Abstract
Disparities that impact equity in access to kidney transplantation for patients with kidney failure have been well described. Many robust clinical trials have tested the effectiveness of interventions to reduce disparities and equilibrate access to kidney transplantation. Moreover, policy changes have been enacted to achieve the same aims. Despite these efforts, rates of kidney transplant wait listing within the first year of end-stage kidney disease have remained unchanged over the past two decades, while incident rates of end-stage kidney disease have climbed. Since prior interventions have not durably increased transplant access, disruptive change is clearly needed. The Advancing American Kidney Health Executive Order sets bold goals to transform kidney care for patients and caregivers. In this spirit, we discuss an Opt Out for Transplant Referral Model as a compelling solution to improve equity in access to kidney transplantation.
Viewpoint:
Kidney transplantation is cost effective, improves patient’s quality of life and provides a survival benefit relative to maintenance dialysis.1,2,3 The benefits of transplantation extend to patients with comorbid conditions and among patients receiving relatively high risk donor organs.4,5 Highly prevalent racial, ethnic, gender, geographic and socioeconomic disparities impact equitable access in kidney transplant. In addition, evidence from the U.S. and Canada has documented substantial variability in referral rates for kidney transplantation among dialysis facilities (from 0–100%), and higher rates of waitlisting among those facilities with higher referral, suggesting there are many ESKD patients that may be eligible for kidney transplantation but have not yet been referred.6,7 Improving access to the kidney transplant waiting list remains a prominent challenge for the nephrology and transplant communities.8,9,10
Numerous interventions have attempted to attenuate disparities in transplantation access, including peer navigation, mobile decision aids, telemedicine, and targeted education among dialysis facility staff, with varying effectiveness. 11,12,13 Despite these interventions, national rates of placement on the waiting list among patients with lower historic rates of transplantation have not increased. Targeted policy interventions contained in the 2014 changes to the kidney allocation system have improved transplant access among racial minorities, whom are placed on the kidney transplant waiting list.14,15,16 In addition Medicaid expansion enabled by implementation of the Affordable Care Act has increased pre-emptive waitlisting for kidney transplant even among minorities. But, it is unclear whether these changes are sustainable.17,18,19
Despite policy reforms and attempted interventions, profound disparities in access to transplantation remain. Based on national data from the United States Renal Data Services, the proportion of patients with End Stage Kidney Disease (ESKD) that are either placed on the waiting list, receive a living or deceased donor transplant within one-year of diagnosis has remained approximately 15% for the past 20 years.20 This wait listing rate has remained stagnant despite increased incidence of ESKD and is unrelated to organ supply.20 (Fig 1) In aggregate, the cumulative effect of numerous targeted interventions and policy reforms have failed to eliminate inequities in the kidney transplantation . This deflating indictment of the ineffectiveness of these multimodal strategies is indicative of how pernicious these healthcare disparities are in our health system, and the formidable steps required for improving processes of care. Transformative approaches for highly effective system-wide change and disruption are urgently needed.
Figure 1.
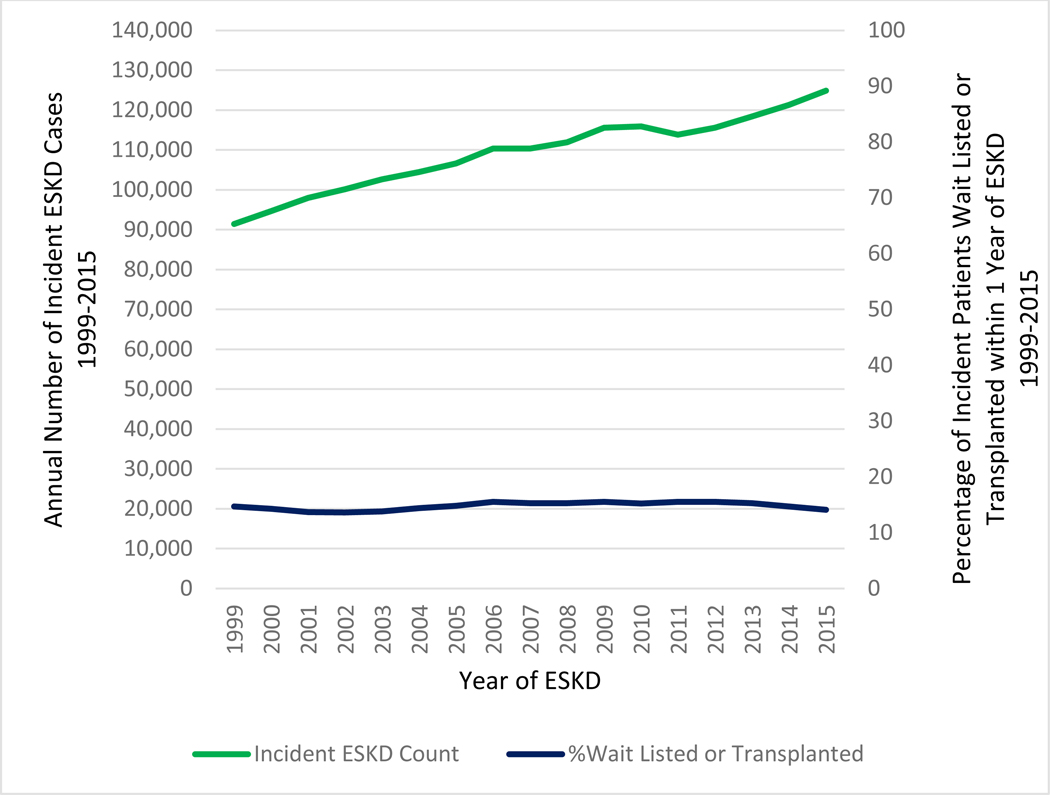
Proportion of Patients either Placed on the Waiting List or Received a Living or Deceased Donor Transplant within One Year of End Stage Kidney Disease and Annual Number of Incident Patients with End Stage Kidney Disease
The impact of large scale quality improvement efforts and other interventions to increase kidney transplant wait listing are limited by many factors. Dialysis unit ownership creates unintended, perverse incentives that reduce transplant referral .21,22 To date, quality oversight for transplant largely address “downstream” factors (e.g. 1 year patient and graft survival) rather than metrics that focus on “upstream” events (e.g. referral, evaluation, and wait listing for candidates).23 Moreover, few incentives exist to implement and sustain promising interventions that have shown efficacy in improving access to transplantation. Finally, there is no national level data collection on the pivotal periods capturing referral, evaluation start and reasons for wait listing decisions among those evaluated, limiting the ability to rigorously investigate mechanisms of disparity, measure quality, or share best practices beyond limited regional examples.24
