Introduction
Globally, low back pain is the leading cause of disability, and its burden is projected to increase with the aging population.1 It has been estimated that up to 80 percent of the population will have an episode of back pain in their lifetime.2 For most individuals, acute low back pain resolves relatively quickly, but for about 5 to 10 percent of the cases, acute low back pain transitions into chronic low back pain (cLBP), lasting more than 12 weeks.3,4 cLBP is associated with low quality of life, chronic stress, decreased productivity, and mood disorders such as major depression.5,6 cLBP affects all segments of the population; however, compared to non-Hispanic Whites, non-Hispanic African Americans (Blacks) experience more severe, and disabling cLBP.7–9 In addition, patients of low socioeconomic status are disproportionately affected by the disease burden of cLBP.10
Existing research supports a biopsychosocial model of pain, which considers other factors in addition to biological processes that may contribute to the etiology, experience, management, and outcomes of cLBP.11–14 These additional factors may include psychological, social, and/or environmental influences.10,13,14 For instance, in the context of cLBP, research has highlighted the importance of psychological factors such as depressive symptoms.14 Depression has been shown to be a reliable predictor of cLBP development, chronification, and related disabilities,12,15,16 and cLBP has been reported as a risk factor for depression.17
In thinking about depressive symptoms and racial differences in cLBP, it is critical to consider racial and ethnic differences in major depressive disorders. Compare to Blacks, White Americans have a higher lifetime prevalence of major depressive disorder.18,19 However, Black individuals and people of lower socioeconomic status are less likely to seek treatment, follow recommendations, and complete treatment regimens for depression. As a result, they tend to have more serious, prolonged, and disabling depression than Whites.20 Multiple studies have reported that among Black individuals, racial discrimination and perceived social status correlate with depression.21,22 Specifically, for among black adolescents higher perceived social status (i.e., position in the social hierarchy) is associated with an increased risk of 30-days, 12-month, and lifetime major depressive disorder.21
Others have found that an individual’s perception of his or her social status is independent of objective measures of SES, and predicts mental and physical health.23–26 Thus, it has been proposed that subjective measures of SES (e.g., perceived social status) and objective measures of SES (e.g., household income, educational attainment, and work status) are not interchangeable.26 Research further suggests that social status differs among racial/ethnic groups as well.26,27 In particular, there is a strong association between objective measures of SES and perceived social status among White individuals; but for Black individuals, objective measures of SES “do not necessarily influence their” perceived social status.26,28,29 Accordingly, an appreciation of racial differences in the experience of pain, which is essential for effective intervention, cannot be fully understood without consideration of SES.30
Although race/ethnicity, SES, and depressive symptoms have been examined in the context of pain, relatively minimal research has examined the potential interplay between these factors on cLBP outcomes. Thus, the purpose of this study was to examine the pathways by which self-identified race influences the relationship between subjective SES and cLBP outcomes. This study had two hypotheses. First, we hypothesized that race moderated the effect of perceived social status in predicting cLBP interference and severity. Second, we hypothesized that race moderated the relationship between perceived social status and depressive symptoms, which conditionally mediated the effect of perceived social status in predicting cLBP interference and severity.
Methods
Study Overview
This study is part of a more extensive ongoing investigation examining ethnic/racial differences in cLBP severity and disability (Examining Racial And SocioEconomic Disparities in cLBP; ERASED). The ERASED cLBP study incorporates a socioeconomic framework from which to consider differences in cLBP outcomes between Black and White adults, as well as the biopsychosocial variables that predict these differences. The participants described in the current analysis were recruited between November 2017 and June 2019 and have not previously been included in any published literature. The measures and procedures described below are limited to those involved in the current study. Study procedures were consistent with the research standards for cLBP proposed by the Research Task Force of the NIH Pain Consortium.31 All procedures were reviewed and approved by the Institutional Review Board at the University of Alabama at Birmingham (IRB-170119003) and carried out in accordance with guidelines for the ethical conduct of research.
Participants
Participants were recruited via flyers posted at the Pain Treatment Clinic within the University of Alabama at Birmingham (UAB), and the surrounding community. Participants were included in this study if they reported non-specific cLBP that had persisted for at least three consecutive months and was present on at least half the days in the past six months (4). Furthermore, participants were only included if they denied any type of surgery on the low back or trauma/accident within the past year. Low back pain had to be the primary pain complaint reported for all participants with cLBP. Participants were between the ages 19 to 85 years; able to read, write, and understand English; and self-identified as non-Hispanic Black/African American or non-Hispanic White/Caucasian. Informed consent for study participation was obtained from each participant before initiating study procedures.
Procedures
Initial screening and review of medical records.
All participants completed initial screening via telephone to determine eligibility for study inclusion. Sociodemographic and health data were also obtained during screening and included: sex, age, and ethnic/racial identity, as well as a brief health history. Review of medical records was subsequently completed for each potential participant to confirm cLBP diagnosis and corroborate self-reported brief health history, as well as document any other comorbid diagnoses and medications actively being prescribed.
Participants were excluded from participation for the following reasons: 1) cLBP attributable to other factors such as ankylosing spondylitis, infection, malignancy, compression fracture or other trauma; 2) Presence of systemic rheumatic conditions (e.g., rheumatoid arthritis, systemic lupus erythematosus, fibromyalgia); 3) Evidence of uncontrolled hypertension (i.e., SBP/DBP > 150/95), cardiovascular or peripheral arterial disease; 4) Poorly controlled diabetes (HbA1c > 7%); 5) Neurological disease (e.g., Parkinson’s, multiple sclerosis, epilepsy); 6) Serious psychiatric disorder requiring hospitalization within the past 12 months; 7) Pregnancy.
Laboratory sessions.
A flow diagram depicting matriculation through the study sessions is presented in Figure 1. Study participants completed two separate study sessions. During the first study session, participants completed measures of clinical pain severity and interference, perceived social status, and depressive symptoms. They also provided information about their socioeconomic status, including annual household income, occupational status, and educational attainment. Approximately one week following the first study session, participants returned to the laboratory and completed a second study session, which included additional measures of clinical pain severity and interference.
Figure 1.
