Abstract
Objective
Emotional or psychological pain is a core symptom of complicated grief (CG), yet its correlates are largely unexamined among bereaved individuals.
Method
Bereaved adults (N=135) completed self-reports regarding psychological pain, CG, depression, and suicidality. We assessed correlations among these variables and tested whether psychological pain was elevated among individuals with CG and individuals with current or past suicidal thoughts and behaviors. Using logistic regression, we also assessed psychological pain, depression, and CG symptom severity as predictors of suicide risk.
Results
Psychological pain was strongly associated with both CG and depression severity and was elevated among subjects reporting current or past suicidality. CG and depression were not statistically significant predictors of suicidal ideation after accounting for the effects of psychological pain.
Conclusions
Psychological pain is strongly associated with bereavement-related psychopathology and warrants further investigation in studies examining the nature and treatment of CG.
Keywords: Emotional pain, Psychological pain, Bereavement, Grief, Depression, Suicide
In the mid-20th century, grief researchers began to systematically describe the mental and physical experiences that accompany bereavement (Granek, 2010). In these early descriptive accounts, there is frequent reference to feelings of pain in those who had experienced the death of a loved one. Lindemann (1944, p. 155) observed recurrent “waves of somatic distress” and “intense […] mental pain.” Parkes (1972, p. 39) similarly described intense pangs of “severe anxiety and psychological pain” and identified this experience as “the most characteristic feature of grief.” These waves or pangs of psychological pain were described as part of a broader grief syndrome that included intrusive thoughts about the death or the deceased, yearning, disruption of sleep and appetite, and decreased behavioral activity.
In the latter half of the 20th century, researchers found that, for some bereaved adults, the grief syndrome persists for years following the loss, causing substantial distress and impairment. Various terms have been used to label this syndrome, including Persistent Complex Bereavement Disorder and Prolonged Grief Disorder. We will refer to it as Complicated Grief (CG). In recent years, the American Psychiatric Association and World Health Organization have released diagnostic criteria for this syndrome (World Health Organization, 2019; APA, 2013). Harkening back to early descriptions of bereavement, diagnostic criteria for CG in both the ICD-11 and DSM-5 include a symptom of “emotional pain.” However, this symptom is not clearly defined and has received little empirical attention in the context of bereavement. Here, we explore the phenomenon of emotional pain by turning to research outside the bereavement literature. We then assess this construct and its correlates among bereaved individuals with and without CG.
Social, Emotional, and Psychological Pain
Pain affect (i.e., the felt unpleasantness of pain, Eisenberger, 2015) is presumed to have evolved as a neural alarm system, motivating rapid withdrawal from sensory pain-inducing stimuli and fostering subsequent avoidance of physical threats (MacDonald & Leary, 2005). Over time, this neural alarm system may have become linked to survival threats beyond physical injury, such as the threat of social isolation or dissolution of attachment relationships (Baumeister & Leary, 1995; Bowlby, 1969/1982; Cacioppo et al., 2006). That is, harbingers of social isolation, including rejection, abandonment, and loss, may have acquired the capacity to trigger pain affect in a similar manner as nociceptive indices of tissue damage (Eisenberger & Lieberman, 2004; MacDonald & Leary, 2005; Panksepp, 1998). This notion of pain arising from non-physical stimuli has been suggested in several areas of psychology and has been variously referred to as emotional, psychological, social, or mental pain (MacDonald & Leary, 2005; Meerwijk & Weiss, 2011; Orbach, Mikulincer, Sirota, & Gilboa-Schechtman, 2003; Shneidman, 1993). For the sake of clarity, we will use psychological pain as an umbrella term to refer to any instance of pain affect arising from a non-physical stimulus.
There are two literatures that have given especially careful consideration to the notion of psychological pain. The first is the literature on “social pain.” MacDonald and Leary (2005, p. 202) coined the term social pain to describe psychological pain that arises specifically from the perception that one is “being excluded from desired relationships” by virtue of rejection, separation, or bereavement. There is evidence that social and physical pain affect share many similarities. For example, substances that relieve physical pain, such as acetaminophen, marijuana, and opioids, also appear to reduce pain affect associated with loneliness, social rejection, and separation distress (Deckman, DeWall, Way, Gilman, & Richman, 2014; DeWall et al., 2010; Panksepp, Herman, Conner, Bishop, & Scott, 1978). Moreover, there is some evidence that social and romantic rejection are associated with activation in brain regions implicated in pain affect arising from physical stimuli (Eisenberger & Lierberman, 2003; Fisher, Brown, Aron, Strong, & Mashek, 2010; Kross, Berman, Mischel, Smith, & Wager, 2011), including the dorsal anterior cingulate cortex (dACC) and anterior insula (for critical discussion of the literature on social and physical pain, see Lieberman, Burns, Torre, & Eisenberger, 2016; Lieberman & Eisenberger, 2015; Wager et al., 2016; Woo et al., 2014). Of particular relevance to the current study, researchers have also observed increased activation in these brain regions in response to grief-related stimuli (Gundel, O’Connor, Littrell, Fort, & Lane, 2003). Together, these studies suggest that bereavement, and reminders of bereavement, may activate the “neural alarm system” subjectively experienced as pain.
The second literature to have examined the notion of psychological pain is the research on “psychache” as a driving factor in the experience of suicidality. Reminiscent of the way that Lindemann described the “mental pain” of bereaved individuals as “waves of discomfort” (1944, p. 155), Shneidman described “overflowing waves of pain” in suicidal individuals (Shneidman, 1998, p. 131). Through case studies and observations, Shneidman developed the concept of “psychache” to describe the intense affective experiences of “hurt, anguish, or ache that takes hold of the mind” (Shneidman, 1998, p. 13). He posited that suicidal thoughts and behavior emerge when death is seen as an escape from this unbearable psychological pain (Shneidman, 1993, 1998). Consistent with this theory, self-reported psychological pain is more strongly associated with suicidal thoughts, motivation, preparation, and attempter status than are other well-established suicide risk factors, such as depression, hopelessness, and perfectionism (Flamenbaum & Holden, 2007; Holden, Mehta, Cunningham, & McLeod, 2001; Troister & Holden, 2010), and change in psychological pain over time is associated with change in suicidal thoughts and preparation for suicide (Troister, Davis, Lowndes, & Holden, 2013).
