Abstract
Percutaneous access for treatment of renal pathologies is a minimally invasive modality, although it can present complications. Small bowel lesions are rare but correct diagnosis and management are essential to prevent major complications. A patient submitted to an uncomplicated percutaneous nephrolithotomy presented jejunal transfixing perforation with a stable clinical progression. It was first managed conservatively unsuccessfully. Therefore, a laparotomy with enterectomy was necessary, with a favorable outcome. In transfixing lesions of the small bowel, diagnosis may be difficult and delayed. This contributes to conservative management failures and the requirement of laparotomy with enterectomy in order to reduce further complications.
Keywords: Jejunal perforation, Percutaneous nephrolithotomy, Percutaneous renal surgery, Small bowel perforation, Small bowel transfixing lesion
Introduction
Percutaneous access for the treatment of renal pathologies is a minimally invasive therapy with proven efficacy. However, it can present complications, such as bleeding, infection, and damage to structures adjacent to the kidneys (lung, spleen, liver, gallbladder, and intestine). Small bowel lesions are rare, but they can occur and lead to infectious complications as a result of peritoneal contamination. Further, if undiagnosed or not properly treated, those lesions can lead to the patient's death.1
Case presentation
Our case involves a 21-year-old female patient having a prior history of renal lithiasis with a complicated evolution that progressed into pyelonephritis and double-J stent implantation. A Computed Tomography (CT) showed a 2.3 cm pyelic stone with mild hydronephrosis in the left kidney and an indication for percutaneous nephrolithotomy (PCNL).
Surgery was performed with the patient under general anesthesia in a supine position. The puncture was guided by radioscopy in the left inferior calyx. Renal access was performed with sequential dilators of up to 30 Fr, with increased resistance in transposition close to the kidney. Intraoperative nephroscopy showed no anatomical changes; the stone was identified and completely fragmented with an ultrasonic lithotripter. Pyelography at the end of the procedure showed a slight contrast leakage near the renal pelvis, and double-J stenting and nephrostomy catheter maintenance were undertaken.
The patient presented localized pain on the left flank during the first postoperative day (POD), with no signs of peritonitis. On the third POD there was peri-nephrostomy enteric secretion leakage with pain persistantion. Antibiotic therapy (Ceftriaxone and Metronidazole) was initiated and an abdominal CT showed pneumoperitoneum, with the nephrostomy catheter properly located in the excretory route. No intraperitoneal collection was found but there was suspicion of jejunal loop transfixation in its skin-kidney path. Therefore, contrast was injected through the nephrostomy catheter in order to relocate it in the suspected compromised bowel lumen. However, there was resistance in the catheter traction and radioscopy showed no image that suggested intestinal lumen. The catheter was kept as a cavity drain and a new CT was programmed.
The exam on the fourth POD showed the absence of intra-abdominal collection and the catheter tip with its balloon inside the peritoneal cavity, reinforcing the suspicion of jejunum transfixation. A new attempt was made to relocate the catheter through traction concomitant with contrast injection, and this time the intestinal lumen was identified (Fig. 1). Since the patient remained clinically stable with low-output drainage of fecaloid content, it was decided to gradually remove the catheter in order to create a drainage tract (directed fistula) as well as to maintain antibiotic therapy and implement fasting and parenteral nutrition.
Fig. 1.
Radiography with contrast injection through nephrostomy catheter showing contrast in the small bowel.
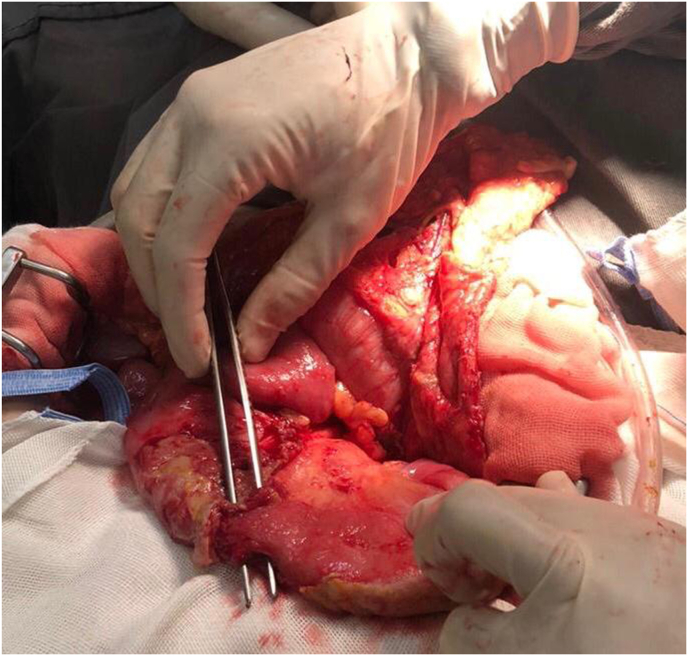
On the thirteenth POD an exploratory laparoscopy was performed as the patient was still presenting moderate abdominal pain. Jejunum transfixation was identified with the probe tip inside the intestinal lumen, blocking the perforation site. Therefore, was decided to do an exploratory laparotomy with drainage of the peritoneal cavity and enterectomy with primary anastomosis. The patient presented satisfactory progress which led to resolution of the case (Fig. 2).
