Abstract
New and innovative approaches are needed to improve the prevention, diagnosis, and treatment of HIV in low-income and middle-income countries. Several trials use conditional economic incentives (CEIs) to improve HIV outcomes. Most CEI interventions use a traditional economic theory approach, although some interventions incorporate behavioural economics, which combines traditional economics with insights from psychology. Incentive interventions that are appropriately implemented can increase HIV testing rates and voluntary male circumcision, and they can improve other HIV prevention and treatment outcomes in certain settings in the short term. More research is needed to uncover theory-based mechanisms that increase the duration of incentive effects and provide strategies for susceptible individuals, which will help to address common constraints and biases that can influence health-related decisions.
Introduction
Nearly four decades into the pandemic, HIV continues to devastate communities around the world, particularly in low-income and middle-income countries (LMICs). The rapid scale up of antiretroviral therapy (ART) has substantially improved survival rates and reduced incidence rates, yet additional efforts are essential to achieve control of the pandemic.1 Recent (2018) global guidance strategies aim to address HIV in the context of multiple social determinants of health, including poverty, income and gender inequality, stigma and discrimination, and social exclusion.2 Conditional economic incentives (CEIs) are a new approach that can improve HIV control and therefore warrant further and expanded application.
CEIs (defined in the panel) can be viewed in the larger context of behavioural economics, which combines traditional economic theory with psychological insights, to produce more realistic models and improve decision making.6 Compared with the standard economic theory, which assumes individuals make rational decisions that maximise overall wellbeing, behavioural economics understands that humans are heuristic in nature7 and make decisions on the basis of non-standard preferences8 and systematic biases.9 By providing insights into the factors that influence decision making, behavioural economics facilitates the design of interventions that address these factors to improve outcomes at both the individual and population levels. General introductions to the topic are available.10–12 Formal models have been summarised in reviews and collected volumes,7,13–15 including applications to health16 and development.17 Regarding health and HIV programming, distinct interventions related to behavioural economics have been applied, including conditional cash transfers to increase the use of preventive services,18,19 CEIs for reducing HIV risk behaviours,3,20 and economic strengthening to improve linkage and adherence to treatment.20–23
HIV testing
Several randomised controlled trials have focused on incentives to increase HIV testing (table; appendix pp 1–8).24–27 For example, one study24 in Malawi involving 2812 participants, tested the use of vouchers (US$0·00–3·00) to increase the frequency of individuals returning to receive their HIV test results. Non-zero incentives more than doubled the percentage of people returning to receive test results and thereby learn their HIV status. Another study in Ethiopia25 tested incentives to increase facility-based voluntary counselling and testing (VCT) in 1658 individuals. HIV/AIDS education, combined with either home-based VCT or conditional incentives ($1·50–2·90) for facility-based VCT, significantly increased the rate of HIV testing uptake.25 A study in Zimbabwe26 randomly assigned 68 rural geographical clusters to incentivise at-risk couples to receive couples HIV testing and counselling. In the intervention communities, couples who tested together could select one of three grocery items (each worth approximately $1·50 in value). The proportion of individuals who tested with a partner increased significantly.26 Another study in Zimbabwe randomly assigned 2050 households to receive either a fixed incentive ($2·00), a lottery incentive ($5·00 or $10·00, with a 12·5% chance of winning), or no incentive, to evaluate the effect of monetary incentives on improving the rates of HIV testing and counselling in children.27 Compared with the control group, both fixed and lottery-based incentives increased the proportion of households in which at least one child or adolescent tested for HIV within 4 weeks of study enrolment.27
Economic incentives, particularly fixed monetary incentives and conditional cash transfers, seem to be effective for increasing HIV testing in LMICs. Researchers and policy makers might choose to provide CEIs to at-risk populations, such as children and serodiscordant couples, to make better use of resources. Ongoing studies include adaptive trials (NCT02735642) and non-monetary and low-valued incentives to increase HIV testing uptake and repeated testing (NCT02890459 and NCT02714140).28
HIV prevention
As with HIV testing, several trials have focused on economic incentives for HIV prevention, including HIV and sexually transmitted infection (STI) prevalence and incidence, as well as male circumcision.29–36 For instance, a trial in Tanzania incentivised being free of new curable STIs (a marker for HIV acquisition), among 2399 adult participants aged 18–30 years.29 Participants were randomly assigned to either a low-value CEI group, in which they received $10·00 every 4 months, or a high-value CEI group, in which they received $20·00 every 4 months. A reduction in the combined point prevalence of four curable STIs in the high-value CEI group was observed.29 Another study in Malawi provided incentives ($0·00–32·00) for participants to maintain their HIV status for 1 year; however, these incentives did not affect HIV incidence.30 An additional study in Malawi involving 3796 participants aged 13–22 years used conditional ($1·00–5·00 per month) or unconditional cash transfers, , to incentivise adolescent girls and young women to stay in school. The results showed reductions in HIV prevalence in the combined intervention group.31 The unconditional cash transfer group had no obvious benefit in terms of reducing HIV prevalence.31 However, unconditional cash transfers were worse incentives than conditional cash transfers in terms of educational outcomes.46,47 By contrast, a study in South Africa involving 2537 participants concluded that conditional monthly cash transfers of $10 for participants and $20 for parents or guardians on the basis of school attendance had no direct effect on HIV incidence rates among adolescent girls and young women aged 13–20 years.34 A study in Mexico evaluated the effect of incentives on the number of sexual partners, condom use, and infection with HIV or STIs, or both, among 267 male sex workers. Participants were randomly assigned to either a control group or to one of two intervention groups with STI conditionality (in which participants received either $50 or $75 at 6 and 12 months if they were free of new curable STIs).35 An additional fourth group received $50 at 6 and 12 months if they simply attended their scheduled clinic visits. The incentives increased clinic visits and condom use but had no effect on the number of partners, nor the combined incidence of HIV and STIs.35 A study in Lesotho involving 3029 males and females aged 18–32 years used a lottery ticket strategy for HIV prevention.36 Tickets were distributed if participants were free of new curable STIs, which meant that the actual probability of winning depended on the number of STI-free lottery ticket holders. Four winners received $50 (low-prize) or $100 (high-prize) per village every 4 months. Everyone received goods worth $3 as a courtesy for participation. The results showed that these incentives reduced HIV incidence.36 The effect of the incentive was stronger (3·3 percentage points or around 28%) in the high prize versus the low prize lottery group, and among women versus men, particularly those who were prone to take financial risks (ie, those classified as showing risk-seeking behaviours in terms of lotteries and investments).
