a corpse has been confirmed [5]. However, being impossible at present to exclude the risk of contagion from corpse to forensic pathologists, technicians, and mortuary workers, international guidelines stress the use of biosafety level (BSL) 3 protection standards in case of suspected or confirmed COVID 2019 cadavers examination [6].
We hereby report persistence of SARS-CoV-2 RNA in post-mortem rhino- and oropharyngeal swabs from a COVID 2019 35-days after death.
2. Case presentation
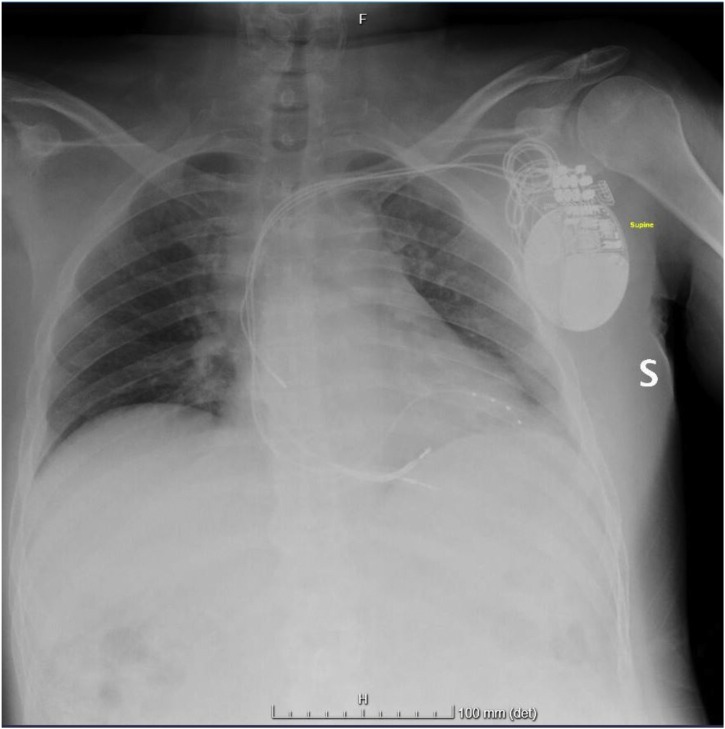
On 15th March 2020 a 60-year-old man, with an history of Obstructive Sleep Apnea Syndrome (OSAS) in former tobacco smoking, Steinert myotonic dystrophy, pace maker implantation for ischemic cardiomyopathy with left bundle branch block, and diabetes, was brought to the regional hospital of Aosta (Italy) after accidental fall at home. On admission, temperature was 37.5 °C and oxygen saturation 90%. Chest radiograph showed band shadows in lower left lobe (Fig. 1 ).
Fig. 1.
Chest Radiograph at Hospital admission.
Blood routine test showed leucocytopenia. Respiratory tract swabs were sent to laboratory. SARS-CoV-2 infection was confirmed by Reverse Transcriptase Polymerase-Chain-Reaction Real Time (RT PCR-RT) on 16th March 2020. The patient was therefore transferred to a COVID 2019 Unit and Non Invasive Mechanical Ventilation (NIMV) was started due to recurring desaturation crisis. Respiratory symptoms worsened during the night. Despite NIMV and vital support therapy, the patient died on 17th March 2020. SARS-CoV-2 pneumonia was reported as primary cause of death, while Steinert myotonic dystrophy, and ischemic cardiomyopathy were listed as contributory. His body was transported to the local crematorium and placed in a refrigerator (−4 °C), pending the wife’s authorization for cremation (required by the Italian Law).
Indeed, during the same time period, the patient wife had also been admitted in a COVID Unit of the same hospital with severe respiratory symptoms. After treatment with antiviral therapy, respiratory symptoms had improved. On April 13th, after two consecutive tests for SARS-CoV-2 RNA resulted negative, the woman had been transferred in a non-COVID unit. She therefore gave authorization for incineration of the husband cadaver. Due to local crematorium technical specifications, removal of pace maker device was required.
On April 22nd 2020, the corpse was extracted from refrigerator and, on the occasion of the removal of the pace maker by the medical examiner, rhino- and oropharyngeal swabs were carried out. The samples were immediately delivered to the laboratory and analyzed with RT PCR-RT according to WHO Protocol [7]. Results were available on the same day, confirming persistence of SARS-CoV-2 RNA.
3. Discussion
The present case highlights the persistence of SARS-CoV-2 RNA in the upper respiratory tract 35-days after death. This is the longest documented detection of SARS-CoV-2 RNA in respiratory specimens from cadaver.
Previous studies highlighted persistence of detectable SARS CoV-2 RNA even in decomposed corpses [8]. Neither the time elapsed between the death and the collection of the swabs nor the time elapsed before their analysis in the laboratory appear to affect the results of PCR-CR [9].
According to previous studies, refrigeration may prolong survival time of coronaviruses [3,10]. The Authors speculate that, in this case, lack of antiviral therapy during the hospitalization, along with refrigeration of the corpse, may have contributed to the lasting persistence of SARS-CoV-2 RNA.