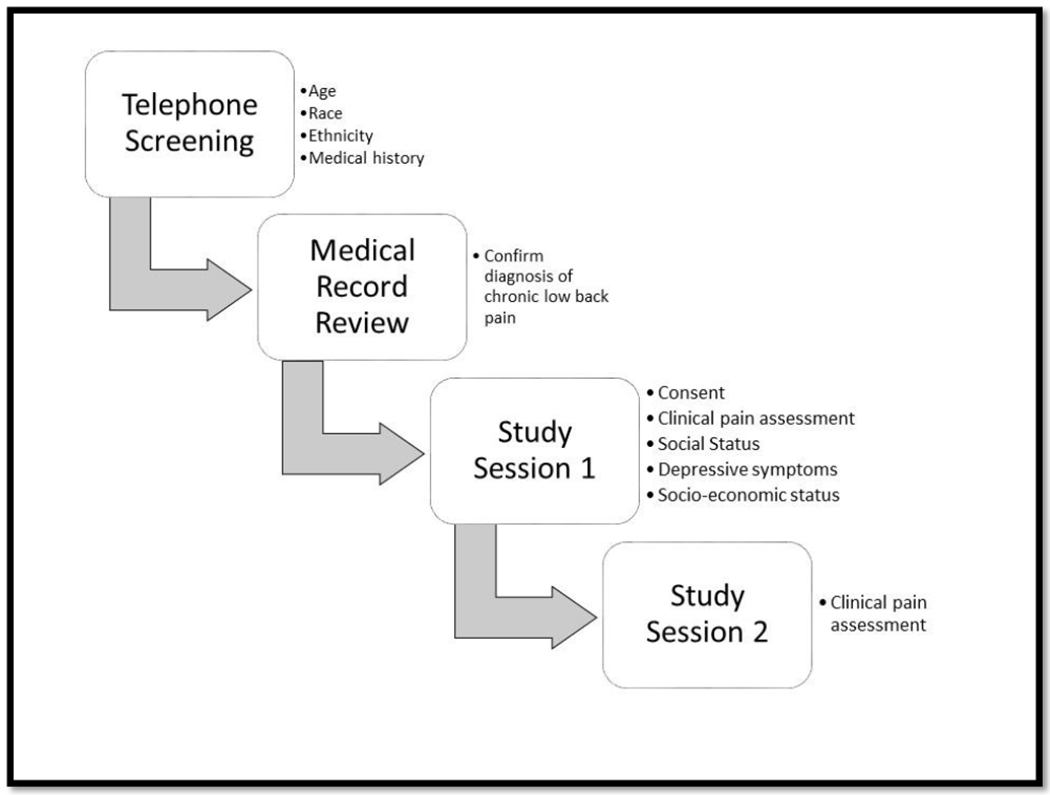
Flow diagram of the study protocol.
Notes: Session two was completed about one week after session one.
Given that participants were primarily recruited from a pain treatment clinic, many were actively prescribed daily analgesic medications, including opioids. Participants using daily opioids were not excluded as this could have undermined the generalizability of study results. Furthermore, they were not asked to withhold pain medications on the days of study participation. This is because temporary withdrawal from these medications could have affected pain perception. Instead, all medications currently prescribed for pain (e.g., opioids, NSAIDs, SSRIs, etc.) were recorded. Also, participants were asked to indicate whether they took any medications (prescription or over the counter) for pain management.
Measures
Ethnicity/Race/Objective SES.
Participants self-reported their ethnic and racial background using response options consistent with the United States census survey. All participants enrolled in the study identified their ethnic background as non-Hispanic and their racial background as either Black/African American or White/Caucasian. Participants self-reported their ethnicity and race during the initial telephone screening. During the first study session, participants self-reported their highest level of educational achievement, work status, and annual household income (money left over after taxes and other deductions).
The MacArthur Scale of Subjective Social Status.
The MacArthur scale is a commonly used measure of subjective social status that assesses an individual’s sense of social status across the socioeconomic status indicators.32 During the first study session, participants were given a drawing of the ladder with the following instructions:
“Think of this ladder as representing where people stand in the United States. At the top of the ladder are the people who are the best off- those who have the most money, the most education, and the most respected jobs. At the bottom are the people who are the worst off- who have the least money, least education, and the least respected jobs, or no job. The higher up you are on this ladder, the closer you are to the people at the very top; the lower you are, the closer you are to the people at the very bottom. Please place a large “X” on the rung of the ladder for where you think you stand at this time in your life, relative to other people in the United States.”
The ladder in the figure has 10 steps, and in the current study, the integer scores of social status range from 0 to 10 corresponding to the where participants placed the “X” on the ladder.
Center for Epidemiological Studies Depression Scale (CES-D).
The CES-D is one of the most commonly used measures of depressive symptoms; it assesses various aspects of depression including mood, guilt, worthlessness, helplessness, hopelessness, loss of appetite, sleep disturbance, and psychomotor retardation. The 20-item self-administered questionnaire is scored on a four-point scale (0 −3) with a possible score ranging from zero to 60, and higher scores reflecting more severe depressive symptoms. The CES-D was administered during the first study session, and before the completion of laboratory pain task. The internal consistency of the CES-D in this current study was good (α = 0.85).
Brief Pain Inventory (BPI) – Short Form.
The BPI is a self-administered questionnaire used to assess pain severity and the impact of pain on the participant’s daily activities (pain interference). To assess pain severity, participants are asked to rate their worst, least, average, and current pain intensity on a scale 0 (no pain) to 10 (pain as bad as you can imagine) in the past 24 hours. The average score on the four-items reflects pain severity in the past 24 hours. Participants also rate the impact of pain on general activity, mood, walking ability, normal work, relations with other people, sleep, and enjoyment of life during the past 24 hours, on a 10 point scale. Pain interference is determined by calculating the average of these items. Higher scores are indicative of greater pain severity and interference. The internal consistency of the BPI in this study was excellent (α = 0.94).
Data Analysis
Data were analyzed using IBM SPSS 24 statistical software. Before hypothesis testing, the distribution of variables was assessed and inspected for outliers. Chi-squared tests and Student’s t-test (or Mann Whitney U test) were used to assess group differences in demographic and clinical features of pain when variables were categorical or continuous, respectively. Given evidence that depressive symptoms, pain interference, pain severity, and perceived social status do not follow normal distributions (p < 0.05 in Kolmogorov-Smirnov and Shapiro-Wilk tests), Mann Whitney U tests and Spearman’s correlation were utilized for assessing relationships between variables of interest. Given no evidence of lack of normality in age distribution, student’s t-test was used to assess group differences. Also, work status, household income, and educational achievement were measured at the ordinal level.
Moderation analysis using the PROCESS plugin for SPSS (Model 1) was used to test for main effects of race, perceived social status, and their interaction on BPI outcomes (pain interference and pain severity).33 In a follow-up analysis, conditional PROCESS model 7 was computed to test the indirect effects of perceived social status (X) on pain outcomes (Y) through depressive symptoms (mediator). The age adjusted relationship between perceived social status and depressive symptoms was thought to depend on race; thus, race (W) was entered as a moderator in the model as recommended.34 95% bootstrapped confidence intervals were generated (with 5000 samples) to test for unconditional and conditional indirect effects. Also, an index of moderated mediation was estimated to test the association between the indirect effect of depressive symptoms and pain outcomes from bootstrapping 5,000 samples. Conceptually, bootstrapping is a non-parametric approach to effect-size estimation and hypothesis testing that makes no assumptions about the shape of the distribution of the variables within a given model (i.e., normal versus skewed).35 All tests were two-tailed with statistical significance at 0.05.