Shneidman (1998, p. 25) argued that psychological pain arises from unmet psychological needs, many of which may arise in the context of bereavement. Most saliently, bereavement frustrates the need for affiliation, nurturance, and succor recognized by Shneidman as creating “a yearning and sense of loss for what (and who) are not in her life” (Shneidman, 1998, p. 72). This observation is consistent with attachment theories of grief, which posit that bereavement removes biological and psychological regulators present in our attachment relationships that, for a subset of individuals, are difficult to fill (Bowlby, 1969/1982; Shear & Shair, 2005). Thus, bereavement likely engenders the frustrated needs that Shneidman believed were the most fertile ground for developing psychological pain and, subsequently, suicidal thoughts and behavior. Consistent with Shneidman’s theory of suicide, bereaved adults with CG are at increased risk for suicidal thoughts and behaviors (e.g., Latham & Prigerson, 2004; Mitchell, Kim, Prigerson, & Mortimer, 2005; Prigerson et al., 1999; Szanto, Prigerson, Houck, Ehrenpreis, & Reynolds, 1997), with more than half of treatment-seeking adults with CG reporting suicidal thoughts (Shear, Frank, Houck, & Reynolds, 2005; Shear et al., 2014).
The Current Study
In the literatures reviewed in the previous section, researchers from disparate backgrounds in psychological and psychiatric research each described a subjective experience of intense pain affect arising not from physical injury, but from exclusion from desired relationships or thwarted psychological needs. Notably, across disciplines, bereavement was identified as being especially likely to elicit this pain affect. Given this consistent observation and the inclusion of “emotional pain” in the ICD-11 and DSM-5 criteria for grief disorders, this painful affective experience warrants further study in bereaved adults.
In the current study, we assessed psychological pain using the Psychache Scale (PAS; Holden et al., 2001), a measured used to assess the “psychache” described in Shneidman’s theory of suicide. We used this scale to achieve three aims. First, we aimed to examine the association between psychological pain and complicated grief. We hypothesized that self-reported psychological pain would be positively correlated with overall complicated grief symptom severity, and that psychological pain would be elevated in individuals with CG. To further inform our understanding of the relationship between psychological pain and CG, we examined the correlations between psychological pain and each individual CG symptom. Second, we examined the association between psychological pain and depression. Given that psychological pain is included as a diagnostic criterion of CG, but not of depression, we anticipated that psychological pain would be more strongly associated with CG symptom severity than it would be with depression symptom severity in bereaved adults. Third, we examined the association between psychological pain and suicidal thoughts and behavior in bereaved adults. Because psychological pain has predicted suicidality in other samples (e.g., Flamenbaum & Holden, 2007; Holden et al., 2001; Troister & Holden, 2010), we hypothesized that psychological pain would be positively associated with suicidality, including current suicidal ideation, risk for suicide, and a past history of suicidal behavior. Further, we hypothesized that psychological pain would remain a significant predictor of suicide risk after accounting for the effects of depression and CG symptom severity.
Method
Subjects
Subjects were adults (age 21–65) who had experienced the death of a loved one at least one year ago and responded to an advertisement for one of two studies examining cognitive factors in bereaved adults with and without CG. Advertisements and flyers were placed in clinic waiting areas, distributed throughout the community, printed in the newspaper, and posted online (e.g., Craigslist). Exclusion criteria included non-English speaking status, current mania, current psychosis, and any other factor that would render the individual unable to provide informed consent, understand task procedures or questionnaires, or adequately ensure safety during the study visit. For inclusion in the current study, individuals must also have completed the two primary outcomes measures (i.e., Inventory of Complicated Grief and Psychache Scale). Of the 164 individuals who provided informed consent, 9 met at least one exclusion criterion. An additional 20 subjects did not complete at least one of the questionnaires that are the focus of the current study. Thus, 135 subjects were included in the final sample.
Procedure
Data for the current study were collected during an initial clinical assessment visit for two studies examining cognitive factors and their relation to CG. In both studies, we first obtained informed consent. Subjects in one study then completed a Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). Subjects in the other study completed a worksheet in which they listed people, places, and objects that were a part of their life in preparation for a later cognitive assessment and then completed the MINI. The MINI was used to assess for the presence of seventeen disorders as well as a screen for potential suicide risk. The interview was administered by trained graduate students and post-baccalaureate research assistants. If subjects endorsed current suicidal thoughts during the MINI diagnostic interview, the interviewer completed a standardized risk assessment. If subjects endorsed moderate or high risk, the interviewer developed a safety plan with the subject and provided referral resources as clinically appropriate. Subjects in both studies concluded the visit by completing a brief series of questionnaires, including the assessments of CG, psychological pain, and depression. Subjects received $20 compensation for completing this initial clinical assessment visit. The Committee on the Use of Human Subjects at Harvard University approved the study protocols.
Measures
Psychological Pain
We administered the Psychache Scale (PAS; Holden et al., 2001) to assess subjects’ experience of psychological pain. The PAS is a 13-item self-report measure. Subjects rate the frequency with which they have experienced nine different exemplars of psychological pain (e.g., “I seem to ache inside;” “My pain makes my life seem dark”) on 5-point scale ranging from Never to Always. Subjects additionally rate their agreement with five items pertaining to the severity of their psychological pain (e.g., “I can’t take my pain anymore”) on a 5-point scale ranging from Strongly Disagree to Strongly Agree. Subjects are explicitly instructed to respond to these items in regards to their psychological pain, not their physical pain (Holden et al., 2001). Scores on the PAS range from 13–65, with higher scores indicating more severe psychological pain. The scale has demonstrated strong internal consistency, reliability, and incremental validity for predicting suicide-related outcomes relative to other established measures of suicidality (Holden et al., 2001). Internal consistency in the current study was excellent (α = .94).