Voluntary medical male circumcision (VMMC) reduces the risk of acquiring HIV in men by more than 50%.48–50 Two studies used incentives to increase uptake of VMMC.32,33 One study in Kenya randomly assigned 1504 uncircumcised men aged 25–49 years to three intervention groups receiving varying amounts of com pen sation conditional on the participants undergoing circumcision within 2 months.32 Compensation was given as food vouchers with values of either $2·50, $8·75, or $15·00. The $8·75 and $15·00 groups had a higher VMMC uptake than the control group, which received no compensation. In another study in Kenya, 909 uncircumcised men aged 21–39 years were assigned to either a control or one of two intervention groups.33 One group of participants were given a fixed incentive ($12·50 in the form of food vouchers) conditional on circumcision uptake. The second group was given a lottery incentive with an equivalent expected value to the fixed incentive (ie, the participants had a 5% chance of winning a smartphone or bicycle worth $120·00, a 10% chance of winning a regular mobile phone or a pair of shoes worth $45·00, or an 85% chance to win a food voucher worth $2·50). Uptake of VMMC increased in the fixed incentive group, but no significant difference in VMMC uptake was observed among the different lottery groups.
CEIs can decrease the risk of acquiring HIV through sexual intercourse, and they can increase protection from HIV infection by reducing the number of sexual partners, increasing condom use, and decreasing biological susceptibility (in terms of VMMC), thereby potentially reducing HIV incidence. Lottery and cash incentives can be more effective when allocated to groups of individuals who adhere to the conditionality. Increasing the use of incentives to control STIs and uptake of VMMC can be one important step towards decreasing HIV incidence. Ongoing and published studies selectively incentivise new approaches, such as pre-exposure prophylaxis (NCT03674983), or use lotteries for dual protection (prevention of HIV and unwanted pregnancy).37
Linkage to care
Some randomised controlled trials have used economic incentives to increase linkage to care.38,39 In India, giving non-monetary vouchers redeemable for food or household goods ($4 for ART initiation, $4 for visit attendance, and $8 for viral suppression) led to higher rates of linkage to HIV care, ART initiation, and retention in care among 120 men who use drugs; however, no differences in HIV RNA levels or CD4 cell counts were observed.38 In South Africa, an incentive ($23 in value) given within 3 months of HIV diagnosis, did not improve linkage to care rates and was not associated with faster linkage to care.5 A cluster trial in eSwatini implemented incentives to promote a combined strategy of linkage to care and retention in care among 2197 adults aged 18 years and older.39 A non-cash financial incentive (phone network airtime) was provided for linkage to care within 1 month of testing, and after attending follow-up visits at 6 and 12 months. Compared with the standard of care, participants receiving incentives were more likely to be screened for ART initiation, to initiate ART sooner (in 7 days vs 14 days), and to be retained in care.39
Retention in care, treatment adherence, and viral suppression
Several studies have focused on the effect of incentives for retention in care, treatment adherence and viral suppression.40–44 A study in the Democratic Republic of the Congo offered small cash incentives (worth $5, increasing in value by $1 upon each visit) to 433 pregnant women who were living with HIV, starting from 28 weeks of gestation. Compared with the control group receiving no compensation, escalating incentives led to higher retention in care at 6 weeks post partum and higher complete utilisation of prevention of mother-to-child transmission (PMTCT) services (complete utilisation of PMTCT services was when the mother attended all clinic visits and used all available services for 6 weeks post partum).40 Cash incentives that increased in value were more strongly correlated with linkage to care and retention in care for mothers who were worse off economically, walked to the clinic, were pregnant for at least a second time, and those who did not disclose their HIV status.40 The same study included a viral suppression biomarker and found that pregnant women living with HIV who received escalating incentives (ie, incentives that increased in value) had higher retention to PMTCT care; however, no increase in the rate of ART adherence or improvement in viral suppression was observed when compared with the control group, which received no compensation.41
To improve ART adherence, one study in Uganda gave small prizes ($1·50 in value) to 155 men and women (aged 19–78 years) infected with HIV on the condition of clinic attendance or when at least 90% adherence was achieved.42 By use of medical event monitoring system caps, the study showed that the adherence rate (defined as the proportion of participants taking at least 90% of pills) improved in those receiving small prizes as an incentive when compared with the control group that received no prizes.42 Another study in Tanzania, evaluated the effect of short-term cash and food assistance incentives to improve adherence to ART and retention in care among 805 adults (aged 18 years and older) who were infected with HIV.43 Cash transfers ($11 per month for 6 or less consecutive months) given to participants on the condition of clinic visit attendance were associated with an increased medication possession ratio (≥95%) at 6 months. This study highlighted that intrinsic motivation is not negatively influenced by the incentives.44
Providing escalating cash incentives can be effective for sustaining retention in care, especially in populations who have greater financial needs. Vouchers or non-monetary incentives can be effective for increasing ART adherence when given on the condiion that participants show repeated viral suppression. Sustaining viral suppression depends on adherence to treatment and care early in the HIV care continuum. At the early stages of HIV care, incentives can be used to first increase retention in care and to subsequently decrease viral load. Ongoing research investigates the potential effects of incentives on continued ART adherence and viral suppression (NCT03494777).45
Psychological responses to CEIs in HIV
Humans can, of their own accord, make decisions that might not be in their best interest, which creates an opportunity for libertarian paternalism.51 Public policy can assist individuals to make informed decisions that are in their better interest, and that align with public health policies.52 CEIs can improve HIV testing rates;24–27 however, the effect of incentives for HIV prevention can be variable. Three studies29,31,36 have shown positive results for HIV prevention by use of biomarkers; however, only two of these studies31,36 were HIV-specific, and only one study36 showed results for the effect of incentives on HIV incidence. Although fixed incentives increase uptake of VMMC, lottery incentives do not.32,33,53 Also, even though three studies38–40 have shown a positive effect of incentives on the intermediate process indicators for linkage and retention, none of these studies included results for biomarkers. Overall, these findings suggest that CEIs have a positive effect on HIV testing rates and VMMC, as well as on HIV prevention and treatment programmes in some settings. These findings are consistent with the results of other previous studies.3,20–23
The next step is to investigate why incentives work in some settings and not in others, focusing on psychological responses and potential pathways (figure 1). Most studies build on existing theoretical frameworks, and some studies explicitly mention potential mechanisms for behaviour change or assess at least one mechanism (appendix pp 9–11). Although material incentives alone should not be interpreted as a form of behavioural economics intervention, some CEIs can be used to increase saliency, offset present-biased decision making, or increase motivation. However, specific theory-based hypotheses related to the mechanisms of behaviour change are not always tested. Furthermore, the existing literature includes many studies that would not be considered as having behavioural economics applications because they are not supported by underlying psychological theories.6 A more strict behavioural economic approach would be to make use of a so-called nudge, or any aspect of the choice architecture that alters an individual’s behaviour in a predictable way without forbidding any options or without substantially changing their economic incentives.10 Some interventions provide large amounts of money (figure 2) that can be as high as 50% of average monthly income, which clearly changes economic incentives. However, not all interventions have significant effects, nor are these effects only from the highest financial incentives (relative to the monthly income of individuals; figure 3). Economic interventions that are not primarily based on psycho logical processes for their effectiveness, are considered as traditional financial incentives rather than behavioural economics applications. Conditional cash transfers, for example, have the explicit target of changing economic conditions, and are therefore structural in nature. Although CEIs can include some non-monetary material rewards, such as vouchers (panel), behavioural economic approaches would explicitly consider non-financial nudges, such as social comparisons, a focus of the literature that is rapidly growing.57 Nevertheless, a few articles explicitly document routes for behaviour change that are based on established psychological theories.24,29,58 Building on these ideas and the results of previous related work,59 we present a conceptual framework that postulates the potential mechanisms or pathways for CEIs (figure 1) and briefly discuss each in more detail.