Results
Participant characteristics
The sample was comprised of 105 eligible participants with cLBP. Most of the study sample was female (59%), and African American (54.3%), with a mean age of 45.8 years (SD = 14.03). Demographic and study variables are summarized in Table 1. On average, women were younger (M = 42.37 years; SD = 13.67) than men (M = 50.6 years; SD = 2.02). This difference was statistically significant (t(101) = 3.05, p = 0.003). There was no significant race difference in age (p = 0.84), and no significant sex difference in pain severity (p = 0.33) and pain interference (p = 0.23)). Participants who self-identified as Blacks reported significantly greater pain severity and pain interference than Whites. There were no statistically significant racial differences in work status, educational achievement, and medication status (whether the participants took pain medications or not) (p > 0.05).
Table 1.
Characteristics of the Participants
| Total n = 105 | Blacks n = 57 | Whites n = 48 | p-valuea | |
|---|---|---|---|---|
| Sex n (%) | ||||
| Male | 43 (41) | 25 (43.9) | 18 (37.5) | 0.55 |
| Female | 62 (59) | 32 (56.1) | 30 (62.5) | |
| Age | 45.8 ± 14.03 | 45.6 ± 13.1 | 46.1 ± 15.5 | 0.84 |
| Education n (%) | ||||
| Partial high school | 7 (6.70) | 4 (7.02) | 3 (6.25) | 0.64 |
| High school graduate | 22 (21) | 14 (24.6) | 8 (16.7) | |
| Partial College | 31 (29.5) | 18 (31.6) | 13 (27.1) | |
| College graduate | 26 (24.8) | 11 (19.3) | 15 (31.3) | |
| Graduate/Professional training | 19 (18.1) | 10 (17.5) | 9 (18.7) | |
| Work Status n (%) | ||||
| Employed | 61 (58.7) | 34 (59.6) | 27 (57.4) | 0.12 |
| Unemployed looking | 8 (7.70) | 5 (8.77) | 3 (6.4) | |
| Retired, homemaker, not looking | 16 (15.4) | 5 (8.77) | 11 (23.4) | |
| Student | 1 (0.95) | 0 | 1 (2.08) | |
| Disabled | 18 (17.3) | 13 (22.8) | 5 (10.6) | |
| Perceived Social status | 5.17 ± 2.04 | 5.0 ± 1.94 | 5.38 ± 2.15 | 0.35 |
| Household Income n (%) | ||||
| $ 0 to 24,999 | 40 (39.6) | 24 (44.4) | 16 (34) | 0.08 |
| $ 25,000 to 49,999 | 19 (18.8) | 12 (22.2) | 7 (14.9) | |
| $ 50,000 to 74,999 | 18 (17.8) | 11 (20.4) | 7 (14.9) | |
| $ 75,555 to 99,999 | 10 (9.9) | 4 (7.4) | 6 (12.8) | |
| $ 100,000 and greater | 14 (13.9) | 3 (5.6) | 11 (23.4) | |
| Medication Status | ||||
| No | 30 (28.8) | 20 (35.7) | 10 (20.8) | 0.09 |
| Yes | 74 (71.2) | 36 (64.3) | 38 (79.2) | |
| CES-D | 17.96 ± 11.48 | 17.73 ± 10 | 18.23 ± 13.12 | 0.73 |
| Pain Interference | 3.59 ± 2.49 | 4.12 ± 2.65 | 2.95 ± 2.13 | 0.02 |
| Pain Severity | 4.87 ± 2.28 | 5.57 ± 2.27 | 3.99 ± 1.99 | <0.001 |
Notes: Values expressed as mean ± SD or n (%). CES-D = Center for Epidemiologic Studies Depression Scale; BPI-I = Brief pain inventory-pain interference; BPI-S = Brief pain inventory- pain severity;
p-value pertains to tests for the difference between Blacks and White groups
Bivariate Correlations
Table 2 summarizes the bivariate relationship between study variables. As expected, there is a strong positive relationship between pain severity and pain interference. Both pain severity and pain interference were moderately positively correlated with depression, but modestly negatively correlated with perceived social status and race. Pain severity and pain interference were not significantly associated with age or sex. Depressive symptom severity was negatively correlated with perceived social status, age, educational achievement, household income. However, the relationship between depression and educational achievement was not statistically significant (p = 0.152). There were no significant relationships between depressive symptoms, race (p = 0.73), and sex (p = 0.50).
Table 2.
Spearman correlation among Variables of Interest
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Pain severity | 1 | ||||||||||
| 2 | Pain Interference | 0.779b | 1 | |||||||||
| 3 | Depressive symptom severity | 0.426 b | 0.562 b | 1 | ||||||||
| 4 | Social Status | −0.207 a | −0.224 a | −0.224 a | 1 | |||||||
| 5 | Medication Use | 0.112 | 0.215 a | 0.168 | −0.144 | 1 | ||||||
| 6 | Race | −0.361 b | −0.220 a | −0.036 | 0.138 | 0.164 | 1 | |||||
| 7 | Age | 0.074 | 0.112 | −0.205 a | 0.126 | 0.275 b | −0.001 | 1 | ||||
| 8 | Sex | −0.097 | −0.117 | 0.069 | 0.167 | −0.061 | 0.064 | −0.300 b | 1 | |||
| 9 | Work Status | 0.226 a | 0.422 b | 0.260 a | −0.266 b | 0.297 b | 0.045 | 0.253 b | −0.227 a | 1 | ||
| 10 | Household Income | −458 b | −0.409 b | −0.372b | 0.346 b | −0.196 | 0.253 a | −0.032 | 0.121 | −0.471 a | 1 | |
| 11 | Education Achievement | −0.218 a | −0.238 a | −0.166 | 0.158 | −0.053 | 0.109 | −0.012 | 0.154 | −0.325 a | 0.462 a | 1 |
= p < 0.05
= p<0.01
Perceived social status modestly positively correlated with household income. 67 percent of Black participants reported an annual household income of less than $50,000 compared with 49 percent of White participants. The relationship between race and household income was statistically significant (p = 0.03), but the relationship between race and perceived social status was not statistically significant (p = 0.16). On average, Whites reported lesser pain severity (t(101) = 3.71, p < 0.001) and pain interference (t(102) = 2.43, p = 0.02) than Blacks. These racial differences were statistically significant. In addition, perceived social status significantly correlated with work status and household income. Finally, as expected, there was a moderately significant relationship between educational achievement, household income, and work status.
Within group analyses revealed that the bivariate relationship between many variables were different between Black and White participants. Results of the Spearman’s rho correlation for both Blacks and Whites are summarized in Supplemental Table 1 and Supplemental Table 2, respectively.