Psychopathology
To assess CG symptom severity, we administered the Inventory of Complicated Grief (ICG; Prigerson et al., 1995), a 19-item measure assessing symptoms of the CG syndrome. Each item is rated on a 5-point scale assessing the frequency of symptoms from Never to Always. ICG scores range from 0 to 76, with higher scores indicating increased symptom severity. Consistent with prior research, we considered a score of ≥ 30 on the ICG in subjects bereaved at least one year to indicate the presence of CG (Shear et al., 2005; Shear et al., 2016; Marques et al., 2013). Internal consistency in the current study was excellent (α = .93).
We administered the Quick Inventory of Depressive Symptomatology – Self Report (QIDS-SR; Rush et al., 2003) to assess symptoms of depression. The QIDS-SR is a 16-item self-report assessment in which subjects rate symptoms of depression on a 4-point scale ranging from Not Present to Severe. A total score is calculated based on 9 symptoms of depression. Total scores range from 0–27, with a score of 6 indicating mild depression, a score of 11 indicating moderate depression, and a score of 16 indicating severe depression. In order to avoid inflating the correlation between depression and suicidal ideation or behavior in the current study, we calculated a second QIDS score omitting the suicidal thoughts question (i.e., QIDS item 12) and used this score for all analyses. Scores on the 15-item version of the QIDS-SR range from 0–24. Internal consistencies of both versions of the measure were good (α = .83 for full QIDS, α = .84 for QIDS without suicide item).
Suicidal Thoughts & Behaviors
To assess suicidal thoughts and behaviors, we administered the suicide risk module of the MINI. This module is a 13-item assessment of current risk factors for suicide (e.g., hopelessness), current thoughts about suicide, and history of suicidal behavior. Each item is rated as being present or absent. These items are then used to assess risk severity by weighting each item according to its assumed contribution to risk (e.g., endorsing hopelessness is given 1 point whereas endorsing a current suicide plan is given 8 points) and summing the items (range 0 – 52). That weighted sum score can then be used to estimate current level of risk for suicide, including low (1–8), moderate (9–16), or high (17–52) risk. Using an abbreviated version of this module, Roaldset, Linaker, and Bjørkly (2012) found that both the weighted sum score and the individual MINI suicidality items each prospectively predicted suicidal behavior at 3 and 12 months post-assessment. In this study, we focused our analyses on the weighted sum score indexing current suicidality and the individual MINI suicidality items, with a focus on items querying passive suicidal ideation (“Did you think you were better off dead or wish you were dead?”), active suicidal ideation (“Did you think about suicide?”) and history of suicide attempt (“Did you ever make a suicide attempt?”).
Data Analysis
All analyses were conducted in R version 3.6.0. Mean replacement was used to account for small amounts of missing data (.7% on the PAS and .4% on the QIDS). Associations among psychological pain and symptoms of CG, depression, and suicidality were assessed by computing Person correlations. A series of t-tests assessed hypotheses regarding greater psychological pain among individuals with CG, as well as among individuals exhibiting current passive or active suicidal ideation, a lifetime history of suicide attempt, or low or moderate risk for suicidal behavior. Multivariate stepwise logistic regression analyses assessed the relative contributions of psychological pain, depression, and CG symptoms to the presence of suicidal ideation, suicidal risk, and lifetime history of suicidal attempt in the current sample of bereaved adults. Full data and code are available at https://osf.io/435qt/.
Results
Subjects
The majority of subjects were female (62.2%) and European American (47.4%) or African-American (43.0%). The mean age was 47.3 years old (SD = 12.1). Most had lost a parent (54.8%), sibling (23.0%), or spouse (11.1%). The most common cause of death was long-term illness (49.6%), followed by short-term illness (28.9%), and accident, homicide, or suicide (18.5%). The mean duration of the relationship to the deceased was 34.4 years (SD = 17.2), ranging from 0 years, for a subject who lost a child at birth, to 61 years. The mean time since death was 5 years (SD = 6.4, range = 1–34 years).
Of the 135 individuals who participated in the study, 58 (43.0%) met criteria for CG (defined as an ICG score of ≥ 30) and 41 (30.4%) met criteria for current depression based on the MINI diagnostic interview. Current depression was notably more common in those with CG (48.3%) than among those without CG (16.9%). Lifetime depression was also more common in those with CG (84.5%) than among those without CG (63.6%). The mean CG symptom severity in the overall sample as measured by the ICG was 27.9 (SD = 16.3). The mean depression symptom severity as measured by the full QIDS (including the suicide item) was 8.5 (SD = 5.2).
In the MINI-Suicide module, most subjects demonstrated no current risk (50.4%) or low risk (41.5%) for suicidal behavior. Eleven subjects were at moderate risk (8.2%) and none were at high risk. The mean weighted sum score was 2.1 (SD = 3.4; range = 0 – 15). The most commonly endorsed item over the past month was hopelessness (39.3%), followed by thoughts that one would be better off dead or wishing for death (19.3%), thoughts about suicide (8.9%), and the desire to harm oneself (7.4%). Overall, 27 individuals (20.0%) reported at least some level of passive or active suicidal thoughts, and 25 (18.5%) reported a lifetime history of a suicide attempt.