Figure 1:
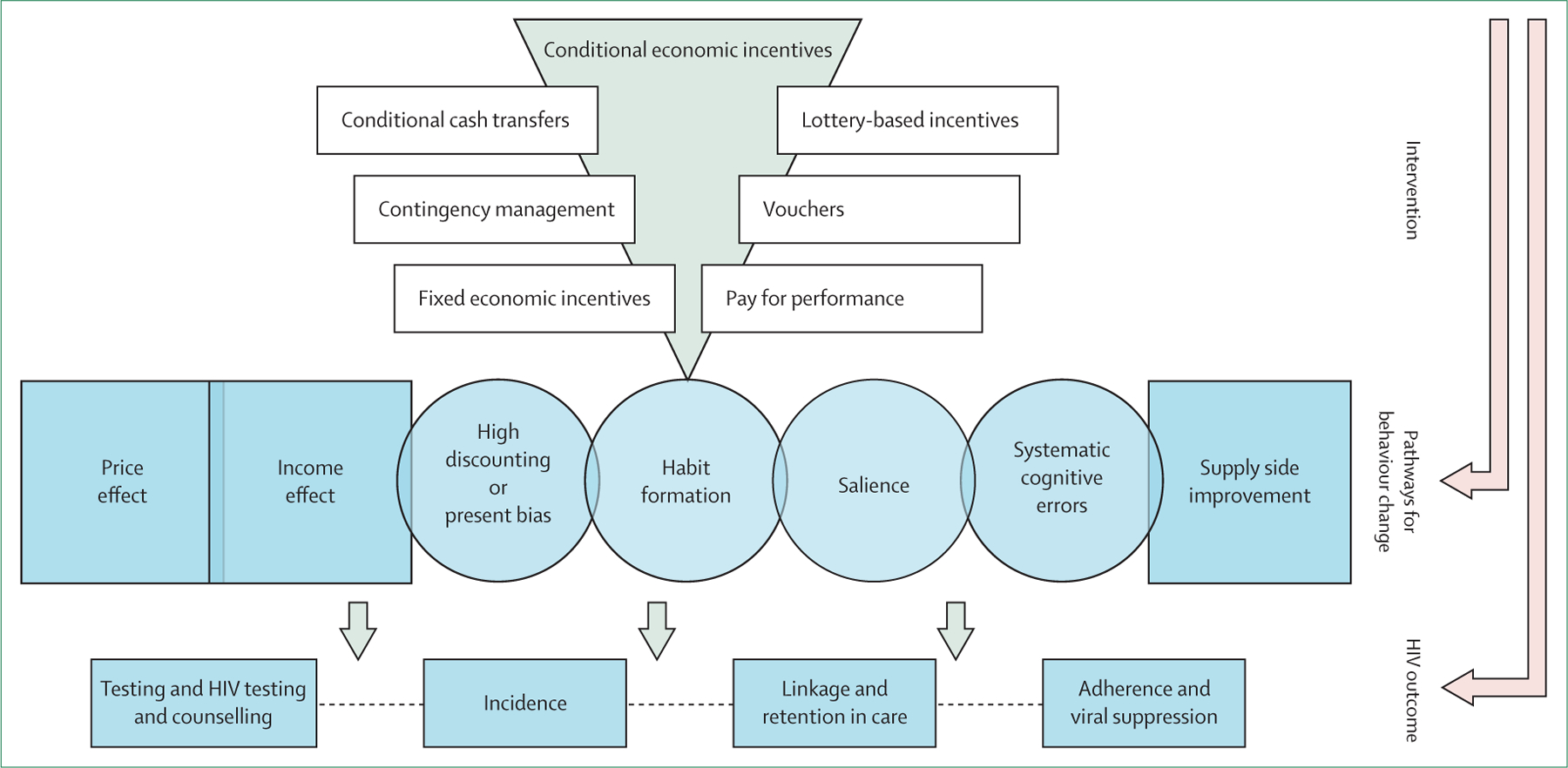
Pathways for behaviour change as a result of conditional economic incentives
Figure 2: Incentive amounts by HIV outcome and country (select studies).
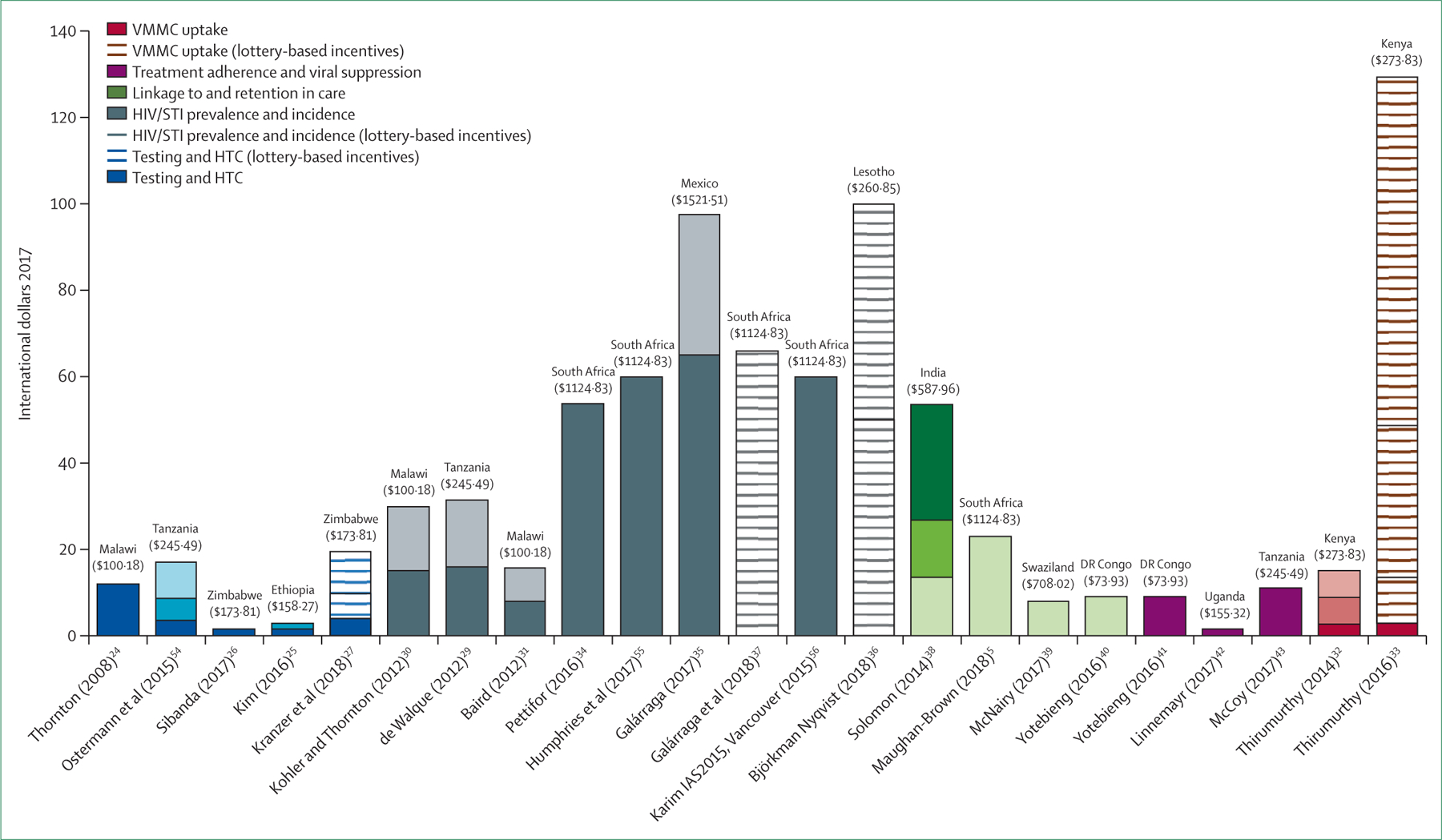
Conversions to international dollars are based on PPP exchange rates and consumer price index. Unless otherwise indicated, all incentive amounts are fixed. Amounts in parentheses are monthly gross domestic product (PPP) per capita. Information sourced from The World Bank Group, 2018 (https://data.worldbank.org/indicator/NY.GDP.PCAP.PP.CD?view=chart). HIV/STI=HIV or STI, or both. HTC=HIV testing and counselling. PPP=purchasing power parity. VMMC=voluntary medical male circumcision.