Moderation Analysis
To understand the relationship between perceived social status and pain outcomes among Blacks and Whites with cLBP, we tested whether race moderated the associations between unadjusted perceived social status pain interference as well as pain severity, respectively, using Model 1 of Hayes’ PROCESS (Hayes, 2012). The overall model accounted for approximately 13 percent of the variance in pain interference (R2 = 0.128). There was a statistically significant interaction between race and perceived social status in relation to pain interference (β = −0.59 t(100) = −2.52, p = 0.01). As shown in Figure 2, the relationship between perceived social status and pain interference differed between Blacks and Whites. Specifically, among White participants pain interference decreases by 0.47 units for a 1 unit increase in perceived social status (95% CI [−0.805, −0.139]); however, Black participants pain interference increases by 0.12 units for a 1 unit increase in perceived social status (95% CI [−0.207, 0.439]). The relationship between perceived social status and pain interference among Black participants was not statistically significant (p = 0.48). The interaction between race and perceived social status in predicting pain interference remained statistically significant after controlling for the covariates (objective measures of SES: work status, household income, and education level) (β = −0.48, p = 0.04; 95% CI [−0.95, −0.01]).
Figure 2.
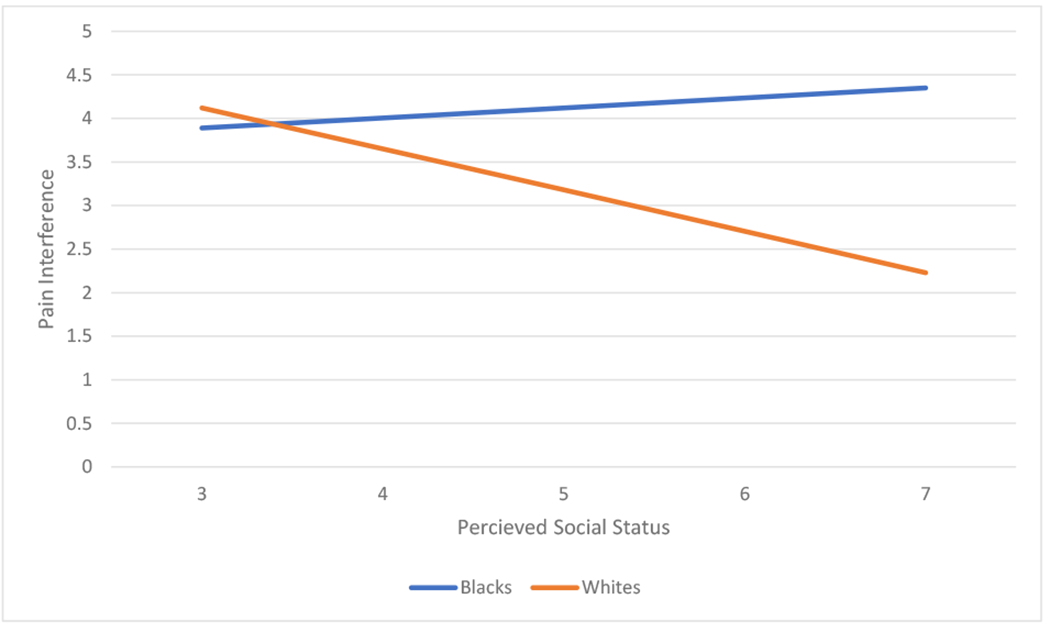
Unadjusted Predicted Moderation Effects of Race on Perceived Social Status in Predicting Pain Interference. The plot shows predicted change in pain interference as a function of perceived social status for Blacks and Whites with chronic low back pain.
We also examined whether the relationship between perceived social status and pain severity was moderated by race. The product term perceived social status x race was not statistically significant (β = −0.154, t (99) = −0.719, 95% CI [−0.580, 0.271). As shown in Figure 3, the conditional effects of race suggested that higher perceived social status decreased pain severity for both Black (β = −0.040, t(99) = −0.272, 95% CI [−0.336, 0.255]) and White (β = −0.195, t(99) = −1.261, 95% CI [−0.501, 0.112]) participants. The interaction of race and perceived social status added 0.45% explained variance to the model and this was not statistically significant (p = 0.474).
Figure 3.
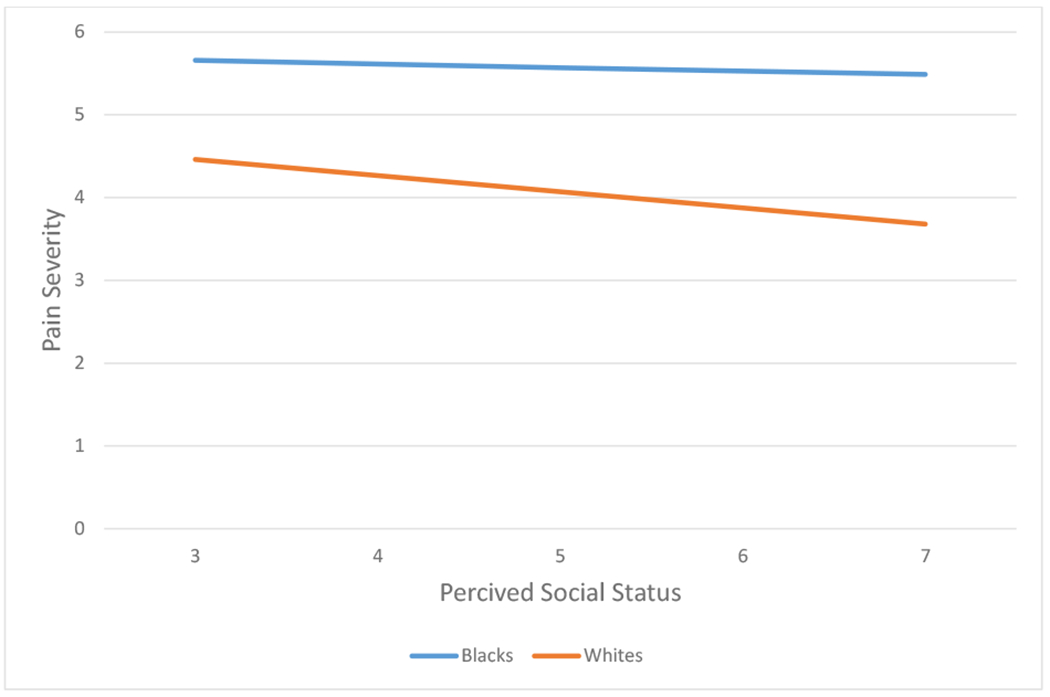
Unadjusted Predicted Moderation Effects of Perceived Social Status on Pain Severity under the Influence of Race. The plot shows predicted change in pain severity as a function of perceived social status for Blacks and Whites with chronic low back pain.
For comparison, we also tested whether race moderated the relationship between objective measures of SES (educational achievement, work status, and household income) and pain outcomes (pain interference and pain severity). As summarized in Table 3, the product terms of race and the objective measures of SES in predicting pain interference were not statistically significant (p > 0.05). Similarly, race did not significantly moderate the relationship between objective measures of SES and pain severity (p > 0.05).
Table 3.