Psychological Pain, Complicated Grief, and Depression
The correlations among psychological pain, depression and CG symptom severity appear in Table 1. Consistent with our hypothesis, psychological pain severity was significantly positively correlated with CG symptom severity, r = .68 [.57, .76], p < .01. Individuals with CG exhibited significantly greater psychological pain, M = 32.28, than bereaved individuals who did not meet criteria for CG, M = 20.92, t(93.21) = 6.78, p < .001, d = 1.30. Psychological pain among bereaved adults who did not meet criteria for CG was comparable to published samples of non-suicidal or non-clinical comparison groups (DeLisle & Holden, 2009; Flamenbaum & Holden, 2007; Holden et al., 2001). Inconsistent with our expectations, the correlation between psychological pain and depression symptom severity (not including the suicidality item) was as strong as the correlation between psychological pain and CG symptom severity (r = .68, p < .01).
Table 1.
Means, standard deviations, and correlations with confidence intervals
| Variable | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Psychache | 25.80 | 10.69 | ||||
| 2. ICG | 27.93 | 16.30 | .68** [.57, .76] | |||
| 3. QIDSa | 8.30 | 4.99 | .68** [.58, .77] | .69** [.59, .77] | ||
| 4. QIDS Suicidality | 0.18 | 0.44 | .44** [.29, .57] | .26** [.10, .41] | .34** [.18, .48] | |
| 5. MINI Suicidality | 2.07 | 3.41 | .51** [.37, .62] | .37** [.21, .51] | .39** [.23, .52] | .75** [.66, .81] |
Note. M and SD are used to represent mean and standard deviation, respectively. Values in square brackets indicate the 95% confidence interval for each correlation. The confidence interval is a plausible range of population correlations that could have caused the sample correlation (Cumming, 2014).
indicates p < .05.
p < .01. Psychache = Psychache Scale, ICG = Inventory of Copmlicated Grief, QIDS = Quick Inventory of Depression Symptoms, MINI = Mini-International Neuropsychiatric Interview suicidality weighted sum score, QIDS Suicidality = QIDS item 12.
QIDS scores were calculated excluding the suicidality item (item 12).
As an exploratory aim, we examined the relationship between psychological pain and specific symptoms of CG (see Supplementary Materials A). Although each symptom was significantly correlated with psychological pain, there was substantial variation in the strength of these correlations, ranging from relatively small (e.g., feeling drawn to places or things associated with the person who died, r = .21) to relatively large (e.g., feelings of loneliness, r =.59). Of particular relevance to the current study, the CG symptoms with the strongest associations to psychological pain were closely tied to a sense of social disconnection, including loneliness (r = .59), feelings of emptiness without the deceased (r = .58), and a feeling of being distant from other people (r = .58).
Psychological Pain and Suicidality
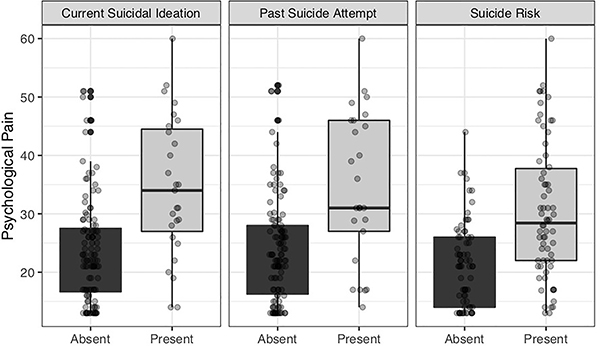
The correlations of psychological pain with MINI suicidality weighted sum score and the QIDS suicidal thoughts item appear in Table 1. Consistent with previous literature, psychological pain exhibited a moderate to strong association with both indices of suicidality, rs = .51 and .44 respectively, ps < .01. As shown in Figure 1, individuals reporting current passive or active suicidal thoughts exhibited significantly greater psychological pain (M = 34.62, SD = 12.06) than did individuals with no current suicidal thoughts (M = 23.60, SD = 9.12), t(33.80) = 4.44, p < .001, d = 1.10. Similarly, those with a lifetime history of suicide attempt reported significantly greater psychological pain (M = 34.63, SD = 12.94) than did those with no such history (M = 23.79, SD = 9.04), t(29.53) = 3.97, p < .001, d = 1.10. Overall, individuals demonstrating low or moderate risk for suicidal behavior reported significantly greater psychological pain (M = 30.43, SD = 11.62) than individuals demonstrating no risk (M = 21.37, SD = 7.16), t(108.75) = 5.37, p < .001, d = .94.
Figure 1.
Mean psychological pain in bereaved adults endorsing and not endorsing suicide risk factors. Psychological pain was measured by the Psychache Scale. Current suicidal ideation is any ideation (passive or active) reported on the Mini-International Neuropsychiatric Interview (MINI) Suicidality module. Suicide risk was assessed based on the MINI Suicidality module and participants were dichotomized into no risk and low/moderate risk groups (no subjects were at high risk). All group differences were significant (p < .001).
As can be seen in Table 2, results of stepwise multivariate logistic regression analyses examining the ICG, QIDS, and Psychache measures as predictors of suicide risk factors suggested that psychological pain remained a significant predictor of suicidal ideation, suicidal risk, and past suicide attempt when controlling for depression and CG symptom severity (βs = .73-.86, ps < .05). Depression was also a significant predictor of low or moderate suicide risk (β = .70, p = .02). However, depression was not an independent significant predictor of suicidal ideation or past suicide attempt, and complicated grief was not a significant independent predictor of any suicide variable in these multivariate analyses.
Table 2.