Figure 3: Significant effect sizes of economic incentives on HIV prevention and control (select studies).
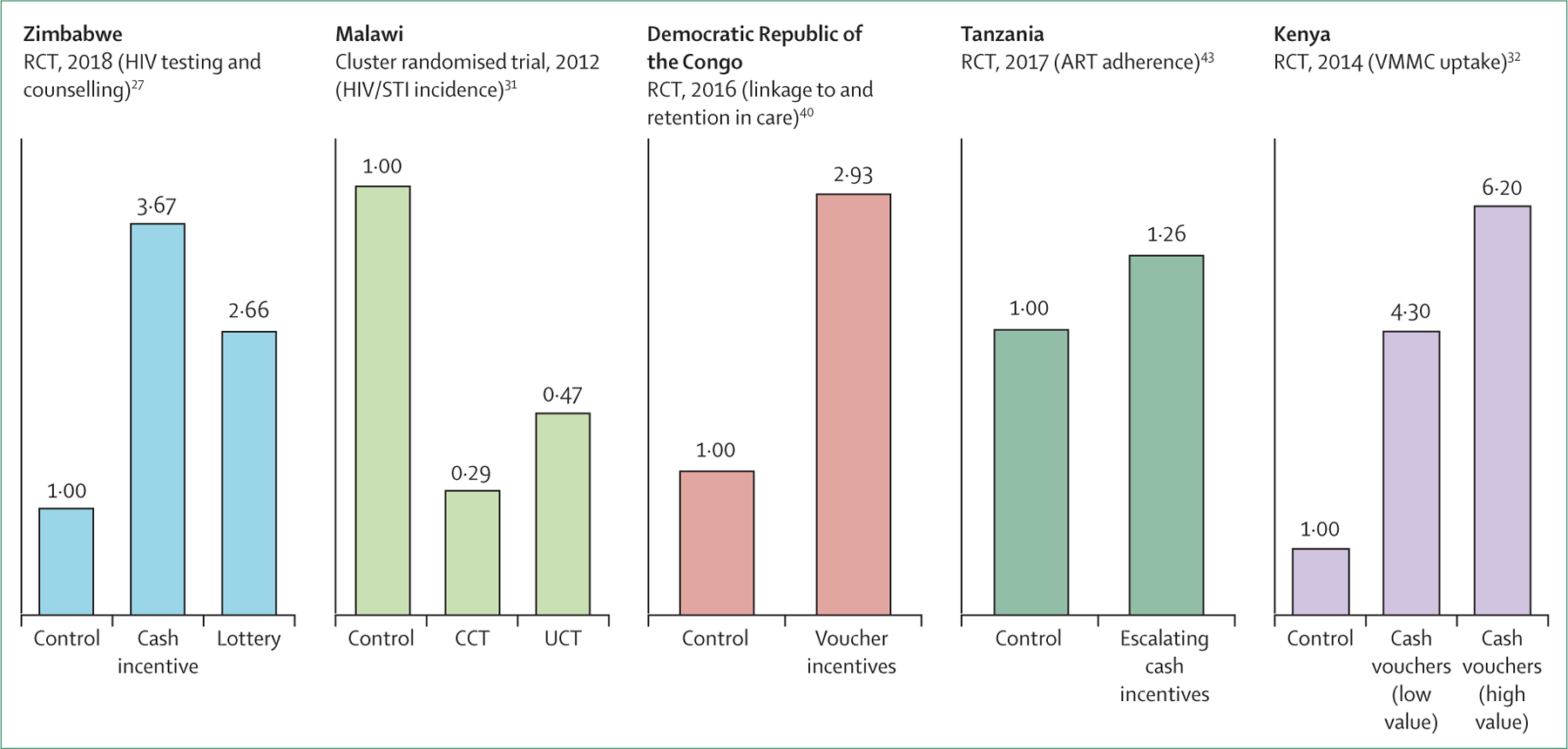
Significant effect sizes compared with the control group were observed in all studies. RCT=randomised controlled trial. HIV/STI=HIV or STI, or both. CCT=conditional cash transfer. UCT=unconditional cash transfer. ART=antiretroviral therapy. VMMC=voluntary medical male circumcision.
Demand side
Depending on the amount of money offered, economic incentives can operate through a so-called price effect, which posits that demand for a good or service changes as the price of that good or service varies.60 An incentive that is conditional on circumcision uptake, for example, can be seen as a reduction in the real price of VMMC because it helps to cover the cost of wage losses (for the few days of recovery time).33 Alternatively, a conditional incentive that is based on staying free of new curable STIs (as has been done in Tanzania29 and Mexico35,61,62) might be understood to increase the real price of risky sexual behaviours, since participants would stand to lose money if they acquired a new curable STI. Early economic analysis has highlighted the importance of considering both the availability and the real price (ie, the true price to consumers) of condoms for HIV prevention inclusive of potential private or public subsidies.63 Furthermore, the zero price model suggests that the intrinsic value of a good increases when the price is reduced to zero.64,65
Some CEI interventions can have a so-called income effect, which implies that consumers would buy more of a normal good or service if they had more income at their disposal.60 If the incentive amount was high (relative to the average earnings of the target population), then there can be a larger income effect, as the participants would have more money to spend (figure 2). Assuming HIV prevention and treatment are perceived as standard goods or services, people would theoretically buy more of these services if they had more money. Incentives might be more effective for people with fewer resources because, for them, even small incentives account for a large share of their income and could constitute a way of dealing with poverty-related barriers.66 This effect was noted in the Democratic Republic of the Congo, where the effects of the incentive on uptake of and retention in prevention of mother-to-child HIV transmission care were stronger among people of lower socioeconomic status.40 Conversely, risk behaviours could also be classified as a normal good, particularly among men. A study in Malawi found significant increases in risky sexual behaviours in men 1 week after they received a financial incentive,30 which shows that the unintended consequences of incentives need to be considered carefully.