Post-mortem swabs for SARS-CoV-2 RNA detection have been recommended by several Scientific Committees and Institutions, including Public Health England, as a standard for staged post mortem assessment of potential COVID-19-related deaths [6].
Current Italian forensic guidelines state that respiratory specimens should be collected shortly after death in suspected cases, preferably within 2-hs [11].
Based on the present report, staged post-mortem swabs should be performed even after a long post-mortem interval. SARS-CoV-2 RNA post-mortem detection could have a key role in deaths lacking medical assistance, unattended deaths, and patients with multiple comorbidities. In the latter, preexisting clinical conditions could have concealed COVID-19 clinical signs. Likewise, SARS-CoV-2 post-mortem amplification should also be carried out to identify undiagnosed COVID-19 related deaths in high risk groups such as medical workers, retirement homes residents, and law enforcement officers to trace ad isolate contacts.
Moreover, during SARS-CoV-2 pandemic, Countries adhering to Berlin Agreement could consider the results of post-mortem RT PCR-RT as part of the “laissez-passer for a corpse” needed for International Transportation [12].
Post-mortem swabs could be used as a valuable tool in preventive evaluation of the risks-benefits ratio associated with autopsy execution, in order to identify the cases in which autopsy can be recommended to determine the cause of death (i.e. negative result of upper respiratory tract swab and no history of suggestive symptoms) [13].
Considering the current lack of studies attesting the reliability of post-mortem SARS-CoV-2 RNA amplification, the implementation of effective BSL standards during cadaver manipulation, examination, and autopsy should be established including both the results of the test on respiratory specimens and clinical and radiological data obtained from medical records or from the history information reported by the kin, if available.
Nonetheless, a positive postmortem swab should not be per se considered diagnostic of death caused by SARS-CoV-2 infection. Conversely, autopsy could highlight signs of independent causes of death, discriminating patients with coexisting SARS-CoV-2 infection [8].
The value of SARS-CoV-2 RNA detection on post-mortem swabs is the subject of an ongoing preliminary study by the Authors of the present report.
References
- 1.WHO . 2020. World Health Organization. Coronavirus Disease Situation Report - 118. [Google Scholar]
- 2.Hui P.Y.K., et al. Tropism, replication competence, and innate immune responses of the coronavirus SARS-CoV-2 in human respiratory tract and conjunctiva: an analysis in ex-vivo and in-vitro cultures. Lancet Respir. Med. 2020;6(11 (May)):846–854. doi: 10.1016/S2213-2600(20)30193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kampf G., et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(March (3)):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nihan Z., et al. Investigation of viral respiratory tract infection agents by multiplex PCR method in autopsy cases: a five-year study. Mikrobiyoloji bülteni. 2019;53(April (2)):179–191. doi: 10.5578/mb.67960. [DOI] [PubMed] [Google Scholar]
- 5.Sriwijitalai W., Wiwanitkit V. COVID-19 in forensic medicine unit personnel: observation from Thailand. J. Forensic Leg. Med. 2020;72(April):101964. doi: 10.1016/j.jflm.2020.101964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanley B., et al. Autopsy in suspected COVID-19 cases. J. Clin. Pathol. 2020;73(5) doi: 10.1136/jclinpath-2020-206522. [DOI] [PubMed] [Google Scholar]
- 7.WHO . 2020. Diagnostic Detection of 2019-nCoV by Real-time RT-PCR. 17 January. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edler C., et al. Dying with SARS-CoV-2 infection—an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int. J. Legal Med. 2020;(04 June):1–10. doi: 10.1007/s00414-020-02317-w. Springer-Verlag GmbH Germany, part of Springer Nature 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dell’Aquila M., et al. Postmortem swabs in the severe acute respiratory syndrome coronavirus 2 pandemic: report on 12 complete clinical autopsy cases. Arch. Pathol. Lab. Med. 2020;144(November (11)):1298–1302. doi: 10.5858/arpa.2020-0362-SA. [DOI] [PubMed] [Google Scholar]
- 10.Mao D., Cheng Jianding, et al. Guide to forensic pathology practice for death cases related to coronavirus disease 2019 (COVID-19) (Trial draft) Forensic Sci. Res. 2020;5(April):1–7. doi: 10.1080/20961790.2020.1744400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fineschi V., et al. Management of the corpse with suspect, probable or confirmed COVID-19 respiratory infection – Italian interim recommendations for personnel potentially exposed to material from corpses, including body fluids, in morgue structures, during autopsy practice. Pathologica. 2020;26(March) doi: 10.32074/1591-951X-13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.League of Nations . 1937. No.4391. Arrangement International Concernant Le Transport Des Corps. Berlin: s.n., 10 February. [Google Scholar]
- 13.Sapino A., et al. The autopsy debate during the COVID-19 emergency: the Italian experience. Virchows Arch. 2020;29(April) doi: 10.1007/s00428-020-02828-2. [DOI] [PMC free article] [PubMed] [Google Scholar]