Logistic regression results of psychache, complicated grief, and depression scores predicting suicide risk factors.
| Predictor | β | AIC | BIC | Pr(>Chi) | |
|---|---|---|---|---|---|
| Ideation | |||||
| Step 1 | (Intercept) | −1.52*** | 131.3 | 140.0 | |
| ICG | 0.69** | ||||
| Step 2 | (Intercept) | −1.61*** | 127.3 | 139.0 | .01* |
| ICG | 0.23 | ||||
| QIDSa | 0.72* | ||||
| Step 3 | (Intercept) | −1.67*** | 122.5 | 136.6 | .007** |
| ICG | −0.16 | ||||
| QIDSa | 0.39 | ||||
| PAS | 0.86* | ||||
| Risk | |||||
| Step 1 | (Intercept) | −0.04 | 181.4 | 190.2 | |
| ICG | 0.62** | ||||
| Step 2 | (Intercept) | −0.03 | 170.2 | 181.9 | .0003*** |
| ICG | 0.02 | ||||
| QIDSa | 0.96*** | ||||
| Step 3 | (Intercept) | 0.01 | 164.6 | 179.1 | .006** |
| ICG | −0.30 | ||||
| QIDSa | 0.70* | ||||
| PAS | 0.83** | ||||
| Past Attempt | |||||
| Step 1 | (Intercept) | −1.72*** | 120.6 | 129.3 | |
| ICG | 0.90*** | ||||
| Step 2 | (Intercept) | 1.74*** | 121.5 | 133.1 | .29 |
| ICG | 0.70* | ||||
| QIDSa | 0.32 | ||||
| Step 3 | (Intercept) | −1.77*** | 118.5 | 133.0 | .03* |
| ICG | 0.36 | ||||
| QIDSa | 0.02 | ||||
| PAS | 0.73* |
Note. Ideation = any passive or active suicidal ideation reported on the MINI; Risk = low or moderate risk as determined by the MINI; Past Attempt = previous suicide attempt reported on the MINI. MINI = Mini-International Neuropsychiatric Interview, PAS = Psychache Scale, ICG = Inventory of Complicated Grief, QIDS = Quick Inventory of Depression Symptoms, β = standardized regression coefficient; AIC = Akaike information criterion.
QIDS scores were calculated excluding the suicidality item (item 12).
indicates p < .05.
indicates p < .01.
indicates p <.001.
Discussion
Psychological pain has been described as a hallmark feature of grief but has received little focus in empirical studies of CG. In this study, we assessed psychological pain in a sample of bereaved adults. Consistent with our hypotheses, psychological pain was strongly correlated with overall CG symptom severity. Relative to those reporting low CG symptom severity, those with elevated CG symptoms reported substantially elevated psychological pain. This finding is consistent with early descriptive accounts of grief (Lindemann, 1944; Parkes, 1972), recent research on the role of emotional pain in the CG symptom network (Robinaugh, Millner, & McNally, 2016), and the inclusion of emotional pain as a criterion of CG in the DSM-5 and ICD-11 (APA; 2013; World Health Organization, 2019). Our exploratory analyses examining the association of psychological pain with individual CG symptoms suggest that it may be especially tied to components of CG that reflect an ongoing sense of social isolation (e.g., loneliness, feeling distant from others, and feelings of emptiness without the deceased).
Contrary to our hypotheses, psychological pain was just as strongly correlated with depressive symptoms as it was with symptoms of CG in this sample of bereaved adults. This finding is noteworthy given that “emotional pain” is explicitly proposed as a symptom of CG in diagnostic criteria sets but is not included as a symptom of depression in the DSM. However, terms indicating pain affect are frequently used in descriptions of severe depression, especially in research on melancholia (Taylor & Fink, 2006). For example, in a memoir vividly describing his personal experience with depression, William Styron frequently referred to the pain of severe depression (Styron, 2010). William James described a “positive and active anguish, a sort of psychical neuralgia” (James, 1902, p. 147). Helen Mayberg described the experience of her depressed patients by noting, “You’re numb but you hurt. You can’t think, but you are in pain” (as cited by Dobbs, 2006). Consistent with these anecdotal observations, self-reported psychological pain has previously been found to be strongly associated with depression symptom severity across several studies (DeLisle & Holden, 2009; Li et al., 2014; Mee, Bunney, Reist, Potkin, & Bunney, 2006; Meerwijk, Ford, & Weiss, 2015; Troister & Holden, 2012, 2013; Xie et al., 2014). Our findings add to this literature, suggesting that psychological pain is also strongly positively associated with depression symptom severity among bereaved individuals.
Finally, we found that bereaved adults reporting current thoughts about suicide, a history of suicide attempt, and overall elevated suicide risk reported significantly elevated psychological pain. This is consistent with previous findings that psychological pain is a predictor of suicidal thoughts and behavior and extends these findings to a sample of bereaved adults. Logistic regression analyses further suggest that psychological pain remained a significant predictor of suicidal ideation and elevated suicide risk after controlling for the effects of depression and complicated grief. Accordingly, psychological pain should be monitored among bereaved adults, especially given the increased risk of suicidal thoughts and behavior in this population (Latham & Prigerson, 2004).
Future Directions
Together, these findings strongly suggest that psychological pain warrants further study in bereaved adults, as well as those with depression and those at risk for suicidal thoughts and behaviors. Central to this effort will be the need to clarify the nature of psychological pain. In other words, it will be important to clarify what is being measured by the Psychache Scale. There are at least three possibilities worthy of further consideration. First, psychological pain may simply denote general emotional distress. From this perspective, the Psychache Scale would capture the intensity of distress wrought by different negative emotional experiences. This perspective is perhaps most consistent with Shneidman’s (1993, 1998) notion of psychological pain, which, he hypothesized, can arise from a wide range of frustrated needs and negative emotions.
Alternatively, psychological pain may refer to a discrete emotional experience that is distinct from other negative emotions. This perspective is perhaps most consistent with the social pain literature, which posits specific evolutionary origins, biological bases, and subjective qualities of social pain that distinguish it from other emotional experiences (e.g., MacDonald & Leary, 2005). From this view, psychological pain is not merely a synonym for distress; it is a distinct affective experience that, our data would suggest, is strongly tied to complicated grief, depression, and suicidal thoughts and behavior in bereaved adults.