After the most obvious aspects of incentives (price and income), people tend to consider timing. Individuals typically attach a greater value to consuming goods, services, or experiences in the present, compared with the value attached when consuming them in the future.67 Moreover, preferences might change over time, such that people prefer immediate gratification rather than delayed rewards.68,69 Incentives could help reduce these time biases, particularly for one-off interventions, such as HIV testing24–27 or male circumcision.33 People might engage in healthier behaviours because health-promoting CEIs can help address present-biased preferences, reduce pro crastination, and increase motivation.44 These potential channels or mediators should be tested further in future studies. The costs—including the logistical costs of transportation and lost time, and the psychological costs of fear or stigma—are often considered less important than the future benefits (eg, knowing their HIV status and initiating treatment). Incentives can reverse the relative weight of the costs and future benefits to individuals.27
Similar to timing, the duration of the effect is also an important factor. Most effective incentive interventions have short-term consequences that disappear after the incentives are stopped.4,35 This outcome seems to be the case even for cash transfers that are conditional on school attendance, which have longer duration effects for educational outcomes and some sexual risk behaviours.31,70,47 However, the effect of incentives on habit formation is debatable. For biomedical interventions, we would not expect the effects of the intervention to continue if we stopped the medication; similarly, perhaps we should not expect all effects of economic incentives to continue after they are removed. The premise of habit formation rests on the assumption that permanent behaviour change is possible, especially if the barriers to behaviour change are either psychological or due to a lack of knowledge.3 However, if barriers to behaviour change are logistical or financial (eg, needing money for transportation to a clinic visit), habit formation cannot rely on incentives alone. Incentives can play an important role at specific stages of the HIV care continuum, such as for testing, VMMC, early treatment initiation, or achieving initial viral suppression. Incentives might be better used to achieve behaviour change if they focused on reducing the constraints rather than increasing the driving forces.71
Incentives can encourage healthier alternatives, which is important because humans tend to make decisions on the basis of what is most salient.72 Nevertheless, previous studies have shown that effective behavioural interventions do not always need to involve economic incentives to increase salience. Interventions aimed at increasing salience could include physical reminders,73 non-monetary gifts, social recognition, public notices, product convenience, inspirational messaging, or regular reminders.17 For example, sending weekly mobile phone messaging reminders to take antiretroviral drugs to individuals with HIV in Kenya was found to be highly cost-effective.73 In Zambia, non-monetary rewards (in the form of publicly displayed stars in hair salons) were more effective at increasing condom purchases than monetary incentives, suggesting that social recognition might be more salient than financial rewards in particular contexts.59
Incentives can help people address cognitive biases. Most people do not understand the true risk of certain behaviours or choices that they face.74 Individuals tend to underestimate the risks they face and overestimate their chances of success.75 Even when the probabilities of outcomes are explained, most people do not have the capacity for intuitive computation.76 Therefore, CEIs might help people to understand the risks associated with their decisions. For example, in a South African township, the perceived risk of men having multiple sex partners, meeting sex partners in street bars, or having sex after drinking, was much higher than the self-reported frequency of those events in the community.77 Conversely, men can underestimate the prevalence of condom use in their community.77 Men can assume that people in their community engage in riskier and less protective behaviours than their self-reported behaviours. Incentives for repeated HIV testing combined with educational components, helped to address cognitive biases in Ethiopia, where there was a low (perceived) severity and susceptibility of a health problem.25
Supply side
Thus far, we have discussed the decisions of the consumers of HIV prevention and treatment services (the demand side), yet providers also clearly play a pivotal role and could also be incentivised. On the supply side, the idea of rewarding providers that offer HIV prevention and treatment services is known as performance-based payment or pay for performance. In Rwanda, a pay for performance intervention increased HIV testing among married individuals and for both partners in serodiscordant couples.78 Also in Rwanda, pay for performance increased the use and quality of several maternal and child health-care services (including HIV services), with larger effects observed for services in which facilities received larger financial incentives and for services over which providers had greater control.79 In Burundi, pay for performance also improved the quality of care for maternity and prenatal care services (including VCT and PMTCT).80 Similarly, health facilities in Malawi were rewarded if they reached performance targets, which reinforced adherence to treatment standards for maternal care (eg, for HIV testing in pregnancy).81 Importantly, pay for performance did not reduce the intrinsic motivation of health workers. Future research could reward clinical teams using a loss or regret framework, which would provide an incentive at the beginning of the year that providers would need to pay back if the goals are not achieved. This loss or aversion framework has shown success in the field of education.82 Similarly, more could be done to implement checklists and other quality-enhancement interventions in HIV prevention programming.83
Ethical considerations
Incentive-based interventions should be based on the most ethical practices that involve informed decision making, expanded choice, non-coercion, and human rights.84 Designing such interventions can support and empower people to achieve their own goals. For example, the Empower Nudge trial37 in South Africa gave lottery incentives to enrolled women who chose long-acting reversible contraception and who agreed to use condoms regularly, thus encouraging dual protection. The enrolled women had accepted dual protection before the study; therefore, the lottery incentives served only as an additional tool to empower and support them in fulfilling their intentions. Providing an incentive that is conditional on a biological outcome, such as HIV seroconversion, can be ethically problematic and might not be effective.30 Evidence should enable evaluation of the likely benefits, risks, burdens, and externalities associated with a conditionality, as well as the receptivity and ability of the participant to comply.85 Using this evidence, incentive programmes can be technically effective while also being ethical.86 A discussion about the ethical implications of providing relatively large amounts of an incentive (in relation to the earnings of the target population), or conversely the issue of underpayment, is largely absent from the medical literature (figure 3).87 Also, more studies are needed to identify the unintended effects of incentives—eg, although most male partners view receipt of incentives as beneficial for young women in South Africa, some relationships might be negatively affected if the woman was to receive more money than the man could earn.88
Future directions
There are several lines of novel research that have potentially important health policy implications (table). To build upon the results of these studies, we first need to integrate incentives that improve HIV testing and counselling as part of the first step in the HIV care continuum by combining incentives for home-based or facility-based HIV testing and counselling with HIV education to increase testing uptake in generalised epidemic settings, and by testing CEI programmes in key populations to increase testing yield and improve the use of available resources. Second, to improve HIV prevention, new research should focus on finding ways to effectively incentivise reductions in high-risk sexual behaviours (eg, concurrent partnerships and sexual intercourse without using a condom) and increases in protective activities (eg, condom use, dual protection, and frequent clinic visits). We should selectively scale up incentives in key populations that have previously shown adherence to the CEI interventions, and use fixed and lottery incentives combined with behavioural economic approaches in key populations to reduce HIV and STI incidence. Third, to increase linkage to care and ART initiation, future studies could investigate the effect of monetary and non-monetary vouchers compared with cash incentives. Also, escalating-fee schedules could be more effective for improving retention in care in populations with greater economic needs. Fourth, for research on treatment adherence and viral load suppression, future studies could provide vouchers or non-monetary material incentives conditional upon repeated demonstration of viral suppression. Finally, incentivising sustained viral suppression can become a form of so-called graduation, such that incentives will be used along the HIV care continuum, first to increase linkage to care and retention in care, and subsequently to decrease viral load and sustain viral load suppression.