For all of these reasons, the current dysfunctional status for improving access to care provides an impetus for a more radical transformation of the process to identifying and caring for patients. These include many patients that have clear potential benefits from transplantation but for numerous reasons never reach the crucial step of a transplant evaluation and are never captured in national transplant system reporting.25 We propose a fundamental shift in the paradigm for providing access to care for ESKD patients in the form of an Opt Out for Transplant Referral Model. This model is based upon the conceptual framework for equity in health and healthcare, and that the ethical treatment of patients requires a foundational paradigm of fairness or justice.26,27 In this system, patients are automatically referred to a transplant center for evaluation if they meet basic eligibility criteria developed by the transplant community. For incident patients, the referral can be made at the time that the Medicare 2728 form (indicating initiation of maintenance dialysis) is filed. Patients would be systematically referred to centers unless they opt out, explicitly declaring lack of interest in the procedure after being given information on the referral and transplant process. In this system, the transplant referrals originate from the nephrology clinics or dialysis facilities and, as is current practice, are determined by patient choice (e.g., transplant center proximity to their home) or the nephrology provider choice (e.g., those that have existing relationships with transplant centers may choose to refer their patients to that particular location). This toggling of default settings for care (e.g. setting electronic defaults rather than manual referrals for cardiac rehabilitation in patients who suffer from myocardial infarction to improve rates of program participation) has demonstrated marked effects on the use of effective healthcare interventions.28 Creating the default as transplant referral stands to improve access to information about the procedure and ultimately health outcomes for patients with ESKD.29,30
There are several compelling benefits of this model that are important to consider. The model would markedly increase the number of referrals by altering the narrative regarding who is or is not viable for transplantation and reducing the heterogeneity in determining appropriateness for transplant by provider. An opt-out system should also attenuate existing disparities associated with disproportionate timeliness and actual referral to transplantation given a systematic process. We would be able to understand if appropriate patients in dialysis units are not actually referred because of existing biases in referral practices that are well described.31,32 Furthermore, we would be able to quantify the actual number of patients with ESKD who may benefit from transplantation and provide objective information regarding the number of patients evaluated and considered as candidates. Based on the number of patients on the national waiting list today, it is likely that our current referral system grossly underestimates the eligible population. Prior single center or small regional studies have estimated that >50% of ESKD patients are eligible for kidney transplantation33,34, and yet fewer than 18% of U.S. ESKD patients are waitlisted nationally.20
There are also legitimate obstacles for application of this Opt-Out model. Certainly, this model would increase the transplant center workload. The onus of follow-up by transplant centers would include initial adjudication of referrals, a screening of all referred patients for absolute contraindications, and calling potential candidates to initiate the transplant evaluation. Many centers already determine candidate eligibility without in person visits (e.g., by reviewing their referral form). An ideal opt-out transplant referral system would permit such screening procedures to reduce the clinical burden on transplant centers, however, this may still necessitate additional resources and personnel. Larger, health system-level changes would need to be made to facilitate this proposal, including reimbursements to transplant centers for a clinical review of each referred patient or opportunities for telemedicine to screen some patients before they start the transplant evaluation process within a transplant