Finally, perhaps psychological pain is neither a broad index of general distress nor a discrete emotion. Instead, pain affect may be best understood as a fundamental ingredient of emotional experience. This possibility is grounded in research suggesting that emotions are not natural kinds, but rather are constructed experiences built from diverse mental components (Barrett, 2006; Lindquist, 2013). As a given emotional experience is constructed, the presence and intensity of pain affect may vary. Psychological pain may describe the category of constructed experiences in which pain affect is the most salient ingredient of the emotional experience. For example, a bereaved individual might experience unadulterated pain affect when confronted with vivid memories of their loved one’s death, leading them to describe their subjective experience as one of intense psychological pain. In other instances, pain affect may be present but secondary to other cognitive and affective experiences. For example, a bereaved individual might experience pain affect alongside thoughts about what life would be like if the deceased were still alive and a desire to be with them again, producing a subjective feeling of intense yearning. Accordingly, the Psychache Scale may assess the extent to which this fundamental ingredient is present in the subject’s broader emotional experiences.
In addition to clarifying the emotional nature of psychological pain, it will also be important to learn more about the overlap between psychological and physical pain. The Psychache Scale (Holden et al., 2001) explicitly instructs subjects to respond to questions with regards to psychological rather than physical pain. However, many of the items could reasonably encompass both emotional and physical experiences (e.g., “I can’t take my pain anymore”; “My pain is making me fall apart”; Holden et al., 2001). Indeed, psychological pain as assessed by the PAS is associated with severity of chronic physical pain (Frumkin, Haroutounian, & Rodebaugh, 2020), and bereavement is related to poorer health including increased incidence of chronic pain (Bradbeer, Helme, Yong, Kendig, & Gibson, 2003; Stroebe, Schut, & Stroebe, 2007). In future studies, it will be important to clarify the nature of psychological pain as it pertains to both emotional and physical well-being.
In addition, it will also be important to clarify who is most susceptible to psychological pain following bereavement. In a prospective study of risk factors and their relation to specific CG symptoms following spousal bereavement, we found that self-reported interpersonal dependence and dependence on one’s spouse were the strongest prospective predictors of bereavement-related emotional pain (Robinaugh, LeBlanc, Vuletich, & McNally, 2014). Accordingly, those with high dependence on others may be especially likely to experience activation of the ‘neural alarm system’ described by Eisenberger and Lieberman (2004), perhaps because the cost of social separation is so great for these individuals.
Finally, it will also be beneficial to clarify which interventions reduce (or increase tolerance of) psychological pain following bereavement, and whether additional targeting of emotional pain is needed. For example, distress tolerance strategies in Dialectical Behavior Therapy (Linehan, 1993) may be one means of managing psychological pain in those with CG (Barrett, Tolle, & Salsman, 2017). In addition, the correlations between psychological pain and symptoms of loneliness, emptiness, and feeling distant from others suggest that efforts to directly enhance the quality and quantity of a patient’s remaining social supports may also contribute to the amelioration of psychological pain. Lastly, it will be valuable for researchers to examine the effects of recently developed cognitive behavioral therapy-based interventions for CG on both psychological pain and tolerance of psychological pain in those with CG.
Limitations
Our study has several limitations. First, although our motivating interest was to deepen our understanding of the “emotional pain” component of CG, the measure we administered was intended to assess the “psychache” construct described in the suicide literature. This measure was chosen because it is a well-established measure of what appears to be a highly overlapping construct. However, it is not clear whether these constructs are equivalent and, thus, it is unclear how well this assessment tool measured emotional pain. In future work, it will be critical to clarify the relationship between these constructs and, potentially, to develop an assessment specifically targeting the experience of emotional pain as described in the bereavement literature.
Our results may also be limited by our assessment of suicidality, as well as our relatively small sample of at-risk individuals. In future studies, it will be important to assess psychological pain among bereaved adults with greater severity of suicidal thoughts and behavior. Additionally, it will be important to obtain a thorough assessment of suicidal thoughts and behavior. In the current study, our assessment of suicide risk was focused on a binary rating of the presence or absence suicidal thoughts and behavior, a “risk score” derived from these ratings, and a single-item self-report assessment of suicidal thoughts. These assessments could potentially contribute to measurement problems and misclassification (Millner, Lee, & Nock, 2015). Finally, our data are cross-sectional, preventing us from determining directional causality in the hypothesized relationships among CG symptoms, depression symptoms, psychological pain, and suicidal thoughts and behavior. Prospective research is needed to clarify the potential role of psychological pain in promoting suicidal thoughts and behavior among bereaved individuals.
Conclusions
To our knowledge, this study was the first to examine psychological pain in the context of bereavement. Psychological pain was associated with CG and depression symptom severity as well as with suicidal thoughts and behavior. Moreover, psychological pain continued to predict suicidal thoughts, past suicide attempt, and risk for suicide after controlling for the effects of CG and depression. Together, these results suggest that further research on psychological pain in bereaved adults is warranted, with particular emphasis on clarifying the nature of psychological pain, identifying those most vulnerable to experiencing it, and developing tools for effectively ameliorating this intensely aversive affective experience.
Supplementary Material
Acknowledgments
This project was supported by the Sackler Scholarship in Psychobiology, the American Foundation for Suicide Prevention, and a National Institute of Mental Health Career Development Award (1K23MH113805-01A1).