Effect of SES on Pain Interference and Pain Severity under the Influence of Race
| Variables |
β | SE B | p-value | 95% CI |
Model R | Model R2 | F | ΔR2 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Predictor | LL | UL | |||||||
| Pain interference | Social status | 0.7 | 0.37 | 0.06 | −0.02 | 1.43 | 0.36 | 0.13 | 4.9 | 0.06 |
| Race | 1.99 | 1.31 | 0.13 | −0.6 | 4.6 | |||||
| Race X social statusa | −0.59 | 0.23 | 0.01 | −1.05 | −0.12 | |||||
| Household income | −0.19 | 0.18 | 0.29 | −0.55 | 0.17 | 0.41 | 0.17 | 6.64 | 0.0002 | |
| Race | −0.62 | 0.96 | 0.52 | −2.52 | 1.28 | |||||
| Race X income | −0.02 | 0.12 | 0.88 | −0.25 | 0.22 | |||||
| Work status | 0.35 | 0.25 | 0.16 | −0.14 | 0.86 | 0.43 | 0.19 | 7.67 | 0.0004 | |
| Race | −1.21 | 0.68 | 0.08 | −2.57 | 0.15 | |||||
| Race X work status | −0.03 | 0.15 | 0.82 | −0.34 | 0.27 | |||||
| Education | −0.43 | 0.63 | 0.49 | −1.67 | 0.81 | 0.3 | 0.09 | 3.35 | <0.0001 | |
| Race | −1.14 | 2.68 | 0.67 | −6.45 | 4.17 | |||||
| Race X Education | 0.01 | 0.42 | 0.97 | −0.81 | 0.84 | |||||
| Pain Severity | Social status | 0.11 | 0.33 | 0.73 | −0.55 | 0.78 | 0.37 | 0.13 | 5.14 | 0.004 |
| Race | −0.73 | 1.2 | 0.54 | −3.11 | 1.65 | |||||
| Race X social status | −0.15 | 0.21 | 0.47 | −0.58 | 0.27 | |||||
| Household income | −0.18 | 0.16 | 0.26 | −0.49 | 0.13 | 0.5 | 0.25 | 10.63 | 0.0003 | |
| Race | −1.04 | 0.83 | 0.21 | −2.69 | 0.6 | |||||
| Race X income | −0.02 | 0.1 | 0.84 | −0.22 | 0.18 | |||||
| Work status | 0.23 | 0.23 | 0.33 | −0.23 | 0.69 | 0.4 | 0.16 | 6.42 | 0.001 | |
| Race | −1.51 | 0.64 | 0.02 | −2.79 | 0.23 | |||||
| Race X work status | −0.05 | 0.14 | 0.74 | −0.33 | 0.23 | |||||
| Education | −0.63 | 0.56 | 0.26 | −1.17 | 0.47 | 0.39 | 0.15 | 5.82 | 0.0029 | |
| Race | −2.87 | 2.38 | 0.23 | −7.59 | 1.86 | |||||
| Race X Education | 0.22 | 0.37 | 0.56 | −0.52 | 0.95 | |||||
Statistically significant interaction; income = Annual household income; CI = confidence interval; LL = Lower limit of 95% CI; UL = Upper limit of 95% CI
Moderated Mediation Analysis
To test our second hypothesis, we used Model 7 of the PROCESS macro to examine the conditional indirect effect of age adjusted perceived social status on pain outcomes through depressive symptoms (mediator). This model tested whether race moderated the relationship between perceived social status and depressive symptom severity, which mediated the relationship between perceived social status and pain outcomes.
First, we examined whether race moderated the relationship between perceived social support and depressive symptoms. After adjusting for age, the interaction term (race x perceived social support) was significant (p = 0.006), adding 8% of explained variance to the model. The conditional effect of race on perceived social support at 16th, 50th, and 84th percentile, depicted in figure 4, reveal that the association between perceived social support and depressive symptoms have a significant relationship only for White participants (95% CI [−3.93, −0.74]), but not for Black participants (95% CI [−0.73, 2.38]). Among White participants, depressive symptoms decrease by 2.33 units for a 1 unit increase in perceived social status (p = 0.005), but for Black participants depressive symptoms increase by 0.83 units for 1 unit increase in perceived social status (p = 0.29). These results suggested that the indirect effect of perceived social status on pain interference through depressive symptoms may depend on the participant’s race. Our model (Figure 5) accounted for about 32 percent of the variance in pain interference. The estimated index of moderated mediation (the effect of race on the indirect of perceived social status on pain interference through depressive symptom severity) of B = −0.39 (Boot 95% CI = −0.73, −0.10), which was statistically significant. Table 4 summarizes the conditional indirect effect of perceived social status on pain interference by race. As hypothesized, the indirect effect of perceived social status on pain interference via depressive symptoms was moderated by race. For white participants pain interference decreases by 0.29 units for a 1 unit increase in perceived social status (Boot 95% CI = −0.53, −0.09), while for Black participants pain interference increases by 0.10 units for every unit increase in perceived social status (Boot 95% CI = −0.10, 0.32).
Figure 4.
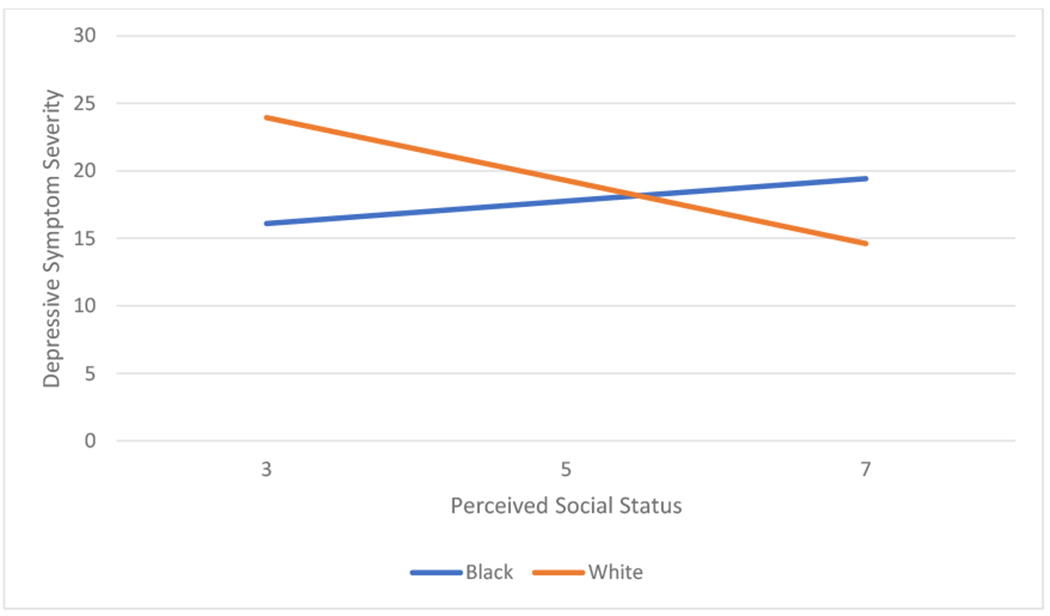
Age-adjusted Predicted Conditional Effect of Perceived Social Status on Depressive Symptom as a Function of Race. The plot shows age-adjusted predicted change in depressive symptoms as a function of perceived social status for Blacks and Whites with chronic low back pain.