Table:
Effect of different economic incentive types on HIV outcomes in completed and ongoing trials
| Target outcome(s) | Key findings | Future directions | |
|---|---|---|---|
| HIV testing and counselling | |||
|
|
|
|
| HIV prevention | |||
|
|
|
|
| Linkage to care and ART initiation | |||
|
|
|
|
| Retention in care, treatment adherence, and viral suppression | |||
|
|
|
|
ART=antiretroviral therapy. CCT=conditional cash transfer. CEI=conditional economic incentive. HTC=HIV testing and counselling. LIMCs=low-income and middle-income countries. MEMS=medical event monitoring system. MPR=medication possession ratio. PMTCT=prevention of mother-to-child transmission. STI=sexually transmitted infection. VMMC=voluntary medical male circumcision.
Supplementary Material
Panel: Conditional economic incentives: definition and examples.
Conditional economic incentives
Financial or other material rewards granted to individuals who accomplish a task or exhibit a specific behaviour that can be objectively monitored3–5
Interventions designed to address the factors that drive individual choices and behaviours in order to improve individual and population-level outcomes
For research that employs conditional economic incentives, the material reward is the critical component of the intervention
Types of conditional economic incentives include
Conditional cash transfers
Contingency management
Fixed economic incentives
Non-monetary (material) incentives
Lottery-based incentives
Vouchers
Pay for performance
Search strategy and selection criteria.
In January, 2019, and June, 2019, we searched the Cochrane Library, PubMed, Health Evidence, EconLit, ProQuest, and ClinicalTrials.gov using the PICO criteria: Patient/Population/Problem (HIV), Intervention (conditional incentives), Comparison (not receiving conditional incentives) and Outcome (HIV testing, HIV treatment, or biomarkers for HIV/sexually transmitted infection incidence or prevalence. The following intervention terms were included: “conditional cash transfers (CCT)”, “conditional economic incentives (CEI)”, “contingency management (CM)”, “financial incentives (FI)”, and “vouchers”. Articles published in English between Jan 1, 2000 and Dec 31, 2018 were considered. Publications were retained for review if they described randomised controlled trials conducted in low-income and middle-income countries (as classified by the World Bank), and they assessed the effect of conditional economic incentives on rates of HIV testing, the incidence and prevalence of HIV and STI co-infection and HIV treatment biomarkers. A total of 596 records were screened.
This review focused on low-income and middle-income countries, which continue to bear most of the prevalent and incident HIV cases. Some of the issues related to incentives and behavioural economics will be different in high-income countries. Because of the large volume of the literature, non-experimental evaluations were excluded from this review, but these evaluations constitute an important source of information relevant to policy that may warrant future review.
Acknowledgments
Roxana Rodríguez-Franco (National Institute of Public Health, Cuernavaca, Mexico) and Marta Wilson-Barthes (Brown University, Providence, RI, USA) provided excellent research assistance. Earlier versions of this paper were presented as a plenary speech at the International AIDS Society conference in Paris, France (July 23-26, 2017), and at the National Center for AIDS Research meetings in Atlanta, USA (Jan 28-29, 2019). This work was partially funded by grants from the National Institutes of Health (R34-MH114664; R21-AI-118393; R03-CA-188473) and was facilitated by the Providence/Boston Center for AIDS Research (P30-AI-042853). We are also grateful to the Population Studies and Training Center at Brown University, which also receives funding from the National Institutes of Health (P2C-HD-041020), for general support. Funders had no role in the design or writing of the manuscript, nor the decision to submit it for publication.
Footnotes
Declaration of interests
We declare no competing interests.
References
- 1.UNAIDS. Miles to go: closing gaps, breaking barriers, righting injustices. Geneva: Joint United Nations Programme on HIV and AIDS, 2018. [Google Scholar]
- 2.UNAIDS. Social protection: a fast-track commitment to end AIDS. Geneva: Joint United Nations Programme on HIV and AIDS, 2018. [Google Scholar]
- 3.Operario D, Kuo C, Sosa-Rubí SG, Galárraga O. Conditional economic incentives for reducing HIV risk behaviors: integration of psychology and behavioral economics. Health Psychol 2013;32: 932–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galárraga O, Genberg BL, Martin RA, Barton Laws M, Wilson IB. Conditional economic incentives to improve HIV treatment adherence: literature review and theoretical considerations. AIDS Behav 2013; 17: 2283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maughan-Brown B, Smith P, Kuo C, et al. A conditional economic incentive fails to improve linkage to care and antiretroviral therapy initiation among HIV-positive adults in Cape Town, South Africa. AIDS Patient Care STDS 2018; 32: 70–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamenica E. Behavioral economics and psychology of incentives. Annu Rev Econom 2012; 4: 427–52. [Google Scholar]
- 7.DellaVigna S. Psychology and economics: evidence from the field. J Econ Lit 2009; 47: 315–72. [Google Scholar]
- 8.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica 1979; 47: 263–92. [Google Scholar]
- 9.Read D, Van Leeuwen B. Predicting hunger: the effects of appetite and delay on choice. Organ Behav Hum Decis Process 1998;76: 189–205. [DOI] [PubMed] [Google Scholar]
- 10.Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth, and happiness. New York: Penguin Books, 2009. [Google Scholar]
- 11.Thaler RH. Misbehaving: the making of behavioral economics. New York: W W Norton & Company, 2016. [Google Scholar]
- 12.Kahneman D. Thinking, fast and slow. New York: Farrar, Straus and Giroux, 2011. [Google Scholar]
- 13.Rabin M. Psychology and economics. J Econ Lit 1998; 36: 11–46. [Google Scholar]
- 14.Camerer C, Loewenstein G, Rabin M. Advances in behavioral economics. New York: Russell Sage Foundation, 2004. [Google Scholar]
- 15.Kahneman D, Tversky A. Choices, values, and frames. New York: Russell Sage Foundation, 2000. [Google Scholar]
- 16.Rice T. The behavioral economics of health and health care. Annu Rev Public Health 2013; 34: 431–47. [DOI] [PubMed] [Google Scholar]
- 17.The World Bank. World development report 2015: mind, society and behavior. Washington, DC: The World Bank, 2015. [Google Scholar]
- 18.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA 2007; 298: 1900–10. [DOI] [PubMed] [Google Scholar]
- 19.Ranganathan M, Lagarde M. Promoting healthy behaviours and improving health outcomes in low and middle income countries: a review of the impact of conditional cash transfer programmes. Prev Med 2012; 55: S95–105. [DOI] [PubMed] [Google Scholar]