center. However, an important benefit of this model, and a way to avoid excessive referrals, would be to allow centers’ to codify their selection criteria and make these publicly available to referring providers and patients for use in their choice of a center. Currently, the relative contraindications for transplant eligibility vary substantially by transplant center, yet are opaque to patients and referring caregivers.35,36 In this model, centers would need to transparently define their criteria and provide information regarding opportunities for candidacy and thus, improve informed decision making while ensuring equity in the process. In an effort to improve the imbalance in organ supply and demand, the Opt Out for Transplant Referral Model may also be an opportunity for pairing education about living donor transplant and increased risk donors (e.g high KDPI) at the dialysis facilities and transplant centers to increase potential acceptance of these organs.
The Opt Out for Transplant Referral Model could also incorporate innovative technologies and use health information systems to disrupt our “manual” referral system in exchange for a more automated one. Leveraging application programming interfaces and cloud based applications to connect patient medical records across nephrology providers (dialysis to transplant centers) may lessen the strain on transplant center staff time.37 Machine learning algorithms could automate matching of individual transplant center criteria for candidacy with patient characteristics, add efficiencies to the referral process and allow for systematic assessments of eligibility using objective longitudinal data.38
The potential net results of this innovation would be to reduce financial disincentives for transplant referral, provide a more streamlined pathway for vulnerable populations, and attenuate disparities among those who are and are not referred. Although the policy may not eliminate all disparities, every patient with ESKD (without an absolute contraindication) would be entitled to a conversation with a transplant center as a standard of care. Most importantly, the Opt Out for Transplant Referral Model creates equity in access to transplant by removing well documented systematic biases when referral has been left up to providers in CKD clinics and dialysis facilities.
The time for implementation of the Opt Out for Transplant Referral Model is now, and could be paired with initiatives to meet mandates in the Advancing American Kidney Health Executive Order and efforts to increase organ availability for those who need a transplant.39 Reforms to increase access to transplant will engage many stakeholders in the kidney community including living donor programs and advocacy groups as well as organ procurement organizations. Incremental gains in organ supply and reduction in discard rates may be expected as proposed objective outcome measures are applied at the level of organ procurement organizations.40 Systematic engagement and open communication between dialysis facilities and transplant centers fits well into the scope of improving kidney health for patients in the United States. Payment models for transplantation centers, nephrologists and dialysis providers will need to be reviewed in order to align incentives across the health care system to optimize outcomes for all patients.41 National data about the pre- wait listing phase in transplant will become available and transparency among centers could facilitate sharing best practices across the nation. We submit that incremental steps to improve access to care and attenuate disparities in care for transplant patients have predominantly not been effective in reducing inequities in the transplant process, and the lack of progress has left patients to suffer the consequences. The time for a transformative shift in the process for caring for patients with ESKD is now and the field of transplantation can leverage this opportunity to improve care for all those who may benefit. We acknowledge that the Opt Out for Transplant Referral Model will not necessarily immediately result in more transplants, but growth of the waiting list and possibly longer waiting times. However, it does hold the potential to get a more accurate count of the true magnitude of patients that can benefit for transplant and stimulate efforts to increase the organ supply through an opt-out system for organ donation, or, more living donor transplants, while ensuring equity is prioritized. The nephrology and transplant community needs to rally around a bold idea to disrupt and address the fundamental problems of the current system. Despite its challenges, it is the right thing to do.