Figure 5.
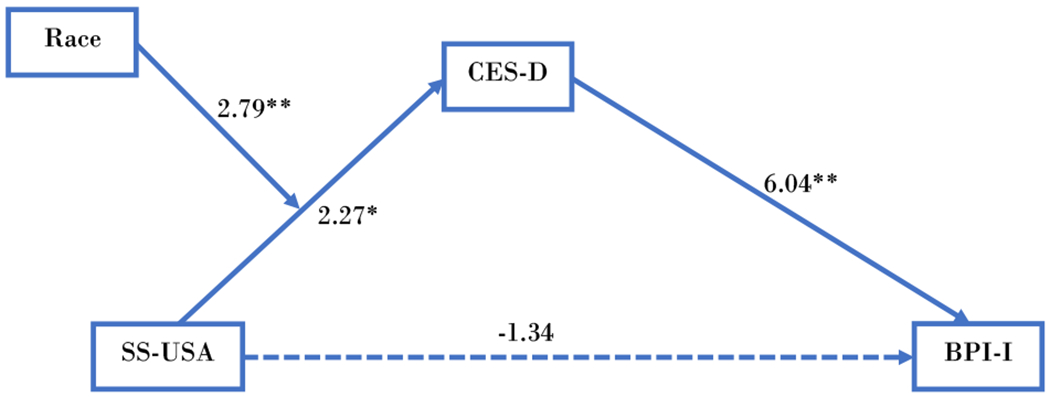
The Interrelationship between Perceived Social Status, Race, Depressive Symptoms, and Pain Interference. Age-adjusted values on the figure are t-statistic. *= p<0.05; ** = p<0.01; SS-USA = Perceived social status in the USA; BPI-I = Brief pain inventory- interference; CES-D = Center for Epidemiological Studies of Depression.
Note: Age-adjusted values on the figure t-statistic. *= p<0.05; ** = p<0.01; SS-USA = Perceived social status in USA; BPI-I = Brief pain inventory- interference; CES-D = Center for Epidemiological Studies of Depression
Table 4.
Conditional Indirect Effect of Perceived Social Status on Pain Interference
| Mediator: Depressive Symptoms | Effect | Boot SE | Boot 95% CI | |
|---|---|---|---|---|
| LL | UL | |||
| Blacks | 0.10 | 0.10 | −0.10 | 0.31 |
| Whites | −0.29 | 0.11 | −0.53 | −0.08 |
| Index of moderated mediation | ||||
| Race | −0.40 | 0.16 | −0.73 | −0.10 |
Note. Bootstrap resample = 5000. SE = standard error; CI = confidence interval; LL = lower limit; UL = upper limit; Age adjusted estimates are calculated using the PROCESS macro.
For comparison, we performed a similar analysis to test the age adjusted conditional indirect effect of perceived social status on pain severity through depressive symptoms. Figure 6 shows the results of the moderated mediation analysis. The model accounted for about 19 percent of the variance in pain severity (R2 = 0.19). The estimated index of the moderated mediation was B = −0.27 (Boot 95% CI = −0.5463, −0.0712). As expected, the indirect effect of perceived social status on pain severity via depressive symptoms (mediator) depended on the participant’s race. For White participants pain severity decreases by 0.20 unit for every unit increase in perceived social status (Boot 95% CI = −0.41, −0.05), while for Black participants pain severity increases by 0.07 units for every unit increase in perceived social status. The indirect effect of perceived social status on pain severity via depressive symptoms was statistically significant for White participants, but not for Black participants (Table 5).
Figure 6.
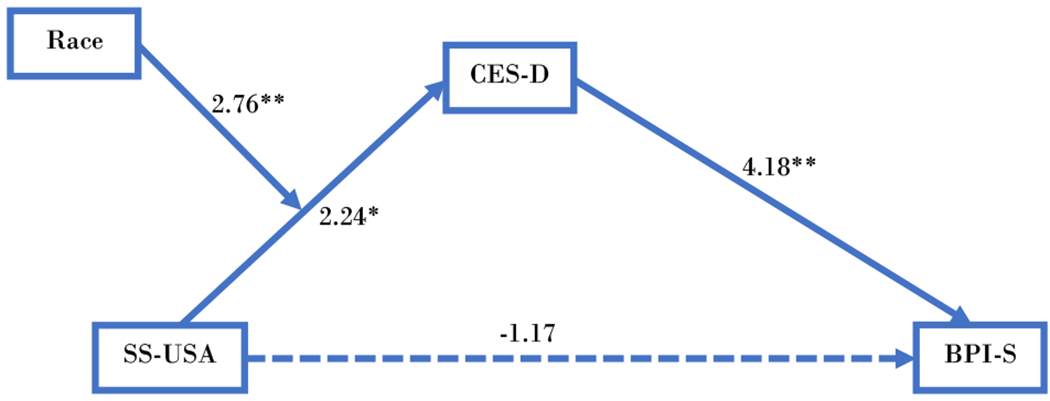
The Interrelationship between Perceived Social Status, Race, Depressive Symptoms, and Pain Severity. Age-adjusted values on the figure t-statistic; *= p<0.05; ** = p<0.01; SS-USA = Perceived social status in USA; BPI-I = Brief pain inventory- severity; CES-D = Center for Epidemiological Studies of Depression.
Note: Age-adjusted values on the figure t-statistic; *= p<0.05; ** = p<0.01; SS-USA = Perceived social status in USA; BPI-I = Brief pain inventory- severity; CES-D = Center for Epidemiological Studies of Depression
Table 5.