- 20.Swann M. Economic strengthening for HIV prevention and risk reduction: a review of the evidence. AIDS Care 2018; 30: 37–84. [DOI] [PubMed] [Google Scholar]
- 21.Swann M. Economic strengthening for HIV testing and linkage to care : a review of the evidence. AIDS Care 2018; 30: 85–98. [DOI] [PubMed] [Google Scholar]
- 22.Bassett IV, Wilson D, Taaffe J, Freedberg KA. Financial incentives to improve progression through the HIV treatment cascade. Curr Opin HIV AIDS 2015; 10: 451–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swann M. Economic strengthening for retention in HIV care and adherence to antiretroviral therapy: a review of the evidence. AIDS Care 2018; 30: 99–125. [DOI] [PubMed] [Google Scholar]
- 24.Thornton RL. The demand for, and impact of, learning HIV status. Am Econ Rev 2008; 98: 1829–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim H, Haile B, Lee T. Promotion and persistence of HIV testing and HIV/AIDS knowledge: evidence from a randomized controlled trial in Ethiopia. Health Econ 2016; 26: 1394–411. [DOI] [PubMed] [Google Scholar]
- 26.Sibanda EL, Tumushime M, Mufuka J, et al. Effect of non-monetary incentives on uptake of couples’ counselling and testing among clients attending mobile HIV services in rural Zimbabwe:a cluster-randomised trial. Lancet Glob Heal 2017; 5: e907–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kranzer K, Simms V, Bandason T, et al. Economic incentives for HIV testing by adolescents in Zimbabwe: a randomised controlled trial. Lancet HIV 2018; 5: e79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linnemayr S, MacCarthy S, Kim A, Giguere R, Carballo-Dieguez A, Barreras JL. Behavioral economics-based incentives supported by mobile technology on HIV knowledge and testing frequency among Latino/a men who have sex with men and transgender women: protocol for a randomized pilot study to test intervention feasibility and acceptability. Trials 2018; 19: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Walque D, Dow WH, Nathan R, et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open 2012; 2: e000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kohler HP, Thornton RL. Conditional cash transfers and HIV/AIDS prevention: unconditionally promising? World Bank Econ Rev 2012; 26: 165–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet 2012; 379: 1320–29. [DOI] [PubMed] [Google Scholar]
- 32.Thirumurthy H, Masters SH, Rao S, et al. Effect of providing conditional economic compensation on uptake of voluntary medical male circumcision in Kenya: a randomized clinical trial. JAMA 2014; 312: 703–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thirumurthy H, Masters SH, Rao S, et al. The effects of providing fixed compensation and lottery-based rewards on uptake of medical male circumcision in Kenya: a randomized trial. J Acquir Immune Defic Syndr 2016; 72: 309–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pettifor A, MacPhail C, Hughes JP, et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob Heal 2016; 4: e978–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galárraga O, Sosa-Rubí SG, Kuo C, et al. Punto Seguro: a randomized controlled pilot using conditional economic incentives to reduce sexually transmitted infection risks in Mexico. AIDS Behav 2017; 21: 3440–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Björkman Nyqvist M, Corno L, de Walque D, Svensson J. Incentivizing safer sexual behavior: evidence from a lottery experiment on HIV prevention. Am Econ J Appl Econ 2018; 10: 287–314. [Google Scholar]
- 37.Galárraga O, Harries J, Maughan-Brown B, et al. The Empower Nudge lottery to increase dual protection use: a proof-of-concept randomised pilot trial in South Africa. Reprod Health Matters 2018; 26: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Solomon SS, Srikrishnan AK, Vasudevan CK, et al. Voucher incentives improve linkage to and retention in care among HIV-infected drug users in Chennai, India. Clin Infect Dis 2014; 59: 589–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McNairy ML, Lamb MR, Gachuhi AB, et al. Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: the Link4Health cluster randomized trial. PLoS Med 2017; 14: 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yotebieng M, Thirumurthy H, Moracco KE, et al. Conditional cash transfers and uptake of and retention in prevention of mother-to-child HIV transmission care: a randomised controlled trial. Lancet HIV 2016; 3: e85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yotebieng M, Thirumurthy H, Moracco KE, et al. Conditional cash transfers to increase retention in PMTCT care, antiretroviral adherence, and postpartum virological suppression: a randomized controlled trial. J Acquir Immune Defic Syndr 2016; 72: S124–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Linnemayr S, Stecher C, Mukasa B. Behavioral economic incentives to improve adherence to antiretroviral medication. AIDS 2017;31: 719–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCoy SI, Njau PF, Fahey C, et al. Cash vs. food assistance to improve adherence to antiretroviral therapy among HIV-infected adults in Tanzania. AIDS 2017; 31: 815–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Czaicki NL, Dow WH, Njau PF, McCoy SI. Do incentives undermine intrinsic motivation? Increases in intrinsic motivation within an incentive-based intervention for people living with HIV in Tanzania. PLoS One 2018; 13: e0196616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thirumurthy H, Emperador D, Ndyabakira A, et al. Randomized controlled trial of financial incentives for achieving viral suppression. Conference on Retroviruses and Opportunistic Infections; Boston, Massachusetts, USA; March 4–7, 2018 (abstr 95). [Google Scholar]
- 46.Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. Q J Econ 2011; 126: 1709–53. [Google Scholar]
- 47.Baird S, Chirwa E, Hoop J De, Ozler B. Girl power: cash transfers and adolescent welfare: evidence from a cluster-randomized experiment in Malawi In: Edwards S, Johnson S, Weil DN. African successes, Vol II: Human capital . Chica: University of Chicago Press/National Bureau of Economic Research, 2016: 139–64. [Google Scholar]
- 48.WHO, UNAIDS. New data on male circumcision and HIV prevention: policy and programme implications. World Health Organization, 2007. https://www.who.int/hiv/pub/malecircumcision/research_implications/en/ (accessed Sept 9, 2019). [Google Scholar]
- 49.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 2007. 369: 643–56. [DOI] [PubMed] [Google Scholar]
- 50.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007. 369: 657–66. [DOI] [PubMed] [Google Scholar]
- 51.Sunstein CR, Thaler RH. Libertarian paternalism is not an oxymoron University of Chicago Public Law & Legal Theory Working Paper No. 43, University of Chicago, 2003. [Google Scholar]
- 52.Roberto CA, Kawachi I. Behavioral economics and public health. New York: Oxford University Press, 2015. [Google Scholar]