Footnotes
Disclosures:
The authors have no conflicts to disclose as described by the American Journal of Transplantation.
Data Availability:
These data were derived from the following resources available in the public domain: United States Renal Data System. 2018 USRDS annual data report: Epidemiology of kidney disease in the United States. [https://www.usrds.org/2018/view/Default.aspx]
References:
- 1.Loubeau PR, Loubeau JM, Jantzen R. The economics of kidney transplantation versus hemodialysis. Prog Transplant. 2001;11(4):291–97. [DOI] [PubMed] [Google Scholar]
- 2.Evans RW, Manninen DL, Garrison LP Jr, et al. The quality of life of patients with end-stage renal disease. N Engl J Med. 1985;312(9):553–59. [DOI] [PubMed] [Google Scholar]
- 3.Port FK, Wolfe RA, Mauger EA, et al. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA. 1993;270(11):1339–43. [PubMed] [Google Scholar]
- 4.Massie AB, Luo X, Chow EK, et al. Survival benefit of primary deceased donor transplantation with high-KDPI kidneys. Am J Transplant. 2014;14(10):2310–16. [DOI] [PubMed] [Google Scholar]
- 5.Jay CL, Washburn K, Dean PG, et al. Survival Benefit in Older Patients Associated With Earlier Transplant With High KDPI Kidneys. Transplantation. 2017;101(4):867–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patzer RE, McPherson L, Wang Z, et al. Dialysis facility referral and start of evaluation for kidney transplantation among patients treated with dialysis in the Southeastern United States. Am J Transplant. 2020;00:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim SJ, Gill JS, Knoll G, et al. Referral for kidney transplantation in Canadian provinces. J Am Soc Nephrol. 2019;30(9):1708–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander GC, Sehgal AR. Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA. 1998;280(13):1148–52. [DOI] [PubMed] [Google Scholar]
- 9.Joshi S, Gaynor JJ, Bayers S, et al. Disparities among Blacks, Hispanics, and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation. 2013;95(2):309–18. [DOI] [PubMed] [Google Scholar]
- 10.Schold JD, Gregg JA, Harman JS, et al. Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol. 2011;6(7):1760–7. [DOI] [PubMed] [Google Scholar]
- 11.Patzer RE, Paul S, Plantinga L, et al. A Randomized Trial to Reduce Disparities in Referral for Transplant Evaluation. J Am Soc Nephrol. 2017;28(3):935–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sullivan CM, Barnswell KV, Greenway K, et al. Impact of Navigators on First Visit to a Transplant Center, Waitlisting, and Kidney Transplantation: A Randomized, Controlled Trial. Clin J Am Soc Nephrol. 2018;13(10):1550–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu M, Petgrave-Nelson L, Smith KD, et al. Transplant Center Patient Navigator and Access to Transplantation among High-Risk Population: A Randomized, Controlled Trial. Clin J Am Soc Nephrol. 2018;13(4):620–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melanson TA, Hockenberry JM, Plantinga L, et al. New Kidney Allocation System Associated With Increased Rates Of Transplants Among Black And Hispanic Patients. Health Aff. 2017;36(6):1078–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stewart DE, Kucheryavaya AY, Klassen DK, et al. Changes in Deceased Donor Kidney Transplantation One Year After KAS Implementation. Am J Transplant. 2016;16(6):1834–47. [DOI] [PubMed] [Google Scholar]
- 16.Hart A, Gustafson SK, Skeans MA, et al. OPTN/SRTR 2015 Annual Data Report: Early effects of the new kidney allocation system. Am J Transplant. 2017;17 Suppl 1:543–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harhay MN, McKenna RM, Harhay MO. Association Between Medicaid Expansion Under the Affordable Care Act and Medicaid-Covered Pre-emptive Kidney Transplantation. J Gen Intern Med. 2019;34(11):2322–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harhay MN, McKenna RM, Boyle SM, et al. Association between Medicaid Expansion under the Affordable Care Act and Preemptive Listings for Kidney Transplantation. Clin J Am Soc Nephrol. 2018;13(7):1069–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goyal N and Weiner DE. The Affordable Care Act, Kidney Transplant Access, and Kidney Disease Care in the United States. Clin J Am Soc Nephrol. 2018;13(7): 982–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Renal Data System. 2018 USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2018. [Google Scholar]