Predicted Conditional Direct and Indirect Effects of Perceived Social Status on Pain Severity
| Conditional Direct Effect | Effect | SE | t | p | 95 % CI | ||
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Perceived Social Status | −0.13 | 0.11 | −1.17 | 0.24 | −0.36 | 0.09 | |
| Conditional Indirect Effect | |||||||
| Mediator: Depressive symptoms | Effect | Boot SE | Boot 95% CI | ||||
| LL | UL | ||||||
| Black | 0.07 | 0.08 | −0.08 | 0.23 | |||
| Whites | −0.20 | 0.09 | −0.41 | −0.04 | |||
| Index of Moderated Mediation | |||||||
| Race | −0.27 | 0.13 | −0.55 | −0.05 | |||
Note. Bootstrap resample = 5000. SE = standard error; CI = confidence interval; LL = lower limit; UL = upper limit; Age adjusted estimates are calculated using the PROCESS macro
Discussion
To the best of our knowledge, this is the first study to empirically examine a moderated mediation model that integrates known predictors of pain outcomes (depressive symptoms, race, and SES) in patients with cLBP. Consistent with the biopsychosocial framework, our model assumed that race is a social construct shaped by lived experiences that affect the experience of pain.36 Our study explicates the pathway by which perceived social status could predict racial differences in cLBP interference and severity through depressive symptoms. Other researchers have reported that perceived social status predicts depressive symptoms,37 and depressive symptoms predict pain outcomes16 in patients with chronic pain conditions. The interactions of race, perceived social status, depressive symptoms, and cLBP interference suggest potential differences in the use/effects of perceived social status between Blacks and Whites. Greater perceived social status is associated with less severe depressive symptoms, which in turn is associated with less pain severity and less pain interference for White participants with cLBP. Although not significantly, the results of the conditional indirect effect of depressive symptoms in Blacks show a positive effect on pain interference. In essence, they suggest that for Blacks individuals, increasing social status increases depressive symptoms that increase pain interference. Others have reported that when Black individuals climb the social ladder, systemic discrimination and organizational structures often limit their potential by placing less value in their experience and rewarding them less economically. Their awareness of these limitations and discriminatory practices may result in more depressive symptoms and fewer health benefits of their perceived social status.38 Hence, Blacks with cLBP, especially those with higher perceived social status, may require more aggressive screening and intervention of depressive symptoms. More studies are needed to understand the factors that mediate the relationship between perceived social status and pain interference in Blacks with cLBP.38
In our sample, race moderates the relationship between perceived social status and pain interference, but not pain severity. Despite the strong correlation between pain interference and pain severity, these findings point to the critical differences between the two measures of pain. Previous studies have shown that the differences in pain severity and pain interference may be because pain severity reflects pain intensity. In contrast, pain interference reflects pain intensity and the participant’s perceptions of the magnitude of the pain and belief about their pain.39 Thus, racial differences in factors such as catastrophizing, coping, and social support that affect pain perception, may influence pain interference. 40,41
Both objective and subjective measures of SES correlated with pain interference. However, when analyzed in a regression model, race moderated only the relationship between the subjective measure of SES (perceived social status) and pain interference. Thus, despite the fact that the relationship between perceived social status and pain interference among Blacks with cLBP was not statistically significant, the results suggest potential opposing trends for Blacks and Whites: among Blacks with cLBP, pain interference appears to increase with higher perceived social status, but pain interference decreases with higher social status for Whites with cLBP. It has been reported that White individuals view their social status as a reflection of objective measures of SES, while Black individuals consider non-objective measures of SES.27,28 Our findings corroborate the findings of other researchers that subjective and objective measures of SES are not interchangeable.26 Investigators and clinicians should consider both objective and subjective SES, and pain severity (intensity) and pain interference when evaluating racial differences in chronic pain.
Depressive symptoms play a critical role in the cLBP experience (especially for White participants). We found that despite the strong positive correlation between pain interference and pain severity in our study, race did not moderate the relationship between perceived social status and pain severity, even after adding depressive symptoms was a covariate. However, when depressive symptoms were analyzed as a mediator, perceived social status predicted pain severity by race. Unlike a moderation analysis that shows when or under what conditions a predictors variable is related to an outcome variable, mediation analysis explains why or “how a causal effect operates”(p47).34 Thus, the focus of mediation is on understanding the mechanism or underlying process. Our findings suggest depressive symptoms severity, is an underlying variable that drives the relationship between perceived social status and pain outcomes in patients with cLBP. This “causal effect” of depressive symptoms is consistent with previous studies which found that depressive symptoms reliably predict the course of cLBP.12,16
This study had some limitations regarding the interpretation of results that must be mentioned. First, the cross-sectional design limits our interpretation of mediation analysis. The time from the assessment of the independent variables (perceived social status and depressive symptoms) to the assessment of pain outcomes was about one week. This time frame is relatively short for the causal effect of the depressive symptoms to become evident in pain interference and pain severity. Thus, these findings must be interpreted with caution with regard to the causal effect of depressive symptoms. In addition, it is possible that the direction of the relationship between the predictor and outcome was reversed, such that the pain outcomes resulted in perceived social status via depressive symptoms. However, based on our theoretical model, these findings would still be valid under those circumstances. Thus, there is a need for a longitudinal assessment of the moderated mediation effect of perceived social status on pain outcomes through depressive symptoms to determine temporality and more robust causal inferences. Second, these findings are part of an extensive ongoing study, which implies that the results may change once the study is completed. From our estimates, a sample size of approximately 105 is large enough to power this study. Besides, boots strapping was used to increase the accuracy of the estimates. Finally, because of small cell sizes, we could not stratify the results by the type of pain medication used by participants. Instead, we categorized the participants by medication status: whether they used pain medications (prescription or over the counter) or not. However, this increases the generalizability of our findings as they reflect the real-life experiences of the participants since all participants were instructed to take their usual medications.
Conclusion
cLBP remains the leading cause of years lived with disability, despite advances in health care and pain management approaches. There are racial and SES differences in cLBP, and this study sheds some light on the complex inter-relationship between subjective SES, depressive symptoms, and racial differences in cLBP. Perceived social status seems to confer mental health and pain benefits for the White participants; however, perceived social status does not provide the same type of benefits for the Black participants. This may be because, among the Blacks, higher perceived social status is (contrary to what might be expected) associated with more pain interference and worse depressive symptoms. A more individualized approach to cLBP management that accounts for the role of depressive symptoms and perceived social status may decrease racial differences in cLBP.
Supplementary Material
What’s already known about this topic?
Globally, low back pain is the leading cause of disability and it disproportionately affects non-Hispanic Blacks and individuals of lower socioeconomic status.
Individual’s perception of their social status can affect their health status.
What does this study add?
Race moderates the indirect relationship between perceived social status and pain outcomes via depressive symptoms.
Perceived social status seems to confer mental health and pain benefits for the Whites, but not for Blacks with chronic low back pain.
Significance-.
It has been suggested that racial differences in chronic pain cannot be fully understood with consideration of socioeconomic status. Our findings suggest race moderates the indirect relationship between subjective social status and pain outcomes through depressive symptoms (mediators). Specifically, perceived social status seems to confer health benefits for the Whites, but not for Blacks, with chronic low back pain. Among the Blacks, higher perceived social status is associated with more pain interference and worsen depressive symptom
Acknowledgments
Funding: Financial support for this research was provided by the NIH/NIMHD Grant R01MD010441 (BRG) and NIH/NIMHD Administrative Supplement R01MD010441-03 (ENA).
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest. All authors discussed the results and commented on the manuscript.