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Barrett JJ, Tolle KA, & Salsman NL (2017). Dialectical Behavior Therapy Skills Training for Persistent Complex Bereavement Disorder. Clinical Case Studies. [Google Scholar]
- Barrett LF (2006). Are emotions natural kinds? Perspectives on Psychological Science, 1(1), 28–58. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, & Leary MR (1995). The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin, 117(3), 497–529. [PubMed] [Google Scholar]
- Bowlby J (1969/1982). Attachment and loss: Volume 1. Attachment. New York, NY: Basic Books. [Google Scholar]
- Bradbeer M, Helme RD, Yong HH, Kendig HL, & Gibson SJ (2003). Widowhood and other demographic associations of pain in independent older people. The Clinical Journal of Pain, 19(4), 247–254. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, & Spiegel D (2006). Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality, 40, 1054–1085. [Google Scholar]
- Deckman T, DeWall CN, Way B, Gilman R, & Richman S (2014). Can marijuana reduce social pain. Social Psychological and Personality Science, 5(2), 131–139. [Google Scholar]
- DeLisle MM, & Holden RR (2009). Differentiating between depression, hopelessness, and psychache in university undergraduates. Measurement and Evaluation in Counseling and Development, 42(1), 46–63. [Google Scholar]
- DeWall CN, MacDonald G, Webster GD, Masten CL, Baumeister RF, Powell C, … Eisenberger NI (2010). Acetominophen reduces social pain: Behavioral and neural evidence. Psychological Science, 21(7), 931–937. [DOI] [PubMed] [Google Scholar]
- Dobbs D (2006). A depression switch. New York Times Magazine, 50–55. [Google Scholar]
- Eisenberger NI (2015). Social pain and the brain: Controversies, questions, and where to go from here. Annual Review of Psychology, 66, 601–629. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, & Lieberman MD (2004). Why rejection hurts: The neurocognitive overlap between physical and social pain. Trends in Cognitive Sciences, 8, 294–300. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, & Lieberman MD (2003). Does rejection hurt? An fMRI study of social exclusion. Science, 302, 290–292. [DOI] [PubMed] [Google Scholar]
- Fisher H, Brown LL, Aron A, Strong G, & Mashek DJ (2010). Reward, addiction, and emotion regulation systems associated with rejection in love. Journal of Neurophysiology, 104, 51–60. [DOI] [PubMed] [Google Scholar]
- Flamenbaum R, & Holden RR (2007). Psychache as a mediator in the relationship between perfectionism and suicidality. Journal of Counseling Psychology, 54(1), 51. [Google Scholar]
- Granek L (2010). Grief as pathology: The evolution of grief theory in psychology from Freud to the present. History of Psychology, 13(1), 46. [DOI] [PubMed] [Google Scholar]
- Gundel H, O’Connor M, Littrell L, Fort C, & Lane RD (2003). Functional neuroanatomy of grief: An fMRI study. The American Journal of Psychiatry, 160(11), 1946–1953. [DOI] [PubMed] [Google Scholar]
- Holden RR, Mehta K, Cunningham EJ, & McLeod LD (2001). Development and preliminary validation of a scale of psychache. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 33(4), 224. [Google Scholar]
- Hooley JM, Franklin JC, & Nock MK (2014). Chronic pain and suicide: Understanding the association. Current Pain & Headache Reports, 18(8), 435. doi: 10.1007/s11916-014-0435-2 [DOI] [PubMed] [Google Scholar]
- James W (1902). The Varieties of Religious Experience (Vol. 15). Cambridge, MA: The Riverside Press. [Google Scholar]
- Kross E, Berman MG, Mischel W, Smith EE, & Wager TD (2011). Social rejection shares somatosensory representations with physical pain. Proceedings of the National Academy of Sciences of the United States of America, 108(15), 6270–6275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham AE, & Prigerson HG (2004). Suicidality and bereavement: Complicated grief as psychiatric disorder presenting greatest risk for suicidality. Suicide and Life-Threatening Behavior, 34(4), 350–362. doi: 10.1521/suli.34.4.350.53737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Xie W, Luo X, Fu R, Shi C, Ying X, … Wang X (2014). Clarifying the role of psychological pain in the risks of suicidal ideation and suicidal acts among patients with major depressive episodes. Suicide and Life-Threatening Behavior, 44(1), 78–88. [DOI] [PubMed] [Google Scholar]
- Lieberman MD, Burns SM, Torre JB, & Eisenberger NI (2016). Reply to Wager et al.: Pain and the dACC: The importance of hit rate-adjusted effects and posterior probabilities with fair priors. Proceeding of the National Academy of Arts and Sciences, 113(18), E2476–2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman MD, & Eisenberger NI (2015). The dorsal anterior cingulate cortex is selective for pain: Results from large-scale reverse inference. Proceedings of the National Academy of Sciences, 112(49), 15250–15255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindemann E (1944). Symptomatology and management of acute grief. American Journal of Psychiatry, 101(2), 141–148. [DOI] [PubMed] [Google Scholar]
- Lindquist KA (2013). Emotions emerge from more basic psychological ingredients: A modern psychological constructionist model. Emotion Review, 5(4), 356–368. [Google Scholar]
- Linehan M (1993). Cognitive-behavioral treatment of borderline personality disorder: Guilford press. [Google Scholar]
- MacDonald G, & Leary MR (2005). Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin, 131(2), 202–223. [DOI] [PubMed] [Google Scholar]
- Marques L, Bui E, LeBlanc N, Porter E, Robinaugh D, Dryman MT, … & Simon N (2013). Complicated grief symptoms in anxiety disorders: prevalence and associated impairment. Depression and Anxiety, 30(12), 1211–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mee S, Bunney BG, Reist C, Potkin SG, & Bunney WE (2006). Psychological pain: a review of evidence. Journal of Psychiatric Research, 40(8), 680–690. [DOI] [PubMed] [Google Scholar]
- Meerwijk EL, & Weiss SJ (2011). Toward a unifying definition of psychological pain. Journal of Loss and Trauma, 16(5), 402–412. [Google Scholar]