Fig. 2.
Intraoperative (laparotomy) photography showing transfixing jejunum lesion.
Discussion
Ascending and descending segments of the colon are more affected by accidental injuries during percutaneous renal access when compared to small intestine due to their close proximity to the kidneys.2 There are two possible explanations for transfixed lesions of the ileum and jejunum: one is their retrorenal position (which can cause their perforation during percutaneous access before reaching the kidney) and the other is their anteromedial location in relation to the renal pelvis (which can inadvertently be perforated during manipulation of the right kidney).
As colonic injuries are more frequent, there is awell-established procedure with conservative management facilitated by the retroperitoneal location. In cases of intraoperative diagnosis, a conservative approach is proposed using the same concepts as controlled fistula. It is important to have adequate drainage of the affected cavity and structures to insure the absence of distal obstruction and local disease and to implement total parenteral nutrition with broad spectrum antibiotic therapy. If there is intraperitoneal perforation, peritonitis, sepsis, or failure in conservative management, an open surgical exploration should be performed and a colostomy is usually necessary.3 Conservative management, when possible, is an attractive choice since it avoids a new surgical procedure. However, delaying a necessary surgical procedure increases the risk of contamination, septicemia, and death.
In a literature review of patients with gastrointestinal injury due to percutaneous renal access, only six cases of jejunum involvement have been described. In the majority of them (five) there was loop transfixation. In one of these cases, diagnosis occurred intraoperatively at the end of the procedure when the loop was visualized with contrast. This allowed adoption of conservative treatment with directed fistula. In the other cases, the diagnosis occurred later, between 24 and 120 hours after the procedure. All patients were submitted to laparotomy with enterectomy and primary anastomosis with good results.4
In the current study, the fact that the patient did not present signs of peritonitis and that there was no suspicion of intraoperative injury led to a delayed diagnosis. The CT had an important role in suggesting transfixed jejunal injury in the two times this was done (Fig. 3). The option to maintain a conservative approach was based on the absence of intra-peritoneal collection and the patient's stable condition. The nephrostomy catheter had been maintained since PNL and prevented gross fecal leakage as well as obstruction of the jejunum, which explains the delayed diagnosis and oligosymptomatic presentation of the case.
Fig. 3.
Computed tomography showing nephrostomy catheter transfixing the small bowel.
Conclusion
Injury to the jejunum during percutaneous renal access is rare, with transfixation of the loop being the most frequent presentation. If not diagnosed intraoperatively, laparotomy with enterectomy is the recommended procedure.
Declaration of competing interest
No competing financial interests exist.
Acknowledgements
None.
Contributor Information
Victor S.S. Fanni, Email: victor_fanni@hotmail.com.
Lucas de O. Ramos, Email: ramoslucas_kta2@hotmail.com.
Marcela C. Leite, Email: urologiaufjf@gmail.com.
Felipe U.P. Martins, Email: felipeuchoap@gmail.com.
Paulo Roberto C. Júnior, Email: paulorcajr@yahoo.com.br.
Humberto E. Lopes, Email: lopesh@terra.com.br.
References References
- 1.Oztürk H., Onen A., Otçu S. Diagnostic delay increases morbidity in children with gastrointestinal perforation from blunt abdominal trauma. Surg Today. 2003;33(3):178–182. doi: 10.1007/s005950300040. [DOI] [PubMed] [Google Scholar]
- 2.Michel M.S., Trojan L., Rassweiler J.J. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 3.Maghsoudi R., Etemadian M., Kashi A.H. Management of colon perforation during percutaneous nephrolithotomy: 12 Years of experience in a referral center. J Endourol. 2017 Oct;31(10):1032–1036. doi: 10.1089/end.2017.0379. [DOI] [PubMed] [Google Scholar]
- 4.Öztürk H. Gastrointestinal system complications in percutaneous nephrolithotomy: a systematic review. J Endourol. 2014;28(11):1256–1267. doi: 10.1089/end.2014.0344. [DOI] [PubMed] [Google Scholar]