References
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubin DI. Epidemiology and Risk Factors for Spine Pain. Neurologic clinics. 2007;25(2):353–371. [DOI] [PubMed] [Google Scholar]
- 3.Meucci RD, Fassa AG, Faria NMX. Prevalence of chronic low back pain: systematic review. Revista de Saúde Pública. 2015;49:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Treede R-D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daubs MD, Norvell DC, McGuire R, et al. Fusion versus nonoperative care for chronic low back pain: do psychological factors affect outcomes? Spine. 2011;36(21 Suppl):S96–109. [DOI] [PubMed] [Google Scholar]
- 6.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Archives of Internal Medicine. 2009;169(3):251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Green CR, Baker TA, Sato Y, Washington TL, Smith EM. Race and chronic pain: A comparative study of young black and white Americans presenting for management. The journal of pain : official journal of the American Pain Society. 2003;4(4):176–183. [DOI] [PubMed] [Google Scholar]
- 8.Meints SM, Wang V, Edwards RR. Sex and Race Differences in Pain Sensitization among Patients with Chronic Low Back Pain. Journal of Pain. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green CR, Hart-Johnson T. The association between race and neighborhood socioeconomic status in younger Black and White adults with chronic pain. The journal of pain : official journal of the American Pain Society. 2012;13(2):176–186. [DOI] [PubMed] [Google Scholar]
- 10.Buchbinder R, van Tulder M, Öberg B, et al. Low back pain: a call for action. The Lancet. 2018;391(10137):2384–2388. [DOI] [PubMed] [Google Scholar]
- 11.Hill JC, Fritz JM. Psychosocial influences on low back pain, disability, and response to treatment. Phys Ther. 2011;91(5):712–721. [DOI] [PubMed] [Google Scholar]
- 12.Campbell P, Hope K, Dunn KM. The pain, depression, disability pathway in those with low back pain: a moderation analysis of health locus of control. Journal of Pain Research. 2017;10:2331–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Main CJ, George SZ. Psychologically informed practice for management of low back pain: future directions in practice and research. Physical therapy. 2011;91(5):820–824. [DOI] [PubMed] [Google Scholar]
- 14.Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 2018;391(10137):2368–2383. [DOI] [PubMed] [Google Scholar]
- 15.Moix J, Kovacs FM, Martin A, Plana MN, Royuela A. Catastrophizing, state anxiety, anger, and depressive symptoms do not correlate with disability when variations of trait anxiety are taken into account. a study of chronic low back pain patients treated in Spanish pain units [NCT00360802]. Pain Med. 2011;12(7):1008–1017. [DOI] [PubMed] [Google Scholar]
- 16.Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. The spine journal : official journal of the North American Spine Society. 2016;16(1):105–116. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez M, Colodro-Conde L, Hartvigsen J, et al. Chronic low back pain and the risk of depression or anxiety symptoms: insights from a longitudinal twin study. The Spine Journal. 2017;17(7):905–912. [DOI] [PubMed] [Google Scholar]
- 18.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of general psychiatry. 2007;64(3):305–315. [DOI] [PubMed] [Google Scholar]
- 19.Woodward AT, Taylor RJ, Abelson JM, Matusko N. Major depressive disorder among older African Americans, Caribbean blacks, and non-Hispanic whites: secondary analysis of the National Survey of American Life. Depress Anxiety. 2013;30(6):589–597. [DOI] [PubMed] [Google Scholar]
- 20.Bailey RK, Mokonogho J, Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatric disease and treatment. 2019;15:603–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assari S, Preiser B, Lankarani MM, Caldwell CH. Subjective Socioeconomic Status Moderates the Association between Discrimination and Depression in African American Youth. Brain sciences. 2018;8(4):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wheaton FV, Thomas CS, Roman C, Abdou CM. Discrimination and Depressive Symptoms Among African American Men Across the Adult Lifecourse. The Journals of Gerontology: Series B. 2017;73(2):208–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine. 2008;358(23):2468–2481. [DOI] [PubMed] [Google Scholar]
- 24.Green CR, Hart-Johnson T. The association between race and neighborhood socioeconomic status in younger Black and White adults with chronic pain. The journal of pain : official journal of the American Pain Society. 2012;13(2):176–186. [DOI] [PubMed] [Google Scholar]
- 25.Garbarski D Perceived social position and health: Is there a reciprocal relationship? Social Science & Medicine. 2010;70(5):692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaked D, Williams M, Evans MK, Zonderman AB . Indicators of subjective social status: Differential associations across race and sex. SSM - Population Health. 2016;2:700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolff LS, Acevedo-Garcia D, Subramanian SV, Weber D, Kawachi I. Subjective Social Status, a New Measure in Health Disparities Research: Do Race/Ethnicity and Choice of Referent Group Matter? Journal of Health Psychology. 2010;15(4):560–574. [DOI] [PubMed] [Google Scholar]
- 28.Jackman MR, Jackman RW. An Interpretation of the Relation Between Objective and Subjective Social Status. Am Sociol Rev. 1973;38(5):569. [PubMed] [Google Scholar]
- 29.Adler N, Singh-Manoux A, Schwartz J, Stewart J, Matthews K, Marmot MG. Social status and health: A comparison of British civil servants in Whitehall-II with European- and African-Americans in CARDIA. Social Science & Medicine. 2008;66(5):1034–1045. [DOI] [PubMed] [Google Scholar]
- 30.Thompson KA, Terry EL, Sibille KT, et al. At the Intersection of Ethnicity/Race and Poverty: Knee Pain and Physical Function. Journal of Racial and Ethnic Health Disparities. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deyo RA, Dworkin SF, Amtmann D, et al. Report of the NIH Task Force on research standards for chronic low back pain. Physical therapy. 2015;95(2):e1–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adler NE, Stewart J. The MacArthur Scale of Subjective Social Status. In. Psychosocial Research Notebook 2007.
- 33.Hayes AF. PROCESS : A Versatile Computational Tool for Observed Variable Mediation , Moderation , and Conditional Process Modeling 1. 2012.
- 34.Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy. 2017;98:39–57. [DOI] [PubMed] [Google Scholar]
- 35.Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Statistics in Medicine. 2000;19(9):1141–1164. [DOI] [PubMed] [Google Scholar]
- 36.Anderson KO, Green CR, Payne R. Racial and Ethnic Disparities in Pain: Causes and Consequences of Unequal Care. The Journal of Pain. 2009;10(12):1187–1204. [DOI] [PubMed] [Google Scholar]
- 37.Diaz OV, Guendelman S, Kuppermann M. Subjective Social Status and Depression Symptoms: A Prospective Study of Women with Noncancerous Pelvic Problems. Women’s Health Issues. 2014;24(6):649–655. [DOI] [PubMed] [Google Scholar]
- 38.Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: how race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. J Youth Adolesc. 2009;38(2):242–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jensen MP, Tomé-Pires C, de la Vega R, Galán S, Solé E, Miró J. What Determines Whether a Pain is Rated as Mild, Moderate, or Severe? The Importance of Pain Beliefs and Pain Interference. The Clinical journal of pain. 2017;33(5):414–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meints SM, Hirsh AT. In Vivo Praying and Catastrophizing Mediate the Race Differences in Experimental Pain Sensitivity. The Journal of Pain. 2015;16(5):491–497. [DOI] [PubMed] [Google Scholar]
- 41.Bartley EJ, Hossain NI, Gravlee CC, et al. Race/Ethnicity Moderates the Association Between Psychosocial Resilience and Movement-Evoked Pain in Knee Osteoarthritis. ACR Open Rheumatology. 2019;1(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