- 53.Bazant E, Mahler H, Machaku M, et al. A randomized evaluation of a demand creation lottery for voluntary medical male circumcision among adults in Tanzania. J Acquir Immune Defic Syndr 2016;72: S285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ostermann J, Brown DS, Mühlbacher A, Njau B, Thielman N. Would you test for 5000 shillings? HIV risk and willingness to accept HIV testing in Tanzania. Health Econ Rev 2015; 5: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Humphries H, Kharsany ABM, Leask K, Ntombela F, Abdul Karim Q. The impact of conditional cash transfers in reducing HIV in adolescent girls and boys (RHIVA): CAPRISA 007 matched pair, cluster randomised controlled trial In: Abdul Karim Q,Abdul Karim S, Baxter C, eds. The CAPRISA clinical trials: HIV treatment and prevention. Switzerland: Springer, Cham,2017: 77–89. [Google Scholar]
- 56.Abdool Karim Q on behalf of CAPRISA 007 Team. Impact of condital cash incentives on HSV-2 and HIV in rural high school students in South Africa. International AIDS Society (IAS) Meetings; Vancouver, Canada; July 19–22, 2015 (abstr TUAC0101LB). [Google Scholar]
- 57.Ashraf N, Bandiera O, Jack BK. No margin, no mission? A field experiment on incentives for public service delivery. J Public Econ 2014; 120: 1–17. [Google Scholar]
- 58.de Walque D, Dow WH, Medlin C, Nathan R. Stimulating demand for AIDS prevention: lessons from the RESPECT trial In: Edward S, Johnson S, Weil DN, eds. African successes, Vol II: Human capital. Chicago: University of Chicago Press/National Bureau of Economic Research; 2016: 85–112. [Google Scholar]
- 59.Linnemayr S. HIV prevention through the lens of behavioral economics. J Acquir Immune Defic Syndr 2015; 68: e61–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Parkin M. Microeconomics, 13th edn. London: Pearson Education Limited, 2018. [Google Scholar]
- 61.Galárraga O, Sosa-Rubí SG, González A, et al. The disproportionate burden of HIV and STIs among male sex workers in Mexico City and the rationale for economic incentives to reduce risks. J Int AIDS Soc 2014; 17: 19218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galárraga O, Sosa-Rubí SG, Infante C, et al. Willingness-to-accept reductions in HIV risks: conditional economic incentives in Mexico. Eur J Heal Econ 2014; 15: 41–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Philipson T, Posner RA. The microeconomics of the AIDS epidemic in Africa. Popul Dev Rev 1995; 21: 835–48. [Google Scholar]
- 64.Shampanier K, Mazar N, Ariely D. Zero as a special price: the true value of free products. Mark Sci 2007; 26: 742–57. [Google Scholar]
- 65.Ma H, Mo Z, Zhang H, Wang C, Fu H. The temptation of zero price: event-related potentials evidence of how price framing influences the purchase of bundles. Front Neurosci 2018; 12: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zullo AR, Caine K, Galárraga O. The dollars and sense of economic incentives to modify HIV-related behaviours. J Int AIDS Soc 2015; 18: 23–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Frederick S, Loewenstein G, O’Donoghue T. Time discounting and time preference: a critical review. J Econ Lit 2002; XL: 351–401. [Google Scholar]
- 68.Laibson D. Golden eggs and hyperbolic discounting. Q J Econ 1997; 112: 443–77. [Google Scholar]
- 69.O’Donoghue T, Rabin M. Doing it now or later. Am Econ Rev 1999; 89: 103–24. [Google Scholar]
- 70.Baird S, Mcintosh C, Özler B. When the money runs out: do cash transfers have sustained effects on human capital accumulation? Journal of Development Economics 2019; 140: 169–85. [Google Scholar]
- 71.Lewin K. A dynamic theory of personality: selected papers. New York: McGraw-Hill Book Company, 1935. [Google Scholar]
- 72.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science 1974; 185: 1124–31. [DOI] [PubMed] [Google Scholar]
- 73.Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS 2011; 25: 825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McNeil BJ, Pauker SG, Sox HCJ, Tversky A. On the elicitation of preferences for alternative therapies. N Engl J Med 1982;306: 1259–62. [DOI] [PubMed] [Google Scholar]
- 75.Camerer C, Lovallo D. Overconfidence and excess entry: an experimental approach. Am Econ Rev 2016; 89: 306–18. [Google Scholar]
- 76.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica 1979; 47: 263–92. [Google Scholar]
- 77.Carey KB, Scott-Sheldon LA, Carey MP, et al. Community norms for HIV risk behaviors among men in a South African township. J Behav Med 2011; 34: 32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.de Walque D, Gertler PJ, Bautista-Arredondo S, et al. Using provider performance incentives to increase HIV testing and counseling services in Rwanda. J Health Econ 2015; 40: 1–9. [DOI] [PubMed] [Google Scholar]
- 79.Basinga P, Gertler PJ, Binagwaho A, Soucat AL, Sturdy J, Vermeersch CM. Effect on maternal and child health services in Rwanda of payment to primary health-care providers for performance: an impact evaluation. Lancet 2011; 377: 1421–28. [DOI] [PubMed] [Google Scholar]
- 80.Rudasingwa M, Soeters R, Bossuyt M. The effect of performance-based financial incentives on improving health care provision in Burundi: a controlled cohort study. Glob J Health Sci 2015; 7: 15–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lohmann J, Muula AS, Houlfort N, De Allegri M. How does performance-based financing affect health workers’ intrinsic motivation? A self-determination theory-based mixed-methods study in Malawi. Soc Sci Med 2018; 208: 1–8. [DOI] [PubMed] [Google Scholar]
- 82.Fryer RG, Levitt SD, List J, Sadoff S. Enhancing the efficacy of teacher incentives through framing: a field experiment. 2012. https://scholar.harvard.edu/files/fryer/publications/enhancing-efficacy-teacher-incentives-through-framing-field-experiment (accessed Sept 9, 2019).
- 83.Gawande A. The checklist manifesto: how to get things right. New York: Metropolitan Books, 2009. [Google Scholar]
- 84.Office for Human Research Protections. The Belmont report: ethical principles and guidelines for the protection of human subjects of research. 1979. https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html (accessed Sept 9, 2019).
- 85.Devine EG, Waters ME, Putnam M, et al. Concealment and fabrication by experienced research subjects. Clin Trials 2013; 10: 935–48. [DOI] [PubMed] [Google Scholar]
- 86.Krubiner CB, Merritt MW. Which strings attached: ethical considerations for selecting appropriate conditionalities in conditional cash transfer programmes. J Med Ethics 2017; 43: 167–76. [DOI] [PubMed] [Google Scholar]
- 87.Brown B, Galea JT, Dube K, et al. The need to track payment incentives to participate in HIV research. IRB 2018; 40: 8–12. [PubMed] [Google Scholar]
- 88.Khoza MN, Delany-Moretlwe S, Scorgie F, et al. Men’s perspectives on the impact of female-directed cash transfers on gender relations: findings from the HPTN 068 qualitative study. PLoS One 2018;13: e0207654. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