- 21.Garg PP, Frick KD, Diener-West M, et al. Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med. 1999;341(22):1653–60. [DOI] [PubMed] [Google Scholar]
- 22.Gander JC, Zhang X, Ross K, et al. Association Between Dialysis Facility Ownership and Access to Kidney Transplantation. JAMA. 2019;322(10):957–973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schold JD, Patzer RE, Pruett TL, et al. Quality Metrics in Kidney Transplantation: Current Landscape, Trials and Tribulations, Lessons Learned, and a Call for Reform. Am J Kid Dis, 2019;74(3):382–89. [DOI] [PubMed] [Google Scholar]
- 24.Patzer RE and McPherson L. Variation in Kidney Transplant Referral: How Much More Evidence Do We Need To Justify Data Collection on Early Transplant Steps? J Am Soc Nephrol. 2019;30(9):1554–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schold JD, Srinivas TR, Kayler LK, et al. The overlapping risk profile between dialysis patients listed and not listed for renal transplantation. Am J Transplant. 2008;8(1):58–68. [DOI] [PubMed] [Google Scholar]
- 26.Ramos HC, McCauley J (2018) Ethical Issues in Organ Transplantation In: Ramirez C, McCauley J (eds) Contemporary Kidney Transplantation. Organ and Tissue Transplantation. Springer, Cham; 343–53. [Google Scholar]
- 27.Braveman P and Gruskin S. Defining equity in health. J Epidemiol Community Health 2003;57:254–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel MS, Volpp KG, Asch DA. Nudge Units to Improve the Delivery of Health Care. N Engl J Med. 2018;378(3):214–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davidai S, Gilovich T, and Ross LD. The meaning of default options for potential organ donors. Proc Natl Acad Sci USA. 2012;109(38):15201–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med 2007; 357:1340–44. [DOI] [PubMed] [Google Scholar]
- 31.Tandon A, Wang M, Roe KC, et al. Nephrologists’ likelihood of referring patients for kidney transplant based on hypothetical patient scenarios. Clin Kidney J. 2016;9(4):611–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tong A, Hanson CS, Chapman JR, et al. The preferences and perspectives of nephrologists on patients’ access to kidney transplantation: as systematic review. Transplantation. 2014. 98(7):682–91. [DOI] [PubMed] [Google Scholar]
- 33.Kabbali N, Mikou S, El Bardai G, et al. Eligibility for renal transplantation: A Moroccan interregional survey. Saudi J Kidney Dis Transpl 2015;26:153–60. [DOI] [PubMed] [Google Scholar]
- 34.Kianda MN, Wissing KM, Broeders NE, et al. Ineligibility for renal transplantation: prevalence, causes and survival in a consecutive cohort of 445 patients. Clin Transplant 2011;25:576–83. [DOI] [PubMed] [Google Scholar]
- 35.Crenesse-Cozien N, Dolph B, Said M, et al. Kidney Transplant Evaluation: Inferences from Qualitative Interviews with African American Patients and their Providers. J Racial Ethn Health Disparities. 2019;6(5):917–25. [DOI] [PubMed] [Google Scholar]
- 36.Pham PT, Pham PA, Pham PC, et al. Evaluation of adult kidney transplant candidates. Semin Dial. 2010;23(6):595–605. [DOI] [PubMed] [Google Scholar]
- 37.Rucker DW. Implementeing the Cures Act—bringing consumer computing to healthcare. N Engl J Med. 2020. March 11 . [DOI] [PubMed] [Google Scholar]
- 38.Rajkomar A, Dean J, and Kohane I. Machine learning in medicine. N Engl J Med. 2019;380:1347–58. [DOI] [PubMed] [Google Scholar]
- 39.Executive order 13879 Advancing American Kidney Health from the Federal Register website. https://www.federalregister.gov/documents/2019/07/15/2019-15159/advancing-american-kidney-health. July 10, 2019. Accessed January 6, 2020.
- 40.Organ Procurement Organizations (OPO) Conditions for Coverage Proposed Rule: Revisions to outcome measures for OPOs website. https://www.cms.gov/newsroom/fact-sheets/organ-procurement-organization-opo-conditions-coverage-proposed-rule-revisions-outcome-measures-opos. Accessed April 20, 2020.
- 41.Mehrotra R Advancing American Kidney Health: An Introduction. Clin J Am Soc Nephrol. 2019;14(12):1788. [DOI] [PMC free article] [PubMed] [Google Scholar]