- Meerwijk EL, Ford JM, & Weiss SJ (2015). Resting-state EEG delta power is associated with psychological pain in adults with a history of depression. Biological psychology, 105, 106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner AJ, Lee MD, & Nock MK (2015). Single-item measurement of suicidal behaviors: validity and consequences of misclassification. PLoS One, 10(10), e0141606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell AM, Kim Y, Prigerson HG, & Mortimer MK (2005). Complicated grief and suicidal ideation in adult survivors of suicide. Suicide and Life-Threatening Behavior, 35(5), 498–506. doi: 10.1521/suli.2005.35.5.498 [DOI] [PubMed] [Google Scholar]
- Orbach I, Mikulincer M, Sirota P, & Gilboa-Schechtman E (2003). Mental pain: a multidimensional operationalization and definition. Suicide and Life-Threatening Behavior, 33(3), 219–230. [DOI] [PubMed] [Google Scholar]
- Panksepp J (1998). Affective neuroscience: The foundations of human and animal emotions. New York, NY: Oxford University Press. [Google Scholar]
- Panksepp J, Herman B, Conner R, Bishop P, & Scott JP (1978). The biology of social attachments: opiates alleviate separation distress. Biological Psychiatry. [PubMed] [Google Scholar]
- Parkes C (1972). Bereavement: Studies of grief in later life. London: Tavistock, 39. [Google Scholar]
- Prigerson HG, Bridge J, Maciejewski PK, Beery LC, Rosenheck RA, Jacobs SC, … Brent DA (1999). Influence of traumatic grief on suicidal ideation among young adults. American Journal of Psychiatry, 156(12), 1994–1995. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Maciejewski PK, Reynolds CF, Bierhals AJ, Newsom JT, Fasiczka A, … Miller M (1995). Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research, 59(1–2), 65–79. [DOI] [PubMed] [Google Scholar]
- Roaldset JO, Linaker OM, & Bjørkly S (2012). Predictive validity of the MINI suicidal scale for self-harm in acute psychiatry: a prospective study of the first year after discharge. Archives of Suicide Research, 16(4), 287–302. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, LeBlanc NJ, Vuletich HA, & McNally RJ (2014). Network analysis of persistent complex bereavement disorder in conjugally bereaved adults. Journal of Abnormal Psychology, 123(3), 510–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ, & McNally RJ (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, … Keller MB (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. [DOI] [PubMed] [Google Scholar]
- Shear MK, Frank E, Houck PR, & Reynolds CF, (2005). Treatment of complicated grief: a randomized controlled trial. Journal of the American Medical Association, 293(21), 2601–2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear MK, Reynolds CF, Simon NM, Zisook S, Wang Y, Mauro C, … & Skritskaya N (2016). Optimizing treatment of complicated grief: A randomized clinical trial. Journal of the American Medication Association: Psychiatry, 73(7), 685–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear K, & Shair H (2005). Attachment, loss, and complicated grief. Developmental Psychobiology: Journal of the International Society for Developmental Psychobiology, 47(3), 253–267. [DOI] [PubMed] [Google Scholar]
- Shear MK, Wang Y, Skritskaya N, Duan N, Mauro C, & Ghesquiere A (2014). Treatment of complicated grief in elderly persons: a randomized clinical trial. Journal of the American Medication Association: Psychiatry, 71(11), 1287–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, … Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59 Suppl 20, 22–33. [PubMed] [Google Scholar]
- Shneidman ES (1993). Suicide as psychache: A clinical approach to self-destructive behavior. London: Rowan & Littelefield publishers. [Google Scholar]
- Shneidman ES (1998). The suicidal mind: Oxford University Press, USA. [Google Scholar]
- Simon NM, Shear KM, Thompson EH, Zalta AK, Perlman C, Reynolds CF, … & Silowash R (2007). The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry, 48(5), 395–399. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H, & Stroebe W (2007). Health outcomes of bereavement. The Lancet, 370(9603), 1960–1973. [DOI] [PubMed] [Google Scholar]
- Styron WC (2010). Darkness visible: A memoir of madness: Open Road Media. [Google Scholar]
- Szanto K, Prigerson H, Houck P, Ehrenpreis L, & Reynolds CF (1997). Suicidal ideation in elderly bereaved: The role of complicated grief. Suicide and Life-Threatening Behavior, 27(2), 194–207. doi: 10.1111/j.1943-278X.1997.tb00291.x [DOI] [PubMed] [Google Scholar]
- Taylor MA, & Fink M (2006). Melancholia: the diagnosis, pathophysiology and treatment of depressive illness: Cambridge University Press. [Google Scholar]
- Troister T, Davis MP, Lowndes A, & Holden RR (2013). A five-month longitudinal study of psychache and suicide ideation: replication in general and high-risk university students. Suicide and Life-Threatening Behavior, 43(6), 611–620. [DOI] [PubMed] [Google Scholar]
- Troister T, & Holden RR (2010). Comparing psychache, depression, and hopelessness in their associations with suicidality: A test of Shneidman’s theory of suicide. Personality and Individual Differences, 49(7), 689–693. [Google Scholar]
- Troister T, & Holden RR (2012). A two-year prospective study of psychache and its relationship to suicidality among high-risk undergraduates. Journal of Clinical Psychology, 68(9), 1019–1027. [DOI] [PubMed] [Google Scholar]
- Troister T, & Holden RR (2013). Factorial differentiation among depression, hopelessness, and psychache in statistically predicting suicidality. Measurement and Evaluation in Counseling and Development, 46(1), 50–63. [Google Scholar]
- Wager TD, Atlas LY, Botvinick MM, Chang LJ, Coghill RC, Davis KD, … Yarkoni T (2016). Pain in the ACC? Proceedings of the National Academy of Arts and Sciences, 113(18), E2474–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo C, Koban L, Kross E, Lindquist MA, Banich MT, Ruzic L, … Wager TD (2014). Separate neural representations for physical and social rejection. Nature Communications, 5, 5380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2019). International Statistical Classification of Diseases and Related Health Problems (11th ed.).
- Xie W, Li H, Luo X, Fu R, Ying X, Wang N, … Wang X (2014). Anhedonia and pain avoidance in the suicidal mind: Behavioral evidence for motivational manifestations of suicidal ideation in patients with major depressive disorder. Journal of Clinical Psychology, 70(7), 681–692. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.